Introduction
Inverted papilloma is the most common benign sinonasal tumour, with an incidence of 0.6–1.5 cases per 100 000 inhabitants per year.Reference Lund, Stammberger, Nicolai, Castelnuovo, Beal and Beham 1 It is characterised by locally aggressive growthReference Lund, Stammberger, Nicolai, Castelnuovo, Beal and Beham 1 and is associated with malignancy in 3.6–7 per cent of cases.Reference Mirza, Bradley, Acharya, Stacey and Jones 2
The pathogenesis of this tumour is not fully understood, although the presence of human papilloma virus (HPV) seems to be involved in the progression of the disease.Reference Govindaraj and Wang 3 Recently, occupational risk factors, such as exposure to organic solvents and welding fumes, have been suggested to play a role.Reference d'Errico, Zajacova, Cacciatore, Baratti, Zanelli and Alfonzo 4
The treatment of choice is surgical excision. This is associated with a high rate of recurrence, which is widely believed to be secondary to incomplete resection.Reference Lund 5 – Reference Dragonetti, Gera, Sciuto, Scotti, Bigoni and Barbaro 7
There have been big advances in surgical techniques since Ward and Billroth first described this pathology back in the 1850s.Reference Lund 5 Historically, the treatment of choice was via an open approach, using lateral rhinotomy and medial maxillectomy.Reference Mackle, Chambon, Garrel, Meieff and Crampette 8 The first endoscopic resection of an inverted papilloma, by Waitz, was described in 1992.Reference Waitz and Wigand 9 Since then, the endoscopic technique has developed and is now widely used to treat this pathology. Different techniques used have ranged from simple ethmoidectomy to endoscopic maxillectomy.Reference Tomenzoli, Castelnuovo, Pagella, Berlucchi, Pianta and Delù 10
It has been recognised that inverted papillomas, even when advanced, have a relatively small area of origin in most cases.Reference Tomenzoli, Castelnuovo, Pagella, Berlucchi, Pianta and Delù 10 – Reference Landsberg, Cavel, Segev, Khafif and Fliss 12 This has led to the development of so-called attachment-oriented surgery. This technique involves identification of the attachment, subperiosteal resection and drilling of the underlying bone at the papilloma origin.Reference Tomenzoli, Castelnuovo, Pagella, Berlucchi, Pianta and Delù 10 , Reference Landsberg, Cavel, Segev, Khafif and Fliss 12 However, if this technique does lead to a reduction in recurrence, it has not been investigated outside of individual case series.
Two reviews comparing the open and endoscopic approaches were published in 2006. The first, a meta-analysis, favoured an endoscopic over an open approach.Reference Busquets and Hwang 13 The second systematic review found a lower recurrence rate for endoscopically operated patients, but concluded that there was not enough evidence to support one approach over the other.Reference Karkos, Fyrmpas, Carrie and Swift 14 Uncertainty therefore remains with regard to the optimal surgical treatment in managing this condition.
Since the 2006 reviews, more recent studies have claimed even lower recurrence rates of 5–6.7 per cent, using either an endoscopic approach or a combined approach.Reference Dragonetti, Gera, Sciuto, Scotti, Bigoni and Barbaro 7 , Reference Lombardi, Tomenzoli, Buttà, Bizzoni, Farina and Sberze 15 – Reference Carta, Blancal, Verillaud, Tran, Sauvaget and Kania 17 Hence, we decided to review the literature since 2007 and determine any factors which might account for the lower recurrence rates.
Materials and methods
A literature search was performed of articles published from January 2007 to December 2013 using the Medline database with the search term ‘inverted papilloma’. Only original articles with a clear statement of the surgical approach (endoscopic, combined or open) were included. The use of additional treatments was recorded. Cases of easily accessible lesions removed via endonasal non-endoscopic procedures were not included in our review.
Previous nasal surgery, with the exception of pre-operative biopsy, was recorded. Subsequent surgery was classified as revision surgery.
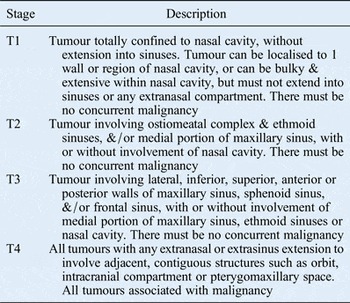
All lesions for which a Krouse staging classificationReference Krouse 18 could not be established were excluded (Table I). Case series discussing isolated sphenoid sinus disease, for example, were included, as these were classified as Krouse stage T3 disease.
Table I Krouse staging system for inverted papillomaReference Krouse 18
Review articles and articles not written in the English language were excluded. To reduce a potential bias, case reports or series consisting of less than five patients were excluded. Similarly, case series containing patients with less than 12 months’ follow up or an average follow up of less than 2 years were not considered in this review. Articles not fulfilling our inclusion criteria were excluded and no further information was gathered by contacting the individual authors.
The main outcome measure was recurrence rate. For analysis, the individual studies were combined and grouped according to the surgical approach and technique used. Fisher's exact test was performed to investigate differences between the studies.
Results
The literature search of the term ‘inverted papilloma’ revealed 328 hits on Medline (Figure 1). After screening, 52 case series and no randomised controlled trials were identified. Of these, 16 articles fulfilled the inclusion criteria (Table II).Reference Mackle, Chambon, Garrel, Meieff and Crampette 8 , Reference Landsberg, Cavel, Segev, Khafif and Fliss 12 , Reference Lombardi, Tomenzoli, Buttà, Bizzoni, Farina and Sberze 15 , Reference Pagella, Giourgos, Matti, Canevari and Carena 16 , Reference Oikawa, Furuta, Nakamaru, Oridate and Fukuda 19 – Reference Sciarretta, Fernandez, Farneti and Pasquini 30 The most common reasons for exclusion were lack of common outcome measures, short length of follow up and variable information with regard to the exact procedures performed.

Fig. 1 Flow chart of search strategy.
Table II Approach and recurrence data for the included case series

Pts = patients
A formal meta-analysis of the specific surgical procedure used was not possible because of inconsistent descriptions of site of origin and procedure.
Demographics
The literature search yielded data for a total of 1385 patients, 1044 men and 341 women, with an average age of 54.1 years. Of the included papers, 7 originated from Asian countries contributing 835 patients, 6 were European papers with 545 patients, 2 were from the Middle East with 86 patients, and 1 originated from South America and comprised 5 patients.
The Krouse stage for all lesions was established. Of the cases, 116 were Krouse stage T1, 498 were stage T2, 716 were stage T3 and 55 were stage T4.
Bilateral disease was found in 3.3 per cent of the cases. Of the patients, 4.4 per cent had a metachronous or synchronous carcinoma.
In 10 of the 16 case series, information regarding primary versus revision surgery was available. Of 1133 cases, 25 per cent were identified as revision surgery cases. A comparison of those studies with a higher proportion of revision cases (45.9 per cent) with those with a lower proportion of revision surgery (21.7 per cent) showed a significantly lower recurrence rate in the case series that had more revision cases (p = 0.0001).
Surgical approach
The majority of patients (n = 1021) were operated upon using a purely endoscopic approach. In 251 patients, the surgeon used a combined endoscopic and open approach; 113 patients were treated via an open approach.
The total recurrence rate for all patients was 11.5 per cent. The recurrence rate was: 11.1 per cent for the endoscopic approach group, 12.0 per cent for the combined approach group and 14.2 per cent for the open approach group (Table II). There was no significant difference in the recurrence rate between the endoscopic and the combined approach groups (p = 0.6574), or between the endoscopic and open approach groups (p = 0.3477).
The included cases were divided into two groups to see whether there was a trend towards a lower recurrence rate in the endoscopically treated patients in more recent years. One group included cases operated upon prior to 2000 and the second group included cases operated upon after 2000. Analysis revealed a higher rate of recurrence (11.6 per cent) in the former group, compared to 7.7 per cent in the more recent group; however, the difference was not statistically significant (p = 0.1960).
Surgical technique
In 10 case series, the authors described attachment-oriented removal of the tumour. These papers showed a highly significant lower recurrence rate of 6.9 per cent (p = 0.0001).
Case reports where intra-operative frozen sections were used to ensure clear resection margins also showed a highly significant lower recurrence rate (of 7.0 per cent) compared to the studies that did not use frozen sections (p = 0.0001). Taking the Krouse stages into consideration, there was no significant difference for the frozen section cohort or for the attachment-oriented treated patients between the compared groups (p = 0.8221 and p = 0.2071 respectively).
Geographical aspects
Analysis of the included papers with regard to their geographical origin demonstrated a difference in recurrence rate between global regions. A higher recurrence rate was reported in Asian papers (835 patients) compared to European and Middle Eastern papers combined (545 patients). This difference was significant for purely endoscopically operated patients (p = 0.0001) and for patients operated on using any technique (p = 0.0003).
Follow up
The average length of follow up was 49.8 months (range, 27–167 months). The average time between surgery and recurrence was 18.7 months. Comparison of the studies with a longer average follow up (85.9 months) with those with a shorter follow up (33.8 months) revealed no significant increase in cases of recurrence (p = 0.4852).
There were no data regarding the incidence of malignant transformation during the reported follow-up periods.
Discussion
Surgical approach findings
An endoscopic approach to treat inverted papilloma seems to be favoured by most authors. The development of curved microdebriders and drills has led to a less invasive endoscopic approach.Reference Pagella, Giourgos, Matti, Canevari and Carena 16 Endoscopic procedures have been shown to shorten the length of hospital stay compared to open surgery.Reference Sauter, Matharu, Hörmann and Naim 31 The absence of any facial scarring is a further major advantage of endoscopic surgery.
The overall recurrence rates reported by the publications included in our review are comparable with the recurrence rates previously established.Reference Busquets and Hwang 13 , Reference Karkos, Fyrmpas, Carrie and Swift 14 The low recurrence rates recently reportedReference Lombardi, Tomenzoli, Buttà, Bizzoni, Farina and Sberze 15 , Reference Liu, Yu, Minovi, Wei, Wang and Zheng 23 , Reference Sciarretta, Fernandez, Farneti and Pasquini 30 have been achieved predominantly using an endoscopic approach.
There appears to be a trend towards a lower recurrence rate in more recently carried out surgery. This may be because of advances in surgical equipment or it may reflect a learning curve in those surgeons managing inverted papilloma.
Surgical techniques to improve tumour clearance
Study protocols describing the use of frozen sections had a significantly lower recurrence rate. Hence, our review suggests that frozen sections used to ensure complete excision may be of benefit in endoscopic surgery. The use of frozen sections in other medical fields, for instance Moh's micrographic surgery, has demonstrated a low incidence of local recurrent disease.Reference Rowe, Carroll and Day 32 However, frozen sections might not be widely available or cost effective.
Tomenzoli et al. advocated the meticulous use of subperiosteal dissection in the involved areas in order to improve recurrence rates.Reference Tomenzoli, Castelnuovo, Pagella, Berlucchi, Pianta and Delù 10 Since then, others have followed this attachment-oriented surgical concept. In this review, those studies that applied the attachment-oriented surgical approach had a significantly lower recurrence rate than those which did not.
Even in advanced tumours, the attachment site is reported to be quite small.Reference Landsberg, Cavel, Segev, Khafif and Fliss 12 The origin of the attachment might play an important role in terms of access. However, Lombardi et al. did not find a statistically significant difference for the risk of recurrence based on site of origin in his case series.Reference Lombardi, Tomenzoli, Buttà, Bizzoni, Farina and Sberze 15
In 10 of the 17 studies, pre-operative histology data were available. In eight case series, the diagnosis of inverted papilloma was confirmed in all patients pre-operatively; in two reports, this was not the case. The studies with a confirmed pre-operative diagnosis showed a significantly lower recurrence rate than the one with a variable pre-operative histological diagnosis (p = 0.0052).
Geographical differences
The reason for the significantly higher rate of recurrence in papers originating from Asia remains unclear. At this stage, no significant racial difference in the prevalence of inverted papilloma is known.Reference Lund, Stammberger, Nicolai, Castelnuovo, Beal and Beham 1 A different distribution of HPV subtypes has been discussed in the past, but a recent meta-analysis did not find a significant difference in HPV prevalence associated with different geographical regions.Reference Syrjänen and Syrjänen 33
It is difficult to determine surgical experience in the individual papers; however, this could be a significant factor as endoscopic techniques were originally established in Europe and the USA.
Alternative surgical techniques
Our literature search revealed one paper describing the use of a computer-guided system.Reference Philpott, Dharamsi, Witheford and Javer 34 In this case series, the recurrence rate was 11 per cent, and therefore similar to the generally accepted rate of 12 per cent.Reference Busquets and Hwang 13 , Reference Karkos, Fyrmpas, Carrie and Swift 14 Nevertheless, the authors concluded that the use of such a system would be beneficial. Following a prospective, non-randomised study of 123 patients, a Swiss team concluded that computer-assisted functional endonasal sinus surgery did not lead to better clinical outcomes.Reference Tschopp and Thomaser 35
Most case series describing the outcomes of surgery for inverted papilloma consist of primary and revision cases. The discussion of both groups combined is controversial as it is not yet clear whether revision cases have a higher recurrence rate than primary surgery cases. Some authors state that there is no significant difference for the risk of recurrence based on previous surgery;Reference Dragonetti, Gera, Sciuto, Scotti, Bigoni and Barbaro 7 , Reference Lombardi, Tomenzoli, Buttà, Bizzoni, Farina and Sberze 15 , Reference Kim, Hong, Lee, Jin, Kang and Lee 26 other authors claim a higher recurrence rate for revision cases.Reference Sham, Woo, van Hasselt and Tong 36
Our review showed a significantly lower recurrence rate for studies with a higher proportion of revision cases. The reasons for this are unclear. A possible explanation could be that more revision surgery is performed in tertiary centres by highly experienced rhinologists. Unfortunately, in most of the reviewed articles it is not obvious what kind of hospital the surgery takes place in.
A few authors have proposed adjunct techniques for the removal of inverted papillomas. Kaluskar et al. described the use of a potassium titanyl phosphate laser in nine patients in 2009.Reference Kaluskar, Mehta, Farnan and Basha 37 The reported recurrence rate was 11.1 per cent during an average follow-up time of 58.7 months; this rate is comparable to the widely accepted endoscopic recurrence rate of 12 per cent.Reference Busquets and Hwang 13 , Reference Karkos, Fyrmpas, Carrie and Swift 14
Our literature search revealed one case report describing the use of suction diathermy as a useful adjunct tool when endoscopically resecting an inverted papilloma.Reference Hughes, Skilbeck, Kwame, Kwa and Choa 38 Unfortunately, the follow-up period in this report was short (only 12 months) and therefore no judgement can be made on its usefulness.
Similarly, radiofrequency coblation was described in one report.Reference Syed, Mennie and Williams 39 In seven patients with inverted papilloma, the authors emphasised the minimal blood loss during surgery. No follow-up data are available to show if there is an advantage over conventional endoscopic resection.
It would be interesting to evaluate the potential role of these three adjunct techniques in inverted papilloma surgery over a longer follow-up period.
Photodynamic therapy using 5-aminolevulinic acid has been described recently.Reference Zhang, Yang and Zou 40 Cotton wool soaked in 5-aminolevulinic acid was applied for 4 hours before the tissue was irradiated with 635 nm wavelength light. Two of three patients were treated under local anaesthetic; one was treated under general anaesthetic. The authors did not find any recurrences or complications in this case series of three patients. Although their follow-up period of eight months was much too short to judge the efficiency of this treatment, it could be an interesting option for patients with contraindications for a general anaesthetic as long as the inverted papilloma is easily accessible.
Follow-up findings
The rate of recurrence and the length of follow up are linked.Reference Kim, Hong, Lee, Jin, Kang and Lee 26 If follow up is too short, recurrence or residual disease will be missed. A study from a French tertiary centre showed, for instance, that the recurrence rate for a minimum of 12 months was only 3.3 per cent; however, for the group of patients with 36 months follow up, the rate was 6.7 per cent.Reference Carta, Blancal, Verillaud, Tran, Sauvaget and Kania 17 Our review has shown that the average recurrence presents at 18.7 months post-operatively.
We excluded from our review studies with a short duration of follow up. Recurrences have been described as occurring as late as 10 years after surgery.Reference Pagella, Giourgos, Matti, Canevari and Carena 16 Other papers have described late malignant transformation occurring 13 years post-operatively.Reference Mirza, Bradley, Acharya, Stacey and Jones 2 Hence, long-term follow up seems advisable. Some authors even suggest a lifelong follow up.Reference Sham, Woo, van Hasselt and Tong 36
Limitations
In our review, a formal analysis of recurrence versus site of origin was impossible because of inconsistent and variable descriptions of the site of origin. The lack of common outcome measurements is a general problem when comparing outcomes of inverted papilloma surgery. This and the heterogeneity of the studies included in this paper are potential risks of selective reporting or publication bias.
Another difficulty is the inability to accurately evaluate the stage of disease.Reference Dragonetti, Gera, Sciuto, Scotti, Bigoni and Barbaro 7 Multiple staging systems have been developed to describe tumour extension.Reference Lund, Stammberger, Nicolai, Castelnuovo, Beal and Beham 1 We applied the Krouse classification system,Reference Krouse 18 as it is the most commonly used. It is based on the tumour extension found on computed tomography (CT) and endoscopy. The European position paper from 2010 does not give an explicit recommendation on which classification system to use.Reference Lund, Stammberger, Nicolai, Castelnuovo, Beal and Beham 1 It would be desirable if the next update of this paper made an agreement on which classification system to use.
The comparison of surgical complications proves difficult, as some authors do not include complications and others have different definitions of what constitutes a complication. For example, for some surgeons dealing with the cribriform plate, a cerebrospinal fluid leak does not count as a complication, as removal of the bone underlying the attachment of the inverted papilloma is necessary to clear the disease.Reference Landsberg, Cavel, Segev, Khafif and Fliss 12 In contrast, some authors include all minor complications, which might not have been mentioned by other authors.Reference Carta, Blancal, Verillaud, Tran, Sauvaget and Kania 17
We are aware that the questions addressed within this paper are challenging because of the considerable variation in technique that has occurred over many years with a variety of surgeons of varying specialist interest. Some surgeons work in more specialist units and deal with complex tertiary referrals, whereas others are more generalist and see a different patient cohort. In addition, inverted papilloma, which used to be treated by surgeons with a specialist interest in the head and neck, is now increasingly treated by specialist rhinological surgeons. There is unfortunately no way to control for these factors, particularly over a prolonged period of time.
It is likely that with knowledge of the improved results of endoscopic attachment-oriented surgery, most series from major centres will accept this technique as standard, and hopefully this will become the norm. However, we encourage future data collection to specify that this technique was performed, and to clarify whether or not the adjacent bone was thoroughly cleared of papilloma or drilled.
The lack of consistent and adequate follow-up duration is another major frustration, and this imposes limitations on the interpretation of results.
Conclusion
It is difficult to determine the optimum treatment for inverted papilloma, as the data published are extremely heterogeneous. Thorough planning with pre-operative CT scanning and confirmed histology findings seem advisable before the decision is made to proceed to excision.
The use of intra-operative frozen sections might be beneficial, although the cost implications of this remain to be established. Attachment-oriented excision has become established in most major centres, but details of the technique should be prospectively recorded.
Prolonged follow up over at least five years and documentation of recurrence should be positively encouraged. Awareness of the possibility of late recurrences and late malignant transformation should be made apparent amongst the specialty.





