Introduction
Nasolabial cysts are benign and rare non-odontogenic masses located in the nasolabial fold.Reference Yuen, Julian and Samuel1–Reference Özer, Cabbarzade and Ögretmenoglu5 These lesions usually present as a painless swelling of the upper lip adjacent to the nasal alar region.Reference Yuen, Julian and Samuel1–Reference Özer, Cabbarzade and Ögretmenoglu5 For surgical treatment of nasolabial cysts, the intraoral sublabial approach and endoscopic transnasal approach have been advocated in the literature.Reference Yuen, Julian and Samuel1–Reference Narain7
This study aimed to identify the clinical characteristics and surgical outcomes of patients with nasolabial cysts presenting at our hospital. We also analysed the treatment results according to the two surgical approaches and evaluated the recent surgical trend in our hospital.
Materials and methods
This study was performed after obtaining approval from the Institutional Review Board of Chonnam National University Hwasun Hospital. Retrospectively, 24 patients with a histopathologically and radiologically confirmed nasolabial cyst between January 2010 and December 2017 were enrolled in this study.
The clinical data of 24 patients with 25 lesions (1 patient had bilateral nasolabial cysts) were analysed, including patient demographics, symptoms, symptom duration, cyst size and location, surgery and anaesthesia methods, post-operative complications, recurrence, and follow-up results.
All patients underwent pre-operative computed tomography (CT) to assess the extent of the lesion and facilitate treatment planning. All cases of nasolabial cysts were confirmed histopathologically after surgery.
The Fisher's exact test was used to determine the association between two categorical variables. SPSS® version 20.0 software was used for all statistical analyses. Statistical significance was considered at p < 0.05.
Results
The clinical findings for the nasolabial cysts are summarised in Tables 1 and 2. Of 24 patients with a nasolabial cyst, 2 were males and 22 were females. Their mean age (± standard deviation) was 50.8 ± 12.8 years (range, 17–72 years). Four patients had previously undergone an aspiration procedure. Three patients had previously received incision and drainage, while one patient had undergone marsupialisation. All patients presented with the mass in the nasolabial fold. Mean symptom duration was 29.5 ± 48.7 months (range, 0.5–216 months). The mean nasolabial cyst size was 1.7 ± 0.6 cm (range, 0.8–3.4 cm). The cyst was located on the right side in 10 cases, on the left side in 13 cases and on both sides in 1 case (Figure 1).
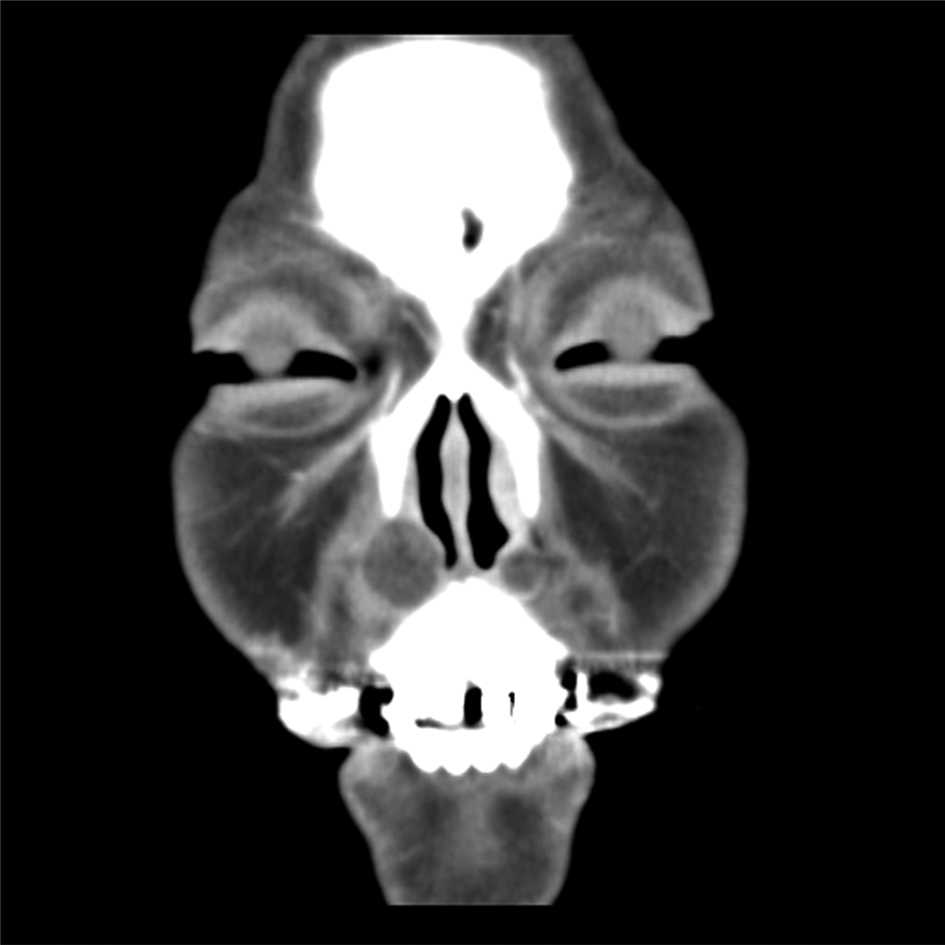
Fig. 1. Coronal computed tomography scan revealing well-defined, low density, bilateral cystic lesions in the anterior nasal floor.
Table 1. Clinical findings of 12 nasolabial cyst cases treated surgically using intraoral sublabial approach

*Indicates the same patient, who had cysts bilaterally, showing data for both sides. FU = follow-up; F = female; GA = general anaesthesia; M = male; I & D = incision and drainage; LA = local anaesthesia
Table 2. Clinical findings of 13 nasolabial cyst cases treated surgically using transnasal endoscopic approach

FU = follow-up; F = female; I & D = incision and drainage; GA = general anaesthesia; LA = local anaesthesia
Surgical treatment involved an intraoral sublabial approach in 12 cases (48.0 per cent) and a transnasal endoscopic approach in 13 cases (52.0 per cent). In 13 cases (52.0 per cent) surgery was performed under local anaesthesia, while in 12 cases (48.0 per cent) the operation was conducted under general anaesthesia. All lesions except four were diagnosed as nasolabial cyst on histopathology. The remaining four lesions were revealed to be chronic inflammation.
There were no major complications resulting from surgical intervention. The most common post-operative complications were numbness of the upper lip or teeth (n = 9, 36.0 per cent). These symptoms resolved within three months. In 12 patients who underwent the intraoral sublabial approach, 6 developed numbness of the upper lip or teeth. Three of 13 patients who underwent the transnasal endoscopic approach also presented with numbness of the upper lip or teeth.
Mean follow-up duration was 44.1 ± 26.9 months (range, 5–99 months). Only one patient (4.0 per cent), who underwent a transnasal endoscopic approach, experienced a reoccurrence. Following re-operation, the patient was disease-free.
Discussion
In this study, the two surgical procedures for nasolabial cysts, namely the intraoral sublabial approach and the transnasal endoscopic approach, were performed at a similar rate. Local anaesthesia and general anaesthesia showed similar rates too. However, there was a statistically significant recent surgical trend in our hospital to treat nasolabial cysts using a transnasal endoscopic approach under local anaesthesia (p < 0.05).
There are two theories for the pathogenesis of nasolabial cysts, but they have not yet been established.Reference Boffano, Gallesio, Campisi and Roccia2,Reference Sheikh, Chin, Fang, Liu, Baredes and Eloy3,Reference Özer, Cabbarzade and Ögretmenoglu5 One theory suggests that nasolabial cysts originate from trapped embryonic nasal respiratory epithelium after the fusion of maxillary medial and lateral nasal processes.Reference Boffano, Gallesio, Campisi and Roccia2,Reference Sheikh, Chin, Fang, Liu, Baredes and Eloy3,Reference Özer, Cabbarzade and Ögretmenoglu5,Reference Cohen and Hertzanu8 The other theory posits that nasolabial cysts are remnants of embryonic nasolacrimal duct tissue.Reference Boffano, Gallesio, Campisi and Roccia2,Reference Sheikh, Chin, Fang, Liu, Baredes and Eloy3,Reference Özer, Cabbarzade and Ögretmenoglu5
Nasolabial cysts were predominant in females (91.7 per cent) and presented more frequently on the left side (54.2 per cent), similar to previous reports.Reference Sheikh, Chin, Fang, Liu, Baredes and Eloy3,Reference Narain7 Nasolabial cyst occurred bilaterally in only one patient (4.2 per cent); this rate of bilateral occurrence is lower than that reported in other studies (approximately 10 per cent).Reference Boffano, Gallesio, Campisi and Roccia2–Reference Yeh, Ko and Wang6 The most common symptom of our patients was a mass in the nasolabial region.Reference Yuen, Julian and Samuel1–Reference Narain7 Imaging studies, including ultrasonography, CT and magnetic resonance imaging, are usually necessary for the diagnosis of nasolabial cysts.Reference Yuen, Julian and Samuel1–Reference Narain7 For accurate diagnosis and economic reasons, we performed CT scans.
Differential diagnoses of nasolabial cysts include both odontogenic and non-odontogenic lesions, such as a radicular cyst, periapical abscess, odontogenic cyst, schwannoma, minor salivary gland tumour, and dermoid and epidermoid cysts, which can develop in the nasolabial fold.Reference Sheikh, Chin, Fang, Liu, Baredes and Eloy3,Reference Narain7
Surgical removal is the treatment of choice for a nasolabial cyst.Reference Yuen, Julian and Samuel1–Reference Narain7 There are two surgical methods for nasolabial cysts: an intraoral sublabial approach and a transnasal endoscopic approach. The intraoral sublabial approach is a classic technique and the most common method used for nasolabial cysts, performed via a sublabial incision.Reference Boffano, Gallesio, Campisi and Roccia2,Reference Sheikh, Chin, Fang, Liu, Baredes and Eloy3,Reference Özer, Cabbarzade and Ögretmenoglu5 This approach can lead to good exposure of lesions. However, it is associated with some complications, such as facial swelling, numbness of gingiva and teeth, and risk of nasal floor perforation.Reference Yuen, Julian and Samuel1–Reference Narain7
The transnasal endoscopic approach is a simple and effective procedure.Reference Boffano, Gallesio, Campisi and Roccia2,Reference Sheikh, Chin, Fang, Liu, Baredes and Eloy3,Reference Özer, Cabbarzade and Ögretmenoglu5,Reference Su, Chien and Hwang9 This approach can lead to a reduced operative time, lower rates of facial swelling and pain, and a lower overall rate of complications.Reference Sheikh, Chin, Fang, Liu, Baredes and Eloy3,Reference Lee, Baek, Byun, Chang, Lee and Kim10 However, a small window on the nasolabial cyst may cause stenosis of the opening and a reoccurrence of the nasolabial cyst, as shown in one of our patients.Reference Özer, Cabbarzade and Ögretmenoglu5,Reference Lee, Baek, Byun, Chang, Lee and Kim10
In this study, the most common post-operative complication was numbness of the upper lip or teeth (n = 9, 36.0 per cent). However, there was no significant difference in post-operative complications between treatment involving an intraoral sublabial approach or a transnasal endoscopic approach (p > 0.05). A previous systemic review showed no difference in complications between the two surgical approaches either.Reference Sheikh, Chin, Fang, Liu, Baredes and Eloy3
• Nasolabial cysts were predominant in females (91.7 per cent) and more frequent on the left side (54.2 per cent)
• Intraoral sublabial and transnasal endoscopic approaches were performed for nasolabial cysts at a similar rate
• Local anaesthesia and general anaesthesia also showed similar rates
• Surgical resection via an intraoral sublabial or transnasal endoscopic approach is the best treatment for nasolabial cyst
• The recent surgical trend in our hospital is to treat nasolabial cysts using a transnasal endoscopic approach under local anaesthesia
Recurrence and malignancy transformation are very rare.Reference Sheikh, Chin, Fang, Liu, Baredes and Eloy3,Reference Choi, Cho, Kang, Chae, Lee and Hwang4 We only had one case of recurrence (4.0 per cent), in a patient who underwent a transnasal endoscopic approach. In a systemic review, Sheikh et al. demonstrated no significant difference in recurrence rates between an intraoral sublabial approach and transnasal endoscopic approach performed for nasal cysts.Reference Sheikh, Chin, Fang, Liu, Baredes and Eloy3
In this study, there were no significant differences in post-operative complications, anaesthesia method, or nasolabial cyst size between cases treated with an intraoral sublabial approach or a transnasal endoscopic approach (all p > 0.05). However, recently, the transnasal endoscopic approach under local anaesthesia has been performed more often in our institute (p < 0.05).
Conclusion
Surgical resection via an intraoral sublabial approach or a transnasal endoscopic approach is the best treatment for a nasolabial cyst, showing very good results with a low recurrence rate. The recent surgical trend in our hospital is to treat nasolabial cysts using a transnasal endoscopic approach under local anaesthesia.
Competing interests
None declared





