Introduction
Vestibular schwannomas, previously often referred to as acoustic neuromas, are rare benign tumours originating from the VIIIth cranial nerve, at the cerebellopontine angle. The presentation of vestibular schwannoma is varied; it often includes audio-vestibular symptoms of asymmetrical hearing loss (which can be of sudden onset), unilateral tinnitus or vertigo.Reference Gupta, Thakker and Gupta1 Neurological symptoms such as facial weakness or numbness can also be presenting features.Reference Gupta, Thakker and Gupta1 The incidence of vestibular schwannoma is variable across the literature, reported at rates of 1.04–1.4 per 100 000 population.Reference Evans, Moran, King, Saeed, Gurusinghe and Ramsden2–Reference Kshettry, Hsieh, Ostrom, Kruchko and Barnholtz-Sloan4 Vestibular schwannomas constitute about 85 per cent of cerebellopontine angle tumours.Reference Gupta, Thakker and Gupta1
Magnetic resonance imaging (MRI) of the internal auditory meatus (IAM) is the most common imaging requested for patients with audio-vestibular symptoms, performed with the intention of ruling out a vestibular schwannoma. The indications include unilateral or asymmetrical hearing impairment, tinnitus, progressive hearing loss, vertigo, facial nerve palsy, and cholesteatoma. With regard to hearing loss and tinnitus, the UK's National Institute for Health and Care Excellence (NICE) has produced guidelines recommending criteria for requesting MRI of the IAM.5,Reference Ftouh, Harrop-Griffiths, Harker, Munro and Leverton6 Audio-vestibular symptoms are relatively common, whereas vestibular schwannoma is relatively rare, even within the cohort of patients presenting with relevant symptoms. With MRI being one of the expensive imaging modalities, there is a significant financial burden associated with investigating common audio-vestibular symptoms in the hope of detecting a rare pathology. Hence, robust selection criteria for requesting an MRI of the IAM are important to streamline service and sustain cost-effectiveness, especially in the context of a stretched National Health Service.
The NICE guideline recommendations for investigation using MRI in adults with hearing loss are: (1) offer MRI of the IAM to adults with hearing loss, and localising symptoms or signs (such as facial nerve weakness) that might indicate a vestibular schwannoma or cerebellopontine angle lesion, irrespective of pure tone thresholds (NICE guideline (NG98) 1.3.1); and (2) consider MRI of the IAM for adults with sensorineural hearing loss and no localising signs if there is an asymmetry on pure tone audiometry of 15 dB or more at any two adjacent test frequencies, using test frequencies of 0.5, 1, 2, 4 and 8 kHz (NICE guideline (NG98) 1.3.2).5 We used unilateral or asymmetrical hearing loss, unilateral tinnitus, facial nerve weakness, numbness or pain, and unilateral hyperacusis as localising symptoms and/or signs as per the guidelines.
This study aimed to compare the local hospital compliance with NICE guidelines and other guidance in terms of the detection rate of vestibular schwannoma.
Materials and methods
We carried out a retrospective study in our hospital: to establish whether we are following the NICE guideline NG98, entitled ‘Hearing loss in adults: assessment and management’,5,Reference Ftouh, Harrop-Griffiths, Harker, Munro and Leverton6 published in 2018; and identify the rate of vestibular schwannoma detected from MRI of the IAM performed at the hospital.
Using data from the radiology department, MRI scans of the IAM requested between July 2017 and June 2019 were identified, and the clinical documentation leading to the request was reviewed. Ethical approval was not required because the study was performed as part of a service improvement project and signed off by the clinical governance, and patient-identifying information was not held. The total number of scans requested during this period was 1312. Included were all patients who underwent MRI of the IAM for audio-vestibular symptoms to exclude retro-cochlear pathology (n = 1300). Those patients who underwent MRI of the IAM for reasons other than audio-vestibular symptoms, such as stroke and cerebellar pathology, were excluded (n = 12).
The patients’ demographic details were analysed for gender and age. All indications for MRI and the pure tone audiograms of patients included were assessed. Scans that fit NICE guidelines and those that did not were separately analysed, with corresponding patient records.
A literature review was performed, and the Oxford guidelines, Northern guidelines, Charing Cross protocol and Nashville Otology Group protocol were compared to evaluate their relative utility in identifying appropriate cases for investigation by MRI.Reference Sheppard, Milford and Anslow7–Reference Welling, Glasscock, Woods and Jackson10
Results
Of the 1300 patients whose scans were included in the study, the male to female ratio was 1.26:1. The age ranged between 11 and 90 years, with the mean age being 56.4 years.
The indication for the scan request was scrutinised: 494 patients (34 per cent) had a primary complaint of unilateral hearing loss, 423 (29 per cent) complained of unilateral tinnitus, whilst 105 (7 per cent) had both tinnitus and unilateral hearing loss. The other indications were: vertigo (n = 163, 11 per cent, with vertigo as the primary complaint); vertigo with hearing loss or tinnitus (n = 60, 4 per cent); sudden-onset sensorineural hearing loss (n = 68, 5 per cent); and ‘other’ indications, such as facial palsy or pain, or cholesteatoma (n = 152, 10 per cent) (Figure 1).

Fig. 1. Indications for requesting magnetic resonance imaging of the internal auditory meatus for audio-vestibular causes. SNHL = sensorineural hearing loss
The scan results were normal in 95 per cent of the patients (n = 1235). Vestibular schwannoma was identified in 24 patients (1.8 per cent). Of these, 16 were newly diagnosed, whilst 8 had been diagnosed previously and the MRI requests had been performed for serial monitoring. Other pathologies were identified in 30 patients (2.3 per cent), including a vascular loop in 3 patients and ischaemia in 8 patients; it is unclear whether these findings explained the presenting symptoms.
The detection rate of new vestibular schwannoma was 1.23 per cent in our study. Scan requests for all 16 patients conformed to the NICE guidelines. We analysed the new positive scans and the indication for the MRI (Figure 2). Twelve patients with a scan positive for vestibular schwannoma had unilateral sensorineural hearing loss, two had sudden-onset hearing loss, one had unilateral tinnitus, one had facial nerve palsy and one had lateralising signs of facial pain. It is noteworthy that one patient fulfilled the criteria for unilateral sensorineural hearing loss but was found to have vestibular schwannoma of the contralateral ear; however, this was not considered an incidental finding, as the patient met the NICE criteria for an MRI.

Fig. 2. Clinical features of 16 magnetic resonance imaging scans positive for vestibular schwannoma. SNHL = sensorineural hearing loss
A total of 281 scan requests did not meet the NICE criteria, meaning that the compliance rate was 78.3 per cent. None of these scans showed any abnormal pathology. The main reason why the scan requests did not meet the criteria was mild sensorineural hearing loss that did not fit the specific hearing threshold levels stipulated by the NICE guidelines (n = 163, 58 per cent). Other conditions for which MRI of the IAM was inappropriately requested included: conductive hearing loss (n = 34, 12.1 per cent), Eustachian tube dysfunction (n = 12, 4.3 per cent), benign paroxysmal positional vertigo (n = 4, 1.4 per cent), bilateral tinnitus (n = 34, 12.1 per cent), and other conditions (n = 34, 12.1 per cent) such as mastoid and vascular pathologies (Table 1).
Table 1. Analysis of MRI scans not adhering to NICE guidelines

MRI = magnetic resonance imaging; NICE = National Institute for Health and Care Excellence; SNHL = sensorineural hearing loss; BPPV = benign paroxysmal positional vertigo
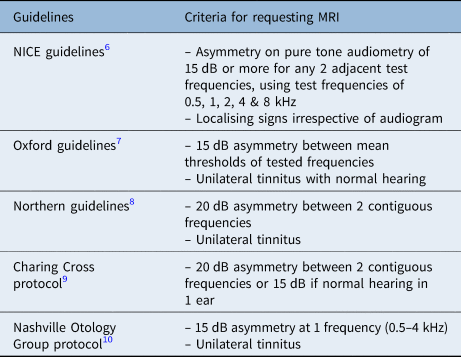
Whilst all patients with scans positive for vestibular schwannoma were picked up using NICE guidelines, up to three patients could have been missed using some of the alternative guidelines (which include the Oxford guidelines, Northern guidelines, Charing Cross protocol and Nashville Otology Group protocol). For instance, three cases might have been missed using the Oxford guidance, three cases by the Nashville Otology Group protocol, one by the Charing Cross protocol and two by the Northern guidelines. The criteria of these alternative guidelines are outlined in Table 2.
Table 2. Different guidelines currently used as criteria for requesting MRI of IAM
MRI = magnetic resonance imaging; IAM = internal auditory meatus; NICE = National Institute for Health and Care Excellence
Discussion
Vestibular schwannomas are diagnosed with different modalities of investigation; however, MRI of the IAM has become the primary modality of investigation, as it is non-invasive, with a sensitivity of 100 per cent and a specificity of 92 per cent.Reference Singh, Singh, Thukral, Rao, Singh and Singh11
There are currently multiple locally produced guidelines for requesting MRI of the IAM to exclude retro-cochlear pathology, including the Oxford guidelines, Northern guidelines, Charing Cross protocol and the Nashville Otology Group protocol.Reference Sheppard, Milford and Anslow7–Reference Welling, Glasscock, Woods and Jackson10 The NICE, as a national organisation, produced clear guidelines in 2018 for requesting MRI scans for audio-vestibular symptoms.5,Reference Ftouh, Harrop-Griffiths, Harker, Munro and Leverton6
To our knowledge, this is the first study to use the NICE guidance for MRI of the IAM selection criteria. In our work we have seen that within our population and practice, the NICE guidelines are suitable for detecting vestibular schwannoma. No underlying pathology was found in those patients who underwent MRI of the IAM without meeting the NICE criteria, further suggesting that the NICE guidelines are unlikely to miss a diagnosis of vestibular schwannoma.
The identification of incidental pathologies on MRI scans of IAM is well documented.Reference Mirza, Malik, Ahmed, Willatt and Hughes12 Our study found vascular loops, ischaemia and other incidental findings. One study reported a detection rate of 47.5 per cent for incidental pathologies,Reference Papanikolaou, Khan and Keogh13 of which a common finding was white matter lesions, which may be indicative of demyelinating disease. These incidental findings can result in patient anxiety and often require referral to other specialties, incurring further costs for the healthcare system. It is also often not clear whether these incidental findings have any relationship to the symptoms for which the MRI was requested.
Our oldest patient who underwent an MRI scan was 90 years old. The NICE guidelines do not state any age criteria for requesting MRI of the IAM in the investigation of audio-vestibular symptoms, but use of flexible terminology such as ‘consider MRI’5 in the guidelines allows clinicians some discretion. Previous studies have shown that elderly patients diagnosed with vestibular schwannoma have smaller tumours, which are now increasingly managed conservatively.Reference Basu, Youngs and Mitchell-Innes14 Some studies suggest that MRI of the IAM should not be recommended for this indication in those aged above 65–75 years, as initiation of interventional management is unlikely.Reference Basu, Youngs and Mitchell-Innes14,Reference Harcourt, Vijaya-Sekaran, Loney and Lennox15 In our study, the mean age of patients with a scan positive for vestibular schwannoma was 52 years; the youngest patient was aged 26 years and the eldest was 71 years.
Other studies have examined the conformity of local centres with other criteria,Reference Nash, Majithia and Singh16 outlined in Table 2, but no comparison of data has been performed with the NICE guidelines. When we analysed our data against the other criteria (Table 3),Reference Sheppard, Milford and Anslow7–Reference Welling, Glasscock, Woods and Jackson10 the negative likelihood ratio was 0.19 for the Oxford guidelines, 0.19 for the Northern guidelines, 0.06 for the Charing Cross protocol and 0.12 for the Nashville Otology Group protocol. It is noteworthy that a total of three patients would have been missed based on these alternative guidelines. One patient with a positive scan did not complain of hearing loss or tinnitus, but had facial pain and trigeminal neuralgia, with a mild sensorineural hearing impairment later revealed on audiogram. Therefore, this patient did fit the NICE criteria based on the unilateral localising symptoms. This might have been missed if the MRI request had been based purely on pure tone audiogram. Similarly, the other two patients would have had their diagnoses missed based on pure tone audiograms using the alternative guidelines.
Table 3. Comparison of data with other guidelines

Values in parentheses are 95 per cent confidence intervals. NICE = National Institute for Health and Care Excellence; PPV = positive predictive value; NPV = negative predictive value
Although NICE guidelines are developed using the processes of systematic review and meta-analysis, they have not been compared within patient populations, as other guidelines have been, to assess reliability. Our study shows sensitivity and specificity rates that are similar to those of the above-mentioned alternative guidelines, which have comparable detection rates.Reference Dawes, Mehta and Arullendran3 There is limited concordance between the various guidelines as to which criteria warrant referral for MRI of the IAM, so agreement on a single, suitable guideline would help clinicians and ensure a consistent standard of patient care.Reference Nash, Majithia and Singh16
Conclusion
The NICE guidelines have raised awareness of limiting requests for MRI. Our study has identified that more than 200 patients locally had an MRI of the IAM requested without fulfilling the NICE criteria. This has resulted in unnecessary costs, potentially increased patient anxiety, and the identification of incidental findings with associated additional costs to the healthcare system. However, no case of vestibular schwannoma has been missed, and our results are comparable to the guidance.
Whilst NICE guidelines are effective in ensuring that those with vestibular schwannoma are investigated appropriately, following the criteria even more closely will enable the detection of vestibular schwannoma without risk of missing this pathology, and at the same time reduce investigation costs. The local detection rate of vestibular schwannoma is similar to other guidelines.
Lastly, questions have been raised over the utility of diagnosing and monitoring vestibular schwannoma in elderly patients; such patients tend to have smaller and slower-growing tumours, and often do not undergo intervention.Reference Basu, Youngs and Mitchell-Innes14,Reference Harcourt, Vijaya-Sekaran, Loney and Lennox15 More advice from NICE regarding the suggestions around age criteria would further strengthen the indications for imaging.
Acknowledgement
The authors would like to thank the Department of ENT, Warwick Hospital, South Warwickshire NHS Foundation Trust, UK.
Competing interests
None declared







