Introduction
Oppositional defiant disorder (ODD) and conduct disorder (CD) represent two of the leading diagnoses for youth referred to psychiatric care (Loeber et al. Reference Loeber, Burke, Lahey, Winters and Zera2000). Furthermore, ODD and CD are associated with later substance use problems (White et al. Reference White, Xie, Thompson, Loeber and Stouthamer-Loeber2001), multiple mood and anxiety disorders (Nock et al. Reference Nock, Kazdin, Hiripi and Kessler2007) and antisocial personality disorder (Kim-Cohen et al. Reference Kim-Cohen, Caspi, Moffitt, Harrington, Milne and Poulton2003). The DSM-IV (APA, 1994) defines ODD as a ‘pattern of negativistic, hostile, and defiant behavior’ toward authority figures continuing for at least 6 months and resulting in significant impairment in functioning. Full DSM-IV ODD diagnosis requires the presence of at least four of eight discrete symptoms (Table 1). CD is characterized by the violation of ‘the basic rights of others … or societal norms or rules' and significant impairment in functioning occurring in an individual under the age of 18. Full DSM-IV CD diagnosis requires at least three of 15 symptoms (Table 1) within the past year and at least one symptom within the past 3 months. ODD and CD share unifying themes of problem behavior in excess of developmental and societal norms, and some CD symptoms seem to represent a more extreme version of ODD symptoms. Despite these unifying themes, the DSM-IV considers CD and ODD distinct diagnostic entities but specifies a hierarchal structure such that a diagnosis of ODD may be applied only if criteria are not met for CD. This is in contrast to ICD-10 (WHO, 1992), in which ODD is treated as a subtype of CD (for a more complete examination of DSM-IV and ICD-10 diagnoses of CD and ODD, see Rowe et al. Reference Rowe, Maughan, Costello and Angold2005).
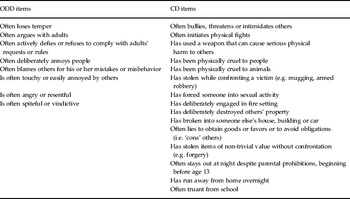
Table 1. DSM-IV items for oppositional defiant disorder (ODD) and conduct disorder (CD)

The DSM-IV conceptualization and specification of ODD and CD lead to an important question: are DSM-IV ODD and CD etiologically distinct or are they manifestations of an underlying shared liability? We can address this through genetically informed designs, which can aid in clarifying the pathogenesis of these behaviors by disentangling sources of covariance while simultaneously allowing the DSM-IV hierarchical structure. Prior studies have indicated a shared liability, suggesting that etiological studies can safely combine CD and ODD symptoms. However, most studies to date have either not used DSM-IV criteria because of timing of data collection or failed to accurately model the DSM-IV hierarchical structure specified for these two disorders. Thus, in this study, we address the questions: (i) what is the etiological structure of the covariation between DSM-IV CD and ODD and (ii) does the etiological structure support the practice of combining CD and ODD when the DSM-IV diagnostic hierarchy is reflected accurately?
Are ODD and CD etiologically distinct?
Genetically informative designs are ideal for the exploration of whether disorders share the same etiology because biometric models can be used to test directly the degree to which symptoms of each disorder, along with their co-morbidity, are explained by common genetic and environmental influences (Rhee et al. Reference Rhee, Willcutt, Hartman, Pennington and DeFries2008). Univariate models of CD and ODD suggest that genetic influences are important for each diagnosis (Ehringer et al. Reference Ehringer, Rhee, Young, Corley and Hewitt2006) and that shared environment plays a crucial role in CD (e.g. Knopik et al. Reference Knopik, Heath, Bucholz, Madden and Waldron2009). In the current study, however, we were primarily interested in whether these two disorders share genetic or environmental influences. More specifically, can, or should, we treat them separately or can we combine them for future genetically informed investigations?
Most studies looking at ODD and CD have created an ODD/CD phenotype by combining ODD/CD symptoms (Silberg et al. Reference Silberg, Rutter, Meyer, Maes, Hewitt, Simonoff, Pickles, Loeber and Eaves1996; Nadder et al. Reference Nadder, Rutter, Silberg, Maes and Eaves2002) and thus making the assumption that these disorders can be combined from an etiological perspective. These investigations have generally provided support for the importance of genetic influences on the ODD/CD phenotype and, because it is typically modeled in the same analyses, a genetic correlation with attention-deficit hyperactivity disorder (ADHD), while the role of shared environment was negligible (Silberg et al. Reference Silberg, Rutter, Meyer, Maes, Hewitt, Simonoff, Pickles, Loeber and Eaves1996; Nadder et al. Reference Nadder, Rutter, Silberg, Maes and Eaves2002). Other investigators, however, have reported the importance of shared environmental effects to the relationship between the ODD/CD phenotype and ADHD (Burt et al. Reference Burt, Krueger, McGue and Iacono2001, Reference Burt, Krueger, McGue and Iacono2003).
There are also some studies that consider the etiology of the covariation between ODD and CD, when modeled as separate behaviors. For example, an investigation that modeled ODD and CD separately (as part of a larger model including ADHD) found support for shared genetic influence across the three phenotypes in a sample of 14-year-old twins (Dick et al. Reference Dick, Viken, Kaprio, Pulkkinen and Rose2005). Eaves et al. (Reference Eaves, Rutter, Silberg, Shillady, Maes and Pickles2000) also explored the shared genetic influences on DSM-III ADHD, ODD and CD in 8–18-year-old twins, with findings suggesting that ODD and CD were more strongly genetically correlated than either disorder was with ADHD.
In one of the only studies to date that considered ODD and CD separately using DSM-IV symptom criteria, Tuvblad et al. (Reference Tuvblad, Zheng, Raine and Baker2009) examined shared genetic and environmental influences on DSM-IV symptoms of ADHD, ODD and CD in 9–10-year-old twins; however, the DSM-IV hierarchical structure was not modeled. Their findings supported a latent externalizing behavior factor underlying covariance among ADHD, ODD and CD, with most of the variance (57%) attributable to genetic influences and 19% associated with non-shared environment. Shared environment did not contribute to the variance of the latent externalizing factor.
There are many risk factors that might plausibly be expected to influence both ODD and CD (e.g. family history of antisocial personality disorder or substance dependence). However, it is also highly likely that there are genetic influences or environmental influences that influence the aggressive behaviors of CD but have no influences on ODD (e.g. Kendler et al. Reference Kendler, Aggen and Patrick2013). Dissecting common versus specific influences on DSM-IV ODD versus CD is important from many perspectives. For the purposes of gene-mapping studies of disruptive behavior, for example, it would be important to know whether genetic influences observed for ODD reflect genetic influences on differences among individuals with risk for ODD, or merely genetic influences on CD that are shared and might be explained by personality or other heritable risk factors. For the purposes of prevention research, it would be important to understand whether genotype × environment interaction effects are arising through influences on genetic effects associated with ODD that may also influence CD, versus genetic effects that specifically influence CD. For example, results might help to inform why not all children with ODD progress to CD (Rowe et al. Reference Rowe, Maughan, Costello and Angold2005) or why ODD has been associated with higher levels of co-morbid psychopathology than CD (Maughan et al. Reference Maughan, Rowe, Messer, Goodman and Meltzer2004).
Current study
The majority of extant studies examining genetic and environmental overlap between ODD and CD have (a) included ADHD and (b) used DSM-III or other diagnostic criteria or, if using DSM-IV, did not model the hierarchical structure. Given the common research practice of combining CD and ODD into one outcome and the clear hierarchical nature of DSM-IV criteria for these two disorders, it is important to determine empirically how best to handle these constructs in future genetically informative research. Thus, in a sample of female twins, we examined the etiological structure of DSM-IV ODD and CD without ADHD and determined whether, in the absence of ADHD, CD and ODD are etiologically distinct or share a common underlying liability. We used a two-stage modeling strategy (Heath et al. Reference Heath, Martin, Lynskey, Todorov and Madden2002b ) to examine genetic and environmental influences on both outcomes and the covariance between them, while accurately reflecting the DSM-IV-imposed structure for these disorders. Thus, we examined the overlap between these disruptive behavior disorders while closely approximating the diagnostic process undertaken by clinicians.
Method
Participants
Data were from the Missouri Adolescent Female Twin Study (MOAFTS), a sample of female adolescent twin pairs and their parents. The MOAFTS is a longitudinal study of the development of alcohol problems and associated psychopathology in females (Heath et al. Reference Heath, Howells, Bucholz, Glowinski, Nelson and Madden2002a ; Waldron et al. Reference Waldron, Madden, Nelson, Knopik, Glowinski, Grant, Lynskey, Jacob, Sher, Bucholz and Heath2012). All twin pairs born in Missouri between 1 July 1975 and 30 June 1985 were identified from birth records. Ascertainment of families occurred from 1995 to 1998. After exclusion of families with no maternal diagnostic interview and missing data, 1446 twin pairs [831 monozygotic (MZ) and 615 dizygotic (DZ) pairs; ∼65% of identified families; for details on non-participation see Heath et al. Reference Heath, Howells, Bucholz, Glowinski, Nelson and Madden2002a ] with complete data on all variables were included in the present analysis. Of this sample, 13% classified themselves as minority and almost exclusively as African-American, reflecting the minority composition of the Missouri population. Self-reported maternal education levels included 9.8% ‘without high school diploma’, 39.5% ‘high school diploma without any college education’, 29.2% ‘some college education’ and 21.4% ‘degree from 4-year college or more’.
Measures
A brief initial parental interview about zygosity (Nichols & Bilbro, Reference Nichols and Bilbro1966) was conducted. Comprehensive structured diagnostic telephone interviews were scheduled with parents and twin pairs. Verbal consent was obtained from all participants prior to participation, in addition to parental consent for the participation of their minor children. The Institutional Review Board at Washington University, St Louis, approved all procedures.
Assessment
The parent interview was a modified version of the Semi-Structured Assessment for the Genetics of Alcoholism (SSAGA; Bucholz et al. Reference Bucholz, Cadoret, Cloninger, Dinwiddie, Hesselbrock, Nurnberger, Reich, Schmidt and Schuckit1994), which is a comprehensive interview that assesses physical, psychological, social and psychiatric manifestations of alcohol abuse/dependence and related psychiatric disorders in adults. Modifications were made to the SSAGA to incorporate DSM-IV (APA, 1994) criteria and to adapt it for telephone use (see Bucholz et al. Reference Bucholz, Cadoret, Cloninger, Dinwiddie, Hesselbrock, Nurnberger, Reich, Schmidt and Schuckit1994; Hesselbrock et al. Reference Hesselbrock, Easton, Bucholz, Schuckit and Hesselbrock1999 for SSAGA reliability and validity data). In this interview, parents (typically mothers) were asked to report about behaviors in the twins, including symptoms of ODD. Parent reports and also twin self-reports were based on the Diagnostic Interview for Children and Adolescents (DICA; Reich, Reference Reich2000) and the child version of the SSAGA (C-SSAGA) adapted for telephone use.
Child CD and ODD
Lifetime diagnoses of child CD and ODD were based on the DICA (Reich, Reference Reich2000). CD was based on twin self-report of the 15 DSM-IV items endorsed and ODD was based on maternal report of the eight DSM-IV items endorsed (Table 1). The use of adolescent ratings for CD and maternal ratings for ODD is supported by findings demonstrating that, although prevalence estimates do not differ for ODD or CD between maternal and adolescent ratings, adolescent ratings of CD result in stronger agreement with lifetime diagnosis from a clinical interview and might better capture true behavior as parents are sometimes unaware of CD-consistent behaviors (Rothen et al. Reference Rothen, Vandeleur, Lustenberger, Jeanpretre, Ayer, Gamma, Halfon, Fornerod, Ferrero and Preisig2009). Maternal ratings of ODD, similar to maternal ratings of ADHD (Biederman et al. Reference Biederman, Ball, Mick, Monuteaux, Kaiser, Bristol and Faraone2007), meaningfully capture ODD symptomatology because ODD behavior is directed towards authority figures and is typically more noticeable at home.
Data preparation
Using a two-stage genetic model, we moved beyond an either/or diagnosis for both CD and ODD, which would have resulted in a binary measure for each disorder. Prior simulations for this two-stage strategy have indicated increased statistical power when outcomes are defined using multiple categories. More specifically, in the two-stage model, it is ideal for the first variable (i.e. CD; Fig. 1 a), to have at least three categories, at least two of which include individuals who can be assessed on the second variable (i.e. ODD). It is also preferable to define the second variable as a quantitative or multiple category variable (Heath et al. Reference Heath, Martin, Lynskey, Todorov and Madden2002b ). In two-stage models using binary measures, the variance components will not be seriously biased; however, a serious bias may arise for estimates of the genetic and environmental correlations between outcomes (Heath et al. Reference Heath, Martin, Lynskey, Todorov and Madden2002b ). These problems can be reduced if several ordered categories can be defined for outcomes.

Fig. 1. (a) Full two-stage model specification (shown for one twin only) and (b) parameter estimates from the full model (model 1, Table 4). For our two-stage modeling approach and according to the DSM-IV hierarchy, oppositional defiant disorder (ODD) was set to missing if an individual endorsed three or more conduct disorder (CD) symptoms. A, Additive genetic; C, shared environment; E, non-shared environment.
Thus, to maximize power and capitalize on the empirical patterns in our data, CD was defined using multiple categories: no symptoms, one symptom, two symptoms, or three or more symptoms. ODD was similarly defined using multiple categories: missing, no symptoms, one symptom, two symptoms, three symptoms, or four or more symptoms. Only in the case where an individual endorsed three or more CD symptoms was their ODD value was set to missing. This data preparation step was performed prior to the structural two-stage modeling to align with the DSM-IV diagnostic structure. It is important to note that, by modeling the data in this way, we excluded only ODD data (i.e. set only ODD to missing) in 145 cases, while leaving the CD value in these 145 cases in the model to contribute to the estimation of variance components for CD. The ODD profiles of these excluded cases and for all other categories of CD are shown in Table 2. Thus, the model jointly analyzes DSM-IV CD and ODD using all information about CD and, according to DSM-IV, ODD information from all individuals who do not meet prior criteria for CD. Analysis of our DSM-IV CD and ODD variables, based on the maximum likelihood estimation of the polychoric correlation (see Olsson, Reference Olsson1979), indicated no deviation from bivariate normality (p = 0.5517).
Table 2. Two-way contingency table and profiles of oppositional defiant disorder (ODD) symptom counts for each category of conduct disorder (CD)

a The ⩾ 4 ODD symptom category is shown broken down by number of symptoms and the sum total.
b The last two columns explicitly show the part of the table that is unobservable according to DSM-IV and thus may be considered to summarize structural missing data because those with a CD diagnosis cannot be characterized on the ODD dimension.
Data analysis
Genetic model fitting
To determine the extent of genetic and environmental influences on risk of DSM-IV CD and ODD, structural equation models were fitted to the data using Mx (Neale et al. Reference Neale, Boker, Xie and Maes2003). In genetic twin analyses, models are tested that partition variance in an outcome into genetic [additive (A) and non-additive (D)] and environmental [shared (C) and non-shared (E)] components. Additive genetic influences (A) describe the effect of multiple genes that exert influence in a linear or additive fashion. In general, non-additive genetic effects (D) describe interactive effects of different alleles and include genetic dominance (within locus interaction) and epistasis (across locus interaction); however, most twin studies interpret D as genetic dominance (Rettew et al. Reference Rettew, Rebollo-Mesa, Hudziak, Willemsen and Boomsma2008). Shared environmental effects (C) are those influences that make members of a family more similar to one another. Non-shared environmental effects (E) make members of twin pairs different. E also includes measurement error. We denote a2 for the proportion of total variance due to additive genetic effects, d2 for non-additivity, c2 for shared environment and e2 for non-shared environmental contributions.
Genetic modeling takes advantage of the differing degrees of genetic relatedness among MZ versus DZ twin pairs. MZ twins share all additive and non-additive genetic effects whereas DZ pairs share, on average, 50% of additive and 25% of non-additive genetic effects. Shared environmental effects are assumed to correlate 1.0 between members of both MZ and DZ pairs. Consequently, the phenotypic correlation between MZ twin pairs is r MZ = a2 + d2 + c2 and the phenotypic correlation between members of DZ twin pairs is r DZ = 0.5a2 + 0.25d2 + c2. Examining the pattern of MZ and DZ correlations can provide guidance on model-fitting strategy, such that (a) 0.5r MZ = r DZ suggests additive genetic influences, (b) 0.5r MZ < r DZ suggests both additive genetic and shared environmental influences and (c) 0.5r MZ > r DZ suggests additive and non-additive genetic influences.
The pattern of univariate and cross-twin cross-trait polychoric correlations (Table 3) suggests that, for CD, ODD and co-morbid CD-ODD, additive (rather than both additive and dominant) genetic factors influence both the variance and the covariance. The pattern also suggests important shared environmental influences for the variance of both outcomes, but not necessarily for the co-morbidity between CD and ODD. Thus, our model fitting includes A, C and E components.
Table 3. Polychoric and cross-twin correlations between DSM-IV-defined conduct disorder (CD) and oppositional defiant disorder (ODD) categories used in the two-stage model
MZ, Monozygotic; DZ, dizygotic.
Two-stage genetic model
To examine whether DSM-IV CD and ODD are etiologically distinct or exhibit shared liability, a two-stage model (Fig. 1 a) was fit to the data. This two-stage model is similar to a Cholesky decomposition model (Neale & Cardon, Reference Neale and Cardon1992) and has been used previously to examine the relationship between initiation of substance use and progression to heavier use (e.g. Heath et al. Reference Heath, Martin, Lynskey, Todorov and Madden2002b ). An important difference from the Cholesky model is that, as part of data preparation, a missing data structure consistent with the DSM-IV is imposed on the data such that, as described earlier, individuals with values of at least three on CD will not have ODD (i.e. ODD is set to missing). The missing data structure is considered Missing At Random (MAR; Little & Rubin, Reference Little and Rubin1987) because the probability of structural missing data on ODD is determined solely by values on CD. This model examines additive genetic, shared and non-shared environmental influences on both outcomes and also the relationship between them. We also computed 95% likelihood-based confidence intervals (CIs).
We extended the two-stage model to control for age by jointly modeling the probit regression of outcome (i.e. CD or ODD) on age and the genetic and environmental contributions to the residual variance and covariance among CD and ODD. To control for the age range in these data and following Knopik et al. (Reference Knopik, Sparrow, Madden, Bucholz, Hudziak, Reich, Slutske, Grant, McLaughlin, Todorov, Todd and Heath2005, Reference Knopik, Heath, Bucholz, Madden and Waldron2009), we modeled age as a contrast coded covariate allowing for three age groups: 11–14, 15–18 and ⩾19 years. Models were fitted by maximum likelihood using Mx (Neale et al. Reference Neale, Boker, Xie and Maes2003), which is designed to handle MAR data and has been shown in simulations to appropriately recover the true polychoric correlation in two-stage models that incorporate structurally missing data (Heath et al. Reference Heath, Martin, Lynskey, Todorov and Madden2002b ). Under this adjusted threshold model, genetic (additive) and environmental (shared and non-shared) parameter estimates were obtained after controlling for age.
Results
Twin pairs ranged in age from 11 to 23 years (mean = 15.15 years). The ODD profiles across categories of CD and the prevalence rates are shown in Table 2. These rates are comparable to similar studies of community-based populations (e.g. Maughan et al. Reference Maughan, Rowe, Messer, Goodman and Meltzer2004; Nock et al. Reference Nock, Kazdin, Hiripi and Kessler2007).
Genetic analyses
The results of the two-stage model are presented in Table 4 and Fig. 1 b. The variance components and correlations obtained from fitting the full two-stage model confirm significant genetic influences on CD (a2 = 0.28, 95% CI 0.06–0.52) and ODD (a2 = 0.60, 95% CI 0.46–0.76) and are consistent with prior reports (Dick et al. Reference Dick, Viken, Kaprio, Pulkkinen and Rose2005; Ehringer et al. Reference Ehringer, Rhee, Young, Corley and Hewitt2006). Shared and non-shared environmental influences were also significant and important for both outcomes, a finding that moves beyond AE models reported for these phenotypes (Ehringer et al. Reference Ehringer, Rhee, Young, Corley and Hewitt2006; see Table 4), although the magnitude of non-shared environmental effects differed between the two constructs. The estimated genetic correlation between CD and ODD was 0.52 (95% CI 0.18–1.0), implying that genetic influences on DSM-IV CD account for approximately 27% of the genetic variance in DSM-IV ODD. The estimated shared (r C = 0.28) and non-shared (r E = 0.03) environmental correlations between CD and ODD from the full two-stage model did not differ significantly from zero.
Table 4. Two-stage model of conduct disorder (CD) and oppositional defiant disorder (ODD) using the DSM-IV hierarchy: model fit statistics, standardized variance components and genetic and environmental correlations. All models were adjusted for age

A, Additive genetic; C, shared environment; E, non-shared environment; df, degrees of freedom.
95% confidence intervals given in parentheses.
We proceeded to formally test whether DSM-IV CD and ODD can be considered etiologically distinct by fitting a series of submodels to the data (Table 4). Model 1 is our full two-stage model described above and the model to which all submodels were compared. Models 2 and 3 dropped shared environmental effects and additive genetic influences respectively, and did not provide a better fit [AE model (model 2): Δχ 2 = 19.01, df = 3, p < 0.001; CE model (model 3): Δχ 2 = 106.5, df = 3, p < 0.001]. Model 4 tested an orthogonal genetic liability model in which the genetic covariance between CD and ODD is set to zero (i.e. r A = 0 or path a21 = 0). This model fit the data poorly (Δχ 2 = 8.65, df = 1, p = 0.003); however, model 5, which tested an orthogonal shared environmental liability model (r C = 0 or c21 = 0), provided a more parsimonious fit to the data (Δχ 2 = 1.45, df = 1, p = 0.229). We then fit two unidimensional models (models 6 and 7) in which the specific genetic (model 6, a22 = 0) and shared environmental (model 7, c22 = 0) paths were dropped. This unidimensional model tests whether all genetic (model 6) or environmental influences (model 7) on ODD are shared with CD. Model 6 did not result in a significant detriment of fit (Δχ 2 = 3.03, df = 1, p = 0.082) and model 7 fit the data poorly (Δχ 2 = 6.65, df = 1, p = 0.01). Finally, we fit a model that combined unidimensional genetic effects (model 6) with orthogonal shared environmental effects (model 5). This model (model 8) also fit well (Δχ 2 = 3.64, df = 2, p = 0.162) and suggests that all of the genetic influences on ODD might be shared with CD whereas shared environmental effects are specific to each disorder.
To compare patterns of results from the two-stage model with the more common practice of analyzing symptom counts, we also ran a bivariate model using DSM-IV CD and ODD symptom counts (Table 5). This model included all individuals and ignored the DSM-IV hierarchy. Overall, the model-fitting results were similar. The correlational structure (r A, r C and r E) was also highly similar whether modeled using DSM-IV criteria or using symptom counts; however, variance component estimates and CIs for ODD (which is defined differently between these two sets of models) did differ, with genetic effects accounting for more of the variance when defined using DSM-IV criteria. Thus, our inferences about genetic effects on ODD change depending on how ODD is defined. This information could be important for future gene identification efforts in terms of how to model these behaviors to be most informative for analyses.
Table 5. Model of conduct disorder (CD) and oppositional defiant disorder (ODD) using DSM-IV symptom counts: model fit statistics, standardized variance components and genetic and environmental correlations. All models were adjusted for age

A, Additive genetic; C, shared environment; E, non-shared environment; df, degrees of freedom;
95% confidence intervals given in parentheses.
Because prior work has examined the covariation among CD and ODD in the presence of ADHD and determined significant shared genetic, shared environmental and non-shared environmental correlations between CD and ODD in the presence of ADHD (Tuvblad et al. Reference Tuvblad, Zheng, Raine and Baker2009), we ran a series of models that included ADHD. Although our results will be included in a follow-up report, our full model resulted in parameter estimates and correlations between CD and ODD (once the genetic and environmental structure of ADHD is modeled) that are entirely consistent with the current report. Specifically, once ADHD is controlled for, heritability estimates were 0.33 (95% CI 0.12–0.57) and 0.64 (95% CI 0.51–0.80) for CD and ODD respectively. Shared environmental effects were estimated for CD at 0.26 (95% CI 0.04–0.37) and for ODD at 0.24 (95% CI 0.10–0.38). The genetic correlation was 0.57 (95% CI 0.26–0.98) and shared environmental effects were not significantly correlated at 0.16 (95% CI −0.51 to 0.71).
Discussion
We examined whether DSM-IV CD and ODD are etiologically distinct or share the same underlying liability in a community-based sample of female twins. The results suggest that, in this sample, covariation among these disorders can be attributed largely to shared genetic influences (r A = 0.52, 95% CI 0.18–1.00). The best-fitting two-stage model allowed genetic influences to overlap completely with no shared environmental correlation between DSM-IV CD and ODD. Although replication is necessary, these findings suggest that DSM-IV ODD and CD should be conceptualized as manifesting primarily from the same underlying genetic vulnerability, with specific shared environmental effects contributing to individual differences in each disorder.
The combination CD/ODD phenotype
These findings suggest that summing symptom counts across these two disorders for the purposes of purely genetic analyses seems to be justified; however, formal testing of that assumption might be warranted as samples and research questions may differ. In contrast to some earlier studies (e.g. Tuvblad et al. Reference Tuvblad, Zheng, Raine and Baker2009), we also find significant specific (i.e. uncorrelated) shared environmental effects that contribute to each behavior (i.e. shared environmental influences could not be dropped from the model but r C could be set to zero). This would suggest that, for analyses that seek to examine shared environmental and also genetic correlations of CD and ODD with other phenotypes, such as substance use, it is important not to combine CD and ODD. In addition, explicating the particular shared environmental influences that contribute specifically to individual differences in each of these phenotypes could highlight potentially important therapeutic targets.
The role of ADHD
Our primary question involved the covariation of CD and ODD in the absence of ADHD. This is supported by prior studies that suggest that ADHD is a qualitatively distinct construct (Clark et al. Reference Clark, Prior and Kinsella2000; Gadow & Nolan, Reference Gadow and Nolan2002; Baving et al. Reference Baving, Rellum, Laucht and Schmidt2006; Yoon et al. Reference Yoon, Iacono, Malone, Bernat and McGue2008) that co-segregates with disruptive behaviors as a unique trait (Jain et al. Reference Jain, Palacio, Castellanos, Palacio, Pineda, Restrepo, Munoz, Lopera, Wallis, Berg, Bailey-Wilson, Arcos-Burgos and Muenke2007). However, as noted earlier, prior work has modeled ADHD alongside CD and ODD (e.g. Tuvblad et al. Reference Tuvblad, Zheng, Raine and Baker2009). In an attempt to delineate these relationships, we extended our two-stage model to include ADHD and our full model yielded results consistent with the results reported here, suggesting that our results are robust to the inclusion of co-morbid ADHD. It is important to extend these findings by including other correlated behaviors in the externalizing or behavioral disinhibition spectrum (i.e. novelty seeking or substance use; Young et al. Reference Young, Stallings, Corley, Krauter and Hewitt2000, Reference Young, Friedman, Miyake, Willcutt, Corley, Haberstick and Hewitt2009).
Contributions and limitations
The use of a two-stage model to explore genetic and environmental overlap between ODD and CD provides a novel extension of an approach often used within the substance dependence literature (Heath et al. Reference Heath, Martin, Lynskey, Todorov and Madden2002b ). This approach provides an innovative and alternative analysis of etiological influences while closely approximating the process undertaken by clinicians in diagnosing and, ultimately, treating disruptive behaviors. This close approximation to clinical diagnosis should not be undervalued. For example, in gene-identification efforts, where large samples are key, researchers might only have access to medical records with diagnostic categories. Thus, a better understanding of the etiological overlap of these disorders, as defined by DSM-IV, will be important in determining how best to model these phenotypes, such that they are the most informative.
Another important contribution is the use of a large dataset ranging in age from 11 to 23 years. Previous studies have generally used younger samples (Dick et al. Reference Dick, Viken, Kaprio, Pulkkinen and Rose2005; Lahey et al. Reference Lahey, Van Hulle, Rathouz, Rodgers, D'Onofrio and Waldman2009; Tuvblad et al. Reference Tuvblad, Zheng, Raine and Baker2009), which might not be optimal because symptoms of CD do not typically develop until later in adolescence. Therefore, prior investigations using younger samples may not completely represent the diagnostic populations they intended to capture.
Our findings have clinical implications and suggest that treating ODD and CD symptoms distinctly (and according to DSM-IV criteria) may not be warranted. This is supported by reports showing that the DSM-IV ODD criteria may miss clinically impaired children (Rowe et al. Reference Rowe, Maughan, Costello and Angold2005; Burke et al. Reference Burke, Waldman and Lahey2010). Taken together, these findings support a more continuous diagnostic approach of ODD and CD over the purely hierarchical rule of DSM-IV (see Burke et al. Reference Burke, Waldman and Lahey2010 for a more complete discussion).
Limitations
First, our sample was entirely female so we could not examine gender differences. Although prior literature suggests that the etiological structure between CD and ODD does not differ by sex (e.g. Eaves et al. Reference Eaves, Rutter, Silberg, Shillady, Maes and Pickles2000; Dick et al. Reference Dick, Viken, Kaprio, Pulkkinen and Rose2005), these prior investigations did not model DSM-IV-defined diagnoses. Furthermore, evidence suggests that both disorders are more common among males (APA, 1994). Therefore, it is important that these questions are tested in male and/or mixed gender samples. Second, future research considering longitudinal extensions of this two-stage model is warranted. For example, ODD is often thought to be a precursor to CD. Given that ODD and CD were assessed concurrently in our sample, we could not directly model this developmental question.
This study is the first to incorporate a two-stage model to explore shared genetic and/or environmental overlap among these disorders as defined by DSM-IV. This is also one of the few investigations to use an older age cohort and to explore potential overlap between CD and ODD in lieu of including ADHD in the statistical model. Replication and extension of these findings will be important for advancing the understanding of the pathogenesis and, ultimately, treatment of these disorders.
Acknowledgments
This work supported by National Institutes of Health (NIH) grants to V. S. Knopik (DA17 671 and DA023134) and A. C. Heath (AA077 28 AA090 22 AA119 98 HD049 024 and AA017 688). L. C. Bidwell is supported by DA033302, C. Flessner is supported by DA023134 (Knopik) and N. Nugent is supported by MH087240.
Declaration of Interest
None.