Background
Problem Statement
While there are now multiple examples of qualitative and semi-quantitative assessments being used for some degree of predicting disaster-related health risk, few models express health risk in terms of the actual probability of health outcomes and uncertainty of evidence.Reference Tracie 1 This is particularly problematic since risk is defined as the probability that a specific outcome will occur. This absence of metrics related to chance and uncertainty limit the utility of most public health disaster risk assessments. This logically results in an acceptably accurate hazard identification and prioritization, but inaccurate and non-reproducible estimations of health-related impact. This lack of information then complicates the ability to prioritize and allocate health resources effectively, before and after the disaster.
Ideally, disaster risk management is based on a prioritization process. Once hazards have been identified, they are assessed in terms of the probability and impact in terms of losses. The hazards associated with the greatest probability and impact are prioritized. In addition to prioritization, risk assessment also offers a process for ongoing research involving the interaction of health determinants, risk, and protective factors that may contribute to future adverse health outcomes. Finally, risk assessment provides a framework for monitoring and evaluating the performance of interventions intended to reduce adverse health outcomes.
More recently, assessments of health risk have become an integral part of public health and medical emergency preparedness programs. 2 One of the strengths of these assessments lies in that these processes typically bring together multi-sectoral input for public health decision making and plans. However, this diversity of input also creates challenges in development of a standardized approach for assessment, as well as a common nomenclature for assessing and communicating the characteristics of this risk.
The utility of existing models for risk assessment is attenuated by challenges with both first- and second-order uncertainty. This uncertainty is often due to a lack of predictability (reflected in the standard deviation) and accuracy (reflected in the standard error) of results from these assessments. Most risk assessment tools currently being used by the public health and medical sectors lack predictive value that would guide accurate cost accounting necessary for large-scale resource allocation or investment. Some apply risk-based models that offer indices derived from semi-quantitative estimation of select disaster risk components (namely hazards, vulnerability, and capacity). Other models offer retrospective analysis of the association between disaster incidence and select risk factors (eg, social vulnerability and capacity).Reference Tracie 1 , Reference Cutter, Boruff and Shirley 3 - 5
However, to date, risk assessments do not yet offer accurate quantification of exposure as a risk factor for disaster-related adverse health outcomes. To date, none are validated as predictive of quantifiable health risk. As a result, a relatively wide variety of semi-quantitative risk assessments are being performed in various locations throughout the US and the world. Measures in many of these assessments are estimated subjectively and indicators are often sufficiently ambiguous so as to limit the reproducibility of the assessment over time or among users. Few include quantifiable representations of uncertainty.Reference Tracie 1
Clear definitions of terminology are essential to the performance of a logical and evidence-based risk assessment. Lack of a standardized nomenclature and approach has the potential to increase variation in the accuracy and reproducibility of the assessment (resulting in a second-order uncertainty).
Perhaps part of the justification for the current level of acceptance of these tools (known to be associated with relatively high degree of uncertainty) may stem from the currently limited applications of disaster risk assessments themselves. Typically, disaster risk assessments are performed in order to gain a prioritized list of hazards before writing a plan that includes an all-hazard approach to preparedness and response. Thus, much of the value and time spent in prioritization of the risk is lost when this level of specificity is not necessarily needed for plans involving risk acceptance, which is largely comprised of general emergency response functions, which are not hazard specific. On the contrary, disaster risk management programs that include risk reduction measures require hazard-specific risk prioritization in order to evaluate cost effectiveness of risk reduction measures being considered. Accuracy and validity of the risk assessment are therefore of key importance for guiding the effectiveness of disaster risk management practice and policy.
These challenges in understanding disaster-related risk assessment have also narrowed scientific progress on risk assessment, in general. In absence of measurable indicators, risk assessments are not monitored and evaluated for quality. There are few linkages between the development of risk assessment methodology and subsequent epidemiological validation or other measures of effectiveness.
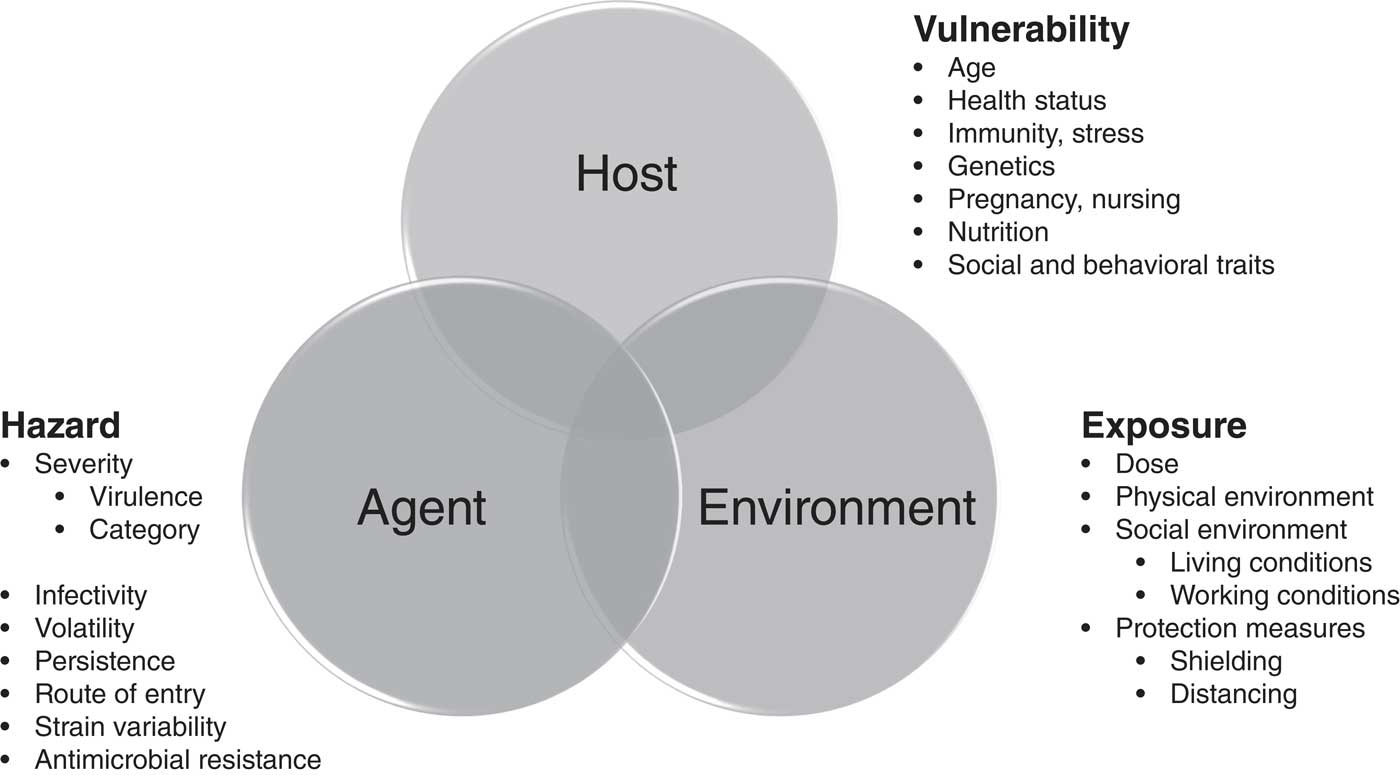
For the past decade, most disaster health studies have extensively investigated those risk factors associated with human vulnerability, while very few epidemiological studies include the widely-recognized influences of capacity and exposure in disaster risk. Epidemiological assessments of disaster-related health risk associated with environmental disasters have also typically under-reported key risk factors related to the environment and agent (exposure and hazard), while focusing almost entirely on characteristics of the host (vulnerability). Figure 1 6 , 7 illustrates how disease is caused by a complex interaction between the person (host), the disease agent (hazard), and the environment (exposure).
There remains a need for a reproducible, well-validated, disaster-related health risk assessment process that is suitable for accommodating the current gaps in certainty. The purpose of this report is to offer a practical framework and nomenclature for assessing disaster-related health risk that is: (1) accurate; (2) based upon historical evidence; (3) quantifiable in public health terms; and (4) inclusive of uncertainty. 7
Overview of Risk Assessment
Risk
In simplest terms, risk is the probability that an outcome will occur. This outcome may be beneficial or adverse. This relationship may be represented as:
Risk is the effect of uncertainty on outcomes. 7 , Reference Wharton 8 Uncertainty is a state or condition that involves a deficiency of information and leads to inadequate or incomplete knowledge or understanding. Uncertainty exists whenever the knowledge or understanding of an event, consequence, or likelihood is inadequate or incomplete. Expressions of risk therefore include estimations of uncertainty:
Impact
In general terms, risk is conceptualized as the probability of events and the severity of outcomes (consequences) that would arise if the events take place. The severity of consequences (usually conceptualized as losses) is frequently described in terms of impact. Correspondingly, the United Nations International Strategy for Disaster Reduction (Geneva, Switzerland) defines impact as “the degree of severity associated with … consequences….”Reference Keim 9 Thus, the term “consequence” is not synonymous with “impact.” Consequence is a qualitative description of the loss, while impact is a quantitative measure of that loss.
Risk Assessment
Risk is assessed as a function of the probability that an adverse event (referred to as a hazard) and its resultant impact will occur during a given timeframe. This relationship is commonly described as follows in what is commonly referred to as the “risk equation:”Reference Keim 10
where, R= risk; H=hazard incidence; and I=degree of impact.
The process for risk assessment is described in Figure 2 and Table 1.

Figure 2 Schematic Overview of Disaster Risk Management Process. 6
Hazard Analysis
Hazard analysis typically involves: identification of those hazards to which the population may potentially become exposed; then identifying the frequency of these hazards; and finally, characterizing the adverse health effects that may result from exposure to the hazard. 11 - 13
Impact Analysis
Impact analysis seeks to quantify the degree of losses (eg, disease) that may be expected when a vulnerable population is exposed to a hazard. Impact analysis typically involves: a determination of those critical assets to be protected (in this case, it is the health and safety of the population), and then an assessment of potential losses among these assets. 11 - 13
For health (as a critical asset of the population), these potential losses include disaster-related morbidity and mortality. Impact analysis therefore includes an assessment of those risk factors which are known to influence disaster-related health outcomes: namely exposures, vulnerability, and capacity.
Exposure Assessment
The first step of impact analysis is to estimate the degree of hazard exposure that the population may be expected to receive over the time in question. 11 - 13 Exposures are assessed for each of the hazards identified in the hazard analysis. Exposures are assessed in terms of dose, which is a representation of the relative magnitude of the hazard and its contact rate for the population over time.
When data are available, the hazard analysis includes a hazard characterization step intended to present quantitative information in terms of dose-response relationship (the relationship between hazard dose and health response). The probability of exposures is estimated through dose reconstruction and dose-response modeling of many physical and biological hazards. It now appears possible to accomplish the same for natural and human-induced disaster hazards.
Vulnerability Assessment
Host-related factors of the target human population can influence susceptibility to the particular hazard, taking into account host intrinsic and acquired traits that modify the likelihood of contracting disease (susceptibility) and the likelihood of complications (severity). Vulnerability assessments identify those (inherent and acquired) risk and protective factors known to influence health outcomes, given exposure to disaster hazard has occurred. Susceptibility is expressed as the slope of the dose-response curve. Severity of physiological response (eg, disease) is correspondingly expressed as a peak value on the x-axis of the dose-response curve.
Vulnerability to the same hazard may differ widely among individuals within the same population. For example, people that have been immunized are much less susceptible to the same degree of exposures to viruses as compared to those who have not been immunized. And when disease does occur, some individuals in the population (eg, elderly or immunocompromised persons) are more likely to suffer a more-severe course of illness, resulting in a higher degree of impairment, disability, or even death.
Capacity Assessment
Capacity is defined as “the combination of all the strengths, attributes, and resources available in a community, society, or organization that can be used to minimize [adverse outcomes] following exposure to a hazard.”Reference Keim 9 Capacity is therefore considered as a measure of resources available to accomplish an objective. Populations apply individual, household, community, and societal capacity to reduce risk at every of possible stage of intervention (eg, avoidance, reduction, transfer, and acceptance). Capacity is quite complex and assessments commonly include economic, material, behavioral, and sociopolitical resources for reducing disaster risk.
Capacity assessments are most commonly represented as an asset inventory (ie, number of meals, amount of water, and number of tents). However, this application recognizes only the resources of the population. Such inventories do not take into consideration the strengths and attributes that are also necessary in order to operate efficiently and effectively achieve the intended outcome over time.
Capacity is expressed as the rate of outputs over time (ie, number of meals delivered per day; liters of water delivered per person - per day; or number of tents erected per day). Thus, the maximum capacity of the population represents a rate limiting step for reducing disaster impact.
Capacity assessments identify those resources (eg, capabilities with corresponding capacities) that are required to reduce the incidence of disease for each of the hazards. The process is as follows:
∙ Capability inventory - identify those capabilities that are required to reduce disease incidence;
∙ Expected capacity - estimate the expected capacity for each capability in the event of disaster;
∙ Current capacity - estimate the current capacity of the population to reduce disease incidence; and
∙ Gap analysis - analyze the gap between expected and current capacity to identify mismatches.
Capacity is applied in order to treat risk at all stages of risk management. Capacity assessment should include evaluations of capacity to be implemented before, during, and after the disaster event.
Table 2 14 provides examples of capabilities that can be applied for managing health risk from environmental (eg, hydro-meteorological, seismic, and technological), societal, and biological disaster hazards.
Table 2 Examples of Societal Capabilities for Prevention of Disaster-Related Mortality 14 Abbreviations: PPE, personal protective equipment; WASH, water, sanitation, and hygiene.

Risk Characterization
Risk characterization involves the integration of the four factors of hazard, exposure, vulnerability, and capacity to obtain a single estimate of risk. This risk is then estimated for the adverse health events of morbidity and mortality for disease directly related to the hazard exposure. Risk may also be characterized for population displacement (a significant risk factor for disaster-related disease).
Perhaps the best developed set of risk data is that available for estimating hazard incidence. Expectedly, the accuracy and validity are relatively high for predictions of commonly-occurring hazards and, of course, less so for the more-rare hazards. Unfortunately, to date, there are very little data available regarding exposure to health hazards during a disaster event. It is possible to evaluate population exposures from historical data (especially those which are collected prospectively for the purpose of improving future risk analyses for predictably recurrent events that are more static and reproducible [eg, mass gatherings–like the Hajj pilgrimage]).
There are also little historical data available that are truly predictive of population vulnerabilities as well as those corresponding capacities necessary to reduce disaster-related health risk. Vulnerability may be extrapolated to some extent by comparing risk factors for population vulnerability associated with historical disaster-related outcomes. Capacities, or proxies thereof, may also be compared to historical values. However, first-order and second-order uncertainty remain relatively high for most public health and medical assessments of disaster-related vulnerability and capacity.
On the contrary, disaster-related health risk may also be forecasted from information directly obtained from historical data (especially for short-term extrapolations).
For calculations involving the coming year, a simple statistical analysis may be applied (in most cases) to estimate disaster-related health risk according to a framework that describes the probability of both hazards and specific health risks (Box 1).
Box 1: Steps for a Simple Calculation of Disaster-Related Health Risk and Uncertainty

Simple calculations of central tendency and variance readily produce this information within an actionable framework that relates both scale of the problem and degree of uncertainty for key policy and decision makers. There is, of course, also the potential to improve accuracy and perhaps validity of these annual projections by way of advanced analyses, such as logistical regression and Monte Carlo simulation based upon historical data for both hazards and associated health risk.
Each estimate of disaster-related health risk includes a requisite statistical probability of a specific health outcome and the relative degree of uncertainty regarding this conclusion. Here is an example based upon 50 years of actual historical data of a real country. During 2017, the mean flood-related health risk for the population of “Nation X” is predicted to occur in the form of two declared disasters (SD=1) that are expected to cause: an annual morbidity of 74 (SD=88); an annual mortality of 140 (SD=227); and an expected annual displacement of 19,215 (SD=43,780) persons. Data used for these calculations are readily available at the national and international level.Reference Keim, Abrahams and Castilla-Echenique 15 Using this information alone, conclusions may be drawn regarding the relative risk and the need for national intervention. Considering this information (even though the degree of uncertainty is high), it can be reasonably concluded that the relatively small numbers of morbidity and mortality could easily be managed according to the absorptive capacity of the country. However, in the case of displacement, there is the potential for over 60,000 persons displaced (as a mean, not the worst-case scenario). This scale of displacement would very likely require national intervention and therefore should be considered.
Risk may also be used to prioritize interventions according to the health impact. For example, one hypothetical risk assessment might identify the following disaster-related health risk for a population:
∙ Earthquake–1.0% probability of 1,000,000 deaths (SD=5,000 deaths)=10,000 (SD=5,000) deaths;
∙ Flood–10.0% probability of 1,000 deaths (SD=500 deaths)=100 (SD=500) deaths; or
∙ Plane Crash–0.01% probability of 200 deaths (SD=25 deaths)=0.02 (SD=25) deaths.
Countermeasure Determination
Once hazards have been identified and prioritized according to potential health risk, countermeasures are then identified that will manage (or treat) the risk for each hazard.Reference Keim 12
Table 2 provides examples of countermeasures that may be applied to reduce disaster-related health risk through hazard avoidance, exposure reduction, and vulnerability reduction. These potential countermeasures should be planned to a level of operational detail sufficient for accurate cost accounting. This is then compared to predictions of cost-benefit. When data and resources are available, countermeasure determination should also be considered as a course of action analysis (eg, a range of options [from “doing nothing” to “doing everything”] intended for subsequent use by decision makers). Thus, for every countermeasure there is an evaluation of the associated cost (eg, $USD) and expected benefit in terms of reducing disaster-related adverse health events (eg, morbidity and mortality rates). Finally, there is the final cost-benefit analysis that not only includes economic considerations, but also includes value judgment involving the tolerability of risk according to social, cultural, political, and national security concerns. This is especially important considering these judgements include the value of health, disability, and life-years lost. For this reason, an accurate risk assessment is important for informing a strategy for risk communication that includes public iteration of these value-based decisions.
Risk Communication
Once cost-effective countermeasures have been identified, these measures must be concisely communicated to decision makers. Messaging includes: the character of the disaster-related health risks; the countermeasures that may be deployed to reduce risks; the cost-benefit ratio of proposed countermeasures; and finally, the degree of uncertainty associated with the assessment.
The risk communication should also take into consideration the target audience of the intended messaging. In most cases, the target audience may include public officials and decision makers involved in program allocations or project funding. These briefings may therefore be more tailored to considerations of policy and process. In other instances, the target audience may be the general public. In this case, messaging may therefore be more directed towards risk awareness and population protection measures.
A Logical Framework for Assessing Disaster-Related Health Risk
Risk assessment provides a logical framework of deduction intended to:
∙ Predict disaster-related morbidity and mortality;
∙ Identify countermeasures that will reduce health risk;
∙ Compare the costs and benefits of countermeasures; and
∙ Communicate the risks and benefits to a target audience.
Table 3 outlines a logical framework for risk assessment performed for two pathways, according to availability historical data. Both pathways result in an estimation of disaster-related health risk in terms of the predicted number of cases. The primary pathway depends upon historical disaster-related health data. However, in cases where historical data may be unavailable, health impact must be alternately estimated as a function of exposure, vulnerability, and capacity. This secondary pathway is therefore less likely to be predictive of outcome and offers a lower degree of reproducibility as compared to the primary pathway.
Table 3 Logical Framework and Steps for Assessing Disaster-Related Health Risk

Limitations
Primary Pathway - When Historical Data are Available
The primary pathway of this logical framework draws from historical data to calculate a reproducible representation of the evidence regarding disaster-related health risk, according to documented events. However, this model (like others currently available) has not been validated by empirical study as truly predictive of disaster-related health risk. That is not to say that such a study would not be feasible (as is the case for some other methods). This modeling of predicted health-related outcomes can be readily calculated from historical trends and then compared with real outcomes over time. The results may then be objectively compared for predictability.
This process represents a quantifiable means for prioritizing various disaster hazards according to potential health impact along with at least some measure of associated uncertainty regarding this risk. Although the degree of uncertainty is relatively high (especially for low-incidence events), it is at least objectively measured and reported in the analysis. Albeit relatively uncertain compared to the hard sciences, these data do represent standardized health risk indicators associated with a measurable degree of predictability and reproducibility (as compared to other methods that lack measurable accuracy and validity).
Secondary Pathway - When Historical Data are Not Available
The secondary pathway of the framework is intended for use when historical data are not available. This pathway offers a process that, at present, may be reasonably considered to result in a relatively high degree of variability for both reproducibility and predictive value. However, the resultant information from this pathway, though derived from non-historical estimates, is presented as standardized health indicators, specifically disease incidence. This format does allow for representation of specific and measurable disaster-related health risks and is suitable for aggregation of data and cross-comparisons estimation of resource allocation and planning purposes.
Like all such analyses, neither pathway of this framework sufficiently addresses the phenomenon of novel or extremely rare events (the so-called “Black Swan”–“when we don’t know what we don’t know”). In this case, historical data are obviously insufficient. In addition, consensus-based decision making is poorly predictive when the subject matter experts have limited prior experience with the event being forecasted. There are no such models currently available that have been validated to accurately predict disaster-related health risk for these rare events.
There are also cases when trends regarding the nature of the hazard may be changing in a manner that is more rapid and/or extensive as compared to the past. In this case, rapidly changing risks (eg, extreme weather events due to climate change or stages within a pandemic) necessitate frequent updates of when there exists a rapidly changing hazard profile.
Conclusion
Current approaches for assessing disaster-related health risk face significant challenges with first-order and second-order uncertainty. Lack of a standardized nomenclature and metric for assessing disaster-related health risk has contributed to a lack of accuracy and reproducibility among many such assessments. An absence of empirical data regarding disaster-related risk and protective factors, such as exposures, vulnerability, and capacity, has resulted in a lack of validity and predictability among assessments that rely upon these factors.
However, in many cases, accurate estimations of disaster-related health risk may be calculated directly from historical data. These evidence-based outcomes may be expressed in terms of rates for morbidity and mortality. This information may then be used to estimate the cost effectiveness of capacity that is necessary to effectively treat the risk, thus reducing disaster-related morbidity and mortality.