Introduction
Obsessive-compulsive disorder (OCD) is a chronic and disabling neuropsychiatric disorder, with a lifetime prevalence of 2%.Reference Ruscio, Stein, Chiu and Kessler 1 Despite its prevalence, OCD is poorly recognized, underdiagnosed, and undertreated, resulting in considerable cost and burden to the individual and to the health economy.Reference Hollander, Stein, Fineberg and Legault 2 Better diagnosis of OCD is a recognized public health priority.Reference Fineberg, Baldwin and Menchon 3 OCD is currently classified by the World Health Organization (WHO) in the International Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) 4 and the American Psychiatric Association (APA) in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). 5 However, these 2 major diagnostic systems show marked differences, either in the description of the disorder or in the diagnostic criteria, specifiers, and differential diagnosis. It is noteworthy that whereas the current version of the ICD-10 was approved in 1990, the DSM-5 was released in 2013, and therefore has benefitted from recent advances in the understanding of the neurobiology of OCD and its nosological relationship with several other disorders characterized by obsessive-compulsive symptomatology.
The removal of OCD from the Anxiety Disorders chapter and the establishment of the Obsessive-Compulsive and Related Disorders (OCRDs) chapter reflects the hypothesis of common external validators other than anxiety within OCRDs,Reference Stein, Fineberg and Bienvenu 6 which represent a group of disorders characterized by compulsivity. The idea of grouping disorders on the basis of compulsive features dates back to Kraepelin’s description of “compulsive insanity” (1899),Reference Kraepelin 7 in which “compulsive ideas and compulsive apprehensions dominate the clinical picture.” Although extremely relevant, Kraepelin’s conceptualization was based on his clinical intuition, whereas the OCRDs chapter in both the DSM-5 and the ICD-11 Beta Draft is now based on increasing evidence of common affected neurocircuits between disorders and reflects the shift of paradigm from the previous clustering rationale, based on interrater agreement. Although the affected neurocircuits and the specific biomarkers for OCRDs are not explicitly mentioned in the DSM-5, this nosological shift is consistent with the increasing evidence of distinct neurobiological profiles separating OCD and anxiety disorders. The neurobiology of OCD has shifted from the anxiety-avoidance paradigm—involving amygdala and prefrontal cortex network dysfunctions as key components of anxiety disordersReference Shin and Liberzon 8 —to a dysfunction of the orbitofronto-striato-pallido-thalamic circuitry and reward circuitry.Reference Menzies, Chamberlain, Laird, Thelen, Sahakian and Bullmore 9 , Reference Figee, Vink and de Geus 10 This also encompasses the identification of distinct compensatory mechanisms, which may represent candidate endophenotypes (see “Future Directions” section).Reference de Vries, de Wit and Cath 11
ICD-10 and DSM-5: Differences in the Approach to OCD and Related Disorders
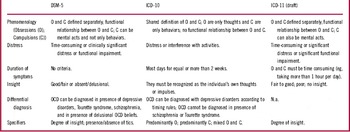
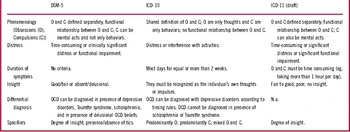
Phenomenology of obsessions and compulsions
Although obsessions and compulsions, similarly defined, represent the core features of OCD in both ICD-10 and DSM-5, there are several differences between the definitions provided in the two systems (see Table 1).
In ICD-10, OCD is characterized by “recurrent obsessional thoughts or compulsive acts.” Obsessions are defined as “ideas, images or impulses,” whereas compulsions are defined as “stereotyped behaviors that are repeated again and again.” These definitions imply a conceptualization of obsessions being uniquely cognitive events, with no mention of the increasingly recognized non-cognitive events called “sensory phenomena,”, which may precede compulsions. “Sensory phenomena” is a term that encompasses a variety of subjective experiences, also referred to as “premonitory urges,” “sensory tics,” “just-right perceptions,” “sensory experiences,” “feelings of incompleteness,” and “not just-right phenomena.”Reference Ferrão, Shavitt and Prado 12 Some authors have hypothesized that such phenomena represent specific pathological pathways and therefore contribute to the identification of OCD subgroups that are more specific.Reference Miguel, Baer and Coffey 13 The presence of these experiences may also have therapeutic consequences, since they may represent a treatment response predictor to pharmacological and behavioral therapy.Reference Miguel, do Rosário-Campos and Prado 14 – Reference Katerberg, Cath and Denys 17 On the other hand, compulsions are conceptualized as being uniquely motor behaviors, with no consideration of mental rituals. Moreover there is no mention of a functional relationship between the 2 (ie, that compulsions may arise as an attempt to reduce anxiety or distress caused by obsessions). Conversely, the DSM-5 refers to obsessions as “recurrent and persistent thoughts, urges, or images” and to compulsions as “repetitive behaviors or mental acts,” underlining in both definitions a mutual relationship between the 2, namely that that the individual may attempt to neutralize obsessions with some other thought or actions (ie, compulsions) or feels driven to perform compulsions in response to an obsession.
Additional differences concern the definition of “distress” associated with obsessions and compulsions. The ICD-10 states that obsessions and compulsions generate distress and are not pleasurable experiences, without clarifying the associated specific affects, whereas the DSM-5 states that they can be accompanied by a broad range of affective responses, some of which represent substrates for new research, such as panic attacks, strong feelings of disgust, or a sense of “incompleteness.” For instance, the feeling of disgust is a prominent negative affect in OCD, and a growing body of research suggests that abnormal disgust responses may be implicated in the OCD symptomatology, with self-reported disgust positively correlating with the severity of other OCD-spectrum symptoms.Reference Whitton, Henry and Grisham 18 The feeling of disgust was also proposed as a prime candidate for a “new” domain of temperament, and it was also proposed to play a role in the pathogenesis and maintenance of OCD.Reference Olatunji, Tart, Ciesielski, McGrath and Smits 19 In addition, whereas the ICD-10 requires a minimum duration for obsessions or compulsions, which must be present almost every day for at least 2 weeks, the DSM-5 does not focus on a specific duration requirement but rather requires symptoms to be time-consuming. This broader conceptualization of OCD can be expected to improve the diagnostic sensitivity of the instrument and capture more cases that might otherwise have been missed.
Specifiers and differential diagnosis
There are also notable differences between ICD-10 and DSM-5 in the use of specifiers and differential diagnosis. The ICD-10 specifiers pertain to the diagnostic picture of OCD, with 3 main diagnostic presentations: predominantly obsessional thoughts, predominantly compulsive acts, mixed obsessional thoughts and acts. No specifiers are provided in regard to the degree of insight, which is implicitly considered as fair/good in the definition of symptoms (“they must be recognized as the individual’s own thoughts or impulses”). The validity and utility of dividing OCD according to these specifiers has been questioned, and it is thought they will change under the ICD-11: according to the online ICD-11 Beta Draft, a new “degree of insight” specifier may be added (see the following paragraphs). Insight can be notably poor or absent in approximately 20% of OCD cases, and in the presence of poor insight, the diagnosis may be missed or confused with delusional disorders. Interestingly, poor insight cases of OCD do not require preferential treatment with antipsychotics and appear to respond just as well as insightful cases to first line treatment with selective serotonin reuptake inhibitors (SSRIs).Reference Eisen, Rasmussen and Phillips 20 On the other hand, patients with poor insight may be more difficult to engage in cognitive behavioral therapies involving exposure and response prevention.Reference Visser, van Megen and van Oppen 21 Therefore, including a specifier that validates poor insight as a recognized “subgroup” could be expected to improve the detection and treatment of OCD and draws attention to poor insight as a cardinal feature of the disorder.
Conversely, DSM-5 has 2 specifiers: the degree of insight (ranging from absent or delusional to good or fair) and the presence or absence of tics. This latter specifier also reflects the distinct “differential diagnosis” approach of DSM-5 compared to ICD-10. The ICD-10 takes a “hierarchical” approach to taxonomy and rules out the diagnosis of OCD in the presence of Tourette syndrome, as a “higher order” disorder, though high rates of comorbidity between these disorders are increasingly recognized.Reference Nordstrom and Burton 22 Moreover, the ICD-10 does not permit an OCD diagnosis in schizophrenia, whereas it suggests careful examination in the presence of depressive disorders: in these latter disorders, OCD can be diagnosed according to onset and persistence. The diagnosis of OCD is only allowed in acute depressive disorders if the OCD occurred first, and in chronic depressive disorders if the OCD symptoms persist for long periods in the absence of depression. Nevertheless, occasional panic attacks or mild phobic symptoms are no bar to the diagnosis. This approach may be considered unduly restrictive, as it hampers the diagnosis and treatment of OCD in the presence of major psychiatric disorders with which OCD is known to share considerable comorbidity, such as affective disorders (approximately 60%)Reference Fineberg, Hengartner, Bergbaum, Gale, Rössler and Angst 23 schizophrenia (approximately 25%).Reference Mukhopadhaya, Krishnaiah and Taye 24 Indeed, the relationship between obsessive-compulsive symptomatology and psychosis is long-known, and the prevalence of OC symptoms in schizophrenia and ultra-high risk (UHR) populations is higher than in the general population,Reference Byerly, Goodman, Acholonu, Bugno and Rush 25 so that OCD has also been hypothesized as a prodrome for schizophrenia.Reference Bottas, Cooke and Richter 26
In contrast, DSM-5 permits an OCD diagnosis in the presence of Tourette syndrome, schizophrenia, depressive disorder, and delusional beliefs, suggesting a differential diagnosis with a broader range of disorders such as anxiety and depressive disorders, other OCRDs, OC personality disorder, and eating disorders. This extended and non-hierarchical approach to OCD differential diagnosis in the DSM-5 is not without consequences at a clinical level. Though the DSM-5 states OCD can be distinguished from the ruminations of major depressive disorder (which are usually mood-congruent and not necessarily experienced as intrusive or distressing), sometimes in clinical practice this differentiation may not be so obvious. Thus, there may be a bias toward over-diagnosis of comorbid OCD in ambiguous cases of depression. From a clinical perspective, obsessions that present uniquely in depressive phases may be suggestive of a bipolar disorder, rather than OCD, as well as an episodic course of OCDReference Swartz and Shen 27 , Reference Zutshi, Kamath and Reddy 28 ; nevertheless the differentiation between ruminative thoughts and obsessions is not always clear, since they both are repetitive cognitive intrusions accompanied by negative emotions, are difficult to dismiss, and are subjectively experienced as loss of mental control.Reference Wahl, Schönfeld and Hissbach 29 These issues may also apply to the depressive phase of bipolar disorder with important clinical implications, since some treatments for OCD (eg, ultra-high dose SSRI) can potentially worsen bipolar symptomatology.Reference Amerio, Odone, Liapis and Ghaemi 30 Moreover, the clear identification of comorbidities between OCD and bipolar disorder may impact the treatment algorithm, favoring the administration of antipsychotics or mood stabilizers.Reference Amerio, Odone, Liapis and Ghaemi 30 , Reference Perugi, Toni, Frare, Travierso, Hantouche and Akiskal 31
On the other hand, allowing the diagnosis of OCD in schizophrenia, given the recognition of the high comorbidity rates, has opened the debate on the still controversial “schizo-obsessive” subtypeReference Poyurovsky, Weizman and Weizman 32 – Reference Varlakova, Patel and Mukhopadhaya 34 and on tentative therapeutic approaches for this highly disabled subgroup of patients.
Obsessive compulsive and related disorders
Arguably, designation by the DSM-5 of a new family of OCRDs, on the basis of age of onset, comorbidities, neurobiological factors, and treatment response, constitutes one of the major modern day advances in taxonomy and will generate considerable and much-needed new interest in the evaluation and treatment of disorders characterized by compulsivity.
A recent reviewReference Ameringen, Patterson and Simpson 35 underlines the clinical significance of grouping OCD with disorders such as body dysmorphic disorder (BDD), trichotillomania (TTM; hair-pulling disorder), excoriation (skin-picking) disorder, and hoarding disorder, and highlights their similarities across a range of validators. Other authors have gone further and have suggested dividing the OCRDs into 2 subgroups, one comprising “cognitive OCRDs” (ie, OCD, BDD, hoarding disorder) and the second comprising “body-focused repetitive behavioral disorders” (ie, TTM and skin-picking disorder).Reference Phillips, Stein and Rauch 36 , Reference Stein, Grant and Franklin 37 This proposal gains some support from the results of a large twin study examining the structure of genetic and environmental risk factors of OCRDs.Reference Monzani, Rijsdijk, Harris and Mataix-Cols 38 Two latent liability factors for OCRDs were found that were largely under genetic control. The first latent factor was common across all OCRDs and was therefore conceptualized as a nonspecific genetic vulnerability, possibly explaining the phenomenologic similarities, patterns of comorbidity, and familiarity described in the OCRD literature. The second factor, which was also strongly genetically influenced, loaded exclusively on TTM and skin-picking disorder, whereas environmental factors were shown to be largely disorder-specific.Reference Monzani, Rijsdijk, Harris and Mataix-Cols 38 In contrast, other contributionsReference Abramowitz and Jacoby 39 have questioned the empirical validity and practical utility of the new OCRDs DSM-5 chapter. The authors critically review the grouping of these disorders on the basis of relatively limited data and suggest that the OCRD concepts are based on the superficial form of symptoms and lacks scientific merit.Reference Abramowitz and Jacoby 39 Notwithstanding, the ICD-11 seems to be moving toward the approach of an OCRDs classification, tracing the DSM-5 model (see the next paragraph).
OCD and OCRDs in the Future ICD-11: Diagnosis and Classification
Recently, the Beta Draft of the ICD-11 (not final, not approved by the WHO and updated daily) has been published online. 40 , Reference Luciano 41 Even though the diagnostic criteria are not yet available, the general description of the disorder seems to reflect the acceptance of already published recommendations for the revised classification of OCD.Reference Simpson and Reddy 42
By definition, OCD in the draft ICD-11 is
… characterized by the presence of obsessions or compulsions, or both. Obsessions are repetitive and persistent thoughts, images, or urges (impulses) that are intrusive, unwanted, and commonly associated with anxiety. The individual attempts to ignore or suppress obsessions or neutralize them by performing compulsions. Compulsions are repetitive behaviors or mental acts that the individual feels driven to perform in response to an obsession, according to rigid rules, or to achieve a sense of “completeness.” In order for obsessive-compulsive disorder to be diagnosed, obsessions and compulsions must be time consuming (eg, taking more than 1 hour per day), and result in significant distress or significant impairment in personal, family, social, educational, occupational or other important areas of functioning.
This reformulated definition, although not final, seems to accept many of the recommendations recently proposedReference Simpson and Reddy 42 for the revision of the diagnostic guidelines, differential diagnosis, and specifiers of OCD. First, the draft ICD-11 has adopted the word “urge” in the definition of obsessions, which is consistent with the DSM-5 definition and is intended to reduce confusion with the impulse control disorders. However, in recognition of the growing neuropsychological evidence suggesting that impulsivity contributes to the generation of obsessive-compulsive behavior, the term “impulse” has not been completely replaced, maintaining an option for clinicians to use both words, and probably facilitating the translation to languages other than English. In addition, whereas the ICD definition still mentions the common presence of anxiety, the statement from the previous ICD-10, in which “anxiety is almost invariably present,” has been reformulated. This is consistent with the removal of OCD from the anxiety disorder section in the DSM, and seems to reflect the recognition of anxiety symptoms as variable and heterogeneous in OCD and, therefore, as a less stable and reliable key indicator of OCD.
Also, in accordance with the DSM, in the draft ICD-11 a functional relationship between obsessions and compulsions has been made explicit. Regarding obsessions, the recommendation that they may be either behaviors or mental acts has been accepted, as well as the removal of the term “stereotyped”, which might be potentially confusing with stereotypies or stereotypic movement disorder.Reference Simpson and Reddy 42 Addition of the “sense of completeness” is also noteworthy, due to the growing evidence that supports the key role and prevalence of the so-called “sensory phenomena” or “not-just-right-experiences” in OCD patients.Reference Ferrão, Shavitt and Prado 12 , Reference Hellriegel, Barber, Wikramanayake, Fineberg and Mandy 43 Last, 3 other changes are to be underlined: the modification of specifiers, which have been partly aligned to those in DSM-5, namely including the degree of insight, ranging from absent insight or delusional beliefs, poor insight, to good or fair insight (the presence of tics has not so far been included); further clarification of the functional consequences of the disorder; and the duration requirement (namely that obsessions and compulsions must be time consuming (eg, take more than 1 hour per day). Up to now, the rules for differential diagnosis are still to be elucidated.
Another key change from the ICD-10 to the ICD-11 Beta Draft involves the move to classify OCD within a broad cluster of Obsessive Compulsive and Related Disorders that is similar to, but extends beyond, that of the DSM-5. OCRDs in ICD-11 Beta Draft are defined as “a group of disorders characterized by repetitive thoughts and behaviours that are believed to share similarities in etiology, genetic determinants, and affected neurocircuits or are commonly co-occurring.” This section currently includes obsessive-compulsive disorder, body dysmorphic disorder (BDD), olfactory reference disorder, hypochondriasis, hoarding disorder, and body-focused repetitive behavior disorders (excoriation disorder and trichotillomania). Up to now, it also comprises other specified/unspecified obsessive-compulsive and related disorders, with no detailed description or definition.
The draft ICD-11 classification also proposes that this group of OCRDs may be divided into subsets, based largely on phenomenology and existing (limited) evidence of shared treatment-response profiles.Reference Grant, Chamberlain and Odlaug 44 For example, one subset may include disorders for which cognitive phenomena, such as obsessions, intrusive thoughts, and preoccupations, are central and in response individuals engage in excessive related repetitive behaviors (ie, obsessive-compulsive disorder, body dysmorphic disorder, hypochondriasis, and olfactory reference disorder). Another may include OCRDs that are primarily characterized by body-focused repetitive behaviors and involve recurrent and habitual behaviors directed at the integument and lack a prominent cognitive aspect (eg, hair-pulling, skin-picking).
New ICD-11 Disorders
In the ICD-11, the OCRDs will also encompass 2 new ICD disorders: hoarding disorder 40 , Reference Fontenelle and Grant 45 and olfactory reference disorder. 40 , Reference Veale and Matsunaga 46 Hoarding disorder is characterized by excessive accumulation of and attachment to possessions regardless of their actual value, resulting in cluttered living spaces, the use and safety of which are compromised. Excessive acquisition, characterized by repetitive urges or behaviors related to buying, stealing, or amassing items, including those that are free, is considered integral to the diagnosis, as is difficulty discarding, due to a perceived need to save items and distress associated with discarding them. In recognition of the poor levels of insight commonly found in cases of hoarding disorder, the degree of insight is included as a specifier. The proposed specifier of “severe domestic squalor”Reference Fontenelle and Grant 45 has not so far been included. Thus, the draft ICD-11 definition is similar to that in the DSM-5, although in the DSM-5 “excessive acquisition” is not essential and is included at the level of specifier.
Olfactory reference disorder is a chronically disabling disorder characterized by persistent preoccupation with emitting a perceived foul or offensive body odor that is either unnoticeable or only slightly noticeable to others and is more common in certain cultures, eg, Asia, Africa. Though the exact prevalence rates are still unknown, owing to a lack of epidemiological studies, a total of 84 case reports worldwide was estimated,Reference Begum and McKenna 47 with most reports consisting of case reports or small case series. The largest series are from Japan (N=38), Canada (N=36), Nigeria (N=32), Saudi Arabia (N=15), and Brazil (n=14).Reference Phillips and Menard 48 In contrast, in the DSM-5, this condition (named “olfactory reference syndrome,” ORS) is not listed as an independent diagnosis, but rather falls in the “Other Specified OCRDs” section and in the “Glossary of Cultural Concepts of Distress” as a restricted variant of the Japanese Taijin kyofusho (“interpersonal fear disorder”).
Clustering OCRDs: From DSM-5 to ICD-11
The ICD-11 has refined and extended the DSM-5 approach to OCRDs clustering, with an arguably stronger focus on the growing evidence supporting a coherent underpinning neurobiology. Both systems recognize compulsivity, rather than anxiety, as the main core dimension of the OCRDs. However, whereas the “etiological similarities” are not defined in the DSM-5, which refers to “a range of diagnostic validators,” the ICD-11 explicitly underlines genetic and neurobiological similarities as a basis for linking the disorders.
Both the DSM-5 and ICD-11 include five disorders in the OCRD cluster (OCD, body dysmorphic disorder, hoarding disorder, excoriation disorder, and trichotillomania), which may represent the core disorders of the section. However, the ICD-11 additionally includes olfactory reference syndrome and hypochondriasis as OCRDs, whereas the DSM-5 includes instead “substance/medication induced OCRDs” and “OCRDs due to another medical condition.” The inclusion of hypochondriasis in the ICD-11 OCRDs is probably due to an emphasis on mental “preoccupation” in its description and to the presence of excessive, repetitive checking and healthcare-seeking behaviors. Hypochondriasis has historically been included in the “anxiety and fear-related disorders” cluster, based on the phenomenological overlap with anxiety disorders including symptoms of hypervigilance toward bodily symptoms and fear-related avoidance. At this preliminary juncture (October 2015), the draft ICD-11 lists hypochondriasis in the OCRDs and the disorder has been removed from the anxiety disorders grouping. This is different from the DSM-5, which still includes “illness anxiety disorder (hypochondriasis)” in the anxiety disorders section. It is to be expected that by moving hypochondriasis into the OCRDs section, the ICD-11 would generate potentially fruitful new research perspectives that may advance understanding of the underpinning neuropsychological mechanisms and encourage new treatment development. On the other hand, the DSM-5 has broadened the OCRDs cluster to include “substance/medication induced OCRDs” and “OCRDs due to another medical condition.” These diagnoses are not considered specific mental disorders in a narrow sense, but are recognized as generic conditions that may be encountered by a mental health clinician. Their inclusion as diagnoses in the DSM-5 OCRDs is intended to raise awareness of the “non-psychiatric” origins of some obsessive-compulsive syndromes, and improve differential diagnosis and treatment.
Obsessive-Compulsive Personality Traits
A major revision to the personality disorder section of the ICD classification has been proposed,Reference Tyrer, Reed and Crawford 49 based on the growing evidence that supports a dimensional approach toward personality pathologyReference Bernstein, Iscan and Maser 50 as opposed to personality disorder categories.Reference Skodol, Gunderson and Shea 51 These dimensions of personality pathology would include “anankastic features,” such as perfectionism, extreme need to control their own and others’ behavior, and rigid adherence to rules consistent with the ICD-10 diagnosis of anankastic (obsessive-compulsive) personality disorder.Reference Tyrer, Reed and Crawford 49
The ICD-11 plans to include a system of “multiple parenting,” which allows certain diagnostic categories that could legitimately be placed in more than 1 section of the classification to be cross-referenced. Multiple parenting is expected to enhance clinical utility by ensuring increased recognition of cross-referenced disorders in differential diagnosis or as comorbidities to improve treatment-planning.Reference Stein, Kogan and Atmaca 52 Anankastic personality disorder is highly comorbid with OCD and shares a significant familial link,Reference Bienvenu, Samuels and Wuyek 53 , Reference Samuels, Nestadt and Bienvenu 54 as well as a similar neuropsychological profile, reflecting cognitive inflexibility and perseveration that corresponds to that of individuals with OCD.Reference Fineberg, Day and de Koenigswarter 55 The ICD-11 workgroup on OCD proposes that the anankastic variant of personality disorders is cross-referenced in the OCRD grouping,Reference Stein, Kogan and Atmaca 52 based on significant similarities in phenomenology (although important differences also exist such as a lack of obsessions and compulsions), as well as major comorbidity with a range of obsessive-compulsive disorders.Reference Coles, Pinto, Mancebo, Rasmussen and Eisen 56 , Reference Pinto, Mancebo, Eisen, Pagano and Rasmussen 57
Future Directions
It is clear that while significant progress is being made in classifying OCD and related disorders, with clear evidence of a convergence in the conceptualization of these disorders emerging from the 2 major global classificatory systems, a great deal of uncertainty remains. While the aspiration of “carving nature at its joints” may not be readily achievable, there are grounds to believe a better understanding of the neurobiological underpinnings will inform a more rational classification and further refine the clinical definition of individual disorders and their taxonomy.
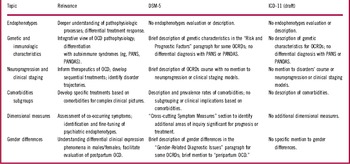
In order to overcome the limitations of the current diagnostic systems and to address the need for a new approach to classifying mental disorders, based on dimensions of observable behavior and neurobiological measures,Reference Insel, Cuthbert and Garvey 58 the National Institute of Mental Health (NIMH) has recently launched the Research Domain Criteria (RDoC) project. This aims to create a framework that integrates the most recent contributions in neuroscience and genomics, with the ultimate goal of “precision medicine,” namely a diagnostic refinement based on a deeper understanding of the circuitries and networks of psychiatric disorders considered to be brain diseases.Reference Insel 59 It is to be expected that future iterations of the DSM and ICD systems will align with the RDoC approach, with the aim of bringing neuroscience and clinical practice closer together (see Table 2).
Table 2 Summary of relevant topics to be considered

Endophenotypes represent a still debated concept, yet they are a hot topic in neuropsychiatric research. They can be conceptualized as a special kind of biomarker, encompassing heritable neurobiological and neurobehavioral characteristics that play an important role for bridging the gap between the microscopic level (eg, molecular genetics) and the macroscopic level (eg, clinical symptoms) in neuropsychiatric disorders.Reference Gottesman and Gould 60 , Reference Insel and Cuthbert 61 Neither of the existing nosological systems have so far included an adequate integration of the current knowledge about neural circuits, neurotransmitters, and behavior, as proposed by the NIMH’s RDoC project.Reference Insel, Cuthbert and Garvey 58 , Reference Cuthbert 62 However, in the DSM-5, there has been an attempt to facilitate the identification and fine-tuning of psychiatric endophenotypes, through the introduction of a “Cross-Cutting Symptom Measures” chapter. This chapter integrates a “dimensional assessment” with a “categorical diagnosis” approach. It aims at addressing the issue of co-occurring symptoms across mental disordersReference Clarke and Kuhl 63 as an adjunct tool “to give clinicians quantitative ratings that characterize patients in a way that is simple, useful, and clinically meaningful.”Reference Berry, Heaton and Kelton 64 From this perspective, the identification of specific endophenotypes, which may cross traditional categorical diagnostic boundaries, would be expected to help in both the diagnostic and therapeutic process, by providing a deeper understanding of the pathophysiological processes specific to a disorder and the differential response to specific treatments.Reference Phillips 65 For example, a better understanding of the cognitive dimension of OCRDs, in terms of overlapping attentional and planning deficits, may be particularly helpful for clarifying the strength of relationship between different OCRDs and devising new treatment strategies that target cognitive deficits.Reference Fineberg, Chamberlain and Goudriaan 66
Genetic studies in OCD are relatively scarce in comparison to those in schizophrenia and affective disorders.Reference Murphy, Moya, Fox, Rubenstein, Wendland and Timpano 67 In addition, the immunologic characteristics of OCRDs do not currently receive adequate attention. Such findings may contribute to the development of an integrative view of OCD pathophysiology, as for example the “glutamate-based genetic immune hypothesis.”Reference Rotge, Aouizerate and Tignol 68
The classification of issues pertaining to the pediatric acute-onset neuropsychiatric syndrome (PANS) highlights some of these deficiencies. PANS refers to a syndrome characterized by an abrupt, dramatic onset of OCD (meeting DSM-IV criteria) or severely restricted food intake, with the concurrent presence of additional neuropsychiatric symptoms, with similarly severe and acute onset, triggered by any infectious agent (not only streptococcal infection) in addition to non-infectious triggers, which are yet to be fully determined.Reference Swedo, Leckman and Rose 69 This syndrome has been proposed as an expanded clinical entity compared to the previous pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS).Reference Swedo, Leckman and Rose 69 Though recognized by the National Institute of Health (NIH), PANS and PANDAS are not yet validated nosological constructsReference Pichichero 70 and are not listed as a diagnosis by the ICD-10 or the DSM-5. From this perspective, a useful future specifier for OCD would be the mode of onset (acute versus progressive), which may help differentiate autoimmune clinical pictures.
A relevant issue that pertains to both diagnostic systems is the concept of staging and “neuroprogression.” Neither the DSM-5 nor the draft ICD-11 have incorporated the long-debated concept of clinical staging, which may differentiate early, milder clinical phenomena from those that accompany illness progression and chronicity. This is already a reality in several fields of medicine, and is based on the assumption that early intervention can produce better clinical and functional outcomes. Nevertheless, it is a currently neglected dimension in most psychiatric disordersReference Fava and Kellner 71 : the concept of clinical staging is emerging in the research on schizophrenia,Reference McGorry, Hickie, Yung, Pantelis and Jackson 72 together with the aim of an identification of the trajectory of the disorder and the investigation of the after effects of the duration of untreated disorder, though this still seems to be a backward approach in the OCD research.
In sum, what is currently missing in both diagnostic systems is the integration of a “clinimetric” perspective,Reference Feinstein 73 , Reference Fava, Rafanelli and Tomba 74 a concept referring to a number of clinical issues that do not find room in the current taxonomy, comprising clinical staging and severity. Such integration would also inform therapeutics of OCD and may help developing sequential treatment strategies, which are, up to now, scarcely investigated.Reference Albert and Brunatto 75 , Reference Albert, Barbaro, Aguglia, Maina and Bogetto 76 Data from the most recent meta-analyses and practice guidelinesReference Koran 77 indicate that serotonin reuptake inhibitors (SRIs) still represent the first-line pharmacological treatment (after a trial with cognitive behavioral therapy [CBT]), yet a large percentage of patients still does not achieve a symptom remission, particularly when the clinical picture includes the presence of comorbidities. Therefore, a diagnostic system allowing the identification of the clinimetric properties would facilitate research and the development of specific treatments strategies in complex clinical pictures and comorbid conditions.Reference Pallanti and Grassi 78
Last, gender evaluation is a relevant factor that should be taken in account in OCD, since gender differences have been shown in the clinical expression of OCD phenomenon.Reference Mathis, Alvarenga and Funaro 79 This is also relevant in regard to postpartum psychiatric disorders; whereas a good deal of attention has been paid to postpartum depression and psychosis, less effort has been devoted to studying OCD with a perinatal onset.
Conclusions
The classification of OCD underwent a noticeable change in the process of revision from DSM-IV to DSM-5. Although the diagnostic criteria for the disorder remained almost the same, the clustering in a new, dedicated chapter of OCRDs reflects the results of 2 decades of intensive study in the field of OCD and the recognition of close relationships and overlaps between this group of disorders.
The DSM-5 has paved the way for the forthcoming revision of the existing ICD-10, which has become outdated. The definitive ICD-11 is expected to be released 2018. A draft version in the latest stage of revision has been made available online and demonstrates prominent changes. Indeed, despite differences in the origins, purpose, and scope of the 2 classification systems,Reference First 80 the process of harmonization between them seems to be crystallizing in the field of OCRDs. These modifications are consistent with the aim of a “scientifically valid” classification system, since the proposed changes are grounded upon recent findings and a thorough review of the latest contribution in the literature. While more remains to be achieved, this represents an important step forward in the development of a “globally applicable” classification system, as it bridges the gap between the 2 nosological systems and facilitates the process of diagnosis worldwide and in both clinical and research contexts.
Disclosures
Dr. Fineberg reports grants from medical research council, grants from ECNP, grants and personal fees from Servier, other from Novartis, grants from Wellcome trust, other from Royal college of Psychiatrists, other from Janssen, other from WHO, other from college of mental health pharmacists, outside the submitted work. Dr. Marras and Dr. Pallanti have nothing to disclose.