Introduction
The ageing cohort of the world population is expected to increase at an unprecedented rate from approximately 8.5 per cent (617 million people) in 2015 to a projected 17 per cent (1.6 billion people) in 2050 (Stewart Williams et al., Reference Stewart Williams, Kowal, Hestekin, O'Driscoll, Peltzer, Yawson and Chatterji2015). Accidental falls are the leading cause of injury-related deaths among older adults of 65 years and older (LeCuyer et al., Reference LeCuyer, Lockwood and Locklin2016) and therefore of grave concern to all health-care practitioners and policy makers. Unsurprisingly, falls are one of the five so-called ‘geriatric giants’, along with dementia, poor mobility, incontinence and polypharmacy (Cumming, Reference Cumming2013). Internationally, it is estimated that a third of community-dwelling older people may experience accidental falls every year and among these fallers, 35.5 per cent may experience recurrent falls (Hung et al., Reference Hung, Wang, Tang, Chen, Peng, Hsiao and Chen2017). According to the Centers for Disease Control and Prevention, more than 2.7 million older adults are injured annually from falls in the United States of America (Homer et al., Reference Homer, Palmer, Fox, Armstrong and Mandl2017).
Older adults show a higher incidence and prevalence of falling and they also experience more severe complications after falls (Flaherty and Josephson, Reference Flaherty and Josephson2013), including medical, psychological and personal consequences. Medical consequences can be severe and include osteoporotic fractures, head injuries, impaired mobility, traumatic brain or head injury, increased risk of future falls, abrasions, lacerations, contusions and functional decline (Calys et al., Reference Calys, Gagnon and Jernigan2013; Flarity et al., Reference Flarity, Pate and Finch2013; Wildes et al., Reference Wildes, Dua, Fowler, Miller, Carpenter, Avidan and Stark2015; Callisaya et al., Reference Callisaya, Blizzard, Martin and Srikanth2016; Deschamps et al., Reference Deschamps, Le Goff, Berrut, Cornu and Mignardot2016; Dueñas et al., Reference Dueñas, Balasch i Bernat, Mena del Horno, Aguilar-Rodríguez and Alcántara2016; Gu and Dennis, Reference Gu and Dennis2016; Kenny et al., Reference Kenny, Romero-Ortuno and Kumar2016; Romli et al., Reference Romli, Tan, Mackenzie, Lovarini, Suttanon and Clemson2017). The personal and psychological consequences of falls can be just as debilitating as the medical and physical consequences, and they do not only affect the older adult who falls, but also the immediate family and/or care-givers. Some of these consequences, as described in the literature, include fear of falling, depression, loss of independence, reduced quality of life, reduced participation in physical and social activities, immobility, early admission to nursing homes, difficulty with activities of daily living, dependency on others, social isolation, anxiety, loneliness, loss of confidence, loss of self-efficacy and decreased self-esteem (Ma et al., Reference Ma, Evans, Bertmar and Krause2014; Callisaya et al., Reference Callisaya, Blizzard, Martin and Srikanth2016; Deschamps et al., Reference Deschamps, Le Goff, Berrut, Cornu and Mignardot2016; Dueñas et al., Reference Dueñas, Balasch i Bernat, Mena del Horno, Aguilar-Rodríguez and Alcántara2016; Greenberg et al., Reference Greenberg, Sommers, Chittams and Cacchione2016; Kenny et al., Reference Kenny, Romero-Ortuno and Kumar2016; Narayanan et al., Reference Narayanan, Dickinson, Victor, Griffiths and Humphrey2016; Palumbo et al., Reference Palumbo, Klenk, Cattelani, Bandinelli, Ferrucci, Rapp, Chiari and Rothenbacher2016; Phelan et al., Reference Phelan, Mahoney, Voit and Stevens2015; Romli et al., Reference Romli, Tan, Mackenzie, Lovarini, Suttanon and Clemson2017). Other consequences of falls in older adults include financial and environmental factors such as hospitalisation, early admission to nursing homes, adaptation of the home environment, socio-economic burden on both the health-care system and the patients’ relatives and prolonged rehabilitation (Da Costa et al., Reference Da Costa, Rutjes, Mendy, Freund-Heritage and Vieira2012; Phelan et al., Reference Phelan, Mahoney, Voit and Stevens2015; Callisaya et al., Reference Callisaya, Blizzard, Martin and Srikanth2016; Dueñas et al., Reference Dueñas, Balasch i Bernat, Mena del Horno, Aguilar-Rodríguez and Alcántara2016). Although age is one risk factor for falls, many other risk factors exist that could increase the likelihood that a person will fall (Phelan et al., Reference Phelan, Mahoney, Voit and Stevens2015), such as gait or balance disorders, dizziness, postural hypotension or environmental-related factors (Rubenstein, Reference Rubenstein2006). Some falls may be prevented if an older adult's risk of falling is identified before their first fall, and this can be done using one of several fall risk assessment tools (FRATs).
An older adult's risk of falling could be identified more effectively if a universal, standard language for measuring fall risk in the ageing population was available. The International Classification of Functioning, Disability and Health (ICF), which was endorsed by the World Health Organization in 2001, views functioning and disability as outcomes of interactions between the health condition (in this case, falls) and the contextual factors (in this case, fall risk factors), which include both personal and environmental risk factors (World Health Organization, 2002). The ICF aims to code a person's functioning and disability based on four categories, namely (a) body function; (b) body structure; (c) activities and participation; and (d) environmental and personal factors (Figure 1).
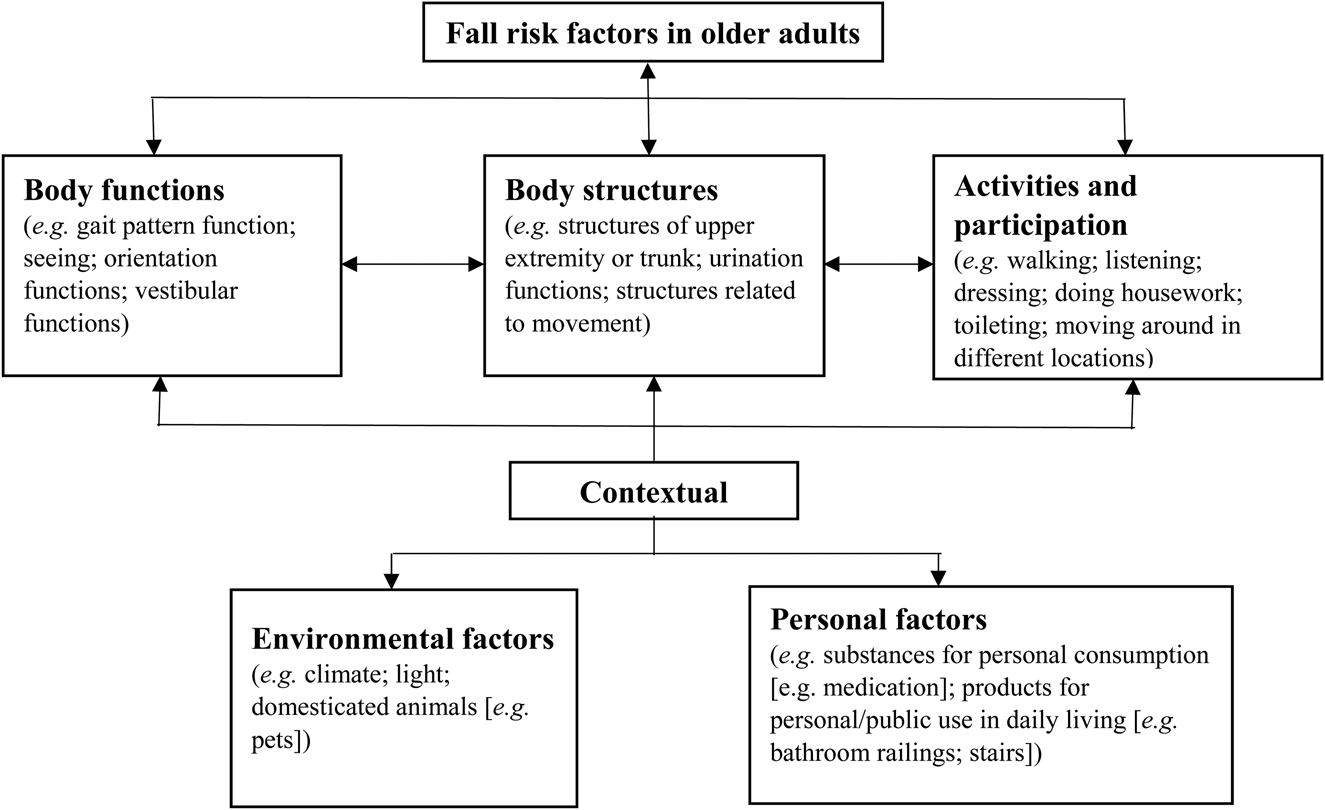
Figure 1. Fall risk factors in older adults in relation to the International Classification of Functioning, Disability and Health (ICF).
Source: Based on the ICF model (World Health Organization, 2002).
The ICF presents a scientific basis for understanding fall risk factors in older adults and provides a holistic model and universal language for health-care practitioners around the world to describe and classify falls and fall risk in older adults (World Health Organization, 2002). Since the ICF transcends professional boundaries across countries, it allows for clear interaction between professionals from different disciplinary backgrounds. It also enables them to discuss falls and fall risk factors without fear of miscommunication or bias due to selective, professional focus – thus increasing the possibility of early identification of fall risk in these individuals. The ICF is a systematic coding system for documenting health information, not simply about fall risk as a condition, but also for explaining how falls can affect the older adult in all aspects of life. It outlines the role of the environment and personal factors, and so allows health-care professionals to obtain a snapshot of the older adult's present health status (Granberg, Reference Granberg2015). Currently, most FRATs do not describe fall risk in terms of the ICF and there is a lack of information about fall risk assessment and the ICF, especially in community-dwelling older adults (Noohu et al., Reference Noohu, Dey, Sharma and Hussain2017). Identifying fall risk factors in current FRATs may be one way to link fall risk assessment to the ICF and gain all the advantages of using the ICF as a model for discussing fall risk in older adults.
The overall aim of this systematic review was to provide an analysis of existing mechanisms and measures for evaluating fall risk in older adults. The specific objectives were (a) to identify factors that had been utilised to quantify fall risk in older adults by means of a FRAT; (b) to map the content of the identified measures (i.e. the fall risk factors) to ICF codes using the ICF linking rules; and (c) to compare the weighted focus of the FRATs items in relation to the body (body function and structure), the individual and society (activities and participation) and the impact of the environment on the individual (environmental and personal factors).
Method
A systematic review based on the five stages suggested by Arksey and O'Malley (Reference Arksey and O'Malley2005) was conducted, and suggestions by Adair et al. (Reference Adair, Ullenhag, Rosenbaum, Granlund, Keen and Imms2018) were followed, who specifically aimed to identify measures and make recommendations for quality assessment. In Stage 1, the research question was identified and articulated as the aim of the review. In Stage 2, the search strategy that was followed involved identifying relevant studies and setting specific search parameters, such as the time and language of the articles. Stage 3 was the study selection which, for a systematic review, was articulated as the inclusion and exclusion criteria. During Stage 4, the data were charted using a customised data extraction sheet. Stage 5 involved collating, summarising and reporting the results as set out in the Results and Discussion section of this paper. The overall PRISMA methodology was included as this is an evidence-based minimum set of items for reporting in systematic reviews and meta-analysis (Moher et al., Reference Moher, Liberati, Tetzlaff and Altman2009).
Search strategy and selection criteria
The structured database search included nine databases and platforms (WorldCat; Medline; PaperFirst; ScienceDirect; SA ePublications and Journal Collection; BioOne; JSTOR Health and General Sciences Collection; JSTOR Life Sciences Collection). The primary purpose was to compile a comprehensive list of published papers on fall risk assessment tools from the literature. The search terms used were ti:(fall*) AND ti:(risk) AND ti:(assess*) AND ti:(tool*). No restriction in respect of date was placed on the search and all articles mentioning the keyword in the title were included in the initial set of results. Articles that had been published in languages other than English were excluded, due to the cost and time involved in translating such material.
Article screening and data extraction
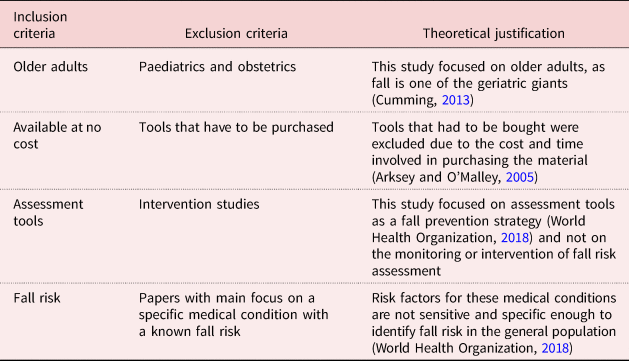
The first author (HdC) performed the initial database search and screened the titles for potentially relevant articles. After screening the titles, the articles were exported to Rayyan, a Web-based systematic review program that allows different reviewers to work on the same project simultaneously and determine the agreement percentage between reviewers (Ouzzani et al., Reference Ouzzani, Hammady, Fedorowicz and Elmagarmid2016). The first and second authors (HdC and AN) then independently screened all the identified potential articles at title and abstract level, using the inclusion and exclusion criteria (Table 1). Any discrepancies related to the inclusion of articles were resolved through discussion, and if consensus could not be reached, the third author (JB) was available to review the article. All three reviewers are dually qualified as speech-language therapists and audiologists, and each has at least ten years’ clinical experience.
Table 1. Inclusion and exclusion criteria
A customised data extraction sheet was compiled to enable consistent and independent data reporting for the search. Data extraction included the article date, author and the names of the FRATs discussed in the article. Data extraction was completed by HdC and AN, and no discrepancies were noted at this level.
Thereafter, two sets of criteria were used for including FRATs in the factor-mapping process. First, the FRAT had to be available at no cost, it had to be named and it had to have a supporting reference in the articles identified in this review to allow it to be located. Second, only those FRATs reported in at least one of the articles identified in the review were included. It is possible that previous researchers frequently chose only ‘popular’ FRATs for assessing fall risk when designing a study, but for this review, we aimed to include all mentioned FRATs, even if the FRAT was mentioned in only one of the articles identified in the search. Thus, our data were not limited to frequently used FRATs only. Two reviewers (HdC and AN) independently reviewed 102 studies for inclusion and excluded 35 studies. Of the 143 articles identified in the initial database search, 125 were subjected to title-level screening, 111 were evaluated on abstract level and 102 articles were evaluated for inclusion on full-text level. Of the latter 102 articles, 67 were eventually included in the data extraction process where a total of 49 tools were identified and 43 tools were included in the results (Figure 2).
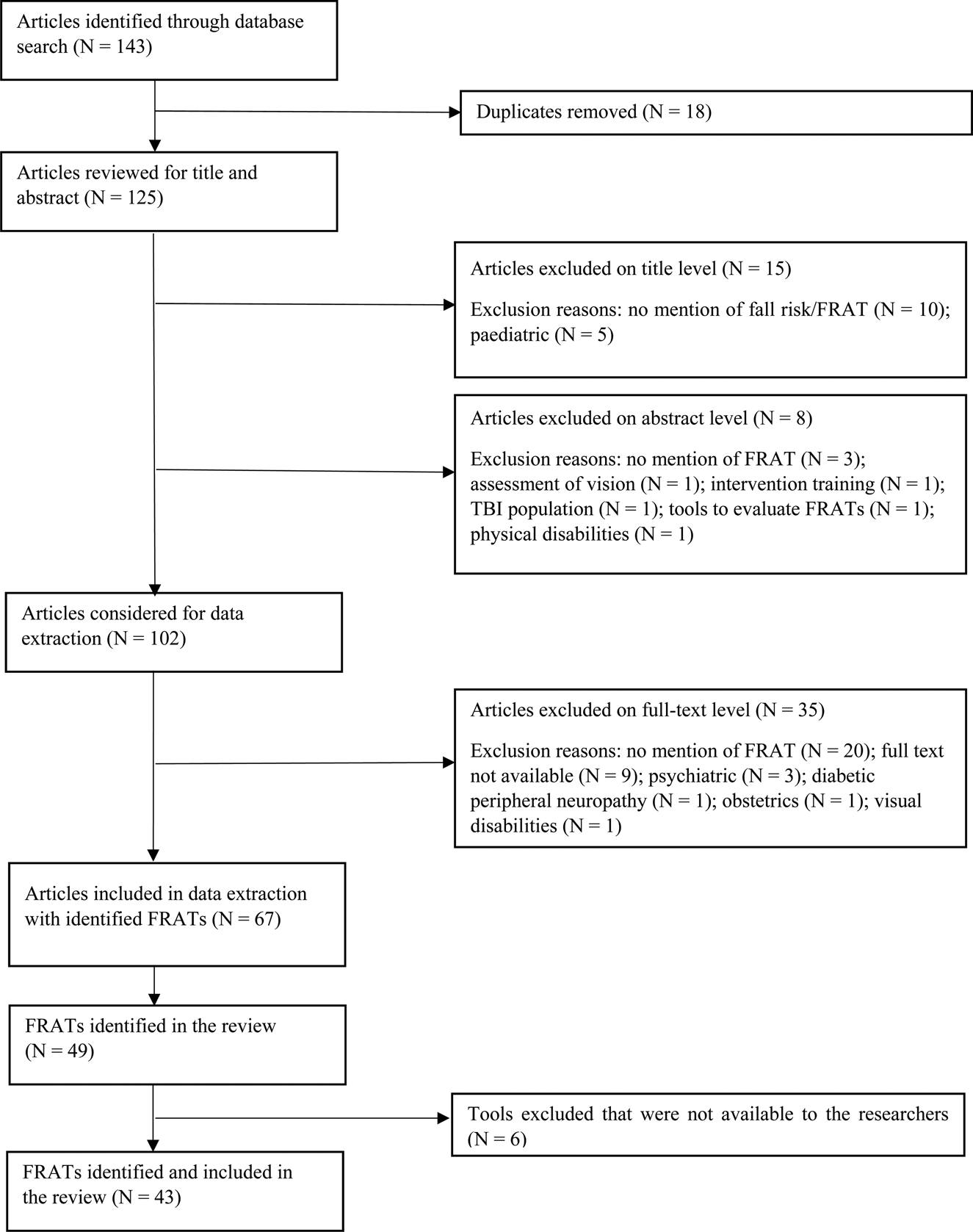
Figure 2. Graphic representation of the methodological process.
Notes: FRATs: fall risk assessment tools. TBI: traumatic brain injury.
Quality assessment
Our systematic review did not aim to summarise the effectiveness of assessment tools, the risk of bias of studies or the quality of the methodology used to design the FRATs (Adair et al., Reference Adair, Ullenhag, Rosenbaum, Granlund, Keen and Imms2018). Given our focus on the identification of FRATs, no formal assessments of methodological quality or risk of bias of the included articles were performed.
Data analysis
The 67 studies included in the review were independently evaluated by two reviewers (HdC and AN) and a 100 per cent agreement score was obtained by these two reviewers. A total of 49 FRATs were identified to be included in the review. Of the 49 tools identified, six were excluded as the researchers were unable to obtain them (Jester et al., Reference Jester, Wade and Henderson2005; Vassallo et al., Reference Vassallo, Stockdale, Sharma, Briggs and Allen2005; Young et al., Reference Young, Liaw and Sulaiman2005; Scott et al., Reference Scott, Votova, Scanlan and Close2007; Hirase et al., Reference Hirase, Inokuchi, Matsusaka, Nakahara and Okita2014; Miyakoshi et al., Reference Miyakoshi, Nasu, Takahashi and Natsume2014), despite contacting the corresponding authors of each article in which the tools were mentioned. The 43 FRATs included in the review were analysed by the first author (HdC) and the items in each tool were identified and extracted via Microsoft® Office Excel. All the tools were independently evaluated by all three reviewers (HdC, AN and JB) and an initial agreement of 92 per cent was established. After discussion of the discrepancies, the reviewers fully agreed on the ICF codes to which each item in the FRATs had been linked, using the ICF linking rules.
Items were linked to corresponding ICF categories by using the ten ICF rules for linking the relevant health information included in instruments and tools to the corresponding ICF categories (Selb et al., Reference Selb, Escorpizo, Kostanjsek, Stucki, Ustun and Cieza2015; Cieza et al., Reference Cieza, Fayed, Bickenbach and Prodinger2016). The first seven linking rules were applied in this study: Rule 1 – acquiring good knowledge of the conceptual fundamentals of the ICF; Rule 2 – identifying the main concept of each item to be linked to the ICF; Rule 3 – identifying additional concepts for each item if needed; Rule 4 – considering the popular perspectives for each identified concept when collecting health-related information; Rule 5 – identifying and document the categorisation of the response options; Rule 6 – linking all meaningful concepts to the precise ICF category; and Rule 7 – using ‘other specific’ or ‘unspecified’ ICD categories as appropriate. Rules 8–10 are only used when a specific code is not available on the third or fourth ICF level. For the purposes of this review, a two-level ICF classification was sufficient (Rules 1– 7) and further classification was not required at the time. All three reviewers independently linked the identified FRAT factors to the corresponding ICF categories. The weighted focus of the FRAT items in relation to the ICF categories was calculated using the confidence intervals to determine the p-values.
Results
On completion of the data extraction, a summary was made of the 43 FRATs included in the review, based on the included 67 articles (see Table 2). These 43 FRATs were categorised according to where their focus lay with regards to the four ICF categories, namely the body (where body function and structure codes are grouped together), the level of the individual (activities and participation) and the impact of the environment on the individual (environmental and personal factors).
Table 2. Summary of included fall risk assessment tools (FRATs) presented in alphabetical order

Notes: N = 67 articles. ICF: International Classification of Functioning, Disability and Health. BF&S: body function and structure. A&P: activities and participation. E&P: environmental and personal factors. 1. The main focus is indicated in bold.
As depicted in Table 2, a total of 43 FRATs were identified. The five FRATs mentioned most often in the review were the Stratify (N = 17), Morse Fall Scale (N = 15), Timed Up and Go (N = 13), Hendrich II Fall Risk Assessment Tool (N = 13) and the Tinetti Balance Assessment Tool (N = 10). Nine tools were mentioned three to eight times, namely the Berg Balance Scale (N = 9), Downton Index (N = 8), Johns Hopkins Fall Risk Assessment Tool (N = 7), Conley Scale (N = 6), Mobility Interaction Fall Chart (N = 6), Functional Reach (N = 5), Dynamic Gait Index (N = 4), FROP-Com (N = 4) and the Melbourne Fall Risk Assessment Tool (N = 3). Eight other FRATs were only mentioned twice, while 21 FRATs (49%) were mentioned only once in the review. A total of 18 tools – developed between 1986 and 1999 – were mentioned in 70 per cent of the articles being reviewed, whereas the 25 tools developed between 2000 and 2018 were mentioned in only 30 per cent of the articles in this review.
Of all 43 FRATs, 39 (91%) focused mainly on the body (body function and structure), while only one tool (LASA Fall Risk Profile) focused mainly on activities and participation (56%). Another tool (Marianjoy FRAT) focused equally (46%) on body function and structure and on activities and participation; the MAHC-10 focused mainly on environmental and personal factors (47%); and the Thai FRAT focused equally (40%) on body function and structure as well as on environmental and personal factors.
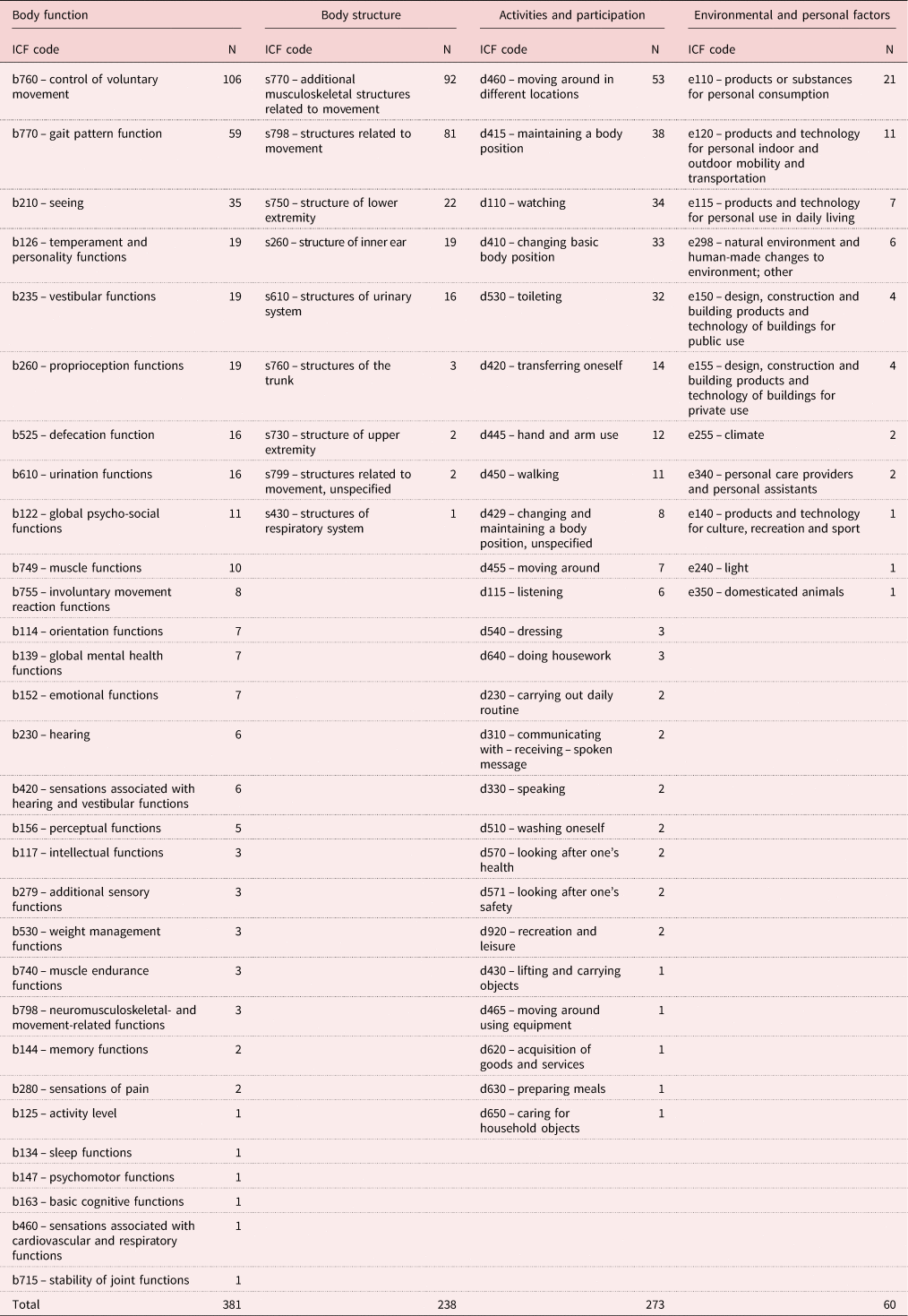
The items included in each of the 43 FRATs were extracted and linked to the ICF codes using the ICF linking rules (Cieza et al., Reference Cieza, Fayed, Bickenbach and Prodinger2016). Each item was categorised based on body function, body structure, activities and participation, and environmental and personal factors. The 43 FRATs produced a total of 493 FRAT items, which were linked to a total of 952 ICF codes (summarised as shown in Table 3).
Table 3. Summary of International Classification of Functioning, Disability and Health (ICF) codes linked to included fall risk assessment tools
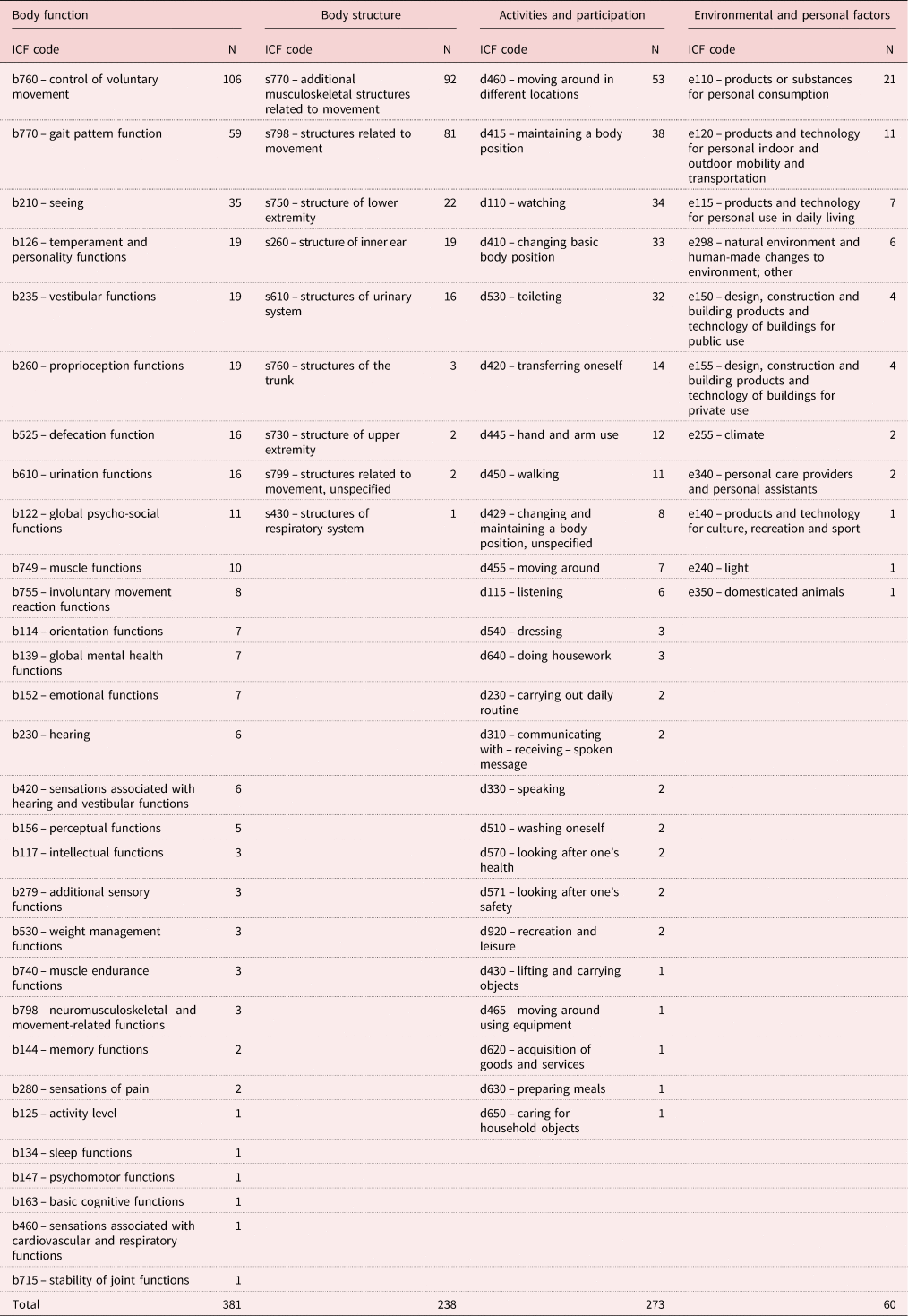
Table 3 depicts the ICF codes extracted from the included FRATs, arranged from most used codes to least used codes. The domain with the most used codes was body function with 381 of the 952 codes used (40%), followed by activities and participation with 273 codes (28%), body structure with 238 codes (25%) and, lastly, environmental and personal factors with only 60 codes (7%). As the body functions and structures are interlinked and both relate to the body, their codes were summed, which resulted in 619 codes and accounted for 65 per cent of the codes identified in the review. The differences between the statistical significance of these groups were calculated to determine the weighted focus of the FRAT items in each ICF category (Table 4).
Table 4. Statistical differences between groups

Note: CI: confidence interval.
Based on these values, a statistically significant p-value of p < 0.0001 and a 95 per cent confidence interval of the difference were reported among all three groups (Table 4), namely body function and structure (N = 619) compared to activities and participation (N = 273); activities and participation (N = 273) compared to environmental and personal factors (N = 60); and body function and structure (N = 619) compared to environmental and personal factors (N = 60) (Altman, Reference Altman1991).
Discussion
In this review, the overall aim was to provide an analysis of existing mechanisms and measures for evaluating fall risk in older adults. We identified the factors in FRATs that are currently available in the literature and mapped these fall risk factors to the ICF. Results indicated that the majority of the linked factors focused on the domain of the body (body function and structure), followed by the activities and participation domain and lastly on the environmental factors. All but four FRATs focused mainly on the body, indicating that ‘the body’ is regarded as the point of failure and of risk in most currently available FRATs.
However, contemporary research is emerging to show that other factors – factors outside the body, such as environmental factors, present immediately prior to and during falls – could hold as much, if not more, significant risks (Klenk et al., Reference Klenk, Becker, Palumbo, Schwickert, Rapp, Helbostad and Kerse2017). In-depth knowledge of falls in older adults therefore needs further development to consider environmental fall risk factors adequately. A recent study by Noohu et al. (Reference Noohu, Dey, Sharma and Hussain2017) agreed with this notion and mentioned that the strongest predictor of a single fall is limitations in both the activities and participation and in the environmental domain, whereas multiple falls are best predicted with limitations in the activities and participation domain. This emphasises the fact that more emphasis needs to be placed on factors other than those related to the body, such as environmental factors and limitations surrounding an individual's ability to perform activities and participate in life situations.
Based on the results of this review and the strong focus on the body as the main contributor to falls in older adults, almost all freely available FRATs which focus on the medical factors and model of assessment neglect considering the contributions of the biopsychosocial model of assessment. Viewing dysfunction through the narrow focus of the medical model (which is strictly concerned with organic dysfunctions) can easily translate to health-care professionals being concerned only with the physical aspects of disease (Farre and Rapley, Reference Farre and Rapley2017), which is translated as ‘the body’ in the ICF. This can place a limitation on the conceptual thinking about assessing fall risk in older adults as it obscures the fact that fall risk assessment in older adults is a collaboration between health-care professionals and older adults, and not just a medical procedure (Légaré et al., Reference Légaré, Adekpedjou, Stacey, Turcotte, Kryworuchko, Graham and Donner-Banzhoff2018). Health-care professionals could address the older adults’ needs more comprehensively by assessing all areas in their lives that could contribute to and increase their risk of falling. Otherwise, by focusing purely on the medical or body aspects when discussing fall risk in older adults, the assessment and intervention process can easily become restrictive as the medical model for intervention is inadequate (Jensen, Reference Jensen2006). Although a need for further research to address problems in implementing a biopsychosocial model to assessment and intervention remains, changes could be facilitated by bringing evidence-based research to health-care professionals on the needs of specific populations (Farre and Rapley, Reference Farre and Rapley2017), such as older adults with a risk of falling.
By shifting the focus away from cause towards impact – such as the impact of the limitations in older adults’ ability to participate in life situations and engage in activities – all health conditions are placed on an equal footing and allowed to be compared using a common metric, the ruler of health and disability (World Health Organization, 2002). When fall risk in older adults is assessed through the lens of the impact of the condition on the individual, older adults are viewed holistically by also considering the activities in which they participate and the environment in which these activities take place. Hence, the ICF highlights the value of including not only activities and participation, but also the impact of environmental and personal factors on a person's abilities in the assessment of health, thereby reiterating that the focus of FRATs should also move towards including these factors. Our results indicated that of the 22 FRATs developed after 2001, all but three FRATs still focused mainly on the body. By neglecting to focus on the individual and environmental levels when assessing fall risk in older adults, important factors, such as quality of life, participation in activities, housing, family caring and even access to health-care services, could be omitted in the older adult's intervention plan.
We found that only a minimal number of codes representative of the environmental influence of fall risk were represented in the FRATs. Within this small number of environmental codes, the majority of these codes were linked to the use of medication. So even when the effects of personal and environmental factors on fall risk is mentioned, the impact of the medical model is still prevalent in the significant number of codes mentioning medication. This could also be because a vast amount of research has been done on the topic of fall risk and medication use. By moving away from the medical model, towards a biopsychosocial model, even our knowledge of the environmental and personal effect of falls on older adults could be enhanced. A major part of existing literature focuses on risk factors in isolation (Ek, Reference Ek2019), ignoring possible interactions that other factors could have on older adults’ fall risk. As risk factors seem to cluster within older adults, it is suggested that both the clinical and research focus of assessing fall risk in older adults should focus more on the whole risk profile of the individual as well as on the effect of cumulative risk, rather than on isolated, medical risk factors (Ek, Reference Ek2019).
This begs the question of whether activities and participation, as well as environmental and personal influences, do not perhaps play a bigger role in increased risk of falling than is currently addressed by available FRATs. The medical focus of the most popular tools used could also discourage health-care professionals from adopting a more biopsychosocial model as they continue to use – on a regular basis – FRATs focused on the medical model. This could be because health-care professionals see the available and validated FRATs as reliable and do not feel the need to search beyond these factors. Health-care professionals should be able and ready to evaluate all factors contributing to a condition, not only the ones they are used to, and also not just the factors supporting a biological or organic cause of the condition (Farre and Rapley, Reference Farre and Rapley2017). By moving away from a medical model and towards a biopsychosocial model such as the ICF, it is during intervention possible to evaluate and consider the effects of fall risk on activities and participation in older adults, as well as the contributing environmental and personal factors.
One way of moving the discourse around environmental and personal factors on fall risk assessment forward could be to capture the perspectives and views of the older adults themselves about their perceptions on their own risk of falling in a qualitative research study on how fall risk assessment in older adults could be improved. As falls and fall risk is a multi-dimensional construct, particularly in older adults, a comprehensive ICF-based FRAT, that not only reflects a medical perspective (with a focus on the body), but that also captures older adults’ perceptions and views about individual factors (related to activities and participation), as well as the influence of the environment, could lead to a more holistic assessment and intervention focus in future.
Limitations of this review
This review did not include all the FRATs identified in the search, as some tools (N = 6) were not available to the researchers. It also did not include only standardised tests, but all FRATs – regardless of normative data. Many of the included FRATs (N = 29) were only mentioned in one or two of the included studies, which may have influenced the data extraction. No computer-based FRATs were included, which may have resulted in some FRATs, such as the Aachen fall prevention app (Pape et al., Reference Pape, Schemmann, Foerster and Knobe2015), not being included in our review. Only FRATs aimed at the adult population were included in the review and all FRATs based on a specific medical condition (e.g. traumatic brain injury, physical disabilities, visual disabilities, diabetic peripheral neuropathy) were excluded.
Recommendations and conclusion
This review highlighted the fact that current FRATs focus on the body, neglecting environmental and personal factors and, to a lesser extent, activities and participation. This over-reliance on the body as the point of failure in fall risk assessment clearly highlights the need for gathering qualitative data, such as from focus group discussions with older adults, to capture the perspectives and views of the older adults themselves about the factors that increase their risk of falling and comparing these perspectives to the data gathered from published FRATs as described in this review.
Furthermore, fall risk assessment should be a multi-disciplinary approach and, as such, data from different disciplinary backgrounds should be collected to determine the factors related to fall risk as identified by each discipline that is involved in fall risk assessment of older adults. The FRATs identified in this review were mostly aimed at the hospital setting, whereas future research should include data for fall risk assessment among community-dwelling older adults, as more and more older adults choose to live in these contexts for a longer period of their lives. Future qualitative research could enhance our knowledge of the experiences of older adults with regard to fall risk and how to address older adults’ needs better. Insight into the perceptions of older adults relating to fall risk could expand the body of knowledge on falls, related injuries and preventive measures for both older adults and the professionals working with them (Gamage et al., Reference Gamage, Rathnayake and Alwis2018).
Acknowledgements
The financial assistance of the National Institute for the Humanities and Social Sciences (NIHSS), in collaboration with the South African Humanities Deans Association (SAHUDA), towards this research is hereby acknowledged. Opinions expressed and conclusions arrived at are those of the authors and are not necessarily to be attributed to the NIHSS and SAHUDA.
Author contributions
All three authors were equally involved in the production of the article and read the final manuscript.
Financial support
This work was supported by a scholarship from the National Institute for Humanities and Social Sciences (HdC).
Conflict of interest
The authors declare no conflicts of interest.