Introduction
Major hemorrhage is a serious condition in the prehospital setting, as uncontrolled hemorrhage, together with traumatic brain injury, represents the leading cause of trauma-related deaths. Reference Griggs, Jeyanathan and Joy1
The mortality is associated with development of the lethal triad, a combination of hypothermia, acidosis, and coagulopathy. Reference Shaz, Winkler, James, Hillyer and MacLeod2 These are common physiological disturbances in hemorrhagic patients, as major hemorrhage leads to hypo-perfusion and cellular hypoxia, causing a shift to anaerobic metabolism and consequently metabolic acidosis. The anaerobic metabolism limits endogenous heat production, causing exacerbation of any hypothermia and further coagulopathy. Reference Jansen, Thomas, Loudon and Brooks3 Low temperature (ie, in the outside) trauma milieu may further aggravate the condition. Dilution, consumption, and use of platelets and coagulation factors, together with various degrees of hyperfibrinolysis, contributes to the development of coagulopathy. The triad drives a worsening cycle, which rapidly can become fatal unless immediate resuscitation is commenced. Upon hospital arrival, approximately 25% of trauma patients are already coagulopathic, which is associated with poor outcomes. Reference Sheppard, Schaub and Cap4 The literature suggests that the mortality is two- to four-times higher in trauma patients who develop coagulopathy compared to those who do not, even after stratification for injury severity score. Reference Sheppard, Schaub and Cap4 Moreover, the coagulopathic trauma patients have an increased risk of multi-organ failure, especially renal failure, and prolonged intensive care stay. Reference Curry and Davis5
The management of hemorrhagic patients has changed significantly over the last decade, among others, based on clinical experiences from military conflict zones. Reference Jansen, Thomas, Loudon and Brooks3 There has been a shift away from aggressive crystalloid fluid resuscitation of hemorrhagic patients. Crystalloid infusion alone can interfere with hemostatic mechanisms and cause dilutional anemia, dilutional coagulopathy, and reduced blood oxygen carrying capacity, together with hyperchloremic acidosis. Reference Holcomb, Donathan and Cotton6 New strategies, such as damage control resuscitation, emphasize minimal use of crystalloid fluids and early transfusion of blood components. Reference Jansen, Thomas, Loudon and Brooks3
This shift towards the use of blood as the primary resuscitation fluid has led to an introduction of early transfusion in the prehospital environment. Several helicopter Emergency Medical Service (HEMS) teams have implemented it, and initial research has shown encouraging results. A United States HEMS study found prehospital administration of red blood cells (RBCs) associated with increased 24-hour survival, lower 24-hour transfusion requirements, and decreased risk of shock. Reference Brown, Sperry, Fombona, Billiar, Peitzman and Guyette7 In another study by a United Kingdom HEMS, a non-significant reduction in mortality among patients with traumatic hemorrhage receiving prehospital RBCs was reported. In addition, the patients were significantly less likely to receive in-hospital massive transfusion. Reference Griggs, Jeyanathan and Joy1 Severe hemorrhage is frequently associated with disruptions of coagulation function, thus plasma transfusion may be a valuable treatment option in the prehospital setting. Yet another study compared trauma patients receiving prehospital RBCs and thawed plasma to a control group receiving crystalloid resuscitation only. This study found improved early outcomes in the transfused group, but no overall survival advantage. Reference Holcomb, Donathan and Cotton6 Moore, et al assigned 144 trauma patients in hemorrhagic shock to prehospital plasma or isotonic saline infusion in a randomized, controlled design. No difference in primary endpoint, 28-day mortality, was reported. Reference Moore, Moore and Chapman8,Reference Naumann, Doughty and Cotton9
Despite different mechanisms, similar clinical manifestations may be seen in patients with non-traumatic hemorrhage. Research on patients with non-traumatic hemorrhage is limited, but it seems likely that prehospital transfusion can prevent death from exsanguination by mitigating coagulopathy and oxygen deficit.
Existing literature on early transfusion in the prehospital environment has mainly involved helicopter services covering a large population, treating patients with traumatic hemorrhage. In this study, a protocol was implemented for prehospital blood component therapy in a Danish, paramedic-doctor-staffed, ground-based prehospital critical care (PHCC) service with the intention to treat patients with either traumatic or non-traumatic hemorrhages covering a medium-sized city and its surroundings. The objective was to investigate whether prehospital transfusions could be feasible, needed, and beneficial in this system.
The aim of this paper was to characterize patients receiving prehospital blood component therapy and to evaluate whether this treatment modality should be available in the future.
Methods
Study Design
This was a prospective, non-randomized, observational clinical study.
Study Subjects
All patients receiving prehospital blood component therapy by the PHCC team during the study period, from May 1, 2017 through October 31, 2018, were included. Other teams in the Central Denmark Region could request assistance from the PHCC team if prehospital transfusion was required, and these patients were also included. No patients were excluded from data analysis. All patients were delivered to a Level I trauma center at a nearby University Hospital.
Setting
The local PHCC team is part of the Emergency Medicine Service in the Central Denmark Region. The team comprises a PHCC-trained anesthesiologist and a paramedic or emergency medical technician that staffs one 24-hour rapid response vehicle. Reference Rognås, Hansen, Kirkegaard and Tønnesen10 It covers a city area with a population of approximately 334,000, including surrounding suburban and rural areas. The city has low crime rates and short transport time to the nearby University Hospital. The PHCC team is dispatched to approximately 5,600 missions per year, treating patients of all ages. Roughly 20% of the treated patients are trauma patients.
Since May 1, 2017, the PHCC team has carried two units of O-negative RBCs and two units of fresh and never-frozen plasma in a specially designed container (Credo Cube, series 4, 2 l Insulation 15 VIP; Pelican BioThermal; Plymouth, Minnesota USA). To reduce waste, the blood products were returned to the blood bank for in-hospital use within a specified time range defined individually for each product upon delivery. An electronic temperature logging device was placed in the container. If, for any reason, temperature exceeded a pre-specified level, the blood products were discarded. The blood bank was located in close geographical relation to the PHCC team’s base, which made recycling logistically convenient.
The decision to administer blood components was on the doctor’s discretion based on clinical signs and international guidelines. Blood products were transfused warm, using Belmont Buddy Lite fluid warmer (Belmont Instrument Corporation; Billerica, Massachusetts USA), unless the need for instant transfusion was considered to outweigh the advantages of warm fluids.
Data Collection
Data were collected prospectively. The records included personal data, indication for transfusion, mechanism of injury, vital signs, prehospital procedures (tranexamic acid, intubation), and units of RBC and plasma transfused. In-hospital data were collected from the Electronic Patient Journal of the Central Denmark Region. The data included initial vital signs, initial blood gas, in-hospital transfusion in the first hour and the first 24-hours, surgical and interventional radiology procedures, hospital length-of-stay, intensive care unit (ICU) length-of-stay, and 24-hour and 28-day mortality.
Approvals
The Regional Committee on Health Research Ethics (reference 1-10-72-1-20) has been notified and approved the study setup. No individual patient’s identification was stored in the file with patient characteristics, thus permission from the National Data Safety Agency was therefore not required.
Results
Patient Demographics
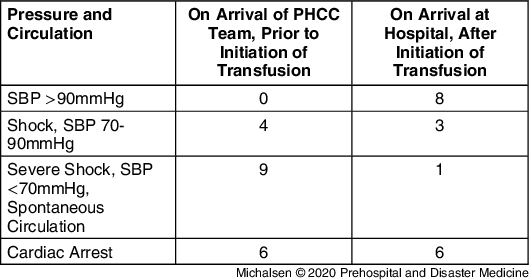
Twenty-one patients (16 male and five female with a mean age at 52 years) received prehospital blood component therapy during the study period and were all included. A small majority of 12 patients (57%) had traumatic injuries, while nine patients (43%) had non-traumatic bleeds. The median number of units transfused was 1.5 (range 1.0-2.0) units of RBC and 1.0 (range 0.0-2.0) unit of plasma. A summary of patient characteristics is given in Table 1.
Table 1. Characteristics of Patients Receiving Prehospital Blood Component Therapy
Abbreviations: PHCC, prehospital critical care; RBC, red blood cells.
Mechanism of Injury
Of the patients with traumatic injuries (57%), the most frequent mechanisms of injury were fall from height (n = 4), penetrating trauma (n = 4), and road traffic collisions (n = 4). For the patients with non-traumatic bleeds (43%), suspected ruptured abdominal aorta aneurysms and gastrointestinal bleeding were the most common causes.
The most frequent trigger to initiate transfusion was on-going excessive bleeding and combined with clinical signs of bleeding like hypotension, tachycardia, loss of radial/carotid pulse, hypovolemic cardiac arrest, and loss of consciousness in a bleeding patient. The physicians could list several triggers per patient.
Prehospital Treatment
The most common additional prehospital procedure was administration of tranexamic acid (n = 13) followed by endotracheal rapid sequence intubation (n = 10). In 11 cases, the team opted not to use the blood-warmer for the prehospital transfusions.
Effect of Blood Component Therapy on Hemodynamic Parameters
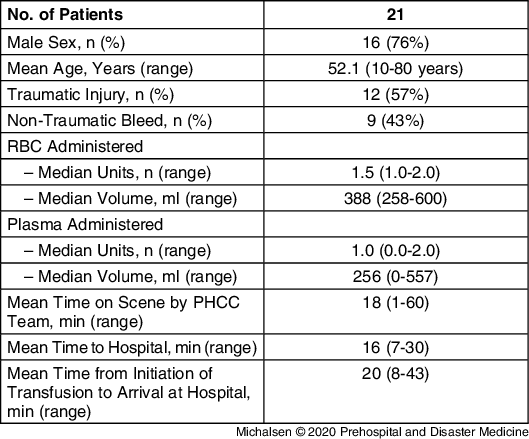
On arrival of the PHCC team, no patients included in the study presented with a normal circulation defined as systolic blood pressure (SBP) >90mmHg. Prior to initiation of transfusion, nine patients presented with severe shock with SBP <70mmHg, and six patients had shock with SBP between 70-90mmHg. After administration of prehospital blood component therapy, a strong majority of the patients improved blood pressure physiology. On arrival at hospital, only one patient was still in a severe-shock condition with spontaneous circulation, while three patients presented increased SBP of 70-90mmHg. Eight patients had stabile SBP >90mmHg, as demonstrated in Table 2. Data on blood pressure were missing for two patients on arrival of the PHCC team and for three patients on arrival at hospital.
Table 2. Prehospital Patient Physiology (Number of Patients)

Abbreviations: PHCC, prehospital critical care; SBP, systolic blood pressure.
Among the six patients with whom cardiac arrest was diagnosed upon arrival of the PHCC team, three patients were declared dead on scene and not transferred to hospital despite advanced treatment, including transfusions. None of the three other patients found in cardiac arrest in whom treatment carried on during transport to hospital had prehospital return of spontaneous circulation (ROSC).
In-Hospital Transfusion and Intervention
Eighteen patients were admitted to hospital, all of them to a Level I trauma center. Mean transport time to hospital was 18 minutes and mean time from initiation of prehospital transfusion to arrival at hospital was 24 minutes. Three patients were taken to hospital without spontaneous circulation but with on-going cardiopulmonary resuscitation. One of these had ROSC in the emergency department and survived past 28-day follow-up, but had a long ICU stay of 34 days. The other two patients were declared dead in the emergency room within the first hour after admission. Of the other 16 patients, full records were available for 12 (75%), while four patients had incomplete records. Blood gas analysis on arrival is illustrated in Table 3.
Table 3. Blood Gas on Arrival at Hospital (n = 14)

Eleven of the patients taken to hospital received further transfusions (61%) and two proceeded with massive transfusion protocol, defined as >5.0 units in the emergency department or >10.0 units in 24 hours. Urgent surgery was required for 13 patients within the first 24 hours and one patient had an interventional radiology procedure, as shown in Table 4.
Table 4. In-Hospital Records on Transfusion and Interventions among Patients Arrived at Hospital (n = 18)

Patient Outcome
For patients surviving the first 24 hours, the mean ICU length-of-stay was eight (range 0-34) days and mean hospital length-of-stay 18 (range 2-64) days. One patient was still hospitalized at day 28 at the cut-off for follow-up. For the patients who survived to hospital, the mortality at 24-hours was 17% and at 28-days was 22%. When including all 21 patients receiving prehospital blood component therapy, the mortality was 29% at 24-hours and 33% after 28-days.
Discussion
These results show that prehospital blood component therapy is feasible in a ground-based, prehospital service in a medium-sized Scandinavian city. Taken into consideration the clinical presentation of the patients treated and the apparent effect of the prehospital blood products, these study results suggest that prehospital transfusion with plasma and RBCs represents a potential benefit for the bleeding patient.
The frequency of transfusion was on average one every 26 days. There were 50% more transfusions in the last six months compared to the first six months of the study period. This may indicate that the frequency will increase as the PHCC team becomes more familiar with the new treatment option, although the frequency of patients treated with prehospital blood component therapy was rather low relative to the total missions. A high ratio of female patients were transfused, that differs significantly from the standard trauma population and most likely reflects the strategy to include all patients with clinical signs of major bleeding.
It was found that the majority of patients receiving prehospital blood component therapy were severely hypotensive on arrival of the PHCC team. Patients with spontaneous circulation upon PHCC team arrival presented less physiological shock after administration of prehospital RBCs and plasma. This was demonstrated by improved blood pressures on arrival at hospital compared to prehospital observations prior to transfusion. The observation of a beneficial effect of prehospital blood component therapy on hemorrhagic shock is in agreement with findings from Lyon, et al Reference Lyon, de Sausmarez and McWhirter11 and Brown, et al. Reference Brown, Sperry, Fombona, Billiar, Peitzman and Guyette7 Base excess at hospital arrival was within the near-normal range, indicating that circulation in this severely affected patient cohort was restored to a sufficient level. During major bleeding, a target level Hb of 7g/dl to 9g/dl is recommended. Reference Spahn, Bouillon and Cerny12 Hemoglobin levels upon hospital arrival were, in more patients, within or close to normal reference levels, that is unnecessary high. This issue reflects the difficulties, especially in the prehospital setting, to use hemoglobin levels rather than clinical and physiologic signs as guidance during acute, major bleeding.
Concerning the patients with presumed hypovolemic cardiac arrest, relatively poor outcomes were found. None of the patients had prehospital ROSC. Nevertheless, one of these six patients survived through the 28-day follow-up period. Lyon, et al Reference Lyon, de Sausmarez and McWhirter11 describes a plausible association between prehospital transfusion of RBCs and a higher ROSC rate, compared with previous studies of traumatic cardiac arrest.
The current study experience and results may have implications for the potential expansion of prehospital blood component therapy to other rapid response vehicles in Denmark and in other Scandinavian cities with physician/paramedic PHCC teams and similar case load and case mix. The frequency of transfusion and the ability to improve patient physiology, in both traumatic and non-traumatic hemorrhages, may justify the implementation. However, a close collaboration and logistical support from the local blood bank is essential to reduce waste and to ensure proper supply of universal donor blood.
Limitations
First, there is a methodological limitation to observational retrospective studies, due to an inherent risk of confounding and uncontrolled bias. Furthermore, the study group contains a small number of patients, and despite a generally high data availability, a few prehospital and in-hospital records were incomplete. In order to evaluate rare outcomes, such as transfusion complications or ROSC in hypovolemic cardiac arrest, a large sample size is needed. Lack of a control group, which makes the study unable to conclude with certainty that prehospital blood component therapy is associated with improved outcomes, represents a major limitation. Lastly, the decision to transfuse, which component to transfuse first, and the total amount to transfuse was a clinical decision made by the anesthesiologist on scene, and not driven by a specific protocol, which makes the decision to transfuse prone to variability.
Conclusion
In this retrospective cohort study, the use of prehospital blood component therapy was evaluated by the paramedic-doctor-staffed PHCC team.
This study confirmed that prehospital blood component therapy is feasible in a ground-based prehospital service in a medium-sized Scandinavian city. In line with previous literature, improved patient physiology was found along with milder degrees of shock after prehospital administration of blood components. The frequency of transfusion and the treatment’s ability to improve patient physiology supports the notion that prehospital blood component therapy may represent a valuable option in the prehospital setting in medium-sized cities.
Further prospective research, with an adequate sample size, is required to conclude with certainty that prehospital blood component therapy is associated with improved outcomes.
Conflicts of interest/funding
The study was based in internal funding only. The authors declare that they have no competing financial or non-financial conflicts of interest.
Acknowledgements
All authors wish to thank the medical staff of the PHCC team for their assistance with data registration. A special thanks to staff secretary Louise Kiib for help with data collection.
Author Contributions
LR conceived the study. LR, CF, CE, and MV designed and implemented the protocol for prehospital blood component therapy. KM collected and analyzed the data. KM wrote first draft of the manuscript. All authors approved the manuscript before submission.