Anomalous origin of a single coronary artery arising from the innominate artery associated with coronary artery fistula and truncus arteriosus is extremely rare. We report the successful surgical treatment of this anomaly in an infant in whom the morphology was found in the operation.
Case report
In May 2018, a 16-month-old infant-girl was charged in our hospital because of heart murmur. The chest radiogram showed cardiomegaly and prominent increased pulmonary vascularity. The electrocardiogram showed biventricular hypertrophy and q-wave in lead I, avL, V5, and V6. Our echocardiogram found truncus arteriosus (Type I, Collett and Edwards) with severe pulmonary hypertension, and the truncal valve had three leaflets with no stenosis or regurgitation. Pulmonary artery pressure was 69/51(60) mmHg, pulmonary vascular resistance was 12.87wood U/m2, and 65/50(60) mmHg, 3.49wood U/m2 after oxygen inhalation, respectively. Measurements were made by performing cardiac catheterization as the patient was older than 6 months. No significant surgical contraindications were found in the preoperative evaluation.
An operation was performed with the plan of the Rastelli procedure. However, after a median sternotomy, we found there was no coronary artery arising from the aorta, but a single artery arose from the innominate artery and branched into the left and right coronary arteries. The distribution was like that of either a right or a left normal coronary artery. The cardioplegia infusion needle was inserted in the innominate artery near the ostium of this single coronary artery, and the proximal and distal of the innominate artery was blocked during the cardioplegia infusion. (shown in Fig. 1) The aorta was cross-clamped and an infusion of HTK solution at 4°C was antegraded through the infusion needle. During the infusion, we found some HTK solution leaked from the ventricles. After the ascending aorta was transected, no coronary artery arose from the truncus, and we found a coronary fistula below the non-coronary aortic sinus, which is an uncommon anomalous communication between the coronary artery and left ventricle. After the fistula closed, the cardiac arrest was obtained successful.
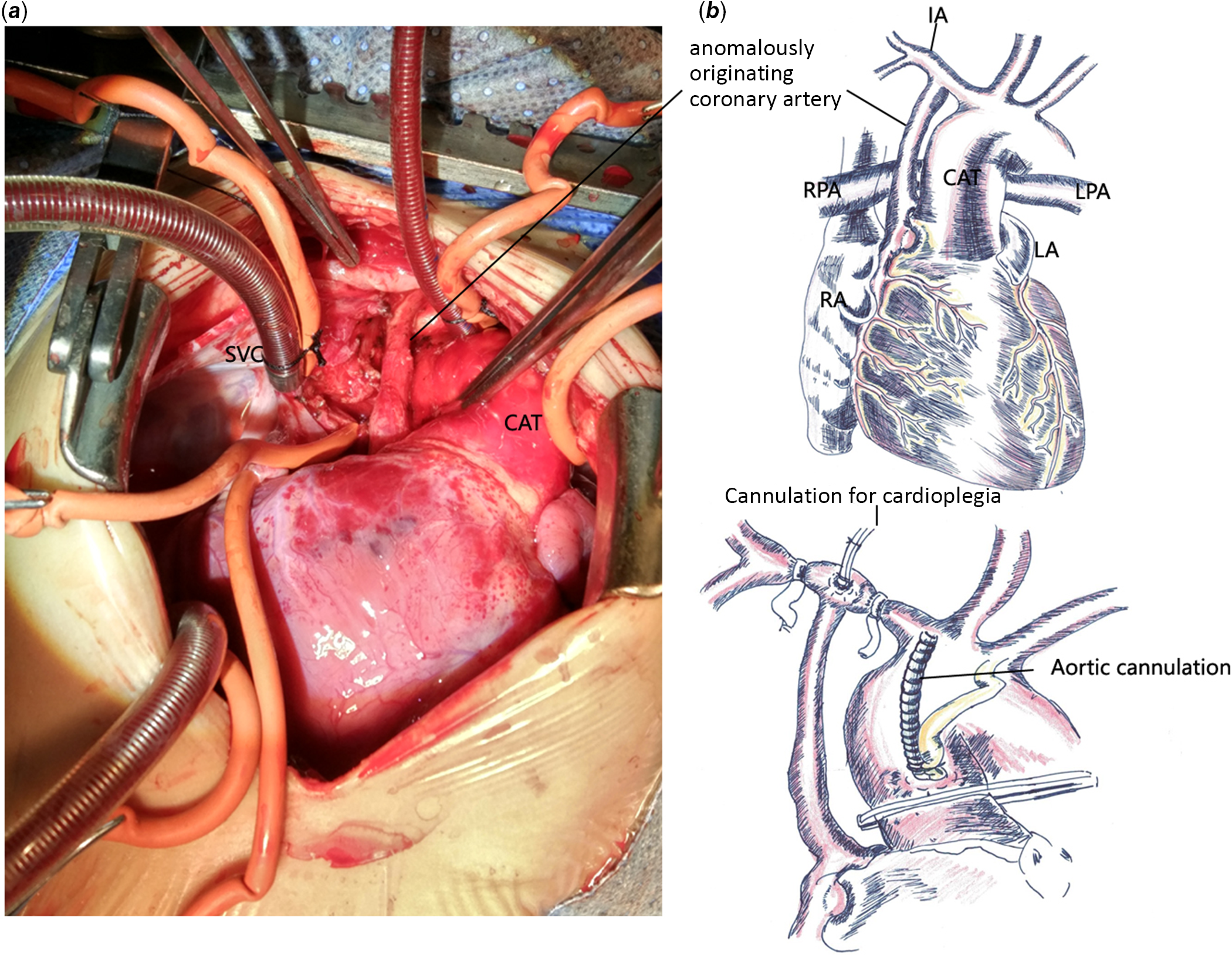
Figure 1. ( a ) A single coronary artery (CA) anomalously originated from the innominate artery (IA) on the large curvatur. It ran down between the common arterial trunk (CAT) and the superior vena cava (SVC) toward the posterior atrioventricular groove. ( b ) The cardioplegia (CP) infusion needle was inserted in the IA near the ostium of this CA. The proximal and distal of the IA was blocked when cardioplegia infusion.
The pulmonary branch arteries were disconnected from the truncus and a 16-mm bovine jugular vein conduit was placed from the right ventricle to the pulmonary branch arteries. A patch was used to close the ventricular defect. Partial closure of atrial septal defect was made with a 4-mm residual shunt. The cardiopulmonary bypass (CPB) and cross-clamp times were 196 and 113 min, respectively. The sternum was closed after weaning from CPB with support from inotropic agents, dopamine, and epinephrine. The intubation time was 4 days and after 1 day of humidified high flow nasal cannula oxygen therapy, the patient left the ICU at post-op day 8 and was discharged from hospital at post-op day 15. The echocardiogram showed satisfactory intracardiac correction with moderate mitral and tricuspid valve regurgitation, and atrial level two-way shunt associated with residual pulmonary hypertension.
At the time of writing, the patient is doing well without any respiratory symptoms or active intolerance 28 months post-operatively. The latest echocardiogram showed a 3-mm left-right shunt of the atrial level and mild mitral and tricuspid and pulmonary valve regurgitation. No pulmonary artery stenosis or dilation was observed. This case report has received approval from the institutional ethics committee of the Guangzhou Women and Children’s Hospital.
Discussion
Truncus arteriosus, also known as common arterial trunk, is an uncommon (1–3% of all cases of congenital heart disease) congenital cardiac defect that presents at birth. Reference Russell, Pasquali and Jacobs1 It supplies blood to the systemic and pulmonary circulation simultaneously, leading to increased pulmonary circulation and congestive heart failure. Within a few weeks after birth, the pulmonary hypertension will significantly increase, even leading to a pulmonary hypertension crisis after operation. Mayo Clinic’s early experience also showed that early mortality was associated with increased pulmonary vascular resistance. Currently, the surgical treatment of truncus arteriosus is generally advocated in neonates or within 3 months after birth to reduce the incidence of pulmonary hypertension crisis. Reference Marcelletti, McGoon and Mair2 In this case, the patient was 16-month-old, so the cardiac catheterization was performed to exclude the surgical contraindication.
Anomalies of the coronary arteries found in approximately 5–20% of truncus arteriosus patients Reference Lenox, Debich and Zuberbuhler3 and has been associated with high mortality following truncus arteriosus repair. Reference Naimo, Fricke and Yong4 The coronary artery pattern in truncus arteriosus should be determined preoperatively. Naimo et al made a retrospective study of 171 children who underwent truncus arteriosus repair, which demonstrated that a coronary artery anomaly carries a significant risk of death after repair of truncus arteriosus. Reference Naimo, Fricke and Yong4 Bonilla-Ramirez and colleagues concluded 34 patients with coronary lesion in 107 with truncus arteriosus. Four coronary lesions were identified: single coronary artery, ostial stenosis, intramural course, and juxtacommissural origin. Patients with complex coronary lesions have poor survival. Reference Bonilla-Ramirez, Ibarra and Binsalamah5
The origin of a single coronary artery outside aortic sinuses or above the aortic valve cusps is extremely uncommon. There are few reported cases of a single coronary artery arising from the innominate artery with additional truncus arteriosus and single ventricle malformations which were diagnosed at necropsy. Liu et al Reference Liu, Huang and Zhang6 in 2010 reported the case of a 42-day-old infant-boy with anomalous origin of a single coronary artery from the right branchiocephalic trunk associated with hypoplastic left ventricle, mitral atresia, and truncus arteriosus. Due to the poor prognosis and challenging surgery, the boy did not receive operation.
In our case of truncus arteriosus, a single coronary arose from a much higher site on the innominate artery. It would have been hard to perform coronary artery bypass grafting for such a small infant. We did not try to perform coronary reimplantation because the coronary button was difficult to procure, and the adequate location for reimplantation was difficult to select. Moreover, no specific surgical technique has been used in cases with a high take-off coronary artery and frequently required reoperation due to coronary artery stenosis. Reference Jung, Kwak and Kim7 Although we performed preoperative cardiac catheterization for this patient, the anomalies of the coronary arteries were not found as coronary angiography was too dangerous to be performed on the infant. Not having CT angiography images for this special patient is a regret. Due to the existing coronary artery fistula, the cardiac arrest could not be obtained successfully. It is important to select the location where cardioplegia infusion needle is inserted. Careful observation is needed when cardioplegia solution is infused.
There may be a connection between a single coronary artery arising from the innominate artery and truncus arteriosus according to the literature reports. The cardiac surgeon must be aware of the abnormal anatomy to avoid accidental ligation or cross-clamping or transection of the anomalous coronary artery during surgery. The three defects described above are rarely found together, and we performed successful surgical treatment; indeed, such a case as ours may be the first reported in the literature.
Acknowledgement
None.
Financial support
This work was supported by the National Natural Science Foundation of China (grant number 81800280).
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical standards
This case report has received the approval from the institutional ethics committee of the Guangzhou Women and Children’s Hospital.
Author contributions
Wenlei Li: writing the article and obtaining funding; Jianbin Li: making the drawing and data acquisition; and Xinxin Chen: designing the study and critical revision of the article.




