Trauma readiness is a prerequisite for adequate strategic planning in the health-care setting. The unpredictable nature of trauma poses a challenge to hospital staffing models because admissions rarely occur in uniform, predictable patterns during any given day. Reference Vaziri, Roland and Robinson1 Hospital personnel must also be prepared to respond to an array of natural and man-made disasters, which are also unpredictable, and that may include numerous trauma victims simultaneously. Reference Ogedegbe, Nyirenda and Delmoro2 Mass casualty incidents (MCIs) may create a large number of victims with the potential to overwhelm the capabilities, resources, and capacity of personnel within the context of the emergency response system. Reference Shartar, Moore and Wood3,Reference Schenk, Wijetunge and Mann4 These events pose a perpetual threat that may just as readily be equated to the summative impact of multiple simultaneous trauma victims.
Accounts of disaster preparedness within the literature tend to focus primarily on evaluating willingness to respond, Reference Ogedegbe, Nyirenda and Delmoro2,Reference Merrill, Orr and Chen5–Reference Burke, Goodhue and Chokshi8 assessment of readiness, Reference Ogedegbe, Nyirenda and Delmoro2,Reference Merrill, Orr and Chen5,Reference Fattah, Krüger and Andersen9,Reference Corrigan and Samrasinghe10 and prehospital and emergency department coordination strategies. Reference Shartar, Moore and Wood3,Reference Corrigan and Samrasinghe10–Reference Dal Ponte, Dornelles and Arquilla12 Perceptions regarding institutional and personal preparedness readiness, nevertheless, have been somewhat scant. Reference Ogedegbe, Nyirenda and Delmoro2,Reference Merrill, Orr and Chen5,Reference Fattah, Krüger and Andersen9,Reference Corrigan and Samrasinghe10 Educational initiatives and disaster simulations are commonly used strategies to prepare individual workers for disaster response. Hospital disaster plans and triage strategies have become an accepted means of curating disaster response at the institutional level. Reference Shartar, Moore and Wood3,Reference Corrigan and Samrasinghe10–Reference Dal Ponte, Dornelles and Arquilla12 Research specific to the volume of hospital personnel necessary for adequate response for trauma patient(s), however, is lacking. Understanding the administrative structure of hospital personnel may have implications in staffing ratios, liability exposure, clinical and personal exposures in the emergency setting, and even in the estimation of administrative bloat. We sought to quantify the number and type of hospital personnel involved directly or indirectly in the care and management of a critically ill Priority 1 trauma patient from arrival in the emergency department (ED) through the first 12 h of care or until patient demise. We hypothesized that the care and management of Priority 1 trauma patients involves the coordination of a complex array of health-care professionals and auxiliary staff in both direct and indirect roles. We further hypothesized that the majority of hospital personnel involvement first occurs in the ED.
Methods
Inclusion and Exclusion Criteria
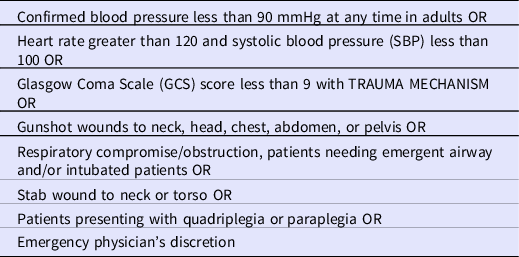
We included patients ≥ 18-y-old who met criteria for Priority 1 trauma status. The characteristics that define a Priority 1 trauma at West Virginia University Medicine are illustrated in Table 1, each of which aligns with standard national definitions. We also excluded pregnant patients in attempt to solely assess hospital personnel involved in adult trauma care rather than those who may additionally be involved in caring for vulnerable populations. All hospital personnel who participated either directly or indirectly in caring for the patient were included without any exclusion criteria in attempt to capture a comprehensive understanding of each person who may be involved in a trauma scenario.
Table 1. Criteria for Priority 1 activation response at West Virginia University J.W. Ruby Memorial Hospital, a Level 1 trauma center
Direct Data Collection
In this observational descriptive study, data were collected prospectively between May 2019 and January 2020 at our Level 1 trauma and quaternary care center, J.W. Ruby Memorial Hospital. We included all staff members who rendered care to the trauma patient, participating either directly or indirectly. Researchers (K.W., W.L., M.P., R.B., K.N.) were summoned to each case using a Priority 1 trauma page emitted when an admitted patient met inclusion criteria. This study does not catalog all Priority 1 trauma patients at the Level 1 trauma center during this period, but rather researchers collected data as time allowed with their personal and professional schedules. J.W. Ruby Memorial Hospital has cared for 10,481 adult trauma patients from 2016 to 2020, with 18.3% categorized as Priority 1. Data were collected starting at the time of patient arrival in the ED and continued for 12 h thereafter or until patient demise. Staff role, designation type, and the number of staff members were each recorded by the hour denoting the clinical setting for each first interaction. We avoided duplication in the counting of personnel more than once during the study period. Each was counted at the time of first interaction with the patient. For example, a trauma surgeon encountering the patient upon arrival to the ED may have also operated on the patient, in addition to providing care on rounds in the intensive care unit. Despite multiple encounters, though, the specified trauma surgeon was counted only once in the total at the time of first interaction, in this example, in the ED during hour 1. The West Virginia University Institutional Review Board approved the study, and informed consent from the patient and hospital personnel was deemed unnecessary given that all data were deidentified and obtained in an emergent manner (protocol 1902469296). This study complies with the STROBE guidelines.
Offsite Data Collection
Following the 12-h study period (or patient demise), researchers determined the number of participating radiologists and radiology resident and fellow physicians by performing a tally of the number of individuals who signed each image report. Laboratory and blood bank personnel involved indirectly in the care of the patient each hour were quantified by reviewing the laboratory information system. These totals were then added to produce a finalized personnel count. We initially sought to achieve a sample population with a precision of ±5. However, in view of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic, data collection was halted in response to the rising number of patients with influenza-like illnesses at the start of the pandemic. This proffered minimal loss in statistical integrity and achieved a precision of ±7. This adjustment was also a deliberate measure to minimize exposure, optimize safety of research personnel and to preserve personal protective equipment (PPE) for essential staff.
Statistical Analysis
Patients were assigned to 4 different Injury Severity Score (ISS) categories for analysis based on total score following the standards used by the American College of Surgeons. Score classifications include the following with increasing ISS indicating increased risk of death: 1-8 minor, 9-15 moderate, 16-24 severe, and >25 very severe. Reference Stevenson, Segui-Gomez and Lescohier13 We generated descriptive statistics to demonstrate frequencies and percentages for categorical variables and median and interquartile ranges (IQR) for continuous variables. We used boxplots to display the proportion of personnel over time. Differences between categorical variables were assessed using chi-squared tests, and differences between continuous variables were assessed using Wilcoxon rank sum tests. All statistics were performed using SAS v 9.4 (SAS, Cary, NC).
Results
We followed a total of 24 patients through their respective admissions and quantified the volume of hospital personnel involved in care and management of trauma patients. The median patient age was 50 y (IQR 35.5-67.5), multiple mechanisms of injury were represented (ie, blunt vs penetrating), and the patient population was predominantly male (n = 19; 79.2%). The ISS category breakdown for these patients was 11 very severe, 4 severe, 5 moderate, and 4 minor. Reference Stevenson, Segui-Gomez and Lescohier13 There were 2 mortalities (8.3%), 1 secondary to blunt trauma from an unknown object and the other secondary to a fatal gunshot wound. The majority of admissions occurred on a weekday (defined as Monday-Friday, n = 20; 83.3%) and during the day shift (defined as 07:00-19:00, n = 15; 62.5%) (Table 2). The average hospital personnel per patient was 79.71 (standard deviation, 17.62; mean standard error 3.6) with a median of 77.5 (IQR, 65.0-93.0) (Table 3). A median of 51.2% (IQR 43.4%-59.8%) of the total number of hospital personnel delivering care over the 12-h period were first involved within hour 1 (Figure 1). By hour 8, a median of 92.5% (IQR 82.8%-96.8%) of the total number of hospital personnel had already rendered care or tended to the patient in some manner. Of note, radiologist data pertaining to patient number 2 were not obtained during data collection; therefore, an average based on the other patients in the study was extrapolated for data analysis.
Table 2. Descriptive table of patient and admission characteristics

Table 3. Descriptive table of hospital personnel characteristics

a Advanced practice registered nurses, physician assistants, and certified registered nurse anesthetists.
b Center for Organ Recovery and Education coordinators, care managers, clinical care coordinators, and nurse coordinators.
c Resident physicians, fellow physicians, pharmacy residents, oral and maxillofacial surgery residents, and oral and maxillofacial surgery fellows.
d Radiologic technologists, computed tomography technicians, emergency department technicians, electrocardiogram technicians, nuclear medicine technicians, surgical technicians, invasive cardiovascular technologists, magnetic resonance imaging technicians, pharmacy technicians, anesthesia technicians, neurodiagnostic technologists, medical technicians, and electroencephalogram technicians.
e Nursing students, medical students, pharmacy students, pharmacy interns, radiologic technologist students, respiratory therapy students, and advanced practice registered nursing students.
f Clinical associates, certified nursing assistants, patient care assistants, laboratory assistants, computed tomography technician assistants, and radiologic technician assistants.
g Special forces medics and oral and maxillofacial surgery attendings.
h Housekeeping assistants, chaplains, security officers, transportation associates, unit clerks, outreach coordinators, surgical schedulers, scribes, sales representatives, concierges, registrations specialists, patient specialists, nutrition care associates, support service assistants, and supply chain associates.
i Advanced practice registered nurses, physician assistants, certified registered nurse anesthetists, respiratory therapists (except those analyzing ABGs), nurses, Center for Organ Recovery and Education coordinators, attending physicians (except radiologists), resident physicians (except radiology), fellow physicians, oral and maxillofacial surgery residents, oral and maxillofacial surgery fellows, radiologic technologists, computed tomography technicians, emergency department technicians, electrocardiogram technicians, nuclear medicine technicians, surgical technicians, invasive cardiovascular technologists, magnetic resonance imaging technicians, anesthesia technicians, neurodiagnostic technologists, electroencephalogram technicians, respiratory therapy students, advanced practice registered nursing students, radiologic technologist students, nursing students, medical students, computed tomography technician assistants, radiologic technologist assistants, clinical associates, certified nursing assistants, patient care assistants, special forces medics and oral and maxillofacial surgery attendings.
j Auxiliary staff H, pharmacists, pharmacy technicians, radiology residents, radiologists, laboratory assistants, medical technicians, respiratory therapists analyzing ABGs, clinical preceptors, anesthesia technicians, pharmacy residents, pharmacy interns, pharmacy students, clinical care coordinators, care managers, and nurse coordinators.
k Physicians, nurses, advanced practice providers A, respiratory therapists, coordinators B, trainees C, technicians D, students E, assistants F, pharmacists, and other G.

Figure 1. Proportion of hospital personnel who first encountered patient cumulatively per hour. Boxes represent IQRs, bold line represents median value, tails represent the minimum and maximum values, and open circles represent outliers.
We delineated job descriptions and stratified these by the direct provision of patient care versus indirect support as typically provided offsite or not requiring actual patient contact (eg, laboratory assistants) (Figure 2). Technicians (radiologic, computed tomography, ED, electrocardiogram, nuclear medicine, surgical, invasive cardiovascular, magnetic resonance imaging, pharmacy, anesthesia, neurodiagnostic, medical, and electroencephalogram) accounted for the largest number of personnel (median, 20.0 [IQR, 15.5-22.5]). A greater number of hospital personnel was involved in direct care (median, 54.5 [IQR, 47.5-67.0] versus 25 [IQR, 22.0-30.5]; P < 0.0001). The median number of health-care professionals (as compared to auxiliary staff) involved with Priority 1 trauma care was 74.5 (IQR, 63.5-90.5). When comparing hospital location of first interaction (Figure 3), a greater number of hospital personnel first rendered care to the patient outside of the ED (in radiologic services, perioperative care, clinical floors [wards, step down units, and intensive care units], blood bank, and laboratory) (median, 53.0 [IQR, 41.5-63.0]) compared with in the ED (median, 27.5 [IQR, 24.0-30.0]) when looking over the full 12-h period, or until demise if within that period (P < 0.0001). The same median number of personnel first rendered care to the patient in the ED (median, 27.5 [IQR, 24.0-30.0]) and the clinical floors (median, 27.5 [IQR, 20.0-31.5]).

Figure 2. Median health-care professionals and auxiliary staff stratified by direct and indirect patient interaction. A, advanced practice registered nurses, physician assistants, and certified registered nurse anesthetists. B, Center for Organ Recovery and Education coordinators, care managers, clinical care coordinators, nurse coordinators. C, resident physicians, fellow physicians, pharmacy residents/interns, oral and maxillofacial surgery residents, and oral and maxillofacial surgery fellows. D, radiologic technologists, computed tomography technicians, emergency department technicians, electrocardiogram technicians, nuclear medicine technicians, surgical technicians, invasive cardiovascular technologists, magnetic resonance imaging technicians, pharmacy technicians, anesthesia technicians, neurodiagnostic technologists, medical technicians, and electroencephalogram technicians. E, nursing students, medical students, pharmacy students, pharmacy interns, radiologic technologist students, respiratory therapy students, and advanced practice registered nursing students. F, clinical associates, certified nursing assistants, patient care assistants, laboratory assistants, computed tomography technician assistants, and radiologic technologist assistants. G, special forces medics and oral and maxillofacial surgery attendings. H, housekeeping assistants, chaplains, security officers, transportation associates, unit clerks, outreach coordinators, surgical schedulers, scribes, sales representatives, concierges, registrations specialists, patient specialists, nutrition care associates, support service assistants, supply chain associates, and support associates. Indirect Patient Interaction: auxiliary staff H, pharmacists, pharmacy technicians, radiology residents, radiologists, laboratory assistants, medical technicians, respiratory therapists analyzing arterial blood gases (ABGs), clinical preceptors, anesthesia technicians, pharmacy residents, pharmacy interns, pharmacy students, clinical care coordinators, care managers, and nurse coordinators. Direct Patient Interaction: advanced practice registered nurses, physician assistants, certified registered nurse anesthetists, respiratory therapists (except those analyzing ABGs), nurses, Center for Organ Recovery and Education coordinators, attending physicians (except radiologists), resident physicians (except radiology), fellow physicians, oral and maxillofacial surgery residents, oral and maxillofacial surgery fellows, radiologic technologists, computed tomography technicians, emergency department technicians, electrocardiogram technicians, nuclear medicine technicians, surgical technicians, invasive cardiovascular technologists, magnetic resonance imaging technicians, anesthesia technicians, neurodiagnostic technologists, electroencephalogram technicians, respiratory therapy students, advanced practice registered nursing students, radiologic technologist students, nursing students, medical students, computed tomography technician assistants, radiologic technologist assistants, clinical associates, certified nursing assistants, patient care assistants, special forces medics and oral and maxillofacial surgery attendings.

Figure 3. Median hospital personnel involved in patient care or management by location of personnel when first interaction occurred. L = wards, step down units and intensive care units.
Patients classified as having an alternative mechanism of injury (ie, explosive) were cared for by a significantly higher median number of hospital personnel on the clinical floors (median, 42.0 [IQR 42.0-46.0]; P = 0.0330) and hospital personnel involved in direct patient care (median, 73.0 [IQR 59.0-75.0]; P = 0.0413). We stratified the results by patient sex, and observed that females had a significantly higher median number of total hospital personnel involved in their care compared with males (median, 102.0 [IQR 80.0-109.0] and 76.0 [IQR, 65.0-81.0], respectively; P = 0.0273). This was true in the rendering of direct care (median, 71.0 [IQR, 56.0-81.0] vs 50.0 [IQR, 47.0-59.0], respectively; P = 0.0297), blood bank/phlebotomy (median, 2.0 [IQR, 1.0-3.0] vs 1.0 [IQR 1.0-1.0], respectively; P = 0.0416), nursing staff (median, 21.0 [IQR, 21.0-22.0] vs 17.0 [IQR, 13.0-18.0], respectively; P = 0.0043), and hospital personnel involved in perioperative care (median, 29.0 [IQR, 17.0-32.0] and 0.0 [IQR, 0.0-9.0], respectively; P = 0.010).
We observed no difference in total hospital personnel based on day of admission when comparing weekend and weekday admissions (P = 0.7270). This was true also of time of admission stratified as day shift (07:00-19:00) versus night shift (19:00-07:00) (P = 0.2098). However, we observed that patients admitted during night shift had significantly fewer assistants (ie, clinical associates, certified nursing assistants, patient care assistants, laboratory assistants, computed tomography technician assistants, and x-ray technician assistants) involved directly compared with the day shift (median, 3.0 [IQR, 3.0-3.0] and 4.0 [IQR, 3.0-6.0], respectively; P = 0.0305). This was reflected also in the number of students involved directly (median, 1.0 [IQR, 1.0-2.0] and 4.0 [IQR, 1.0-4.0], respectively; P = 0.0237), as well as respiratory therapists involved indirectly in patient care (median, 1.0 [IQR, 1.0-2.0] and 2.0 [IQR, 1.0-2.0], respectively; P = 0.0393).
We observed no difference in ISS based on sex or age (P = 0.6579 and P = 0.6087, respectively). Total median hospital personnel was not statistically different based on ISS (very severe median, 79.0 [IQR 76.0-100.0]; severe median, 78.5 [IQR 67.5-94.5]; moderate median, 81.0 [IQR 70.0-81.0]; minor median, 60.5 [IQR 53.5-70.5]; P = 0.1266). Only the number of trainees (defined as resident physicians, fellow physicians, pharmacy residents, oral and maxillofacial surgery (OMFS) residents, and OMFS fellows) involved was significantly different by ISS (P = 0.0433). All other personnel categories, including both direct and indirect patient care, were not significantly different based upon ISS (all P > 0.05).
Discussion
Our research demonstrates that a complex array of hospital personnel is involved directly and indirectly in the care of Priority 1 trauma patients. The majority of these provide care during the initial hours of admission. The hospital personnel vary by job type and include both health-care professionals and auxiliary staff. The staffing of EDs and hospitals represents a substantial logistical challenge. Schedules must accommodate daily fluctuations and unpredictable presentations of trauma patients and MCIs. Reference Vaziri, Roland and Robinson1 Indeed, intricate mathematical and computer models are used often to assist with staffing strategies. Michelson et al. used computer modeling to study infrastructural constraints in an academic pediatric ED and determined that the ED had space limitations 5.0% of the time, physician limitations 0.1% of the time, and nurse limitations 16.1% of the time. Patients that presented during these limited times also had significantly longer lengths of stay compared with nonlimited presentation time. Reference Michelson, Stack and Bachur14 Tucker et al. used queuing theory to determine if activating an overnight backup operating room was necessary at a Level 2 trauma center, defined as a center that may initiate but not necessarily provide exhaustive care of all injured patients. The backup operating room was ultimately deemed unnecessary based on the discovery that the probability of 2 or more surgical cases occurring simultaneously overnight was less than 0.1%. Furthermore, the authors identified queuing theory as a useful tool in assessing staffing needs. Reference Tucker, Barone and Cecere15
Despite these models, research has not comprehensively quantified the number or categorized the type of personnel involved directly and indirectly in the management of a Priority 1 trauma patient. The simultaneous demand for personnel within the ED, nevertheless, is a more plausible eventuality. Although our data are not granular enough to evaluate the occurrence and magnitude of this coincident demand, it may theoretically be quantified by the adjudication of those presentations that pertained to patients who crossed a specific threshold of injury (ie, ISS of 15). When these admissions may have occurred within a few minutes of each other, they are likely to have competed for the same cadre of personnel or resources. There are thus numerous, unquantifiable opportunity costs that may affect patients based on the timing of presentation and the ongoing demands in the ED at any given time. These costs represent a complex matrix with the consideration that the higher the level of specialization, the greater the demand for those personnel and the greater the impact of the delay on the patient. The deployment of a hand surgeon performing reconstructive surgery, for example, would necessarily delay the definitive care rendered to the next patient presenting with a similar hand injury a few minutes later than the first patient.
Disaster preparedness research has historically focused on willingness to respond, Reference Ogedegbe, Nyirenda and Delmoro2,Reference Merrill, Orr and Chen5–Reference Burke, Goodhue and Chokshi8 assessment of readiness, Reference Ogedegbe, Nyirenda and Delmoro2,Reference Merrill, Orr and Chen5,Reference Fattah, Krüger and Andersen9,Reference Corrigan and Samrasinghe10 and prehospital and ED coordination strategies. Reference Shartar, Moore and Wood3,Reference Corrigan and Samrasinghe10–Reference Dal Ponte, Dornelles and Arquilla12 An estimated 34-93% of health-care workers are willing to respond in an emergency. Reference Ogedegbe, Nyirenda and Delmoro2,Reference Merrill, Orr and Chen5,Reference Dovgalyuk, Brady and Sidebottom6,Reference Burke, Goodhue and Chokshi8 Common barriers include childcare, pet care, eldercare, transportation, and commuting distance. Increasing age, by contrast, is deemed to facilitate response. Reference Ogedegbe, Nyirenda and Delmoro2,Reference Qureshi, Gershon and Sherman7,Reference Burke, Goodhue and Chokshi8 Surge capacity protocols help to determine the number of patients that may be managed without compromise to care. Reference Shartar, Moore and Wood3 Our study provides an alternate point of view by the provision of numerical evidence on which these protocols and other staffing policies may be based. This is relevant because shortage of responders is common in MCIs. Following an MCI in Brazil, Dal Ponte et al. reported “the number of capable first responders and available rescue supplies was insufficient to cater to the number of victims in need.” Reference Dal Ponte, Dornelles and Arquilla12 Therefore, a growing necessity exists for more published data to delineate staffing requirements beyond the assessment of willingness and barriers to response. Thus, the quantification of personnel needed to drive preparedness planning is important to mitigate inadequate responses to such disasters.
Our data indicate that nearly 80 individuals are involved in Priority 1 trauma response with a wide array of job descriptions ranging from laboratory assistants to security officers and including both direct and indirect patient encounters. The number of hospital personnel did not differ significantly by ISS and even the traumas classified as minor based on ISS had a median of nearly 61 hospital personnel involved. The largest overall resource use occurred within the first hour, during which approximately half of first contacts occurred. Nearly all first contacts occurred by hour 8. This indicates a front-loading of care but does not downplay the number of personnel required subsequently during that same encounter. Several people continue to care for the patient numerous times and even continuously throughout the study period. It is also important to note that multiple of the same personnel type commonly work together to perform certain aspects of trauma care (eg, multiple nurses transferring patient from gurney to bed, etc.); this may explain any perceived redundancy in personnel counts. Overall, these data demonstrate the complex array of diverse personnel involved and help to define the number and types of personnel required.
The disaster preparedness and trauma literature base, to our knowledge, offers little by way of quantification of personnel involved in trauma response by hospital location. Our findings may inform daily trauma care and can be extrapolated to disaster preparedness. We observed that numerous hospital personnel first cared and continued to care for patients in perioperative care areas, clinical floors, the blood bank, the laboratory, and radiologic services as well as the ED. In fact, our study revealed, in opposition to our hypothesis, that more personnel first cared for the patient outside of the ED. Furthermore, the ED and clinical floors totaled the same median number of personnel. Although the median number of hospital personnel for perioperative care was 0, the mean was nearly 9. This difference in statistical measurements likely occurred because only 9 of the 24 patients required operative management and, as previously described, many hospital personnel cared for the patients in multiple clinical settings with the data only accounting for first contact site. Accounting for hospital personnel at each clinical location in which care was provided rather than only the site of first interaction would lead to an even larger number of personnel caring for patients in areas such as the clinical floors, etc. As such, Priority 1 trauma care is robust and requires a large volume of personnel beyond the ED. Patients cannot be effectively transitioned out of the ED for new arrivals if staffing is not sufficient in other clinical settings. Therefore, our data provide guidance for planning for initial and continued care of trauma and disaster related patients hospital-wide. Our results offer a quantitative analysis upon which trauma staffing and preparedness planning can be derived.
Trauma research on sex differences has primarily focused on outcome differences and has yielded contradictory results. Age, ISS, non-Caucasian race, revised trauma score, blunt injury type, and certain preexisting conditions have each been shown to be independent predictors of trauma mortality. Reference Gannon, Napolitano and Pasquale16 However, the same study showed no significant difference in mortality by sex. Reference Gannon, Napolitano and Pasquale16 Our study showed that females had higher median total hospital personnel and personnel involved in perioperative care than males. ISS did not significantly differ by sex alone, so the difference in personnel numbers is less likely related to injury severity. However, only 5 of the 24 patients followed were female, so the patient profile might not be powered enough to accurately parse out the trends.
We observed no difference in total hospital personnel involved based on day or time of admission. This suggests that trauma response may be uniform regardless of the day of the week or hour of the day. This is intriguing given previous reports that a greater volume of trauma patients is admitted over the weekend and that a higher percentage of severely injured patients present overnight compared with daytime. Reference Carmody, Romero and Velmahos17 These findings suggest the need for, at a minimum, equal staffing overnight and on weekends as is seen in our data. There are conflicting data regarding outcomes based on time of admission. Our findings corroborate research that has demonstrated no difference in mortality or unfavorable outcomes based on admission day and time. One study showed no significant difference in death rate or rate of delayed laparotomy based on time of day or day of week. Reference Carr, Jenkins and Branas18 Arabi et al. reported intensive care units with onsite intensivist coverage do not demonstrate increase in negative outcomes (ICU and hospital mortality rate, ICU length of stay, mechanical ventilation duration, etc.) based on time of the day or day of the week. Reference Arabi, Alshimemeri and Taher19 In contrast, Egol et al. reported a higher adjusted mortality for overnight trauma admissions (18:00-06:00) compared with those during daytime admissions (06:00-18:00). Reference Egol, Tolisano and Spratt20 Similar findings have been noted regarding prolonged door-to-balloon time(s) for percutaneous coronary intervention during off hours (weekends and 17:00-07:00 on weekdays). Reference Magid, Wang and Herrin21 Our study does not address outcomes but instead focuses on the number of responders.
In this unprecedented SARS-CoV-2 pandemic, the literature has been inundated with discussion pertaining to availability, use, and preservation of PPE. Reference Bauchner, Fontanarosa and Livingston22–Reference Ranney, Griffeth and Jha24 As this is a novel coronavirus, decisions had initially been guided primarily by real-time anecdotal experience rather than robust research due to the short timeframe after virus detection. Our study has implications specific to the SARS-CoV-2 pandemic, an ongoing MCI in many hospitals globally. Priority 1 trauma patients arriving to the ED during this pandemic will often be classified as high-risk for carrying the virus as they frequently cannot provide any history and family is often initially unavailable to provide further information. We observed that nearly 55 hospital personnel directly participate in care for Priority 1 trauma patients within the first 12 h. This indicates a significant quantity of PPE may be required to care for just 1 trauma patient during the pandemic to optimize the safety of personnel involved in responding. Shortages have been and are occurring nationwide and globally, and our data reiterate the need to bolster PPE supplies and conservation efforts when possible. Moreover, the sheer number of personnel who may be involved may have policy implications for efficient Priority 1 trauma patient SARS-CoV-2 viral testing.
Our study has limitations. First, the data pertain to a single Level 1 trauma and quarternary care center, limiting extrapolation to smaller community-based facilities or dissimilar populations. Second, our trauma teams do not routinely downgrade trauma patients once they have arrived regardless of whether they end up being less severely injured than initially anticipated. This may have skewed the data without accounting for decreased clinical severity. Third, all participating hospital personnel were included in the total so as not to impart bias in attempting to determine who “contributed in a meaningful way.” This may have led to an overestimation of the number involved. Fourth, our methodology of counting personnel once even if they contributed to care in multiple settings may underestimate the need for certain personnel in terms of disaster planning for MCIs. We were also unable to quantify the impact of coincident demand resulting from simultaneous presentations. Finally, our sample size was small but still achieved a precision of ±7. Despite these limitations, our results provide important numerical data that have the potential to influence policies and procedures surrounding trauma care and disaster preparedness. It is the first of its kind and serves as a foundation on which future research can be built.
Conclusions
In summary, a paucity of data exists regarding the number and type of hospital personnel involved in the care of a Priority 1 trauma patient. In this study, we describe the significant impact of a Priority 1 trauma patient on hospital resources. This is particularly evident in both the number of hospital personnel involved within the first hour and in the overall array of personnel involved. These data are an important addition to current evidence-based literature that may guide day-to-day staffing assignments in preparation for Priority 1 trauma patients as well as in the refinement of current disaster preparedness policies in attempt to most adequately respond to MCIs.
Author Contributions
Kaitlin Woods: Participated in concept design, data collection, literature search, data interpretation, and manuscript writing. J.W. Awori Hayanga: Participated in concept design, data interpretation, and manuscript writing. Jeffrey Cannon: Participated in literature search, obtaining IRB approval, and manuscript editing. Wesley Lemons: Participated in data collection and manuscript editing. Michael Philips: Participated in data collection and manuscript editing. Ashley Schmidt: Participated in data collection and manuscript editing. Roosevelt Boh: Participated in data collection and manuscript editing. Kinza Noor: Participated in data collection and manuscript editing. Lisa Fornaresio: Participated in concept design, obtaining IRB approval, and manuscript editing. Dylan Thibault: Participated in data analysis and manuscript writing. PS Martin: Participated in concept design, data interpretation, and manuscript editing. Alison M. Wilson: Participated in concept design, data interpretation, and manuscript editing. Heather K. Hayanga: Participated in concept design, data interpretation, and manuscript writing.
Conflict of Interest
We have no conflicts of interest to declare.
Ethical Standards
Approval was obtained by the West Virginia University Institutional Review Board; informed consent from the patient and hospital personnel was deemed unnecessary given that all data were deidentified and obtained in an emergent manner.








