Earthquakes, especially major ones greater than 7.0 on the Richter scale, can cause great damage to life and property. Evidence has shown that the victims of earthquakes can suffer from mental disorders, which can also affect their physical health and quality of life in the future.Reference Lo and Su 1 A mental disorder is characterized as a set of behavioral or psychological symptoms or patterns occurring in an individual that causes distress or disability and that reflects underlying psychobiological dysfunctions, as defined by the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-V).Reference Stein, Phillips, Bolton, Fulford, Sadler and Kendler 2
A number of studies about earthquakes and mental disorders in the victims, eg, posttraumatic stress disorder (PTSD), major depression, social anxiety disorder, and dysthymic disorder has been reported.Reference Lo and Su 1 , Reference Xu and Song 3 , Reference Hussain, Weisaeth and Heir 4 , Reference Nishio, Akazawa and Shibuya 5 – Reference Chan, Wang and Ho 11 An association between stress and mental disorders in pregnant women also has been made in both animal experiments and human studies.Reference Brummelte 12 , Reference Burke, Davis and Otte 13
In general, among all victims of traumatic incidents such as earthquakes, women have been found to be more vulnerable than men to mental disorders.Reference Lo and Su 1 Studies have observed that during pregnancy and in the postpartum period women experience hormonal fluctuations, including changes in their ovarian hormone and cortisol levels. These fluctuations have been reported to be related to a decrease in the volume of the hippocampus and in neurogenesis function, which play a role in the pathophysiology of major depressive disorders.Reference Campbell and MacQueen 14 Stress has been found to influence the fluctuation of hormones, subsequently increasing the susceptibility of pregnant women and animals to depression.Reference Brummelte 12 , Reference Burke, Davis and Otte 13
Among the most stressful of events, earthquakes may have a direct effect on the mental health of peripartum women. Normally, without the impact of an earthquake, the prevalence rates for major depressive disorders in pregnant and postpartum women range from 7% to 15%, which is higher than among the general population.Reference Choate and Gintner 15 – Reference Ohayon 17 The prenatal and postnatal periods, when women experience great physical and psychological changes, may be particularly important times to study the association between earthquakes and the mental health of these women. The psychological responses of pregnant women to earthquakes may have a negative impact on them and their babies, resulting in consequences such as suicide and preterm birth.Reference Kõlves, Kõlves and De Leo 18 , Reference Oyarzo, Bertoglia and Avendano 19 The effects on their mental health also may extend beyond the postpartum period.
Although some evidence of a relationship between stress and mental disorders in pregnant women is available, whether mental disorders are more prevalent after earthquakes is unclear. A comprehensive understanding of the impact of earthquakes on the mental health of pregnant and postpartum women and over the longer term is needed so that appropriate interventions can be designed to better help these women recover from such a major disaster. The aim of this systematic review is to provide an evidence-based overview of the psychological impact of earthquakes on pregnant and postpartum women, and other factors affecting their mental health.
Methods
The Search Process
A systematic search through 5 health science databases (MEDLINE, Pubmed, CINAHL, Journal@OVID, and PsycInfo) was conducted for relevant studies published in English within the last 30 years, using the key words “mental disorders”, “psychological disorders”, “psychiatric disorders”, “mental health”, “pregnant women”, “prenatal”, “postpartum women”, “postnatal”, “earthquake”, and “disaster”.
Inclusion and Exclusion Criteria
All reports relating to mental disorders in pregnant and postpartum women after an earthquake, and describing the design of experimental studies (if available) and observational studies with or without a baseline comparison group(s), were included. Excluded were reports with the following focuses: (1) other sources of stress (disasters) apart from earthquakes, (2) other study populations apart from pregnant and postpartum women, (3) outcome measures that targeted physical health only, (4) the analysis of secondary data (eg, systematic reviews), and (5) expert opinions (eg, qualitative studies, theoretical studies).
The abstracts of all of the searched articles were first examined with the inclusion and exclusion criteria in mind. Full texts of the relevant reports were subsequently retrieved for appraisal.
Results
Based on the key word searches, 89 titles were retrieved. Title screening was subsequently performed to remove duplicate reports. The abstracts of the remaining 65 reports were screened based on the inclusion and exclusion criteria. After this process, 8 reports were included for further evaluation. A flowchart of the searching and screening process is shown in the Figure.
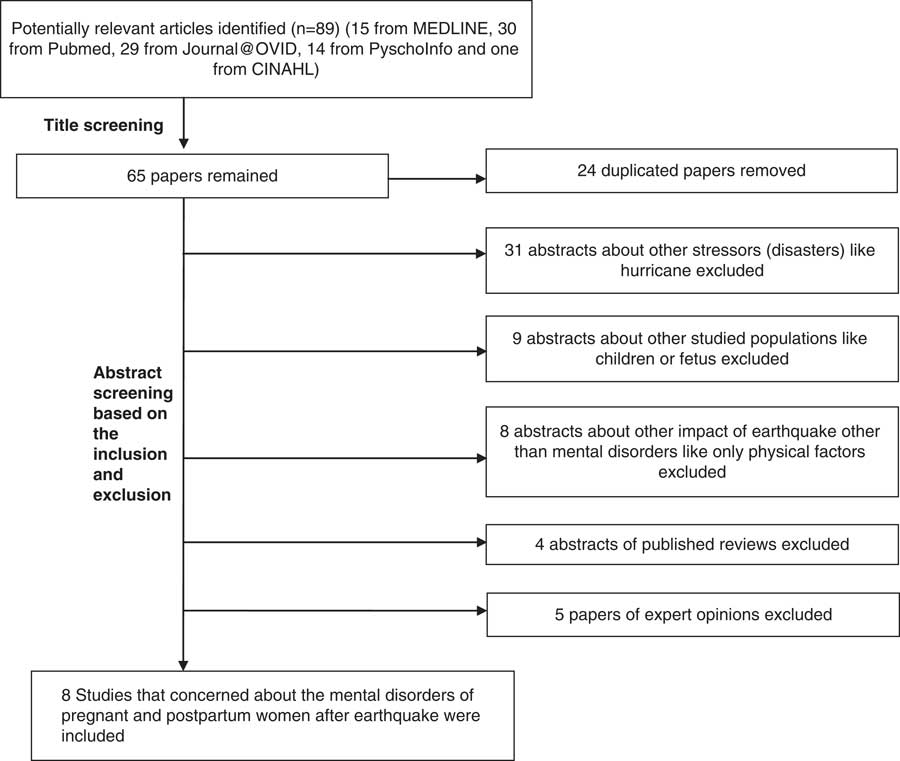
Figure Flow chart of the Search Process
Table of Evidence
The contents of the 8 studies are summarized in the Table. The variables that were recorded for this summary included the participants, the time period and scale of the earthquake, the instruments used for assessing mental disorders, the mental disorders that were studied and their prevalence, and factors apart from the earthquake that would affect the mental condition of pregnant and postpartum women.
Table Summary of the 8 Identified Papers

Abbreviations: CHQ, Chinese Health Questionnaire; EPDS, Edinburgh Postnatal Depression Scale; ESDS, Epidemiologic Studies Depression Scale (Chinese edition); IES-R, Impact of Event Scale-Revised; PTSD, posttraumatic stress disorder.
Assessing the Quality of the Studies
The quality of each article was evaluated according to the method for evaluating research guideline evidence (MERGE) checklist, developed by the New South Wales Department of Health.Reference Liddle, Williamson and Irwig 20 Similar to other evidence-assessment systems, MERGE defines the levels of evidence used in assessing the quality of research studies. The classification ranges from level 1 (the highest) to level 5 (the lowest). Level 1 represents the best evidence from results generated from a systematic review of all relevant randomized controlled trials, while level 5 represents the lowest, consisting of the opinions of respected authorities and descriptive studies. In terms of the risk of bias, there are sublevels of 1a and 1b, 2a and 2b, and 3a and 3b; a refers to low risk, and b to moderate risk.
Depression and Its Risk Factors Among Pregnant Women
The Sichuan Earthquake of 2008
Depression and its risk factors among pregnant women were assessed 4 years after the Sichuan earthquake of 2008 in China.Reference Dong, Qu and Liu 21 The strength of this exploratory cross-sectional survey was the inclusion of a comparison group. However, demographic differences were noted among the comparison group, for example, in education levels and family income. Although descriptive analyses of the demographic data for both groups were carried out in this study, the differences in the demographics were not statistically tested. Taking into consideration the design of the study and the problem of the comparability of the earthquake and comparison groups, the quality of the evidence generated from this study was considered level 4.
Another study of the impact of the Sichuan earthquake on PTSD and depression in pregnant womenReference Qu, Tian and Zhang 22 used a cross-sectional survey, randomized sampling, and the psychometrics of the instruments to assess the mental health and risk factors that were acceptable. However, no comparison group or a clear cause-and-effect relationship between the earthquake and the mental health of pregnant women could be established from the survey. Due to the observational design and the limitations of this study, the evidence generated from this study was also considered level 4.
A third study evaluated PTSD and depression among new mothers 8 months after the Sichuan earthquakeReference Qu, Wang and Tian 23 in another cross-sectional survey, and participants were randomly selected using a set of explicit inclusion criteria. Good psychometrics were reported for the instruments used in this study, eg, the Impact of Event Scale-Revised for measuring PTSD and the Chinese edition of the Center for Epidemiologic Studies Depression Scale for measuring depression. However, the scale used to evaluate earthquake experiences was not clearly defined. The lack of evidence on the reliability and validity of this scale cast doubt on the results of this study. The lack of a comparison group and the design of the study contributed to the verdict that this study was level 4 in terms of evidence.
The Wenchuan Earthquake of 2008
Symptoms of antenatal depression in Chengdu, China, 3 months before and 3 months after the Wenchuan earthquake of 2008Reference Lau, Yin and Wang 24 were investigated in this study with the use of an exploratory and comparative cross-sectional design. The setting was a city (Chengdu) located 90 km from the epicenter of the earthquake. Because Chengdu suffered less damage from the disaster than Wenchuan, this factor may have affected representativeness of the subjects. Furthermore, all of the data were collected among women who were at 12 to 24 weeks’ gestation, meaning that the sample did not comprehensively represent the antenatal population. A non-probabilistic convenience sampling strategy was used in this study, which increased the risk of sampling errors. At level 4, the quality of this study was also evaluated as low.
The 2007 Noto Peninsula Earthquake in Japan
The depressive moods of pregnant women living in the area affected by the 2007 Noto Peninsula earthquake in JapanReference Hibino, Takaki and Kambayashi 25 were studied. All of the participants in this longitudinal study were pregnant during or immediately after the earthquake, and all were followed up until 6 weeks after delivery to determine whether they suffered from depressive moods. The instruments used in this study carried good evidence of reliability and validity, but only a within-group comparison was made, without controlling for other possible factors. Thus, the cause-and-effect relationship between the earthquake and the depressive moods of pregnant women could not be clearly established.
The participants in this study received routine prenatal care at hospitals. The risk was that the prevalence of mental disorders in this sample might have been underestimated because pregnant women with severe mental symptoms were less likely to attend routine prenatal care, and might have been omitted from this study. The longitudinal design was a strong point, but considering the possibility of bias, the level of evidence for this study was rated 4.
In another study, the relationship between the Noto Peninsula earthquake and maternal postnatal depressionReference Hibino, Takaki and Kambayashi 26 was assessed in a cross-sectional survey with 155 women who had experienced the event and returned the questionnaires after childbirth. The researchers mainly focused on the relationship between the earthquake and maternal postnatal depression from 3 to 9 months after the earthquake. The participants were not randomly selected, and they were not compared with the general population. In addition, other pregnant women with mental problems who did not attend the routine prenatal care in the hospital were not included in this study. A higher risk of selection bias could not be ruled out. Due to its design, a cause-and-effect relationship could also not be established. Consequently, the evidence generated from this study was deemed to be level 4.
Taiwan 921 Earthquake of 1999
The study of psychiatric morbidity and pregnancy outcome in a disaster area of Taiwan 921 earthquake of 1999 in ChinaReference Chang, Chang, Lin and Kuo 27 included a cross-sectional survey that investigated the prevalence of PTSD and minor psychiatric disorders in pregnant women 6 to 12 months after the earthquake. The reliability and validity of the Posttraumatic Stress Reaction Checklist and the Chinese Health Questionnaire (CHQ-12) used for this study were not mentioned in the article. There was no control group for comparison that could better demonstrate a cause-and-effect relationship between the earthquake and PTSD and minor psychiatric disorders. The level of evidence for this study was 4.
The effects of the timing of the earthquake during pregnancy on emotional responses and birth outcomesReference Glynn, Wadhwa, Dunkel-Schetter, Chicz-Demet and Sandman 28 was assessed in this quasi-experimental study. The effects of the earthquake were randomly distributed across women at different stages of their pregnancies. As earthquakes are not predictable, the participants could not be randomly allocated in advance into different time groups for comparison. In addition, the psychometrics of the life-events inventory used to assess psychological responses to the earthquake were not mentioned; therefore, the criteria for evaluating outcomes were not adequately met in this study. Women who experienced the earthquake during their first and second trimesters and reported their psychological responses at 32 weeks’ gestation might have contributed to the recall bias. According to the MERGE checklist, the level of evidence for the quality of this study was 3b.
In summary, an assessment of the quality of the 8 studies in this review showed that, methodologically, most of them were cross-sectional surveys in which it was not possible to control for the impact of factors other than the earthquake on the mental health of pregnant women, given the lack of a comparable group. According to MERGE,Reference Liddle, Williamson and Irwig 20 these studies were of an insufficiently high quality to provide strong evidence of the potential mental health impact on pregnant and postpartum women after an earthquake.
DISCUSSION
Meta-analysis
The 8 studies in this systematic review varied greatly in their outcomes, which can partly be explained by the differences in the periods of time after the earthquake, and in the study designs and instruments selected for the mental health assessments in each. Given the heterogeneity of these factors, it would not be viable to conduct a meta-analysis of the studies that would combine the effects of earthquakes on the mental health of pregnant and postpartum women.
The Types of Mental Disorders
The researchers who conducted the 8 studies tended to focus on depression and PTSD. Because symptoms of depression are common in women during pregnancy and in the postpartum period, this may have contributed to the hypothesis that earthquakes, as a major stressor, could lead to a higher risk of depression in this specific group.Reference Harville, Xiong and Buekens 29 An earthquake, which can result in the loss of loved ones and in great damage to property, may have a direct effect on the mental health of pregnant women.
On the other hand, a higher rate of birth complications (eg, preterm birth, low birth weight, restricted intrauterine growth, and birth defects such as ear malformations) after an earthquake may serve as a secondary stressor specifically for peripartum women and contribute to the pathophysiology of peripartum mental disorders.Reference Oyarzo, Bertoglia and Avendano 19 , Reference Tan, Li and Zhang 30 – Reference Chazelle, Lemogne, Morgan, Kelleher, Chastang and Niedhammer 32 Major earthquakes could also potentially be traumatic for survivors, and PTSD could be an outcome of studies on the impact of earthquakes. The focus on depression and PTSD in the reviewed studies was in line with most studies on the psychological impact of earthquakes on the general population.Reference Lo and Su 1 , Reference Altindag, Ozen and Sir 6 , Reference Zhang, Shi, Wang and Liu 7 , Reference Kun, Chen and Han 9 – Reference Chan, Wang and Ho 11
Apart from depression and PTSD, minor psychiatric morbidities (MPDs) were also reported in a study about the psychiatric impact of earthquakes on pregnant women in Taiwan.Reference Chang, Chang, Lin and Kuo 27 MPDs are clinical symptoms of individuals which, in addition to depression, include anxiety, fatigue, sleep disturbances, and somatic symptoms. MPDs do not satisfy all of the criteria in defining a mental disorder according to the international classification of disease.Reference Tavares, Beck, Magnago, Zanini and Lautert 33 Symptoms of MPDs, such as anxiety and sleep disturbances, have been studied frequently in other populations after earthquakes,Reference Ehring and Razik 8 , Reference Yang, Yeh and Chen 34 and in the perinatal population that did not experience an earthquake.Reference Aktan 35 , Reference Hung, Tsai, Ko and Chen 36
Researchers have rarely taken MPDs into consideration in studies about pregnant and postpartum women after earthquakes. Because MPDs have been related not only to disaster but also to pregnancy, and because little is known about the impact of a combination of these factors, a more comprehensive exploration of this aspect of mental health is necessary. This additional evaluation would be particularly welcome, as the current review of related studies has demonstrated that such studies contain relatively low levels of evidence (3b and 4, based on MERGE).Reference Liddle, Williamson and Irwig 20
The Prevalence of Depression and PTSD
The prevalence of antenatal depression in women who experienced an earthquake during pregnancy ranged from 7.1%Reference Lau, Yin and Wang 24 to 40.8%.Reference Qu, Tian and Zhang 22 Compared with those who had not experienced an earthquake recently, the rate of antenatal depression ranged from 7% to 13%.Reference Choate and Gintner 15 Given the similar rate of 7% to 7.1% at one end, the range in the prevalence of depression among pregnant women after an earthquake (40.8%Reference Qu, Tian and Zhang 22 ) was wider than among those who had not experienced an earthquake (13%Reference Choate and Gintner 15 ). This finding clearly demonstrates that antenatal depression is more prevalent among women who experienced an earthquake during pregnancy than among those who had not.
However, the prevalence of postpartum depression among women who experienced the earthquake during pregnancy differed in range from 11.6% to 29%Reference Qu, Wang and Tian 23 , Reference Hibino, Takaki and Kambayashi 26 versus 3.5% to 63.3%Reference Klainin and Arthur 37 , Reference Tian, Li and Xie 38 when compared with those who had not experienced an earthquake. We have been unable to determine whether earthquakes are associated with a higher rate of postpartum depression.
The prevalence of PTSD after the 2008 Wenchuan earthquake was 12.2% in pregnant womenReference Qu, Tian and Zhang 22 and 19.9% in postpartum women.Reference Qu, Wang and Tian 23 These rates were higher than in the general population after the earthquake in Taiwan (10%)Reference Chou, Chou and Su 39 but lower than in the general population of mainland China (56.8%).Reference Xu and Liao 40 Nevertheless, both studies by Qu et alReference Qu, Tian and Zhang 22 , Reference Qu, Wang and Tian 23 yielded a relatively low level of evidence because, methodologically, they are cross-sectional observation studies with no concurrent comparable groups
It is unclear whether the rate of PTSD was significantly and statistically higher in pregnant and postpartum women after an earthquake than in the general population who experienced an earthquake. Further evidence is needed to demonstrate whether the incidence of depression in postpartum women and of PTSD in pregnant and postpartum women is higher in those who have experienced an earthquake, as compared to those who have not.
Timing of Studies on the Psychological Impact of Earthquakes
In this review, 7 of the 8 studies were found to have focused on relatively short-term reactions to an earthquake.Reference Qu, Tian and Zhang 22 – Reference Glynn, Wadhwa, Dunkel-Schetter, Chicz-Demet and Sandman 28 The studies were conducted at 3 monthsReference Lau, Yin and Wang 24 and up to 21 months after the incident.Reference Qu, Tian and Zhang 22 It was not unusual for researchers to pay more attention to the acute psychological reactions to the earthquake, because the earthquake was an acute stressor that happened in a very short period of time. It was also believed that individuals, including perinatal women, can recover from the mental health consequences of a disaster through adaptation after some time,Reference Harville, Xiong, Buekens, Pridjian and Elkind-Hirsch 41 and that the impact from an earthquake also would lessen with time. Although some studies have reported that disasters also can have a long-time impact on the mental health of survivors,Reference DiGrande, Neria, Brackbill, Pulliam and Galea 42 , Reference Yule, Bolton, Udwin, Boyle, O'Ryan and Nurrish 43 the participants of those studies were not pregnant or postpartum women.
On the other hand, if studies on the impact of a disaster on pregnant or postpartum women take place long after the disaster, a potential recall bias and influencing factors would weaken the rigor of those studies. Therefore, assessments on the psychological impact of an earthquake on pregnant or postpartum women should not be conducted too long after the occurrence of earthquake.
Factors Relating to the Psychological Impact of Earthquakes
To investigate appropriate interventions for the psychological disorders suffered by pregnant and postpartum women after an earthquake, it is essential to have a full understanding of the factors influencing these disorders. Various factors have been identified from the reviewed studies. They have included experiences relating to the earthquake,Reference Qu, Tian and Zhang 22 , Reference Hibino, Takaki and Kambayashi 25 – Reference Chang, Chang, Lin and Kuo 27 family relationships,Reference Dong, Qu and Liu 21 – Reference Qu, Tian and Zhang 22 , Reference Lau, Yin and Wang 24 economic factors such as family income and employment,Reference Qu, Wang and Tian 23 support from society and family,Reference Dong, Qu and Liu 21 , Reference Lau, Yin and Wang 24 , Reference Hibino, Takaki and Kambayashi 25 the timing of the earthquake during pregnancy,Reference Glynn, Wadhwa, Dunkel-Schetter, Chicz-Demet and Sandman 28 and birth history and baby-rearing.Reference Hibino, Takaki and Kambayashi 26 Earthquakes are stressful events in which differences in severity and timing may also contribute to various mental health outcomes. As such, the diversity of the individual experiences of pregnant women to earthquakes and their social support in terms of various familial factors deserve more research.
Social support, which is widely regarded as a key factor in buffering against peripartum depression in the general population,Reference Xie, He, Koszycki, Walker and Wen 44 – Reference Spoozak, Gotman, Smith, Belanger and Yonkers 48 was identified as playing an important role after an earthquake.Reference Dong, Qu and Liu 21 , Reference Lau, Yin and Wang 24 – Reference Hibino, Takaki and Kambayashi 25 Researchers clearly pointed out that social support has a positive effect on the level of psychological stress that a person suffers. It would influence the way people cope with and adjust to stressful events, thereby buffering them against adverse effects on their mental and physical health.Reference Cohen and Wills 49 , Reference Giesbrecht, Poole, Letourneau, Campbell and Kaplan 50 In this regard, it could alleviate the stress caused by an earthquake.
However, some studies have found that an earthquake could also destroy support systems, consequently leading to a higher rate of mental disorders in survivors.Reference Lau, Yin and Wang 24 , Reference Toyabe, Shioiri and Kuwabara 51 It appears that social support may act as a mediator between earthquakes and stress, and is further related to the mental health of peripartum women. However, the roles and dynamics of social support in mitigating the negative psychological effects of disasters are not very clearly or comprehensively explained in the reviewed studies (only a quantitative correlation between social support and mental disorders after an earthquake was identified). To use social support to help peripartum women after an earthquake, further evidence is needed to understand the roles and mechanism of this factor.
Among the factors related to peripartum mental health after an earthquake, family income, employment, family relationships, support from society and family, and baby-rearing were all related to the family. It was observed that for family members dealing with the demands of stress, family income and employmentReference Campbell and MacQueen 14 were necessary material resources, and family relationshipsReference Dong, Qu and Liu 21 , Reference Qu, Tian and Zhang 22 , Reference Lau, Yin and Wang 24 were the emotional resources. According to Lau et al,Reference Lau, Yin and Wang 24 Qu et al,Reference Qu, Tian and Zhang 22 , Reference Qu, Wang and Tian 23 and Dong et al,Reference Dong, Qu and Liu 21 a positive association exists between functional family relationships, especially a functional marital relationship, and the mental health of pregnant women after an earthquake. The marital relationship might serve as a resource to help family members (including pregnant and postpartum women after an earthquake) to recover from or adapt to the stress of change. Other studies also discovered that particular patterns in family relationships influenced the physiological and psychological processes of individual family members.Reference Mahboubeh, Maryam, Maryam, Masoumeh and Shokouh 52 , Reference Mash and Johnston 53
All of the described factors are aspects of family system resources that can play a role in mediating between stress and adaptation.Reference Boss and Mulligan 54 According to the Double ABCX model, family system resources are developed to satisfy the demands on the family or to help the family to adapt stressful events.Reference McCubbin, Cauble and Patterson 55 The role played by the family in dealing with the mental disorders suffered by pregnant and postpartum women after an earthquake is important and should not be underestimated. For instance, as a type of informal social support, family supportReference Martinez and Abrams 56 could play a large part in maintaining the psychological health of the family members.Reference Nygaard, Wentzel-Larsen, Hussain and Heir 57
Family support refers to a range of supportive behaviors (emotional support and instrumental support), which are provided by a family member or intimate partner through interpersonal relationships and received by another family member.Reference Kamen, Cosgrove, McKellar, Cronkite and Moos 58 Various studies have indicated that greater family support is associated with better psychological adjustment among adolescents,Reference Taylor and Roberts 59 fewer symptoms of depression,Reference Kamen, Cosgrove, McKellar, Cronkite and Moos 58 and lower rates of PTSD after a psychiatric breakdown.Reference Bokszczanin 60
Natural disasters such as an earthquake could thrust a family into a state of instability and reduce the support that family members are able to give, or lead to family dysfunction. These events could, in turn, give rise to a series of psychological problems among family members, including pregnant women.Reference Cao, Jiang, Li, Lo and Li 61 Such problems might improve or deteriorate, depending on the level of family support that is extended. This factor suggests that it is important to conduct further studies about family support for pregnant women.
The studies that were reviewed reveal a very imperfect understanding of the influence of family on the mental disorders of pregnant and postpartum women,Reference Dong, Qu and Liu 21 – Reference Lau, Yin and Wang 24 , Reference Hibino, Takaki and Kambayashi 26 as the various researchers did not conduct an in-depth investigation of the influence of family factors. As a result, information is very limited about the interactions between family and perinatal mental health. The lack of specific and robust studies about the family relationship and the mental disorders of pregnant and postpartum women after a major earthquake suggest a specific direction that can be investigated within this larger topic.
Limitations
A limitation of this review is that the searches were restricted to published papers in English. Useful information in other languages from certain countries, such as China and Japan, might have been missed. Nevertheless, this review included studies on those countries that were published in English. Because earthquakes often occur in Japan, researchers there have more experience with the psychological impact of earthquakes on pregnant and postpartum women. In future reviews, well-designed studies in the Chinese and Japanese languages could be included to generate more comprehensive results about the impact of earthquakes on pregnant and postpartum women.
Future Research
The most commonly identified mental disorders of pregnant and postpartum women were depression and PTSD. The prevalence of these mental disorders was higher after an earthquake, but some studies found it to be similar to that of the general population. The potential association between earthquakes and a higher incidence of those mental disorders in pregnant and postpartum women needs to be further explored.
In the future, more critical consideration should be given to the timing of the study of pregnant and postpartum women after an earthquake. Mental symptoms such as those for PTSD and depression in association with stressors may decrease over time.Reference Eksi and Braun 62 The mental health of pregnant and postpartum women in the period after an earthquake should be studied to better understand if earlier interventions, which may further reduce or prevent mental health problems in the long term, are warranted. The evidence from this review suggests that such a study should be conducted within 2 years after the occurrence of an earthquake.
Other influencing factors such as family support or family system resources are also important variables for future studies about the psychological impact of earthquakes on pregnant and postpartum women. Although these factors have been investigated in some of the reviewed studies and associations with mental disorders after an earthquake were found, a more comprehensive discussion of these factors was not available. These factors may act as mediators or moderators in addressing the mental disorders of pregnant and postpartum women after earthquakes. Additional studies about these factors may contribute to identifying appropriate and effective interventions for these women to recover from the associated mental health problems.
Because high-quality original studies about the mental disorders of pregnant and postpartum women after earthquakes are lacking, it is important to conduct well-designed studies such as cohort, case-controlled, or quasi-experimental studies to explore the cause-and-effect relationship between major earthquakes and the mental disorders of pregnant and postpartum women (randomized controlled studies cannot be used to explore this causal relationship because earthquakes are unpredictable). If stronger evidence existed for this relationship, the best intervention(s) to relieve the mental disorders and symptoms of pregnant and postpartum women after an earthquake would be an essential area and direction of future research. This sysematic review did not offer strong evidence as to which particular types of interventions should be considered for the mental disorders or symptoms of pregnant and postpartum women after earthquakes.
Quantitative studies are not the only choice for exploring the dynamics between family and mental disorders after an earthquake. Although 5 articles containing expert opinions were retrieved by keyword searches before abstracts were screened, terms such as qualitative descriptive study, phenomenology, ethnography, grounded theory, and focus group, which are signs of qualitative studies, did not appear in those reports. In future studies, the multifaceted human complexity and phenomenon of family support, interactions, and dynamics involving pregnant and postpartum women suffering from mental disorders after a major earthquake can be better explored with qualitative designs. For instance, a substantive theory generated from a grounded study can contribute insights for further research or for current practice.
Conclusions
As identified from this review, the current literature lacks clear indications for a better understanding of the relationship between family factors and the potential impact of earthquakes on the mental health of pregnant and postpartum women. Therefore, it is currently difficult to ascertain the evidence for a specific theoretical model that explains the essential family factors that may have an impact on the psychological and mental health of those women after an earthquake. Better evidence of the dynamics and interactions of family in relation to mental health in such a situation are necessary, before appropriate interventions to relieve any related mental health problems can be considered.
Such information could inform practice and further research. Case-controlled, quasi-experimental, and other types of assessments may be used to strengthen the research in this area of study. In particular, to better investigate and understand family support and dynamics, qualitative studies or a mixed-method approach (eg, a quantitative survey that includes more family factors and measures, supplemented by a qualitative inquiry) could be used to investigate the role of family in the mental health of pregnant and postpartum women after earthquakes.




