With the risk of terrorist bombings increasing worldwide, it is important for health care providers to become familiar with the spectrum and management of injuries inflicted by blasts and explosions. In 2005, the US Department of State reported approximately 11 000 international terrorist attacks resulting in excess of 14 600 deaths and more than 24 700 people injured.1 In the United States alone, between 1983 and 2002, there were 36 110 bombing incidents resulting in 5931 injuries and 699 deaths.Reference Kapur, Hutson, Davis and Rice2 Explosions and bombings are the most common deliberate weapon of terrorism because of their potential to quickly and inexpensively inflict considerable harm and devastation on large groups of people. The victims of bombings experience a combination of blast, blunt, penetrating, and thermal injuries that fall outside the routine experience of most health care providers. This article reviews the ocular injuries associated with explosive blasts and provides early responders and emergency department (ED) personnel with some basic concepts with which to approach the blast-injured patient with eye trauma.
A MEDLINE literature search (June 2007) with an Ovid interface was performed for citations relating to ocular trauma and blast injuries. We searched on the following terms: blast injuries and the eye, ocular blast injuries, ocular trauma and bombing, terrorism and ocular injuries, management of ocular blast injuries, military ocular injuries, and IED and ocular injuries, and similar terms and combinations. The search yielded 244 articles. Most were from the 2000s, with some articles dating back nearly 40 years. Abstracts were reviewed to select articles with clinical relevance to blast injuries and the eye. We selected 55 articles to review in depth. Most of these articles were retrospective case series describing the outcomes of ocular blast injuries that occurred during a specific terrorist event or military campaign.
BASICS OF BLAST INJURIES OF THE EYE
The mechanism of blast injuries traditionally has been divided into 4 categories: primary, secondary, tertiary, and quaternary. Primary blast injuries are the direct result of an intense overpressurization caused by a blast or shock wave generated by an explosion. Air-filled structures, such as the lungs, tympanic membranes, and gastrointestinal tract, are most susceptible to primary blast injuries. With a powerful-enough blast, however, any organ may be disrupted or destroyed. The intense overpressurization wave applies force to tissues that results in rapid deformation and disruption. The eye, with its protective orbit, tarsal plates, and tough sclera, is resistant to traumatic rupture, but given enough force, rupture can occur. Lesser force can result in internal ocular disruption. Secondary blast injuries are caused by flying debris or fragments accelerated by the energy of the explosion. Often exposed and unprotected, the head and eyes are particularly susceptible to secondary blast injuries. Rapidly accelerated sharp particles, large or small, can lacerate or rupture the cornea or sclera and enter the eye. Given the small and complex organizational structure of the eye, severe, sight-threatening damage can occur from secondary blast injuries. Tertiary blast injuries result from structural collapse and fragmentation of buildings or from a victim's body being displaced by the wind from explosions. Quaternary blast injuries refer to other explosion-related injuries, including chemical or thermal burns, toxic inhalation, radiation exposure, and asphyxiation.Reference DePalma, Burris, Champion and Hodgson3Reference Wightman and Gladish45Reference Pennardt and Lavonas6 Secondary and tertiary blast injuries constitute the predominant injuries among survivors of bombings. In general, damage produced by blast waves decreases exponentially with increasing distance from the point source of the blast.Reference DePalma, Burris, Champion and Hodgson3 In contrast to open-air bombings, which allow rapid dissipation of the shock, indoor detonations allow the blast wave to be magnified and result in higher morbidity and mortality rates.Reference Frykberg7
EPIDEMIOLOGY OF BLAST EYE INJURIES
Ocular injury is a frequent cause of morbidity in terrorist blast victims, both in military and civilian settings. The rate of eye injuries from terrorist bombings has ranged from 3% of blast survivors in the 1996 Manchester, UK, bombing to 28% of survivors from the 1998 terrorist bomb attack on the US embassy in Nairobi, Kenya.Reference Mines, Thach, Mallonee, Hildebrand and Shariat8Reference Odhiambo, Guthua, Macigo and Akama910Reference Carley and Mackway-Jones11 In the World Trade Center (WTC) disaster in 2001, ocular injuries were reported to be the second most common type of injury among survivors after inhalation injuries. Among 790 WTC survivors treated within 48 hours, 26% had ocular injuries, mostly attributed to smoke, dust, debris, or fumes.10
The number and types of injury vary, depending on the type of explosive, proximity to the blast, and the victim's environment. Epidemiological studies from blast explosions in modern buildings frequently cite glass as a major source of lacerations and foreign bodies affecting the eye. Blast explosions in buildings can also create foreign-body injuries from concrete, metal, wood, and other materials.Reference Thach, Ward, Hollifield, Cockerham, Birdsong and Kramer12 Blast explosions in open spaces, such as those from land mines, tend to accelerate metallic shrapnel from the bomb itself and soil and organic matter.
Ocular injuries occurring from terrorist blasts can be extensive and involve any blunt or penetrating trauma or blast-related injury to the tissues of the eye, orbit, or ocular adnexa. Frequently, injuries are bilateral, and multiple traumas involving the lids, globe, and orbit are noted. Blast-related eye injuries can range from minor corneal abrasions and foreign bodies to extensive eyelid lacerations, open globe injuries, intraocular foreign bodies, and fractured orbits. More serious eye injuries have been associated with close proximity to the blast and areas of heavy building damage. In the 1995 Oklahoma City bombing, 83% of open globe injuries were sustained by people who were inside the Alfred P. Murrah Federal Building at the time of the attack.Reference Mines, Thach, Mallonee, Hildebrand and Shariat8
Injuries associated with bomb blast victims can be closely compared to injuries sustained by soldiers and civilians during warfare. During Operation Desert Storm, eye injuries were reported to account for 13% of all injuries, and 78% of all serious eye injuries were caused by blast fragmentation from munitions.Reference Heier, Enzenauer, Wintermeyer, Delaney and LaPiana13Reference Mader, Aragones and Chandler14 Although glass window fragments cause the majority of injuries in terrorist bombings, most fragments in the military setting are due to munitions shells and debris from the ground. During the Iraqi insurgency in 2004, more than half of all injuries were caused by improvised explosive devices, which are loaded with metallic objects (eg, metallic ball bearings, nails) to inflict penetrating injuries in crowded civilian settings.Reference Mader, Carroll, Slade, George, Ritchey and Neville15
OPHTHALMIC INJURIES ASSOCIATED WITH BLAST INJURIES
Primary blast injuries to the eye can result in rupture of the globe, hyphema (bleeding in the eye), or other internal ocular disruption. Only 1 case of a pure primary blast injury of the eye has been reported in the literature: Recurrent hyphema and angle recession (damage to the glaucoma drainage inlet of the eye) was described in a patient as a result of a high-pressure wave blast injury alone, with no foreign body or blunt trauma to the eye.Reference Beiran and Miller16 A globe weakened by previous trauma or surgery may be at higher risk for damage from a primary blast injury. Dislocation of an intraocular lens resulting only from the concussive force of a blast has been observed at Walter Reed Army Medical Center in a patient with a history of open globe trauma and cataract extraction with intraocular lens placement.
Secondary blast injuries (ie, foreign bodies) cause the majority of eye injuries among blast victims. The eye is vulnerable to small fragments of glass, cement, or other debris that may be stopped by clothing or may minimally affect other parts of the body.Reference Thach, Ward, Hollifield, Cockerham, Birdsong and Kramer12 Small or large projectiles and fragments from the explosions can enter the eye and cause severe blunt or penetrating injuries.
Minor blast-related eye injuries include corneal abrasions, conjunctivitis, and superficial foreign bodies (Figure 1). Chemical conjunctivitis and corneal abrasions were the second most frequent cause of morbidity noted after the 2001 WTC disaster.Reference Feeney, Goldberg, Blumenthal and Wallack17 Following land mine blast injuries, which typically cause peppering of the eye and face with minute particles, up to 94% of eyes can be found with superficial foreign bodies in the lids, cornea, conjunctiva, and sclera (Figure 2).Reference Muzaffar, Khan, Akbar, Malik and Durrani18
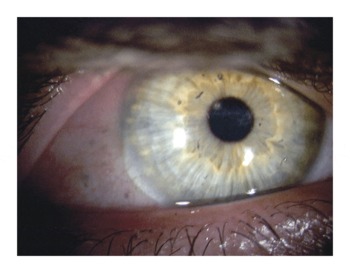
FIGURE 1 Slit lamp photograph of a patient with multiple corneal and conjunctival foreign bodies. “Tattooing” of the lids or cornea is common following blast injuries.

FIGURE 2 Facial sandblasting with multiple foreign bodies. Patient sustained multiple face and lid foreign bodies and bilateral intraocular foreign bodies following explosion of an improvised explosive device in Iraq.
Open globe injuries, including penetrating and perforating injuries to the cornea and/or sclera, are the most common serious blast-related eye injuries and occur in up to 20% to 50% of eyes.Reference Mines, Thach, Mallonee, Hildebrand and Shariat8Reference Odhiambo, Guthua, Macigo and Akama9Reference Thach, Ward, Hollifield, Cockerham, Birdsong and Kramer12Reference Muzaffar, Khan, Akbar, Malik and Durrani18 The incidence of intraocular foreign bodies (IOFBs) associated with penetrating or perforating injuries ranges from 4% in the Oklahoma City bombing to up to 30% to 65% of penetrating injuries encountered during warfare.Reference Mines, Thach, Mallonee, Hildebrand and Shariat8Reference Wong, Seet and Ang19 Retained IOFBs resulting from fragmentation injuries during war may be multiple or bilateral. IOFBs may be large and obvious or small and difficult to diagnose and may be located in any part of the eye (Figures 3 and 4). Between 80% and 90% of IOFBs are located in the posterior segment of the eye, and a significant number have associated complications of cataract, vitreous hemorrhage, or retinal detachment.

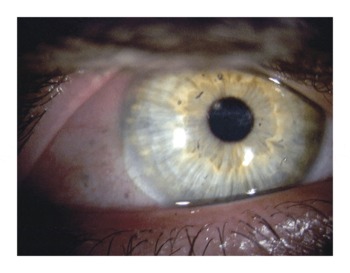
FIGURE 3 Ruptured globes may be subtle. Slit lamp photograph of a subtle penetrating corneal foreign body.

FIGURE 4 Ruptured globes may be obvious. Slit lamp photograph of a patient with a corneoscleral laceration from a glass intraocular foreign body.
Eyelid lacerations, which are often extensive, account for 20% to 60% of blast-related eye injuries.Reference Mines, Thach, Mallonee, Hildebrand and Shariat8Reference Odhiambo, Guthua, Macigo and Akama9Reference Muzaffar, Khan, Akbar, Malik and Durrani18 Orbital fractures, frequently accompanied by IOFBs and massive maxillofacial damage, occur in approximately 10% of ocular blast injuries (Figure 5).Reference Mines, Thach, Mallonee, Hildebrand and Shariat8 Serious nonpenetrating eye injuries include hyphema, traumatic cataract, vitreous hemorrhage, retinal detachment, choroidal rupture, and optic nerve injuries. Traumatic hyphema may be associated with blunt rupture of the globe.Reference Shingleton and Hersh20 The incidence of endophthalmitis (infection inside the eye) following penetrating injuries was reported to be 7.9% during the Vietnam war and 8.4% in a review of terror-related open globe injuries at a tertiary referral center in Turkey.Reference Wong, Seet and Ang19Reference Sobaci, Akyn, Mutlu, Karagul and Bayraktar21

FIGURE 5 Blast eye trauma often involves multiple trauma. Computed tomography scan of a large intraorbital foreign body with ethmoid sinus involvement.
POLYTRAUMA IN BLAST VICTIMS
Serious ocular injuries are commonly associated with other injuries, especially of the head and neck. Military surgical teams often consist of ophthalmologists, neurosurgeons, and otolaryngology surgeons who work as a team to repair the complex, traumatic head and neck injuries that frequently occur in blast-injured patients.Reference Mader, Aragones and Chandler14 Some concomitant blast injuries (especially in gas-containing organs such as the lungs, bowel, and ears) are serious but less dramatic than a severely disfiguring facial injury and can therefore be overlooked. Carrying out a trauma survey is critical to avoid missing these associated injuries.
CLINICAL PRESENTATION
Blast eye injuries can present with a wide range of symptoms, from minimal discomfort to severe pain or loss of vision. It is critical to appreciate that significant eye damage may be present despite normal vision and minimal symptoms. Symptoms can include eye irritation or pain, foreign body sensation, decreased or altered vision, bleeding, and periorbital swelling or bruising. Patients may present for care immediately or not until days or weeks after the event. Ocular injuries may present late because of the presence of multiple other injuries, diminished consciousness of the patient, or the silent nature of the eye injury.Reference Holmes, Coombes, Rice and Wilson22 On examination, patients with eye trauma may have considerable and obvious face, lid, or eye defects or more subtle injuries that although initially appearing limited, after careful examination, may be recognized as far more severe. Because serious ocular injuries may have subtle presentations, the examination of blast victims should be approached with a high level of suspicion for occult eye injuries and a low threshold for referral for ophthalmologic evaluation.
EARLY HOSPITAL TREATMENT
The Table summarizes the recommendations regarding the management of ocular blast injuries. The evidence supporting these recommendations consists primarily of current clinical practice patterns with relatively few strong evidence-based studies to guide management.
TABLE 1 Blast Eye Injuries: What Providers Need to Know

ED physicians treating blast injuries often are overwhelmed with the simultaneous arrival of many seriously injured patients. To maximize their effectiveness, the ED physician should keep the following simple concepts in mind:
1. First do no harm. Keep the eye covered and free from any pressure to avoid expulsion of intraocular contents in the presence of a ruptured globe. A convex metal or plastic shield is preferred. Patches should be avoided because of the pressure that they apply to the globe.
2. Obtain an objective measure of best visual acuity; this is the “vital sign” of the eye.
3. Initiate basic treatment in preparation for transfer to the ophthalmology service:
• Order computed tomography (CT) scans of brain/orbits, cervical spine, and chest and abdomen, as necessary.
• Prepare the patient for the operating room (laboratory tests, complete blood count, type and cross, urinalysis, coagulation studies, electrocardiogram, as necessary).
• Administer tetanus inoculation, as necessary.
• Administer intravenous antibiotics.Reference Colyer, Weber and Weichel23
• Administer antinausea medications.
• Administer analgesics; avoid narcotic analgesics until after obtaining informed consent from the patient for surgery.
Initial evaluation of the blast-injured patient requires a full-body, unclothed evaluation so that all injuries are detected promptly. Because ocular injuries often do not occur in isolation, it is important that an obvious, distracting injury, such as a bloody eyeball on a person's cheek, does not obscure a potentially fatal but less obvious associated injury such as blast lung injury. Taking a brief history can be helpful in understanding the circumstances of the site of the blast and the nature and composition of the shrapnel (copper and some bronze foreign bodies are particularly inflammatory to the eye). Any available witnesses to the injury should be interviewed if the patient is unable to provide a careful history. When possible, documentation should include details of the incident, time since the injury and treatment during that interval, medical and surgical histories, ocular history, tetanus status, and medication allergies.
A preliminary ocular examination should focus on searching for and treating ophthalmic emergencies, such as chemical burns, ruptured globes, or lid compartment syndromes. If a chemical burn of the eye is determined and there is no globe rupture, then irrigation with sterile saline should be initiated without delay. A comprehensive examination begins with an external inventory of the face and eyelids to determine the presence of foreign bodies or lacerations. The presence of a lid laceration, however insignificant, mandates careful exploration of the extent of the wound. Periorbital and lid ecchymosis, subcutaneous emphysema, hypoesthesia of the cheek, motility disturbance, and enophthalmos may indicate an underlying orbital fracture. The presence of particulate matter on the face or lids could be an indication of possible occult penetrating foreign bodies.
A careful assessment of visual acuity and a pupillary examination should be performed. An objective measure of visual acuity is important in the immediate and delayed decision-making process. Visual acuity should be tested 1 eye at a time, testing initially for the ability to count fingers. A near card or eye chart, if available, may be useful to document acuity in a patient who is able to count fingers. In patients who cannot count fingers, testing for perception of hand motion or light perception should be performed. No–light-perception vision is an indication of poor prognosis. An irregular pupillary response may indicate intracranial pathology, whereas a peaked or eccentric pupil could indicate intraocular damage or globe rupture with iris prolapse. An anterior segment examination is ideally performed by slit lamp biomicroscopy, but a handheld penlight examination can be effective. Diffuse subconjunctival hemorrhage or abnormal pigmentation of the conjunctiva may indicate globe rupture. Corneal abrasions or foreign bodies, hyphema, or traumatic cataracts may be detected with a careful penlight inspection. When a ruptured globe is obvious, for example, a flat globe or prolapse of intraocular contents, the examination should be abbreviated to avoid unnecessary manipulation of the eye. If a ruptured globe is suspected, then the examination should be performed without applying any pressure to the globe or orbit to avoid extrusion of intraocular contents.Reference Hamill25
A CT scan with thin cuts (1.0–1.5 mm) of the brain and orbits (axial and coronal views) should be obtained if there is concern about an orbital fracture or a retained intraocular foreign body. If wood, plastic, or organic foreign bodies are suspected and the CT scan does not show metallic foreign bodies, then magnetic resonance imaging may be useful for identifying nonmetallic foreign bodies. Plain films of the orbit are helpful if CT scanning or magnetic resonance imaging is unavailable.
It should be emphasized that no pressure should be applied to an eye suspected of harboring a rupture. If significant eyelid edema makes opening of the lids difficult, then the examination should be deferred. Zealous examination can result in extrusion of intraocular contents, making repair even more complicated. In the ED setting, objects penetrating the eye should not be removed. Instead, the eye can be covered with an eye shield or paper cup, which will not exert pressure on the globe.
After initial stabilization of the patient and protection of the eye, all serious blast eye injuries should be immediately referred to an ophthalmologist for definitive treatment. ED physicians should initiate basic treatment until ophthalmological support is available. Ruptured globes typically require urgent operative intervention, and preparing the patient for the operating room is essential. The goals should be to prevent further damage to the eye, reduce the risk of infection, and stabilize the patient for surgery.
Blast-injured patients with ruptured globes and unstable pulmonary or airway status may require endotracheal intubation. The use of succinylcholine during intubation in patients with ruptured globes has long been thought to be potentially harmful due to the theoretical risk of raising intraocular pressure and contraction of the rectus muscles. The data behind this assertion are largely anecdotal, and some eye centers in the United States routinely use succinylcholine without difficulty. In 1 study, pretreating 100 patients with a nondepolarizing agent before administering succinylcholine resulted in no extrusion of intraocular contents.Reference Vachon, Warner and Bacon24
DISPOSITION AND OUTCOME
Similar to eye injuries encountered during warfare, serious penetrating and nonpenetrating blast eye injuries have been associated with a poor visual prognosis. Because a tremendous amount of energy is imparted onto the globe by missiles and fragments, both penetrating and nonpenetrating blast injuries are associated with severe anterior and posterior segment damage. Ocular injuries produced by land mine blasts appear to be the most severe, with 37% of injured eyes becoming totally blind (no light perception) and 73% becoming legally blind (visual acuity ≤20/200). Bilateral eye injuries from land mine explosions have been noted in 78% of patients.Reference Muzaffar, Khan, Akbar, Malik and Durrani18 Improvised explosive devices have also been a major cause of significant vision loss, being responsible for 59% of all enucleations performed during the Iraqi insurgency.Reference Mader, Carroll, Slade, George, Ritchey and Neville15 Of all eye injuries during Operation Desert Storm, 18% resulted in enucleation, 94% of which were the result of munitions fragments.Reference Mader, Aragones and Chandler14
Certain aspects of the injured eye are associated with a poor prognosis: severe intraocular hemorrhage, prolapse of ocular contents, double perforating injuries, more extensive or posterior globe lacerations, and endophthalmitis. The 8% incidence of endophthalmitis previously reported following blast-related penetrating injuries is slightly higher than a normal endophthalmitis rate of 2% to 7% of all penetrating injuries.Reference Wong, Seet and Ang19Reference Sobaci, Akyn, Mutlu, Karagul and Bayraktar21 Modern improvements in diagnostic and surgical techniques as well as intravitreal antibiotic therapy, however, have resulted in a lower endophthalmitis rate. Recent published and unpublished data from Walter Reed Army Medical Center during Operations Iraqi Freedom and Enduring Freedom showed no cases of endophthalmitis in 160 eyes with open globe injuries with or without IOFBs.Reference Hamill25 Despite recent improvements in the incidence and treatment of endophthalmitis, the overall prognosis in traumatic endophthalmitis remains poor compared to that in cases occurring after intraocular surgery.Reference Levin and D'Amico26
Visual acuity at the time of presentation appears to be the single most important factor in predicting final visual acuity in patients with penetrating injuries, with no light perception vision being an indicator of poor prognosis.Reference Sternberg27 Timing of treatment is also crucial in determining prognosis. In a review of civilian eye injuries during warfare, victims who experienced more prolonged delays of treatment were determined to have a higher rate of complications and subsequent enucleations.Reference Khouri28 Significant improvements in diagnostic and surgical techniques during the past few decades have resulted in improved visual prognosis and a decreased rate of enucleation following ocular blast injuries. During the Algerian war (1957-1961), 26% of blast-injured eyes underwent enucleation, compared with 18% reported during the Persian Gulf war.Reference Mader, Aragones and Chandler14Reference Quere, Bouchat and Cornand29 Despite the notable decrease in enucleation rates, blast eye injuries remain a significant cause of vision loss worldwide. Although protective eyewear has been shown to be efficacious in decreasing the rates of eye trauma during wartime,Reference Wong, Smith, Lincoln and Tielsch30 many terrorist blasts, unfortunately, are targeted against unsuspecting and unprepared civilian victims.
SUMMARY
Ocular injury resulting from secondary blast injuries is a frequent cause of morbidity in terrorist blast victims. Serious eye injuries can present with subtle signs and symptoms. Management of the blast-injured patient should be approached with a high level of suspicion for occult eye or other associated injuries. The frequency of eye injuries after an explosion and the significant potential for severe vision loss make it imperative that injured survivors be examined by an ophthalmologist at the earliest opportunity.
Authors’ Disclosures: The authors report no conflicts of interest.