Introduction
Mass-casualty incidents (MCIs) are events which overwhelm the resources for emergency response by the quantity and severity of casualties.Reference Kuhls, Chestovich, Coule, Carrison, Chua, Wora-Urai and Kanchanarin 1 This broad definition applies to both large-scale natural disasters with many thousands of victims and small-scale incidents which overwhelm local emergency resources despite only a handful of victims. Many otherwise treatable injuries result in fatalities due to inadequate preparedness and rationing of medical resources. Survivors of MCIs often carry long-term physical, mental, and emotional disabilities.Reference Mistovich, Karren and Hafen 2 , Reference Reinhardt, Li and Gosney 3 Although the number of first responders is variable in each locale, education in disaster preparation, triage, and treatment is vital to maximize the utility of all available personnel and minimize the loss of life.
Mass-casualty incidents are both infrequent and difficult to predict, making advance preparation a challenging endeavor. According to the World Health Organization (WHO; Geneva, Switzerland) and Centre for Research on the Epidemiology of Disasters (CRED; Brussels, Belgium), the number of recorded natural disasters and victims have increased since 1975.Reference Chakrabhan, Chandra and Levav 4 Thailand in particular has suffered both natural and man-made MCIs. On December 26, 2004, a 9.1 magnitude earthquake struck off the coast of Indonesia, triggering a tsunami which caused considerable casualties in several countries in Southeast Asia. In Thailand alone, this event resulted in 5,388 confirmed fatalities, 3,120 missing, and 8,457 injuries.Reference Braine 5 In 2011, widespread flooding in 65 of Thailand’s 77 provinces resulted in at least 884 confirmed deaths and 1.4 trillion baht (US $45 Billion) in economic damage.Reference Schwartz, Goldberg and Ashkenasi 6 Furthermore, militant Islamic secessionists in southern Thailand have terrorized citizens through bombings, arson, and other forms of violence since early 2004. Total casualties from this violence as of January 2012 were 5,243 lives and 8,941 injuries. 7 These MCIs prompted several Thai medical centers to develop disaster education programs to improve disaster and MCI preparedness.
The National Disaster Life Support (NDLS) training program was developed in 2003 to address the lack of a standardized training program for disaster management in the United States. 8 The program includes several courses which stress a comprehensive approach to help physicians, nurses, emergency responders, and other health professionals respond to MCIs. Basic Disaster Life Support (BDLS) is a one-day course within the NDLS training umbrella and provides a basic overview of the critical points to be addressed in each unique MCI scenario. Several Thai medical training programs integrated BDLS into their education to improve MCI preparedness. This paper describes the impact of BDLS training on self-assessed confidence to respond to MCIs among Thai medical professionals.
Methods
At the request of Phramongkutklao Hospital (Bangkok, Thailand), faculty from the University of Nevada School of Medicine (Las Vegas, Nevada, USA) and Medical College of Georgia (Augusta, Georgia, USA) administered a BDLS course in Bangkok, Thailand on July 14, 2008 for Thai health care professionals. The course lasted eight hours, and all participants were required to pass a written test at the end. Course content included the following subjects: (1) disaster paradigm; (2) natural disasters; (3) traumatic and explosive events; (4) nuclear and radiologic events; (5) biological events; (6) chemical events; (7) psychological aspects of disasters; and (8) public health implications of disasters. Information was collected on the participants’ demographics, occupational and military experience, prior disaster management experience, and disaster training.
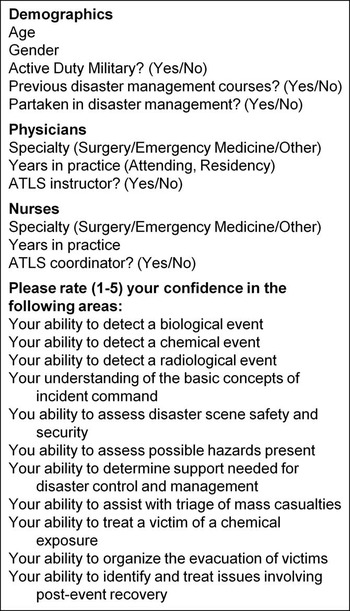
A self-assessment survey was developed by the authors who are BDLS faculty to measure the impact of the course on the participants’ confidence to manage specific disaster scenarios. 9 The self-assessment survey is based in part upon the work of Coule et al.,Reference Gist and Mitchell 10 enhanced with self-efficacy methodology; the survey was reviewed by two educational experts in this methodology. The questions were written to match the language used in the BDLS course and the survey was administered immediately after the BDLS course to minimize situational bias. Each question asked participants to rate confidence in managing certain events before and after the course, all of which were covered in the course curriculum. Confidence was measured in each of 11 BDLS topics and was based upon a five-point LikertReference Coule, Schwartz, Swienton, Olson, Hargreaves and Schieve 11 scale, with five being extremely confident and one being not at all confident (Figure 1). All participants in the BDLS course took the survey. Results were compiled, including means with 95% confidence intervals (CI) and medians with interquartile range (IQR). Differences between pre- and post-course confidence were calculated as the difference between the two mean values. Individual groups tested included occupational (physician, nurse, or other), specialty (surgery, emergency medicine, and other), military experience, Advanced Trauma Life Support (ATLS) experience (instructor or coordinator), prior disaster course, prior disaster management experience, age (<40 years), and job experience (<10 years). Statistical analysis was conducted with STATA Version 11.2 (StataCorp; College Station, Texas USA). Student’s t-test was used for analysis with P<.05 being significant. The Institutional Review Board at the University of Nevada School of Medicine granted a waiver of review for this research project.

Figure 1 Survey Administered to Basic Disaster Life Support (BDLS) Course Participants. Note: Demographic information was collected, and survey questions were asked based on a 5-point Likert scale, with 5=extremely confident and 1=not at all confident. Participants were asked to rate confidence before and after the course. Abbreviations: ATLS, Advanced Trauma Life Support; BDLS, Basic Disaster Life Support.
Results
Of 163 health care professionals taking BDLS, 162 completed the surveys which comprised the study cohort. This group included 78 physicians, 70 nurses, and 14 other health care workers. Internal consistency of the survey instrument was verified with Cronbach’s alpha test, which was measured at 0.934 for the confidence measurement survey.
Participant demographics are summarized in Table 1. Average age was 39 years with a slight female majority (M:F 45% to 55%). Physicians were mostly male (77%) while nurses mostly female (93%) and even gender distribution for other health care professionals. Fifty-five participants (34%) had military experience, 35 (22%) had previous experience in MCI training, while only 27 (17%) had previously taken disaster management courses. Advanced Trauma Life Support experience was surveyed in physicians and nurses: 26 physicians (33%) were ATLS instructors while 36 nurses (51%) were ATLS coordinators.
Table 1 Demographics, Specialties, and Experience of BDLS Participants

Abbreviations: ATLS, Advanced Trauma Life Support; BDLS, Basic Disaster Life Support.
Most physicians in the group were surgeons (44%) or emergency physicians (31%). The majority of physicians were attending level (74%) with an average of 12 years clinical attending experience, while resident trainees made up 18% with an average of 2.1 years of experience. Only six percent of the nurses surveyed worked in a surgical field while nearly one-half (47%) worked in emergency medicine; the remainder (43%) worked in other areas of nursing. Nurses had an average 15.6 years of work experience.
Participants reported an overall confidence improvement of 2.1 to 3.8 (P<.001) with a +1.7 increase in confidence. Figure 2 shows the confidence before and after the course for each subject area in the survey. Table 2 displays the mean confidence with 95% confidence intervals of all participants, and Table 3 displays the median confidence and interquartile range for each area surveyed before and after the course. Confidence increased in all measured areas (P<.001). Table 4 displays the net increase in confidence for each occupational group (physicians, nurses, and other). All occupational groups reported a significant confidence increase after completing BDLS (P<.001).
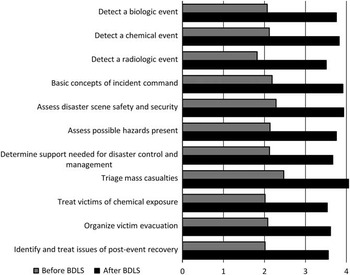
Figure 2 Summary of Self-Reported Confidence of BDLS Course Participants to Respond to Different Mass-Casualty Scenarios. Note: Significant increases in confidence were found in all areas (P<.001). Abbreviation: BDLS, Basic Disaster Life Support.
Table 2 Summary of Confidence Pre- and Post-BDLS Course

Note: Means and 95% CI shown. Statistically significant confidence increases were measured in each category surveyed (P<.001).
Abbreviation: BDLS, Basic Disaster Life Support.
a Highest value per category.
b Lowest value per category.
Table 3 Median and Interquartile Range (IQR) for Confidence in Each Area Tested

Table 4 Comparison of Demographic Factors in Mean Confidence Before, After, and Net Change from BDLS Course

Note: P<.05 was considered significant.
Abbreviations: ATLS, Advanced Trauma Life Support; BDLS, Basic Disaster Life Support; NS, Not Significant.
A summary of all survey responses is shown in Table 2. The group as a whole was most confident in their ability to triage mass casualties both before and after the course (2.5, 4.1) and least confident in their ability to detect a radiological event (1.8, 3.5). The greatest gain in confidence was seen on basic concepts of incident command (+1.7 points), while the smallest confidence gain was in the subject of chemical exposure (+1.5 points).
Physicians were most confident in their ability to triage mass casualties both before and after BDLS (2.7, 4.2). Pre-course physicians were least confident in detecting a radiological event (1.9), but after the course, they were least confident in their ability to identify and treat issues involving post-event recovery (3.5). Physicians had the greatest confidence increase in their ability to detect a chemical event (2.30 to 4.00; +1.7 points), while the least increase was in organizing the evacuation of victims (2.4 to 3.7; +1.3 points).
Nurses were most confident in their ability to triage mass casualties both before and after the course (2.2, 4.0). Pre-course, nurses were least confident in their ability to detect a radiological event (1.6), while post-course they were least confident in their ability to treat a victim of chemical exposure (3.4). The greatest confidence increase was in the basic concepts of incident command (1.9 to 3.7; +1.8), while the least increase was in ability to determine support needed for disaster control and management (1.9 to 3.5; +1.6).
Other health care workers were most confident in their ability to assess disaster scene safety and security prior to the BDLS course (2.6), while afterward, they were most confident in understanding the basic concepts of incident command (4.1). Before the course, they were least confident in two areas: ability to determine support needed for disaster control and management; and organize the evacuation of victims (2.1). After the course, they were least confident in their ability treat a victim of chemical exposure (3.4). The greatest confidence increase was in two areas: ability to detect a radiological event; and understanding the basic concepts of incident command (+1.6 points). The smallest increase was seen in their ability to treat a victim of a chemical exposure (2.2 to 3.4; +1.2).
A comparison of other demographic variables is displayed in Table 4. Physicians had significantly higher confidence levels both before and after the course, while nurses had significantly less confidence both before and after BDLS. These trends are visually displayed in Figure 3. Nurses also had significantly greater confidence increase compared with the rest of the participants. Physicians and nurses who listed either surgery or emergency medicine showed no difference before, after, or change from the course.

Figure 3 Net Change in Confidence of Physicians, Nurses, and Other Health Care Personnel. Note:All occupational groups reported confidence increase in each area surveyed (P<.001).
Participants with military experience reported less confidence before the course but showed a greater confidence increase. Post-course confidence was equivalent between military and civilian. Advanced Trauma Life Support experience did not significantly impact pre- and post-course confidence, but participants with ATLS experience reported greater confidence increases.
Previous disaster experience significantly increased pre-course confidence, both in participants with previous course training and real-world experience. Consequently, net confidence increases were less than with participants without disaster experience. Work experience >10 years or age>40 years did not affect confidence. Thus, older or more experienced participants did not report confidence increases in any category.
Discussion
If current trends continue, MCIs will continue to increase throughout the world in both frequency and severity.Reference Likert 12 , 13 The United States has made advances in disaster preparedness by developing the NDLS, of which over 100,000 health care workers and first responders have participated.Reference Guha-Sapir and Hoyois 14 The effectiveness of disaster preparedness training is difficult to measure. Disasters cannot be predicted or replicated, and disasters of similar type contain mitigating factors which may alleviate or exacerbate their destructive capacity. Furthermore, it is impossible to replicate disasters for comparative purposes. Mass-casualty incidents in Thailand have increased in number, while casualties have decreased during the same period. This is most likely a result of a better overall health care, Emergency Medical Services (EMS), and a disaster preparedness system. 15
Mass-casualty incidents often necessitate a large emergency response, and there is typically substantial variability in the background, training, and experience of the first responders. Disaster preparedness plans should include the possibility that responders of different backgrounds will respond to the same incident. Such a plan should address challenges of establishing leadership and creating synergy between different groups. These may include prehospital and in-hospital personnel; civilian and military; public health and public safety agencies; medical and non-medical responders; and local, state, and federal personnel. If the concept of educating a diverse group of people was not daunting enough, when different groups have different types of disaster response training, it can lead to a chaotic MCI response. The creation of a standardized plan with clear, common goals facilitates an environment where unacquainted individuals can cooperate and work as a team, while assuming their appropriate roles in the response to an MCI. These are the hurdles which the NDLS educational program helps to overcome.
This work describes the effectiveness of administering BDLS to a group of health care practitioners in Thailand, demonstrates their ability to successfully complete the course, and shows their confidence improvement in preparing for a MCI. Preparedness at the local level is of particular importance, as discussed in a thorough analysis of the 2004 Tsunami.Reference Angthong, Kumjomkijjakam, Pangma and Khorram-Manesh 16 Preparation for MCIs is most effective by preparing local medical volunteers to face the crisis, with international support aiding and accountable to the local providers. Very few countries are capable of facing such a large-scale disaster with strictly domestic resources, so neighboring countries are best suited to provide additional support to the affected country or region. However, foreign medical teams rarely arrive in time to help in the acute setting, and are often unfamiliar with the local language, customs, and health concerns. Thus, administering BDLS to local health care practitioners can have significant impact on disaster preparedness.
The EMS system in Thailand at the time of this training involved largely hospital-owned EMS as well as EMS operated by local public agencies and varied throughout the country. The majority of patients arriving at emergency rooms in Thailand arrived by non-EMS transport at the time BDLS was administered. Doctors and nurses in this group had the greatest confidence in triaging victims, both before and after the course, while other providers felt greatest comfort with incident command and triaging victims. These areas of confidence likely reflect each specialty’s inherent strengths and weaknesses. Detection of radiologic events was the area of least confidence, likely due to the lack of any recent radiologic events in Thailand. Thailand has never experienced a nuclear attack, and currently has no operating nuclear facilities, although the government is pursuing the possibility of nuclear energy in the future.Reference De Ville de Goyet 17 Physicians had the greatest confidence increase in detection of chemical events, while nurses and other providers received the greatest confidence boost in incident command. The course both enhances what participants are already comfortable with, while strengthening areas of weakness.
This group of BDLS participants included physicians, nurses, and first responders. Although all occupations reported confidence improvement in each area, nurses had the greatest confidence increases. Military personnel had lower pre-course confidence and had greater confidence gains than the remainder of the group. Thus, nurses and military personnel seemed to benefit the most from the course. Although nurses were not the majority in this group, they comprise the overwhelming majority of health care workers in Thailand, numbering over 138,000 nurses compared with 26,000 physicians.Reference De Ville de Goyet 17 The Royal Thai Armed Forces number over 300,000 active and an additional 245,000 reserve personnel.Reference Ruwitch 18 Due to the strong increase in confidence in these groups, and the large population of both nurses and military in Thailand, focusing on these populations for BDLS training would likely be very effective in preparing for a MCI. Adequate training of a large quantity of local providers who can render immediate aid in a disaster is the best preparation to respond to a mass-casualty or disaster situation.
Limitations
The limitations in this work are inherent to survey studies, which may lead to cognitive biases in the participants. A response bias may be present in the survey subjects, as they were surveyed immediately following the course and may have been more inclined to respond in the affirmative. Furthermore, participants were surveyed immediately before and after the course, which is effective for measuring the increase in confidence, but cannot determine how well the knowledge is maintained in the long term. These limitations will be addressed by further work in the area of MCI preparedness.
Conclusion
This study shows that BDLS significantly improves self-assessed confidence of health care providers to respond to MCIs in Thailand with more effectiveness and efficiency. Nurses and military personnel seem to acquire the greatest confidence benefit from participating in BDLS, and preparation should focus on these groups to prepare for future disasters.
Acknowledgements
The authors would like to thank Christopher L. Heath, EMT-P from the Medical College of Georgia for his assistance in conducting the NDLS program; Donald A. Risucci, PhD and Gwen S. Shonkwiler, PhD for their assistance in the survey design; and John J. Fildes, MD for administrative support of this project.
Supplementary Material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1049023X17006550