Atrial septal defects are the second most common type of CHD, making up 15% of all subtypes. Reference Liu, Chen and Zühlke1 They have a prevalence of around 1.4 per 1000, and this rate is rising due to improving detection rates. Reference Liu, Chen and Zühlke1
Closure is often required to control the physiological consequences of the shunt produced by the atrial septal defect. Reference Fraisse, Latchman and Sharma2 The two principal methods for atrial septal defect closure are either surgical closure or transcatheter closure with device implantation, Reference Fraisse, Latchman and Sharma2 the latter being the treatment technique most commonly used in the United Kingdom. Reference Farooqi, Stickley and Dhillon3 However, complex atrial septal defects (multiple defects, >38 mm diameter, deficient posteroinferior rim) are often referred for surgical closure. Reference Fraisse, Latchman and Sharma2
Literature has previously made comparisons between surgical and transcatheter closure, with the benefits of transcatheter closure often highlighted due to it being less invasive. Reference Kotowycz, Therrien and Ionescu-Ittu4 However, there is still a need for surgical closure due to variations in atrial septal defect anatomy making transcatheter repair unviable, particularly in those with large atrial septal defects and insufficient rims. Reference Fraisse, Latchman and Sharma2
In cohorts consisting of both adults and children, the literature makes few distinctions between results across the different age groups. Reference Kutty, Hazeem and Brown5,Reference Xu, Liu, Zhao and Qin6 However, these cohorts are important to differentiate for a number of reasons, as age can impact upon patient outcomes and management. Reference Saritas, Yucel, Demir, Demir, Erdem and Celebi7 This systematic review therefore aims to comprehensively examine current literature comparing clinical outcomes of transcatheter and surgical closure for atrial septal defects and perform a meta-analysis of results, which will be subdivided into cohorts of either adults or children.
Materials and methods
Literature search strategy and inclusion criteria
The preferred reporting items for systematic reviews and meta-analyses guidelines were utilised in order to perform this review. Reference Moher, Liberati, Tetzlaff and Altman8 Electronic databases used for searching included Embase, PubMed, Medline, and Scopus to identify all studies comparing transcatheter closure of atrial septal defects to surgical closure. Searches were conducted in August 2020. Search terms included “transcatheter,” “TCC,” “percutaneous,” “minimally invasive,” “endoscopic,” “surg*,” “conventional,” “open,” “ASD” and “atrial septal*.” Terms were combined with Boolean operators “AND” and “OR” and were searched for as keywords and Medical Subject Headings terms. Hand searching of reference lists was conducted to ensure that all relevant literature was identified. After initial articles were identified, titles and abstracts were screened using the selection criteria below.
Selection criteria
Articles were eligible if they reported clinical outcomes of transcatheter versus surgical closure of atrial septal defects; studies which looked at one type of intervention only were excluded. Randomised controlled trials and observational study types were eligible for inclusion. Other study types including case reports, narrative reviews, and consensus documents were excluded. We considered studies in the English language that were published from 2000 onwards.
Data extraction and quality assessment
Outcomes collected included the following: 30-day-mortality, residual atrial septal defects, hospital stay length, reintervention rates, and post-operative complications, for example, arrhythmias and pericardial effusions. An analysis of total complications was performed, where all reported complications were included. Additional variables collected included demographic and peri-operative characteristics, including atrial septal defect diameter. Studies were categorised into either the adult or paediatric groups based upon the mean age of the population included. If the mean age of patients was age less than 18 years old, the study was categorised as paediatric, and if the mean age was greater than 18 years old, the study was categorised as adult. The Newcastle–Ottawa scale was used to perform a qualitative assessment of studies included, see Supplementary Table 1.
Statistical analysis
All statistical analysis was done on review manager V.5.4.1 (Cochrane collaboration, Oxford, UK). Clinical outcomes were assessed with odds ratios and mean differences. Where the effect measure of odds ratio was used, the statistical method was Mantel−Haenszel, and the analysis model was random effects. Where the effect was measured with mean difference, the statistical method used was inverse variance with a random effects analysis model. Heterogeneity was assessed with X2 and I2 with a cut-off value of 40%. p-values of 0.05 or less were considered significant.
Results
Included studies
The preferred reporting items for systematic reviews and meta-analyses flow chart illustrates our search results (Fig 1). Reference Moher, Liberati, Tetzlaff and Altman8 Thirty-three studies were included in meta-analysis, all were observational, of which 22 were retrospective, 7 prospective, and 4 used retrospective and prospective methods. Characteristics of the included studies are described in Table 1.

Figure 1. PRISMA flow diagram demonstrating the literature search completed. PRISMA = preferred reporting items for systematic reviews and meta-analyses.
Table 1. Study characteristics

A = adults; ASD = atrial septal defect; Paeds=paediatrics; SD = standard deviation; PTC = percutaneous transcatheter closure; Surg = surgical.
Baseline characteristics and operative information
Table 2 summarises the baseline characteristics and operative information of patients included. The majority of atrial septal defects were secundum, except for two studies which included sinus venosus. Reference Schneeberger, Schaefer and Conradi31,Reference Bakar, Burns, Diamantouros, Sridhar, Kiaii and Chu32 Overall, atrial septal defect sizes were larger in the surgical groups across both the adult and paediatric cohorts, and this was statistically significant in the adult cohort, 95% confidence interval, mean difference 112.62 [46.41, 178.84], p = 0.0009.
Table 2. Baseline characteristics

ASD = atrial septal defect.
Procedure success and residual atrial septal defects
Post-operative data for adult and paediatric populations have been summarised in Tables 3 and 4. Twelve studies reported procedure success in adults, while 7 studies reported procedure success in paediatrics. The mean procedure success in adults, for the surgical and transcatheter group, was 99.8% and 87.46%, respectively. In adults, procedure success favoured surgery; odds ratio 4.40 (95% confidence interval 1.99–9.72) p = 0.0003, Figure 2a. The mean procedure success in paediatrics, for the surgical and transcatheter group, was 95.76 and 95.43%, respectively. In paediatrics, procedure success favours neither intervention method, odds ratio 0.96 (95% confidence interval 0.37–2.48) p = 0.94, Figure 2b.

Figure 2. Forest plots showing procedural success for adult ( a ) and paediatric ( b ) populations. The adult plot ( a ) favours a surgical approach. The paediatric plot ( b ) favours neither intervention method. CI = confidence interval; OR = odds ratio; PTC = transcatheter approach.
Table 3. Operative/post-operative characteristics – adult

ASD = atrial septal defect; PTC = percutaneous transcatheter closure.
Table 4. Operative/post-operative characteristics – paediatrics
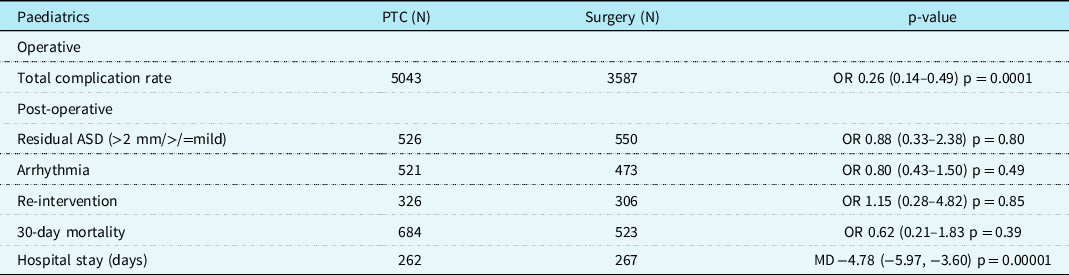
ASD = atrial septal defect; PTC = percutaneous transcatheter closure.
Twenty studies (12 adult and 8 paediatric) reported data on significant residual atrial septal defects. Atrial septal defects were considered significant if over 2 mm in diameter or classified as larger than “mild” on follow-up. In adults, there were less residual atrial septal defects in the surgical compared to the transcatheter cohort, with a mean number of residual atrial septal defects of 1.08 and 3, respectively (odds ratio 2.24 [95% confidence interval [1.16–4.32] p = 0.02). In the paediatric age group, there were no differences between the number of residual atrial septal defects reported in either the surgical or transcatheter cohorts.
Complications and mortality
Twenty-six studies (19 adult and 7 paediatric) reported mortality data, with both groups in both cohorts having a mean 30-day mortality of 1. There was no significant difference in 30-day mortality between the surgical and transcatheter groups in both the adult (surgical versus transcatheter; odds ratio 0.76, 95% confidence interval, [0.40, 1.45], p = 0.41) and paediatric cohorts (Surgical versus transcatheter; odds ratio 0.62, 95% confidence interval, [0.21, 1.83], p = 0.39).
Twenty-six studies (18 adult and 8 paediatric) reported arrhythmias as a complication. There were no significant differences in the number of arrhythmias reported between the surgical and transcatheter groups in the adult cohort (surgical versus transcatheter; odds ratio 0.84, 95% confidence interval, [0.44, 1.59], p < 0.58), Figure 3a. There was also no significant difference in the paediatric cohort (surgical versus transcatheter; odds ratio 0.80, 95% confidence interval, [0.43, 1.50], p = 0.49), Figure 3b.

Figure 3. Forest plots showing arrhythmias for adult ( a ) and paediatric ( b ) populations. The adult plot ( a ) favours a transcatheter approach. The paediatric plot ( b ) favours neither intervention method. CI = confidence interval; MH = Mantel–Haenszel; OR = odds ratio; PTC =transcatheter approach.
There was a significant difference in the total complications reported between the surgical and transcatheter groups in the adult cohort (surgical versus transcatheter; odds ratio 0.45, 95% confidence interval, [0.28, 0.72], p < 0.00001), Figure 4a. The mean total complication rate in the adult surgical and transcatheter groups was 24.32% and 12.47%, respectively. There was also a significant difference in the paediatric cohort (surgical versus transcatheter; odds ratio 0.26, 95% confidence interval, [0.14, 0.49], p < 0.00001), Figure 4b. The mean total complication rate in the paediatric surgical and transcatheter groups was 19.08 and 8.47, respectively.

Figure 4. Forest plots showing mortality for adult ( a ) and paediatric ( b ) populations. Both plots do not favour either the transcatheter or surgical approach. CI = confidence interval; MH = Mantel–Haenszel; OR = odds ratio; PTC = transcatheter approach.
Hospital stay
Ten studies reported total hospital stay in adults. Adult weighted mean total hospital stay was 5.6 days. This was found to be 4.2 days in the transcatheter group and 7.8 days in the surgical group in the adult cohort. Mean total hospital stay was significantly shorter in the transcatheter group, 95% confidence interval, mean difference −4.05 (−4.78, −3.32) p < 0.00001, Figure 5a. In the paediatric cohort, total hospital stay was reported in 4 studies with the weighted mean 2.6 days. This was 1.5 days in the transcatheter group and 4.2 days in the surgical group. Therefore, the mean total hospital stay was again significantly shorter in the transcatheter group, 95% confidence interval, mean difference −4.78 (−5.97, −3.60) p < 0.00001, Figure 5b.

Figure 5. Forest plots showing the mean total hospital stay for adult ( a ) and paediatric ( b ) populations. Both plots favour the transcatheter approach for ASD closure for this variable. CI = confidence interval; PTC = transcatheter approach.
Reintervention
Reintervention data were reported for 13 studies (9 adult and 4 paediatric). There was no significant difference between the surgical and transcatheter groups in both the adult (surgical versus transcatheter; odds ratio 0.42, 95% confidence interval, [0.09, 1.96], p = 0.27) and paediatric cohorts (surgical versus transcatheter; odds ratio 1.15, 95% confidence interval, [0.28, 4.82], p = 0.85).
Discussion
This systematic review and meta-analysis have compared key outcomes across both adult and paediatric populations undergoing transcatheter versus surgical atrial septal defect closure. The results have highlighted key advantages of transcatheter atrial septal defect closure, including reduced total hospital stay and a lower total complication rate across both cohorts, as well as demonstrating minimal or no significant advantages, including mortality and reintervention. This review has also highlighted important distinctions between outcomes in adult and paediatric populations; for procedural success, the surgical route was favoured in adult patients; however, in the paediatric cohort, neither technique proved superior, therefore, providing further insight into the most appropriate technique for each population group, which can be considered going forwards by performing clinicians.
Previous meta-analyses have reported findings not dissimilar to our own. We found that in both cohorts, surgical patients had larger atrial septal defects and experienced more complications and longer hospital stays than transcatheter patients, similar to findings by Butera et al and Mylonas et al. Reference Butera, Biondi-Zoccai and Sangiorgi9,Reference Mylonas, Ziogas and Evangeliou10 Mylonas et al Reference Mylonas, Ziogas and Evangeliou10 also found a higher treatment efficacy (99.8% versus 97.3%) and less residual shunts in the surgical compared to transcatheter group (0.95% versus 3.9%), similar to our results for the adult but not paediatric cohort. We found that transcatheter patients tend to be older than surgical patients in both the adult and paediatric cohorts; however, this finding is not consistently found in other literature. Reference Mylonas, Ziogas and Evangeliou10 This discrepancy may in part be due to differences in patient selection criteria depending on the type of surgical interventions included (e.g. minimally invasive).
Our results also showed that neither group experienced significantly different rates of arrhythmias. There is limited analysis in the literature; however, Vecht et al Reference Vecht, Saso and Rao11 found that both transcatheter and surgical closure resulted in a reduction in the prevalence of arrhythmias compared to pre-intervention in the short to medium term, transcatheter [odds ratio = 0.49 (95% confidence interval 0.32–0.76)] and surgical closure [odds ratio = 0.72 (95% confidence interval 0.60–0.87)].
In order to further the work completed within this study, more research comparing both treatment techniques in terms of cost-effectiveness would be beneficial. Studies without a focus on clinical outcomes were excluded from this review; however, studies such as those by Da Costa et al Reference Da Costa, Da Silva Santos, Sarti, Senna, Tura and Goulart12 suggest that percutaneous closure is more cost-effective than surgical closure. This is due to factors such as the lower chance of complications, shorter length of hospital stay and no requirement for extracorporeal circulation with transcatheter closure helping to compensate for the costs of the devices themselves.
This systematic review and meta-analysis is not without limitations. Firstly, the majority of the evidence appraised consisted of cohort studies, of which a significant proportion was retrospective; there were no randomised controlled trials included. This leads to the usual limitations associated with retrospective cohort studies, but of particular relevance to this analysis: susceptibility to confounding variables, bias in the selection and allocation process to each arm of the studies, and loss to follow-up.
Detail concerning the allocation of patients to each arm (surgical or percutaneous) was often somewhat lacking, and where it was included, the decision was often based on advanced clinical experience. Moreover, where crossover between the two arms occurred, there was not sufficient detail to factor in nor exclude such cases from our analysis. Therefore, this limits the degree to which the percutaneous and surgical approach of atrial septal defect repair can be compared. Some patients included in the surgical arm did not have the option of an interventional method for the atrial septal defect repair, either because these technical advances had not yet been developed or they were unsuitable for such an approach due to larger or more complex defects. One could argue this potentially impacts the rates of complications reported for each group; however, it is important to take into account the logistical and ethical implications of randomising this type of treatment and how it could be deemed an impossible task.
In conclusion, this systematic review and meta-analysis has been able to compare the outcomes of adult and paediatric populations undergoing transcatheter versus surgical atrial septal defect repair. This has demonstrated the overall benefits and drawbacks of both techniques but has highlighted, in line with previous findings, the advantages of transcatheter closure as having lower complication rates and length of hospital stay. However, there is still a continued role for surgical closure for larger or more complex atrial septal defects.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1047951121004583
Acknowledgements
None.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interest
None.












