Introduction
Negative schematic beliefs play a key role in psychological models of psychosis (Garety et al., Reference Garety, Kuipers, Fowler, Freeman and Bebbington2001; Morrison, Reference Morrison2001). Early experiences and negative life events (e.g. trauma, neglect) may lead to the development of negative beliefs about the self and others. These negative beliefs then contribute to the development and maintenance of psychotic symptoms such as hallucinations and delusions. Negative schemas have been defined as stable negative beliefs about the self and others which influence interpretations of specific situations, and often develop from early negative experiences (Beck, Reference Beck2011). High levels of negative beliefs about the self and others are common in people with psychosis (Fowler et al., Reference Fowler, Freeman, Smith, Kuipers, Bebbington, Bashforth and Garety2006). Two recent reviews have identified a connection between paranoia and negative self-beliefs (Kesting and Lincoln, Reference Kesting and Lincoln2013; Tiernan et al., Reference Tiernan, Tracey and Shannon2014). Early maladaptive schemas in individuals with psychosis have also been associated with distress and low social functioning (Taylor and Harper, Reference Taylor and Harper2017).
A case study outlined the use of imagery within cognitive therapy for psychosis some years ago (Morrison, Reference Morrison2004). Several years later, Schulze and colleagues (Reference Schulze, Freeman, Green and Kuipers2013) examined intrusive images in 40 individuals with psychosis who had persecutory delusions. Seventy-three per cent (n = 29) reported persecutory beliefs, paranoid related images and associated beliefs (e.g. ‘I am vulnerable and need to be on my guard’) related to these images. In recent years, a small number of studies have examined imagery-focused work in relation to different aspects of psychotic experience, such as voices (Ison et al., Reference Ison, Medoro, Keen and Kuipers2014), and more recently in relation to voice hearers with traumatic experiences (Paulik et al., Reference Paulik, Steel and Arntz2019), nightmares (Sheaves et al., Reference Sheaves, Onwumere, Keen and Kuipers2015) and in generating positive imagery in first episode psychosis (Laing et al., Reference Laing, Morland and Fornells-Ambrojo2016). In relation to imagery and paranoia, there have been two studies in non-clinical analogue samples: Bullock et al. (Reference Bullock, Newman-Taylor and Stopa2016) and Newman-Taylor et al. (Reference Newman-Taylor, McSherry and Stopa2019). To date, none of the above studies has focused on using an imagery-focused approach to work with images and schemas to reduce paranoia.
Taylor et al. (Reference Taylor, Haddock, Speer and Bee2020) used a qualitative approach to explore core beliefs and schema in psychosis and their links with hallucinations and delusions. Four emergent themes were identified: the solidity and permanency of core beliefs, the synergy between beliefs and symptoms, the concordance between life events and interpersonal relationships, and links between beliefs and images. The first examination of schemas in psychosis using the experience sampling method demonstrated that negative-self and negative-other schematic beliefs predicted severity of hallucinatory and delusional psychotic experiences and distress and functioning problems associated with these (Taylor, Bee, Emsley, Taylor, Ibbs, Baker and Haddock, manuscript Reference Taylor, Bee, Emsley, Taylor, Ibbs, Baker and Haddockunder review).
Freeman et al. (Reference Freeman, Pugh, Dunn, Evans, Sheaves, Waite and Fowler2014) tested a brief intervention to reduce negative self-beliefs. The therapy aimed to improve self-confidence using strategies including positive psychology techniques and activities. The study found that both the therapy and the trial design were feasible and acceptable. Although this was not an efficacy study, outcomes were reported, indicating only a small reduction in negative schemas (Cohen’s d = –.24) and a moderate reduction in paranoia (d = 0.59). There was no reported use of imagery-focused techniques to change beliefs or schema.
A recent systematic review examined whether schema therapy, a therapy incorporating imagery techniques, changed schema across mental health disorders (Taylor et al., Reference Taylor, Bee and Haddock2017), but no studies were found which tested schema therapy for psychosis. Imagery-focused cognitive behavioural approaches have previously been described (Hackmann et al., Reference Hackmann, Bennett-Levy and Holmes2011) in the treatment of other disorders, e.g. social phobia (Wild et al., Reference Wild, Hackmann and Clark2007) and bipolar disorder (Holmes et al., Reference Holmes, Bonsall, Hales, Mitchell, Renner, Blackwell and Di Simplicio2016) which have shown benefits in reducing negative beliefs (Morina et al., Reference Morina, Lancee and Arntz2017), but again, no studies have tested these techniques in psychosis to reduce schema and images.
Imagery and perception both derive from shared neural mechanisms and in addition, a number of studies have highlighted that imagery is distinct from language (Kosslyn et al., Reference Kosslyn, Ganis and Thompson2001; Pearson et al., Reference Pearson, Naselaris, Holmes and Kosslyn2015).
The links between schemas and images highlighted in the earlier qualitative study (Taylor et al., Reference Taylor, Haddock, Speer and Bee2020) suggest that targeting both schemas and images may reduce distress in psychosis. Imagery can also have a more powerful effect on emotion than verbal language (Holmes and Mathews, Reference Holmes and Mathews2010), and so has the potential to achieve more powerful change (compared with standard cognitive or thought-based approaches) if used within therapy for people with psychosis.
Given the close links between negative events, images, negative schema and paranoia, we developed a strategy to work with negative intrusive images and schema. We anticipated that that a reduction in negative schematic beliefs and improvement in positive schematic beliefs, through an imagery-focused therapy approach would lead to indirect change on persecutory delusions.
Case series multiple baseline designs are an established strategy for developing treatments (Craig et al., Reference Craig, Dieppe, Macintyre, Michie, Nazareth and Petticrew2008). Benefits include the creation of control measurements without the addition of separate control participants and controlling for the therapeutic effect of contact with a therapist but without therapy being undertaken. It is also important to measure the therapeutic alliance, as this plays a crucial role in influencing outcomes (Priebe and McCabe, Reference Priebe and McCabe2006; Mulligan et al., Reference Mulligan, Haddock, Hartley, Davies, Sharp, Kelly, Neil, Taylor, Welford, Price, Rivers and Barrowclough2014). Furthermore, an area that has been under-examined previously in psychological studies is possible adverse effects of therapy (Klingberg et al., Reference Klingberg, Herrlich, Wiedemann, Wölwer, Meisner, Engel, Jakobi-Malterre, Buchkremer and Wittorf2012).
Imagery rescripting has not yet been utilised in individuals with persecutory delusions. This study aimed to formally test the feasibility and acceptability of an imagery-focused approach for individuals with delusions, exploring the impact on negative schematic beliefs, imagery characteristics and persecutory delusions. This involved examining if participants could be recruited to a case series study, the number who completed sessions, the number who dropped out, reasons for dropping out, feedback on the intervention, and feedback on any adverse effects of therapy.
Method
Design
A non-concurrent A-B multiple baseline design was used. Participants were randomised to a multiple baseline of 2–5 assessments delivered weekly but flexibly. Participants then received six sessions of therapy and an end-of-therapy assessment.
Procedure
Participants were randomised to a specific baseline length by an independent researcher at a different institution using a secure web-based randomisation service (Sealed Envelope). This allowed allocation to differing baselines (2, 3, 4 or 5). Randomisation over differing baseline length conditions allowed treatment effects to be delineated from the effect of time. Therapy began at the end of the baselines, if there was stability in delusions. Similar to other multiple baseline designs, we defined stability as either a stable or worsening clinical presentation on the basis of PSYRATS (i.e. an absence of improvement; Wells et al., Reference Wells, Fisher, Myers, Wheatley, Patel and Brewin2009). If the participant reported improved psychotic experiences within the baseline period, the baseline period would be extended for additional visits to assess if symptoms were continuing to improve. A further option was to offer the opportunity to be re-contacted at a future point to re-assess if symptoms and psychotic experiences had changed (either stablised or worsened).
The intervention was planned to be six sessions, with flexibility for one or two additional sessions, if indicated by presentation.
Participants
Inclusion criteria were: (i) a current or recent (within last 2 weeks) persecutory delusion meeting criteria outlined by Freeman and Garety (Reference Freeman and Garety2000) (the individual believes that harm is occurring or is going to occur to him or her and the persecutor has the intention to cause harm), (ii) identifying a distressing image related to a persecutory delusion, (iii) capacity to give informed consent, (iv) finding their reported paranoid beliefs distressing or be help seeking for paranoid or suspicious beliefs (persecutory delusions; defined as distress rating of minimum 1 out of 4 on PSYRATS), (v) aged 18–65 years, (vi) meeting criteria for a schizophrenia-spectrum diagnosis (schizophrenia, schizoaffective disorder, delusional disorder; ICD-10; WHO, 1992), (vii) receiving care from an NHS mental health service, (viii) able and willing to complete the interview and assessments in English with scores which demonstrate either stability or an absence of improvement as defined by PSYRATS, and (ix) medication stable for ≥1 month prior to the study. Exclusion criteria were: (i) moderate/severe learning difficulties, acquired by brain injury/neurological impairment, (ii) severe substance misuse judged to be the acute cause of psychosis, (iii) experiencing an acute episode requiring in-patient care, or (iv) currently participating in treatment studies or receiving psychological therapy.
Feasibility and acceptability
Our primary interest was the feasibility and acceptability of iMAPS therapy. This was assessed by measuring recruitment rates (numbers of potential participants approached, screened for eligibility, eligible and declined, eligible and consented), attendance at therapy sessions [did not attend (DNA) and could not attend (CNA) rates], adverse effects, whether therapeutic alliance was established and maintained, and serious adverse events. Previous CBT for psychosis trials have aimed to recruit one consenting participant for every three approached (Freeman et al., Reference Freeman, Kingdon, Startup and Dunn2011). We set a criteria of attending ≥3 sessions as reflecting reasonable attendance of a 6-session intervention. Therapeutic alliance scores below 30 or substantial discrepancies between therapist and client versions were considered poor according to the Working Alliance Inventory (WAI-SR; Hatcher and Gillaspy, Reference Hatcher and Gillaspy2006). A substantial number of adverse therapy effects (e.g. all participants worsening following therapy) or serious adverse events were indicators of therapeutic safety. Adverse effects were determined on a case-by-case basis.
Exploratory measures
We did not specify a primary outcome, as the study aimed to identify a suitable primary outcome for a larger trial (Lancaster et al., Reference Lancaster, Dodd and Williamson2004). Diagnosis was confirmed by the participant’s psychiatrist, a case note review and a standardised ICD-10 checklist by the first author. The sessional and outcome measures were: the Psychotic Symptom Rating Scales (PSYRATS; Haddock et al., Reference Haddock, McCarron, Tarrier and Faragher1999), the Positive and Negative Syndrome Scale Positive subscale (PANSS; Kay et al., Reference Kay, Fiszbein and Opler1987), The Calgary Depression Rating Scale for Schizophrenia (CDSS), an interview schedule adapted from an imagery interview previously used in social phobia (Hackmann et al., Reference Hackmann, Surawy and Clark1998; Ison et al., Reference Ison, Medoro, Keen and Kuipers2014), the Mental Imagery in Psychosis Questionnaire (MIPQ; adapted from Holmes et al., Reference Holmes, Bonsall, Hales, Mitchell, Renner, Blackwell and Di Simplicio2016), the Spontaneous Use of Imagery Scale (SUIS; Reisberg et al., Reference Reisberg, Pearson and Kosslyn2003), the Brief Core Schema Scales (BCSS; Fowler et al., Reference Fowler, Freeman, Smith, Kuipers, Bebbington, Bashforth and Garety2006), the Young Schema Questionnaire-Short Form (YSQ-S; Young, Reference Young2003), the Schema Mode Inventory (SMI; Lobbestael et al., Reference Lobbestael, van Vreeswijk, Spinhoven, Schouten and Arntz2010), the Working Alliance Inventory (WAI-SR; Hatcher and Gillaspy, Reference Hatcher and Gillaspy2006) and the Adverse Effects in Psychotherapy (AEP) measure (Hutton, Reference Hutton, Wood and Johnson2016; Pyle et al., Reference Pyle, Norrie, Schwannauer, Kingdon, Gumley, Turkington and Morrison2016). A measure of trauma was considered, but not included to reduce participant burden. Full details of the measures, the frequency of administration (sessionally, pre-post) and psychometrics are reported in the Supplementary Material. Higher scores across the measures generally indicate greater symptoms or greater distress.
The baseline and sessional measures were the PSYRATS Delusions scale, the MIPQ Imagery questionnaire and associated imagery interview questions and sessional mood. The AEP was offered after therapy was completed. All other measures were administered at assessment and end-of-therapy only. Participants were reimbursed £20 in total for participating in the initial assessments and end-of-therapy assessments, but not for the briefer baseline assessments or for attending therapy. Assessments were conducted by the first author, a clinical psychologist with extensive training and experience of the PSYRATS and PANSS, including good inter-rater reliability with other raters (average ICC 0.93).
iMAPS intervention
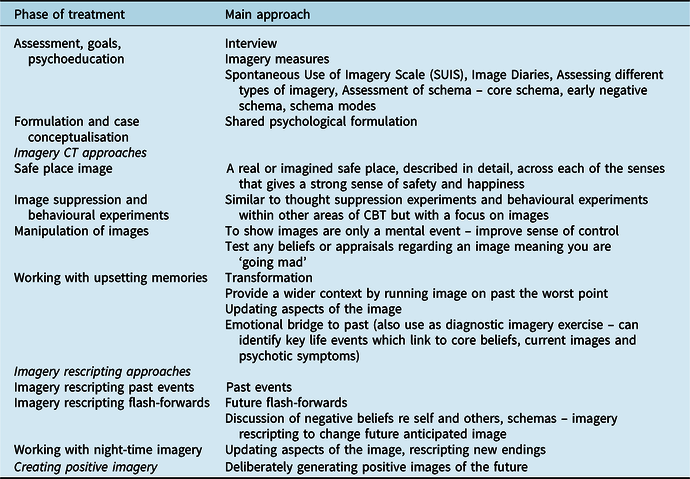
The intervention was developed by the authors from a number of sources, including a systematic review of schema therapy across mental health disorders (Taylor et al., Reference Taylor, Bee and Haddock2017), a qualitative study of core beliefs in psychosis (Taylor et al., Reference Taylor, Haddock, Speer and Bee2020) and a daily experience sampling method study of positive and negative core schema in psychosis (Taylor et al., manuscript Reference Taylor, Bee, Emsley, Taylor, Ibbs, Baker and Haddockunder review). The approach was also influenced by existing cognitive behavioural imagery work (Hackman et al., 2011), an adapted formulation model (Hales et al. (Reference Hales, Blackwell, DiSimplico, Iyadurai, Young, Holmes, Brown and Clark2014) and some schema therapy techniques (Young et al., Reference Young, Klosko and Weishaar2003; Arntz and Jacob, Reference Arntz and Jacob2012); and the researchers’ theoretical knowledge and clinical experience. These were utilised to create a new therapy manual. The iMAPS sessions followed standard CBT practices, including an agenda, regular summaries, feedback, and use of techniques such as a collaborative approach, socratic questioning, guided discovery and between-session tasks (Beck, Reference Beck2011). The therapy is briefly described in Table 1 and in detail in Taylor et al. (Reference Taylor, Bee, Kelly and Haddock2019). It was delivered over six sessions; an additional booster session or two were offered depending on the individuals’ presenting difficulties. Sessions were usually weekly, but were held more or less frequently if requested.
Table 1. Description of iMAgery focused therapy for persecutory delusions in Psychosis (iMAPS)

The first session involved psychoeducation about images and imagery, identified images and negative schematic beliefs, and introduced a diary as a between-session task. A maintenance formulation was developed by the first or second session. Based on the assessment, the therapeutic techniques utilised included a safe place image to help practice imagery. The target for intervention was informed by the iMAPS collaborative formulation. Depending on the nature of the formulation, and discussion with the participant regarding goals, this informed whether a single image was chosen as the target for intervention, or multiple images or if an imagery rescript in relation to a past negative life event or future flash-foward was agreed. The image which was most distressing and the greatest focus of the therapy sessions is the one reported. The formulation informed which techniques could be chosen to be used in the sessions and these were selected from those listed in Table 1. Similar to CBT for Psychosis principles, depending on the presentation, all techniques listed may not necessarily be used, but this could be considered the range of interventions which the therapist could draw from.
Techniques also included image suppression experiments, behavioural experiments, manipulation of images and working with upsetting memories. Imagery rescripting was a key technique used to facilitate belief change and working with past events, flash-forward images, night-time imagery and creation of positive imagery.
Therapy was delivered by the first author who met BABCP (British Association for Behavioural and Cognitive Psychotherapies) minimum training standards for CBT, and who had previous experience as a CBT trial therapist on a recovery-focused CBT for psychosis clinical trial and post-qualification continuous professional development in psychosis. Treatment fidelity was ensured through (1) using the iMAPS manual, supervised fortnightly by the third and last authors (J.K. and G.H.), both experienced clinicians, and (2) audio recording and reviewing sessions in supervision for fidelity. Our study was approved by the United Kingdom Health Research Authority National Health Service (NHS) and from the NHS Trust R & D committee (reference no. 14/NW/1490).
Data analysis
The evaluation focused on feasibility, through assessing number of sessions attended, number of drop-outs, adverse effects of therapy and therapeutic alliance. Descriptive summary statistics for the outcome measures are reported. Visual inspection was used to establish whether therapy commencement preceded improvements in outcome variables. Following advice for pilot studies (Lancaster et al., Reference Lancaster, Dodd and Williamson2004), the analysis did not report p-values (Lancaster et al., Reference Lancaster, Dodd and Williamson2004). The standard deviation of the change scores are used. This was calculated as Cohen’s D = (meanpre – meanpost)/SD(meanpre – meanpost), where ‘pre’ is the initial assessment score and ‘post’ is the end-of-therapy score.
Clinically significant change
Clinically significant change was a ≥25% reduction in PSYRATS delusions from baseline to end-of-therapy assessment (Durham et al., Reference Durham, Guthrie, Morton, Reid, Treliving, Fowler and MacDonald2003). A 50% change was considered ‘much improved’. All analyses were conducted utilising SPSS version 23.0 (IBM, 2015).
Results
Feasibility of recruitment
Eleven service users were approached by their care coordinators; three declined to find out more about the study. Eight participants were assessed for eligibility, with three excluded due to: (i) images resolved from referral to assessment (i.e. they no longer reported intrusive mental images), (ii) high levels of delusional beliefs interfering with ability to engage in assessments in the community, and (iii) disengagement from the assessment. Five participants were assessed as eligible. Therefore, 62.5% of participants who were eligible to consent ultimately participated, consistent with previous studies. These five attended all assessment, baseline and therapy sessions. One declined to attend the end-of-therapy assessment (Participant 5) due to a duty of care issue raised in the final session (see below).
Participants received a mean of 6.40 sessions (SD = 0.89; minimum = 6, maximum = 8). All participants had six sessions, except Participant 2 who had two extra sessions. Thus, all participants exceeded the 3-session attendance threshold previously set as a reasonable level of attendance. Each session lasted 60 to 80 minutes and were offered weekly. Adherence to iMAPS was acceptable, with all participants attending all sessions. Retention was good, with no withdrawals during therapy. There was one withdrawal from the end-of-therapy assessment, due to the disclosure of a risk issue which the therapist was duty bound to report to their manager, the trust and the local council and led to the participant declining the end-of-therapy assessment. Participant 2 had eight sessions because at session 3, he attended in a state of distress, wanting to discuss another mental health issue, and aside from completion of the sessional measures, this session did not focus on the imagery protocol.
Potential adverse therapy effects are reported in the following section (and supplementary table S4), showing low incidence of negative effects of iMAPS therapy. Those reported were relatively minor, such as one participant reporting that taking part made them feel ‘a little embarrassed talking about my problems with people I had not met before’, ‘a little more anxious’, and taking part made them think a little ‘too much about bad things which have happened in the past’. The one item which scored ‘quite a lot’ was regarding concerns about the stigma of psychosis (‘people would think badly of me because of diagnosis’), although this was Participant 2, who overall seemed to benefit. Of the participants who reported one or two items having impacted them ‘very little’, there did not seem to be a pattern between benefiting from therapy and not benefiting from therapy, although this was a small sample size study. There were no serious adverse events related to participation.
During the study, an ethical amendment was submitted to the ethics committee to revise the number of baseline assessments to between two to three on the basis of participant feedback.
Finally, on the shortened Working Alliance Inventory (WAI Hatcher version), which measures therapeutic alliance on the basis of three componments (goals, tasks and bond), therapist ratings were slightly lower than client ratings. The client average score was 46.25 (SD 11.21). Therapist scores were slightly lower.
Baseline data can be seen in Table 2.
Table 2. Outcome data and Cohen’s D effect sizes
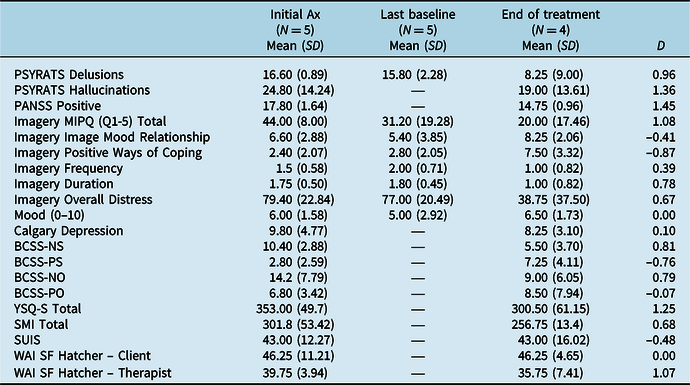
SD, standard deviation; PSYRATS, Psychotic Symptom Rating Scale (Haddock et al., Reference Haddock, McCarron, Tarrier and Faragher1999); PANSS, Positive and Negative Syndrome Scale (Kay et al., 1988); Imagery MIPQ, Mental Imagery in Psychosis Questionnaire; YSQ, Young Schema Questionnaire-Short Form (Young et al., Reference Young, Klosko and Weishaar2003); SMI, Schema Mode Inventory (Lobbestael et al., Reference Lobbestael, van Vreeswijk, Spinhoven, Schouten and Arntz2010); SUIS, Spontaneous Use of Imagery Scale (Reisberg et al., Reference Reisberg, Pearson and Kosslyn2003); WAI-SF Hatcher, Working Alliance Inventory-Short Version (Hatcher and Gillaspy, Reference Hatcher and Gillaspy2006).
The PSYRATS scores indicated high levels of distressing and pre-occupying persecutory delusions. The BCSS negative-self rating was low and positive-self beliefs were slightly lower than this (similar to Freeman et al., Reference Freeman, Pugh, Dunn, Evans, Sheaves, Waite and Fowler2014). Intrusive images were high in imagery characteristics, such as how compelling, vivid, real, absorbing and pre-occupying an image was (average 44.0 out of a possible 50) and highly distressing (79/100).
Demographic and clinical details
Five participants (three men and two women) meeting criteria for a schizophrenia spectrum disorder under the care of an NHS early intervention psychosis service were recruited. Participant ages ranged from 19 to 34 years (mean = 23.40; SD = 6.42). One participant met criteria for schizophrenia, one for delusional disorder, one for schizoaffective disorder and two had no formal diagnosis but were experiencing psychosis and met criteria for entry to receive care from an early intervention psychosis service. All five participants described themselves as White British. Participants’ living arrangements included living in supported accommodation, in a bail hostel, with their partner and parents, and with parents and their child. Four participants were single and one was living with their partner. Two participants were in higher education and three were unemployed. Four were experiencing auditory hallucinations at initial assessment. All five were experiencing persecutory delusions at initial assessment and all had been prescribed one or more anti-depressant medications previously. Three continued with anti-psychotics and other medications during the study (see case descriptions for details). Participants’ details were anonymised to protect confidentiality, and can be found in the supplementary material.
Feasibility and acceptability of therapy
As highlighted above, adherence to iMAPS was acceptable, with all five participants attending all sessions. Retention was good, with no withdrawals during therapy.
Clinical outcomes
Tables 2 and S3 offer a summary of the main outcome measures and the assessments of the proposed psychological maintenance factors. On initial assessment, the reported imagery characteristics, negative schematic beliefs (as measured by BCSS) and psychotic symptoms were high. Figures 1 and 2 display participants’ MIPQ total scores and PSYRATS delusion total scores from initial assessment, baselines, therapy sessions and end-of-therapy assessments. Figure 3 displays the BCSS initial assessment and end-of-therapy assessment scores. As Participant 5 declined to attend the end-of-therapy assessment, each of the figures for Participant 5 has this data missing.

Figure 1. Changes to participant scores on the MIPQ characteristics of images.

Figure 2. Changes to participant scores on the Psychotic Symptom Rating Scales (PSYRATS) Delusional beliefs.
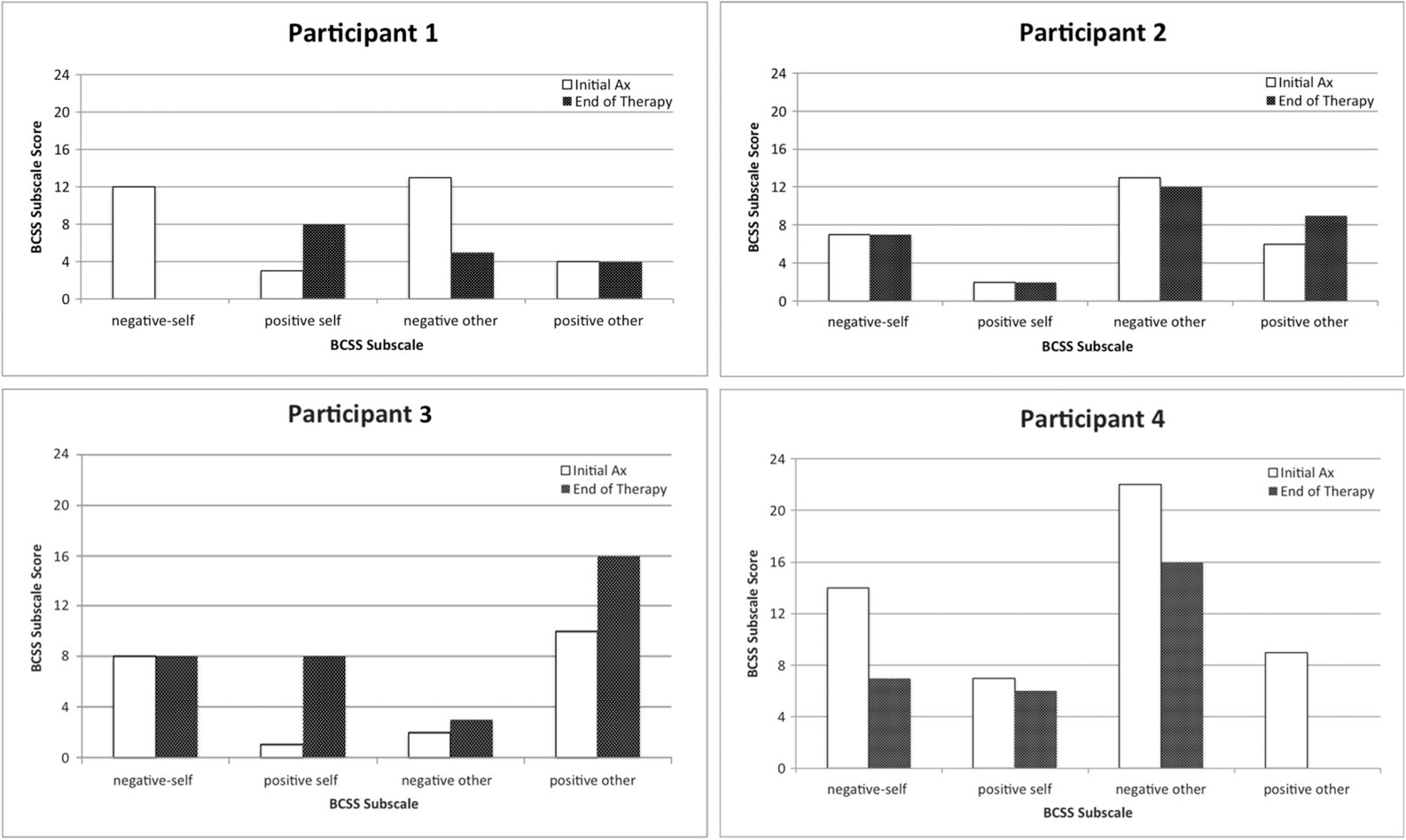
Figure 3. Changes to participant scores on the Brief Core Schema Scales.
Clinically significant change
The results are examined in terms of the Durham et al. (Reference Durham, Guthrie, Morton, Reid, Treliving, Fowler and MacDonald2003) criteria, i.e. a 25% drop is ‘clinically significant change’ and 50% is ‘much improved.
Imagery characteristics
With regard to the overall imagery characteristics, two participants had a ‘much improved’ clinically significant change, with drops of 88.6 and 68%, respectively (Participants 1 and 2). Participant 3 had slight drop in imagery characteristics total score (6.4%). Participants 4 and 5 had slight increases in imagery.
Delusions
On the Durham et al. criteria basis, two participants achieved a 100% drop in PSYRATS delusions (Participants 1 and 2), suggesting much improved clinically significant change, and a third participant was approaching this 25% drop (Participant 3). These changes appear to suggest that imagery characteristics change and core schema change leads to improvement in symptoms. One participant had a slight increase in PSYRATS Delusions (Participant 4) and another had a more significant increase (Participant 5), which in the clinical judgement of the therapist was due to other factors such as chronic insomnia which appeared to worsen their persecutory delusions and additional stress of exacerbated physical health difficulties. PANSS Positive subscale decreased by 17.1 %, which is in the direction of clinical significance, with a large effect size (d = 1.45).
Imagery distress
Across participants (see Table 2), imagery distress dropped by 50% from initial assessment to end-of-therapy assessment with a medium effect size (d = 0.67). Frequency of images decreased by 33%. Duration of images also decreased. However, it is notable that there appeared to be no change in mood mean scores on the Calgary Depression Scale across the participant group.
Schema change
As we were interested in whether an imagery-focused intervention would result in imagery change and change to schematic beliefs (with an indirect reduction on persecutory delusions), we also measured schema using two additional scales, the YSQ and the SMI. Three of the participants had reductions in early maladaptive schemas, as measured by the YSQ, but none of these reached clinical significance. Participant 3 had a 21% drop in YSQ total score, Participant 1 had a 17% drop, Participant 4 had a 13% drop, and Participant 2 had a very slight 1% increase. In terms of schema modes overall score, again three of the participants had reductions in schema modes as measured by the SMI but again, none of these reached clinical significance. Participant 3 had a 16% drop in modes, Participant 1 a 14% drop, Participant 4 had a 4% drop, and Participant 2 a 0.4% increase. In terms of the overall change for participants, supplementary table S3 highlights a 15% change in total scores on the YSQ (d = 1.25). The SMI also demonstrated a significant 14% reduction overall (d = 0.68). As can be seen in supplementary table S3, the 18 early maladaptive schemas all demonstrated a decrease, except emotional deprivation and unrelenting standards.
Hospital admission and serious adverse events
One serious adverse event was reported, for Participant 3 who also had co-occurring substance misuse and used cannabis between sessions 1 and 2, resulting in an increase in persecutory delusions, intrusive images and an informal admission to hospital. There was no evidence to suggest the admission was linked with the therapy intervention. No other serious adverse events occurred.
Discussion
The iMAPS therapy was received well by participants with persecutory delusions, as demonstrated by the high uptake and session completion rates. In three of the five cases, there were positive changes, with two cases achieving much improved clinically significant change with their images, schematic beliefs and persecutory delusions as measured by the PSYRATS. One participant had many more missed sessions, believed to be linked to co-occurring intravenous street diamorphine (heroin) substance misuse and various life events, and experienced a slight increase in PSYRATS. The final participant had numerous physical health problems and chronic insomnia which had an ongoing contribution to her difficulties, in addition to her images.
There was only one serious adverse event during the study, which was not related to the therapy intervention. More broadly, very few negative adverse effects of therapy were reported and these were relatively understandable for a one-to-one therapy intervention (e.g. feeling anxious, worrying what the therapist might think of them, thinking about the past). One participant worried people would ‘think badly of me because of my diagnosis’, highlighting the ongoing difficulties people with psychosis endure with stigma (Wood et al., Reference Wood, Burke, Byrne and Morrison2016). Although we did not specifically target stigma, it is reasonable to consider that future participants who reported images related to stigma or stigmatising episodes from their past might use the imagery techniques to reduce this distress.
Improvements on symptoms and beliefs measures demonstrated large effect size changes. The therapy aimed to work with intrusive negative images and then to use rescripting to achieve change in schematic beliefs and for three of five participants the iMAPS therapy achieved this. There was no overall change in mood, which was surprising. Examining the individual profile of mood changes, there were slight improvements or reductions in negative mood across the participants. Although several participants experienced change in intrusive images and schematic beliefs, and an indirect reduction in persecutory delusions, they also had a number of other symptomatic issues which were not addressed with the brief six-session iMAPS intervention. On the SMI, the negative schema modes all demonstrated a reduction, although some of these were limited, particularly the ‘self-aggrandiser’ mode (where the individual is self-absorbed and lacks empathy) barely changed. Usually, in schema therapy, this mode would be formulated and worked with therapeutically using a two-chair technique, a way of creating change between two sides of one’s self (which was beyond the scope of the present study). The positive schema modes, such as ‘contented child’ and ‘healthy adult’ demonstrated some small increases too. Schema therapists formulating difficulties using a schema mode model would use imagery rescripting to work with vulnerable child modes, so it is notable that of the schema modes which did show change on their scores, vulnerable child mode appears to have one of the largest changes. As other modes were not specifically targeted during this brief imagery-focused therapy intervention, it makes sense that there was more limited change observed on these. The first trial of schema therapy for borderline personality disorder had a therapy window of three years (Giesen-Bloo et al., Reference Giesen-Bloo, van Dyck, Spinhoven, van Tilburg, Dirksen, van Asselt and Arntz2006) and while subsequent trials have reduced this to 50 sessions (Bamelis et al., Reference Bamelis, Evers, Spinhoven and Arntz2014) this is considerably longer than the intervention delivered here.
There are some issues around the style of the intervention which it is worth commenting on. These include that there was little discussion of persecutory delusions, except to acknowledge them in terms of weekly PSYRATS sessional assessment and that in the formulation images and beliefs contributed to making these fears worse for participants (rather than working with delusional beliefs in a traditional CBT for psychosis approach; Kingdon and Turkington, Reference Kingdon and Turkington1994).
In terms of engagement, people with psychosis were willing to talk about these very distressing, vivid, real compelling internal mental images. Engagement was aided by usually spreading the initial assessment over two sessions, to allow trust to begin to be developed with the therapist and for participants to open up about any images which were ego dystonic. All participants also tolerated frequent and repeated assessment of the images and delusional beliefs using the PSYRATS from session to session. The assessment and multiple baselines design meant that the therapist and client were able to quickly move to formulation by session 2 when therapy began. Some case series studies give participants measures while in the waiting room or before the therapy session begins. We integrated this as part of the therapy session structure, having a brief state review and update, then collaboratively agreeing the agenda to include this detailed review of the images and fears, which we believed enhanced engagement in the therapy.
For the two participants where the intervention did not appear to work, in addition to the issues mentioned already, it is also worth noting that Participant 4 struggled to identify a safe place image, a useful first step. This participant struggled to identify any safe place image which can be common for individuals with difficult life histories (in this case, parents who were intravenous drug users). On reflection, moving onto the rescripting work sooner may have yielded more promising results. With Participant 5, a very distressing intrusive, flash-forward mental image had been present throughout the baseline period and sessions, but remained undisclosed until session 5. The addition of a standing agenda item about disclosing new images would be important in future work.
Some participants’ scores were beginning to drop slightly during the baseline period and this could be attributed to the early stages of change which are known to occur when repeated and frequent measurement begins. Research into recovery from psychosis has identified that it consists of a much wider and greater range of facets than reduction in persecutory beliefs (Pitt et al., Reference Pitt, Kilbride, Nothard, Welford and Morrison2007). In terms of the therapeutic alliance, the shortened WAI Hatcher version therapist ratings were slightly lower than client ratings, consistent with previous studies in psychosis (Mulligan et al., Reference Mulligan, Haddock, Hartley, Davies, Sharp, Kelly, Neil, Taylor, Welford, Price, Rivers and Barrowclough2014). As highlighted in the results, the client average score was 46.25 (SD 11.21), similar to a previous study of acceptance and commitment therapy in psychosis (White et al., Reference White, Gumley, McTaggart, Rattrie, McConville, Cleare and Mitchell2011). Therapist scores were slightly lower (although this therapist Hatcher version has ten items and scores range from 10 to 50), suggesting that the client thought the alliance was better than the therapist’s perception of the alliance.
As a brief targeted intervention, it could be added as a module to other theoretically based approaches, which also have initial feasibility and acceptability (Freeman et al., Reference Freeman, Bradley, Waite, Sheaves, DeWeever, Bourke and Lister2016; Hayward et al., Reference Hayward, Strauss and Bogen-Johnston2014). In terms of the change in these other brief targeted approaches, Freeman et al. (Reference Freeman, Bradley, Waite, Sheaves, DeWeever, Bourke and Lister2016) found using strategies to improve self-confidence a small reduction in negative schemas (Cohen’s d = 0.24) and a moderate reduction in paranoia (d = 0.59). Hayward et al. (Reference Hayward, Strauss and Bogen-Johnston2014), in a pilot randomised controlled trial of relating therapy, found a larger effect size of d = 1.30 on PSYRATS distress at end-of-therapy. Our much smaller case series would appear to compare favourably; however, larger studies need to be conducted before meaningful comparisons could be made.
Techniques from schema therapy could be piloted in a similar way for people with psychosis, or a full schema therapy protocol could be tested to assess if wider change in that conceptualisation of schematic beliefs results in a wider symptom improvement. Although this study recruited individuals who were reporting negative intrusive mental images related to their persecutory delusions, this would not necessarily be essential. An imagery-focused approach could have been used in relation to using imagery rescripting of past negative experiences.
Limitations
This was an uncontrolled study meaning that the improvements cannot be attributed with confidence to the iMAPS intervention. The assessments were not blinded, which increases risk of bias, and there was no follow-up to assess if the changes were maintained. Three participants achieved change on images, schematic beliefs and reductions in persecutory delusions. Effect sizes were large and the change for two of the participants was highly clinically significant, and significant for a third participant. Therapy lasted on average six sessions to achieve change. However, two participants did not appear to gain substantial benefit, but did have significant other issues such as undisclosed intravenous drug use while in a bail hostel (Participant 4) and a wide range of physical health problems (Participant 5). Non-specific factors often appear to contribute to positive results, but the multiple baseline randomisation and several assessments can be argued to offer some control for these effects. A further limitation was that the participants recruited described their ethnicity as White British, limiting generalisability.
Our results suggest that iMAPS therapy for persecutory delusions should be evaluated further, in a larger case series or in a randomised controlled trial to overcome several of limitations highlighted above, including a follow-up period to see if change is sustained.
Acknowledgements
We are very grateful to participants and to colleagues within Lancashire Early Intervention Service who referred service users to the study. We acknowledge the National Institute for Health Research Clinical Research Network (NIHR CRN). We thank Neil Caton, Tim Rawcliffe and Rory Byrne for Service User Consultation. We thank Dr Paul Hutton, Edinburgh Napier University, for independently uploading the randomisation to baseline list with the Sealed Envelope system and providing the adverse effects psychotherapy measure.
Conflicts of interest
G.H. receives a share of royalties from manuals on cognitive behaviour therapy and has received fees for delivering workshops on CBT. J.K. receives a share of royalties as a co-author from a CBT manual. The other authors have no financial conflicts of interest to declare.
Financial support
This report is independent research arising from a Research Fellowship Award supported by the National Institute for Health Research (DRF-2012-05-211) awarded to Dr Christopher D.J. Taylor. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health.
Supplementary material
To view supplementary material for this article, please visit: https://doi.org/10.1017/S1352465820000168







Comments
No Comments have been published for this article.