Introduction
During intensity-modulated radiation therapy (IMRT), there is a possibility that critical organs might receive high doses if there is an error during immobilisation and patient set-up procedures, due to the high-dose gradient.Reference Contesini, Guberti and Saccani1 In addition, there is a possibility of dose calculation errors in the treatment planning system (TPS) which may not be accurate in the air cavity regions of the patient body. Therefore, there is a need to measure the dose delivered to the patient by in vivo dosimetry which enables us to quantify the dose that is received by the patient, detect the errors during treatment and verify whether the planned and the delivered doses are in agreement.Reference Engström, Haraldsson and Landberg2 However, the in vivo dosimeter used must be sensitive and accurate enough to detect the possible errors during the treatment.Reference Aznar, Andersen and Bøtter-Jensen3 Currently used dosimeters such as metal–oxide–semiconductor field-effect transistors (MOSFET), thermoluminescent dosimeters (TLD) and diodes have several disadvantages. MOSFETs show radiation damage and have finite lifetime.Reference Viamonte, da Rosa and Buckley4 TLDs are temperature dependent, labour intensive, highly sensitive to light, limited by one-time readout, susceptible to loss of signal due to fading, environmentally unstable and consume more time for annealing. Diodes show varying dose response at different temperatures and are highly energy dependent while their sensitivity varies with accumulated dose.Reference Essers and Mijnheer5–Reference Ferguson, Lambert and Harrison8
The introduction of the optically stimulated luminescence dosimeter (OSLD) with its unique advantages has brought in a new revolution in in vivo dosimetry. The OSLD is a new type of dosimeter which has made a key breakthrough in measuring low dose. Aluminium oxide doped with carbon (Al2O3:C), which is known as supersensitive thermo-luminescent material, was later used in luminescence dosimetry. Al2O3:C is one of the most widely used OSL materials in radiation dosimetry. OSLDs are temperature independent and allow multiple readouts in addition to a faster readout mechanism.Reference Jursinic9
In this study, the characterisation of OSLD properties, such as their sensitivity variation, reproducibility, dose-rate dependence, energy dependence, output factor measurement and comparison between two methods of bleaching, was analysed. The in vivo dose assessment involved the eye dose measurement, which was performed for 3 consecutive days for head and neck IMRT and the dose measured by OSLD was compared to that of the dose calculated by the TPS.
Theoretical Background
OSL is a phenomenon of stimulated light emission by a crystal that is irradiated and then it is exposed to a light of particular wavelength. Al2O3:C has its stimulation spectra at 540 nm green light and emission spectra at 420 nm blue light.Reference Jursinic9 The OSL signal is directly proportional to the absorbed dose. When the ionising radiation passes through the OSL material, it produces electron–hole pairs and the free electrons move towards the conduction band and are held by the pre-existing defects. At the same time, the holes get excited and are trapped in the luminescent centres. Thus, the electrons exist in a metastable state. When the dosimeter is illuminated with light of appropriate wavelength, the trapped electrons get excited to the conduction band and combine with the holes which are in the luminescent centres, resulting in the emission of light.
Materials and Methods
The Clinac 2100C/D linear accelerator (Varian Medical Systems, Palo Alto, USA), which could generate two photon energies of 6 and 15 MV and electron energies of 4, 6, 9, 12 and 15 MeV, was used in this study. It has tertiary multi-leaf collimators (MLC) with a maximum field size of 40 × 40 cm2. The MLC has 120 leaves of which the 40 pairs located at the centre have a width of 0·5 cm, while the remaining 20 pairs have a width of 1 cm at isocentre. This has the feature of dynamic MLC that is used to modulate the photon beams according to the shape of the tumour during treatment delivery. This enables the beam modulation during the mode of treatment delivery which is known as IMRT. The Eclipse™ TPS (v10.0; Varian Medical Systems, Palo Alto, USA) was used for the planning of all the IMRT cases included in this study. The linear accelerator also consists of kV on-board imager (OBI) with a cone beam computed tomography (CBCT) facility and an aS1000 flat-panel electronic portal imaging device (EPID).
Each nanoDot™ OSLD (Landauer, Glenwood, USA) consists of a single Al2O3:C crystal of 5 mm diameter and 0·9 mm thickness, with an effective atomic number of 11·28. This crystal is enclosed within an acrylonitrile butadiene styrene (ABS) plastic case of dimensions 1 × 1 × 0·3 cm3, as shown in Figure 1a and 1b. As Al2O3:C has stimulation and emission spectra at 532 nm green light and 420 nm blue light, respectively, the OSLD reader is designed such that an array of green light-emitting diodes is used for stimulation and the blue light emitted from the OSLD is filtered using a blue filter, as shown in Figure 2. The readout of OSLD was processed using the microStar reader (Landauer, Glenwood, USA), as shown in Figure 3. In-house made hemispherical build-up caps made of bee wax and having a thickness of 1·5 cm were used for in vivo measurement, as shown in Figure 4.

Figure 1a. Active material outside the plastic case.

Figure 1b. Back view of nanoDot OSLD.

Figure 2. Readout process inside OSLD reader.

Figure 3. MicroStar nanoDot™ OSLD reader.

Figure 4. In-house build-up cap made of bee wax.
Characteristic Study of OSLD
Sensitivity measurement
For the purpose of sensitivity measurement, the OSLDs were irradiated with 200 cGy at a depth of 1·5 cm and a field size setting of 20 × 20 cm2. A 10 cm of water-equivalent Perspex was used for backscatter, as shown in Figure 5. Inter-comparison factor (ICF) was calculated by taking the ratio between OSL signal of each OSLD and the average OSL signal of all the OSLDs. The ICF converts the variation of different OSLD sensitivities into an identical response. The measurements were carried out for three trials.
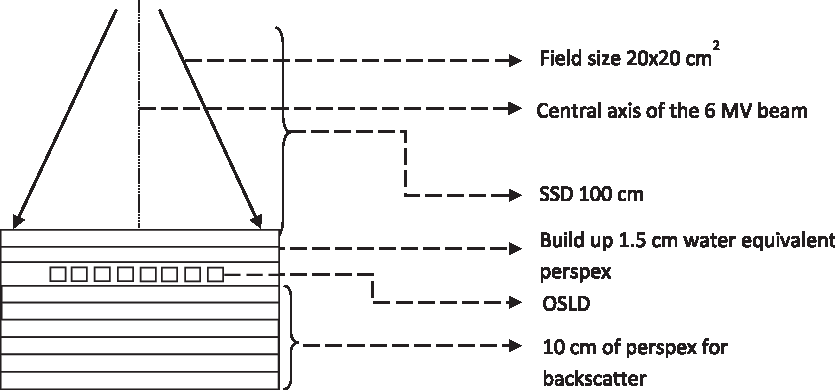
Figure 5. Setup diagram for sensitivity measurement of OSLD.
Reproducibility of OSLD
To investigate the reproducibility, five OSLDs were irradiated for 200 cGy at the depth of d max and the responses of the OSLDs were noted. This investigation was performed for three consecutive trials.
Output factors and beam quality dependence
OSLD response for field sizes of 5 × 5, 10 × 10, 15 × 15, 20 × 20 and 25 × 25 cm2 was measured with a constant monitor unit setting for each field size. The response of OSLDs for different beam energies such as 1·25 MeV (mean energy of Co60), 6 MV and 15 MV X-ray beams was measured by irradiating the OSLDs for a dose of 200 cGy at a depth of 5 cm with 10-cm-thick Perspex to account for backscatter.
Dose-rate dependence
The OSLD response for various dose rates, ranging from 100 to 600 MU/minute in steps of 100 MU/minute, was measured by irradiating three OSLDs for the same dose with a reference field size of 10 × 10 cm2.
Calibration of OSLD for 6 MV beam using linear accelerator
The OSLDs were irradiated to doses ranging from 5 to 400 cGy, at 1·5 cm depth in a Perspex phantom with sufficient thickness to extract maximum backscatter, and their response for different doses was plotted. The set-up for calibration is illustrated in Figure 6.

Figure 6. Calibration setup of OSLD in Clinac 2100C/D.
Bleaching of OSLD
Bleaching is a technique by which the residual traps are removed by exposing the OSLDs to visible light. Comparison between the two types of bleaching was carried out. Three OSLDs were chosen and were irradiated for 200 cGy at the depth of d max, and the OSL response was measured. The OSLDs were then bleached using a halogen source and the residual readings were noted. Similarly, the same OSLDs were once again irradiated for 200 cGy and bleached using compact fluorescent lamp (CFL), and the residual doses measured were noted for three successive trials. Comparison between these two methods of bleaching was established.
Halogen bleaching
In this technique, OSLD was bleached using a halogen source. As it produces more heat, the OSLDs were kept at a distance of 15 cm away from the source, as shown in Figure 7. The time set for bleaching was 15 minutes.

Figure 7. Bleaching of OSLD using halogen bulb (150 W).
CFL bleaching
The OSLDs were bleached using a CFL source that could be placed at a distance of 3 cm from the light source (as shown in Figure 8) due to the lower heating effect. The time set for bleaching was 15 minutes.

Figure 8. Bleaching of OSLD using CFL bulb (15 W).
In vivo dose measurement
The in vivo measurement involved the eye dose verification for five head and neck IMRT patients with mean age and SD of 29·6 ± 3·206 years. The coordinates corresponding to the OSLD measurement points on the eye were initially noted from the CT images and marked on the patient by applying the shifts from the CT. The reason for applying the CT shift is to account for positional accuracy because these measurements were performed on 3 consecutive days, and the dose measured by the OSLDs was compared to that of the dose calculated by the TPS. Each OSLD was placed on the patient with a water-equivalent wax bolus of 1·5 cm, which was used as a build-up to maintain the electronic equilibrium and to reduce the fluctuation.Reference Jursinic and Yahnke10
Results
Sensitivity of OSLD
In this study, 50 OSLDs were irradiated with 200 cGy. A graph was plotted between dosimeter number and the normalised OSL signal. The maximum percentage deviation in sensitivity was found to be within ±5% when irradiated with a dose of 200 cGy. The ICF for each OSLD was calculated using Equation (1). These sensitivity variations were corrected by means of applying the ICF, as shown in Figure 9.
where M s is the measured OSL signal of a single dosimeter and M a is the average OSL signal of all the dosimeters.

Figure 9. Response of OSLDs made similar after applying ICF.
Reproducibility of OSLD
Five OSLDs were chosen and irradiated for a uniform dose of 200 cGy. The reproducibility was checked by repeating this measurement 3 times and a graph was plotted between the dosimeter number and the normalised OSL signal, as shown in Figure 10. From these measurements, we have found the maximum percentage deviation for reproducibility in the OSLDs to be within ±3%.

Figure 10. Reproducibility of OSLDs.
Output factors and beam quality dependence
The output factors for each field size normalised to the reference field (10 × 10 cm2) were obtained and there was a linear increase in OSL signal with an increase in field size. The output factors of OSLDs were compared to ionisation chamber results. It was found that the output factors of OSLDs for field sizes of 15 × 15, 20 × 20 and 25 × 25 cm2 were +0·5%, +1·2% and +1·4% higher than the corresponding ionisation chamber readings, as shown in Figure 11. The OSLDs showed a 5% higher response to the Cobalt-60 beam when compared to 6 MV photon beam, while there was a 3% lower response for 15 MV beam when compared to 6 MV beam, as shown in Figure 12.

Figure 11. Relative output factors for a 6 MV X-ray beam measured with OSLDs and 0·6 cc PTW ion chamber.

Figure 12. Energy dependence of OSLD with 6 MV as normalised value.
Dose-rate dependence of OSLD
For dose-rate dependence, the OSL signal was found to be less dependent on the rate at which the dose was being delivered. The OSL signal for different dose rates was within a percentage deviation of ±3%, as shown in Figure 13.

Figure 13. Dose-rate dependence of OSL detectors in a 6 MV linac beam where the response was normalised to the reading at a dose rate of 100 cGy/minute.
Calibration of OSLD for 6 MV beam using linear accelerator
The OSLDs were irradiated for different doses at the d max position and the dose–response graph was plotted, as shown in Figure 14. It is was found that the OSL signal increased with a delivered dose and showed linearity from 5 to 400 cGy with a root mean square value of 0·999. Therefore, a single calibration was found to be sufficient to measure doses of this range.

Figure 14. Normalised OSL signal versus increase in the dose (cGy) for 6 MV X-ray beam irradiation.
Bleaching of OSLD
Bleaching is a technique by which the residual traps are removed by optical exposure of OSLDs to visible light for a certain period of time. The comparison between the two types of bleaching was carried out. It was found that the average residual doses were 3 and 15 cGy for CFL and halogen-based methods of bleaching, respectively, as shown in Figure 15.

Figure 15. Comparison of OSL residual on different modalities of bleaching.
In vivo dosimetry
The in vivo dose measurements were performed and analysed for the five patients involved in the study. The measurements were carried out for 3 consecutive days for each patient and compared with that of TPS calculated dose values. The percentage deviation of the OSLDs when compared to the TPS dose was found to be within ±2·77% and ±2·03% for the right eye and left eye, respectively, as shown in Table 1. Therefore, the maximum percentage deviation was found to be within ±2·77%. These results were found to be in agreement with dose measurements performed by Meeks et al. using TLD for IMRT patients.Reference Meeks, Paulino and Pennington11
Table 1. In vivo dose measurement for five IMRT patients

Discussion
The key reason for using OSLDs in this study is to characterise this potential dosimeter and implement the same for accurate and precise in vivo dose measurements. The OSLDs showed good reproducibility, indicating that even their sensitivity variation for the same dose can be corrected using ICF. The OSL signal for field sizes greater than 10 × 10 cm2 was higher than the ionisation chamber signal for output factor measurement, potentially proving that OSLDs are highly sensitive to scatter dose compared to ionisation chambers. These results were comparable to Viamonte et al.Reference Viamonte, da Rosa and Buckley4 who reported less than 1% difference between output factor measurement with OSLD and ionisation chamber. Therefore, OSLDs can serve as effective dosimeters for measuring scatter dose. While the OSLDs showed 3% lower response for beam energy of 15 MV when compared to 6 MV in our study, Schembri and Heijmen reported a difference of 4% between 6 and 18 MV.Reference Schembri and Heijmen12 In order to reduce the uncertainties in measuring doses, it is always better to use separate calibration for 6 and 15 MV beams. OSLDs showed over-response with a decrease in beam energy for Co60 beam. As there is a fluctuation observed for different beam qualities, OSLDs are not suitable for dose measurements involving mixed beam energies. The reason for higher response of OSLDs for lower energies is due to the non-tissue equivalence of Al2O3:C. OSLDs were found to be less dose-rate dependent, which was found to be similar to the data published by Schembri and Heijmen.Reference Schembri and Heijmen12 OSLDs can measure doses in a wider range when compared to other relative dosimeters. They also show linear response for doses from 5 to 400 cGy from which it is concluded that OSLDs are useful in measuring doses for the clinically relevant dose range that are conventionally used for treatment. The CFL method of bleaching was found to be more effective when compared to the halogen method of bleaching, and it was concluded to be a safer and more proficient method of bleaching. The OSLDs could be placed closer to the CFL source while bleaching due to the less heat produced by this light source. The proximity of the OSLDs to the light source increased the intensity of light, thus facilitating rapid bleaching. ABS plastics are likely to get deformed due to heat when kept closer to the halogen source. In order to reduce the effect of heat, the OSLDs were kept at a distance of 15 cm and were successfully bleached using the halogen source. The advantage of halogen method of bleaching is that a greater number of OSLDs can be uniformly bleached at the same time. During in vivo eye dose measurements, we have found that OSLDs were able to detect low dose and the response was comparable to that of calculated TPS dose. However, this study reveals the dose–response characteristics of OSLDs up to 4 Gy which was the maximum dose used in the calibration process. Also, the maximum dose rate that was studied was 600 MU/min. Therefore, for advanced radiotherapy techniques involving higher doses (>4 Gy), namely, stereotactic radiosurgery (SRS) and stereotactic body radiotherapy (SBRT), the response characteristics of OSLD at higher dose rates must be investigated in addition to raising the maximum dose in the calibration procedure.
Conclusions
The characterisation of the OSLD has proven it to be a perceptible dosimeter which provided accurate dose measurements within ±2·77% in the patient study. In addition to excellent dose linearity, reproducibility, sensitivity and dose-rate independence, OSLDs have added advantages such as quick and multiple readout capabilities and faster bleaching process. Optimisation in OSLD bleaching must be taken into consideration as different bleaching techniques have different effects over time. From this study, we conclude that OSLD is a precise dosimeter that can be used for routine in vivo measurements for sophisticated treatment techniques such as IMRT involving conventional dose rates and doses. For modern techniques involving newer dose regimens, we recommend extending this work to understand the OSLD response at higher dose rates and dose per fractions to enable accurate dose measurements.
Acknowledgements
The authors would like to thank the staff of the Department of Radiation Oncology, Christian Medical College, Vellore, for their support. The authors thank Mr. Joshua P. Giftson for his help in editing the manuscript.
Funding
Institutional research grant from Christian Medical College, Vellore.
Conflict of interest
The authors declare that there is no conflict of interest regarding the publication of this paper.




















