Introduction
Angioedema of the tongue can occur as an adverse effect of certain medications.
We present a case of an elderly man who had been taking perindopril for three months, and who presented with the acute onset of unilateral tongue angioedema following surgery.
Case report
A 71-year-old man was admitted for worsening subdural haemorrhage. He had a history of deep vein thrombosis of the left femoral and external iliac vein, and right temporal subdural haemorrhage secondary to warfarin therapy. He also had newly diagnosed hypertension, and had been taking oral perindopril (8 mg once daily) for three months. He reported experiencing itchiness after taking the perindopril tablets, but had not sought medical treatment and had continued this medication.
The surgeons performed a burr hole and evacuation of subdural haematoma under general anaesthesia.
The day after surgery, the patient developed the sudden onset of painless left tongue swelling. This rapidly worsened over 3 to 4 hours, causing difficulty in chewing. He had no dysphagia, odynophagia or breathing difficulty. There was no fever, and no history of foreign body ingestion or trauma to the tongue or neck. The patient's other medication included oral pantoprazole (40 mg once daily), and one dose of intravenous ceftriaxone (2 g) received for pre-operative prophylaxis.
On examination, the patient was comfortable breathing room air, with no stridor, no respiratory distress and stable vital signs. He had a ‘hot potato’ voice. There was non-pitting oedema of the left half of the tongue. The tongue had restricted protrusion (Figure 1). The floor of the mouth was also oedematous, and there was diffuse, painless left submandibular swelling. There was no evidence of peritonsillar abscess or tonsillitis, and no foreign body or fish bone was seen.
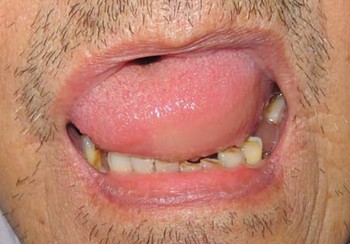
Fig. 1 Examination of the oral cavity revealed oedema of the left side of the tongue with restricted protrusion.
Flexible nasopharyngolaryngoscopy revealed oedema of the tongue on the left, extending to the vallecula and the lingual surface of the epiglottis (Figure 2). The larynx, supraglottis and arytenoids were normal. Both vocal folds were mobile, with a good airway.

Fig. 2 Endoscopic view of the laryngeal inlet showing oedema of the base of the tongue on the left (black arrow), extending to the vallecula and lingual surface of the epiglottis.
The patient's white cell count was normal.
The patient was treated with intravenous dexamethasone (8 mg immediately and thence thrice daily), and was kept under close observation for impending airway obstruction. His perindopril was discontinued. Four hours later, his tongue swelling had reduced significantly. By the following day, his voice had returned to normal and he was able to eat without difficulty. A reduced dose of dexamethasone (4 mg thrice daily) was given for another day, and the patient was then switched to oral prednisolone (20 mg once daily) for another 5 days. His tongue oedema subsided completely over the next 2 days.
Two weeks later, the patient was well with no residual tongue oedema. Flexible nasopharyngolaryngoscopy revealed normal oropharyngeal and laryngeal structures.
Discussion
Angiotensin-converting enzyme (ACE) inhibitors are one of the commonest drugs prescribed for hypertension and heart failure. They have been shown to reduce mortality and cardiac events in high risk patients, and also to reduce the degree of microalbuminuria in type two diabetes mellitus patients. Generally, ACE inhibitors are well tolerated. Their commonest side effects include cough and acute renal failure.
Angioedema is defined as self-limiting, localised swelling of the periorbital region, lips, tongue and occasionally the extremities and bowel wall. It occurs due to the release of vasoactive mediators and the resulting transient increase in the permeability of postcapillary venules in the subcutaneous or submucosal tissues. Causes of angioedema include: idiopathic recurrent angioedema; allergy (mediated by immunoglobulin E); hereditary forms (type one due to deficiency of C1 esterase inhibitor protein, type two due to dysfunctional C1 esterase inhibitor protein, and type three due to coagulation factor XII gene mutation associated with exogenous oestrogen administration (e.g. oral contraceptives and hormone replacement therapy)); acquired forms (type one associated with lymphoproliferative diseases, and type two autoimmune-mediated with production of anti-C1 esterase inhibitor protein antibodies); medication; physical factors (i.e. cold, heat, vibration, trauma, emotional stress and ultraviolet light); cytokine-associated angioedema syndrome (Gleich's syndrome); and thyroid autoimmune disease associated angioedema.Reference Temino and Peebles1
The reported incidence of angioedema secondary to ACE inhibitors ranges from 0.1 to 0.7 per cent.Reference Nazaneen, Ziad and Stanley2 Incidence is highest in the first month of ACE inhibitor usage, but angioedema can occur even after years of use.Reference Malde, Regalado and Greenberger3 Angioedema of the face, extremities, lips, tongue, glottis and/or pharynx, and gastrointestinal system have been reported in patients taking ACE inhibitors.
Unlike allergy-induced angioedema, in which histamine plays a major role, angioedema induced by ACE inhibitors is postulated to be secondary to increased levels of bradykinin. Angiotensin-converting enzyme, also known as kininase II, converts angiotensin I to angiotensin II, but also inactivates bradykinin. Angiotensin-converting enzyme inhibitors reduce bradykinin catabolism, thus increasing bradykinin level, and raising the risk of angioedema.Reference Cugno4
Angioedema involving the tongue, oral cavity or oropharynx usually occurs suddenly and progresses rapidly. Patients can present with acute upper airway obstruction and require resuscitation or urgent medical and surgical intervention. In our patient, rapid, progressive, non-pitting oedema of one side of the tongue suggested the diagnosis of angioedema, although the opposite side of the tongue remained normal. A rapid response to steroids confirmed the diagnosis. Apart from his history of ACE inhibitor usage, our patient had no other cause for angioedema (endotracheal tube intubation would be more of a precipitating factor than a cause).
A thorough English language literature search revealed only two previously reported cases of unilateral tongue angioedema secondary to ACE inhibitors. The first case involved a patient who had been taking enalapril for at least three years.Reference Mlynarek, Hagr and Kost5 The second case involved a patient who had been taking benazepril for several months.Reference Chan, Kalira and Hore6 Both patients presented to the emergency department with unilateral tongue swelling. No similar cases involving perindopril have been reported.
• A case is presented of an elderly man receiving perindopril treatment, who presented with angioedema of the left side of the tongue, floor of the mouth and upper neck
• Although angioedema generally occurs during the first few months of antiotensin-converting enzyme inhibitor use, its onset can be more delayed, even by years
• Angiotensin-converting enzyme inhibitor induced angioedema can be fatal if it involves the airway; early recognition can prevent unnecessary surgical intervention and complications
The treatment of angioedema depends on the site of the swelling.Reference Ishoo, Shah, Grillone, Stram and Fuleihan7 Lip and facial angioedema can be observed and treated medically. Antihistamines and glucocorticoids can reduce angioedema and improve symptoms during the acute episode.Reference Temino and Peebles1 Lingual and oropharyngeal angioedema need to be closely monitored for airway compromise, as oedema at these sites typically progresses rapidly. Patients with laryngeal angioedema may need early elective intubation, as intubation can be difficult if the oedema progresses. Occasionally, tracheostomy is needed.Reference Zirkle and Bhattacharyya8 Once the diagnosis of ACE inhibitor induced angioedema has been made, the causative medication needs to be stopped, and the patient should avoid all other ACE inhibitors.Reference Temino and Peebles1 Occasionally, patients who developed angioedema after taking ACE inhibitors can also develop angioedema secondary to angiotensin receptor blockers.Reference Haymore, Yoon, Mikita, Klote and DeZee9 Thus, it is best to avoid angiotensin receptor blockers in patients with a history of severe or life-threatening angioedema.




