Introduction
Nasal airway obstruction is one of the most common patient complaints, both in the primary care setting and in general or subspecialty otolaryngology practice.Reference Stewart, Ferguson and Fromer1 The differential diagnosis for this complaint is broad, ranging from conditions involving simple anatomical obstruction such as septal deviation or turbinate hypertrophy to immunological causes such as allergy or chronic rhinosinusitis, or less commonly neoplastic or vascular aetiologies.Reference Corey, Houser and Ng2
Several structural abnormalities, including septal deviation, turbinate hypertrophy and adenoid hypertrophy, are well known to cause a sensation of nasal airway obstruction. As a result, these areas are routinely assessed by otolaryngologists, either with nasoendoscopic or radiological techniques to facilitate efficacious surgical intervention in the treatment of nasal airway obstruction.Reference Joniau, Wong, Rajapaksa, Carney and Wormald3–Reference Ciolek, Xu, Anne and Geelan-Hansen5
The septal swell body is a distinct structure of the anterior nasal septum, which sits anterosuperior to the middle turbinate.Reference Costa, Sanford, Janney, Cooper and Sindwani6 It is composed of thicker cartilage and mucosa in comparison to the rest of the nasal septum. Clinically, it is identifiable on nasoendoscopy (Figure 1) as a bulge of the nasal septum anterior to the middle turbinate head and radiologically as a high anterior septal swelling. Some researchers have suggested that the septal swell body may represent a vestigial remnant of the vomeronasal organ, which is responsible for pheromone detection in animals.Reference Negus7 Nevertheless, recent studies have noted that the septal swell body histologically resembles turbinate tissue and is rich in seromucinous glands and venous sinusoids.Reference Costa, Sanford, Janney, Cooper and Sindwani6,Reference Wexler, Bravermann and Amar8

Fig. 1. Nasoendoscopic photo showing the septal swell body (arrow) located in the superior nasal septum anterior to the middle turbinate head.
However, there is limited evidence in the literature that details the role that the septal swell body has in normal physiology and in disease. In particular, it is unclear whether the septal swell body has a significant impact on nasal airflow or limitation, and therefore its importance as a potential therapeutic target in nasal obstruction is yet to be determined. The density of vasoactive structures may indicate that, like turbinates,Reference Martinez, Nissen, Stock and Tesmer9 the septal swell body may be involved in the regulation of nasal airflow, air humidification and temperature regulation.Reference Smith, Brook, Virani and Platt10 It may also follow that, similar to the turbinates, the thickening, fibrosis and chronic inflammation of the septal swell body, caused by pathology such as allergy or altered immunology, may impact its morphology leading to nasal airflow obstruction.Reference Berger, Gass and Ophir11
As a result, this study aimed to determine if the septal swell body, in a similar way to the turbinates, is a dynamic structure that changes in size over time. If this is established, the study then aims to determine how changes in the size of the septal swell body correlate with the same changes in the inferior turbinate. If these questions pertaining to the underlying normal physiology of the septal swell body can be established, then recognition of the septal swell body as a ‘septal turbinate’ that may play a role in nasal breathing could promote further study of its role in nasal airway obstruction and pathology and therefore potential surgical interventions to this area.
Materials and methods
Patient population and data collection
Consecutive patients who underwent at least two high resolution computed tomography (CT) scans of their brain, paranasal sinuses or petrous temporal bones performed at a single tertiary hospital (Westmead Public Hospital, Australia) were identified by electronic medical records and databases held on the hospital premises.
Patients and scans were then excluded if imaging demonstrated primary pathology of the nose or paranasal sinuses, such as chronic rhinosinusitis or previous sinonasal surgery. Scans that did not include images of the septal swell body were also excluded. Scans that had a slice thickness of greater than 1 mm were also excluded.
De-identified data were then obtained from referral letters for each scan. Basic demographic data were collected, including patient age and sex. The indication for imaging, based on the referral form, was also recorded. The duration in days between the two CT scans was also calculated.
Ethical approval was received from the Western Sydney Local Health District Human Research Ethics Committee prior to data collection.
Assessment of imaging
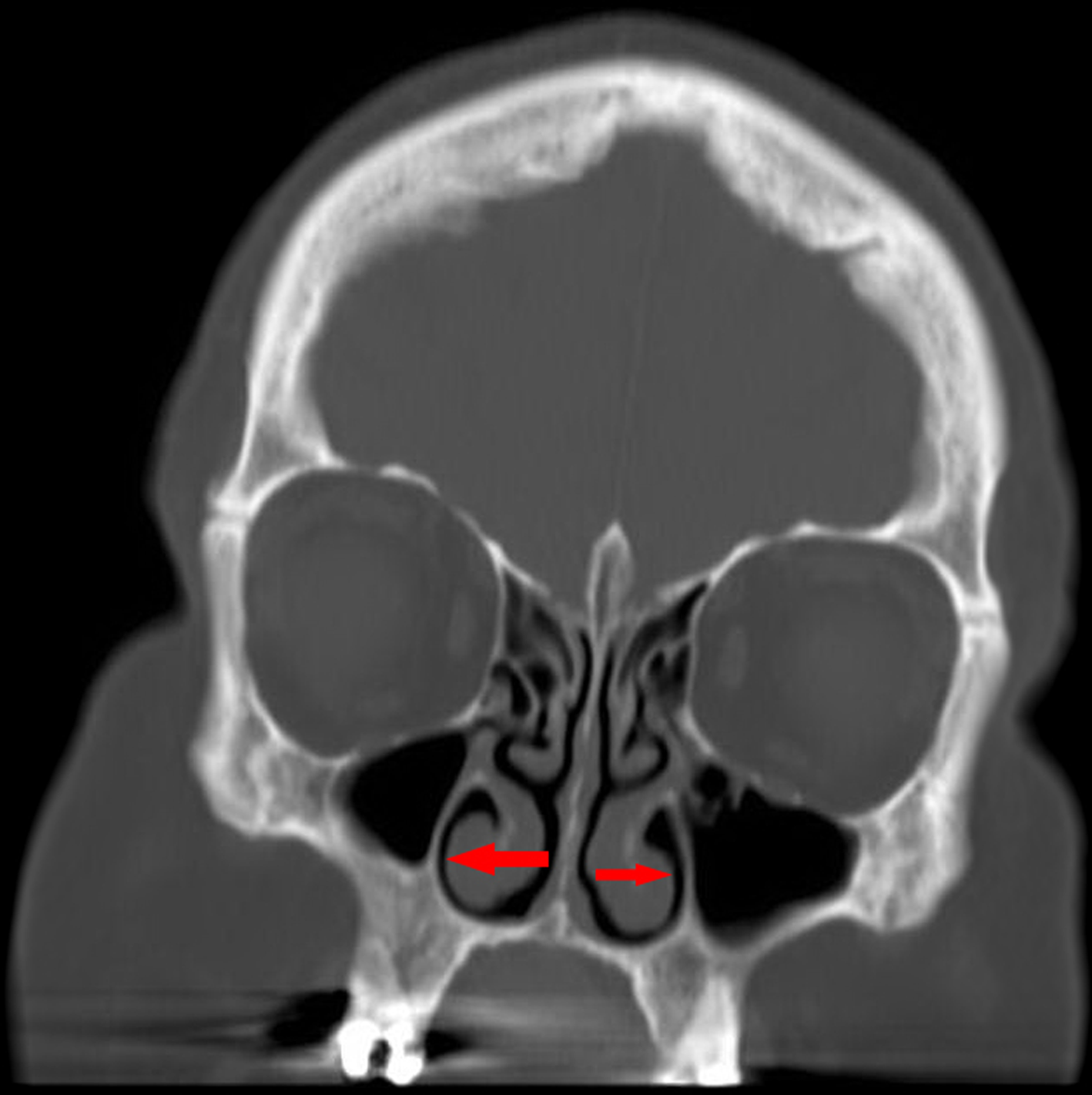
Each CT scan was assessed and measured to obtain the width and height of the septal swell body using a DICOM® viewer. The width of the septal swell body was assessed by measuring the total width (from the left nasal cavity to the right) using coronal CT slices in a horizontal plane. The slice containing the largest width was then used. At this slice, the height of the septal swell body was then also collected (Figure 2).

Fig. 2. High resolution image of the paranasal sinuses at a coronal slice demonstrating maximum width of the septal swell body.
The total inferior turbinate width was also measured. Each turbinate was measured from the most medial edge of the mucosal turbinate horizontally to the lateral nasal wall. The slice containing the largest combined width was used (Figure 3).

Fig. 3. High resolution image of the paranasal sinuses at a coronal slice demonstrating maximum width of the inferior turbinates.
The difference in septal swell body width and total turbinate width between scans for each patient was then calculated.
Statistical analysis
Patient age, time between CT scans, total turbinate width as well as septal swell body width and height were analysed as continuous data that were normally distributed and therefore reported as means with standard deviations. Sex was reported as categorical data as percentages with raw numbers. Correlations between the septal swell body width and height with total turbinate width was assessed using a Pearson's correlation coefficient. Statistical analysis was performed using SPSS® (version 25) statistical software.
Results
After exclusion of 20 patients because of sinonasal anatomy abnormalities or incomplete imaging of the septal swell body, a total of 34 patients (53 per cent female, n = 18) with a mean age of 58.3 ± 20.2 years were identified and met the criteria for inclusion in the study. The vast majority of patients underwent CT imaging for otological indications, and the remainder underwent imaging for skull base tumours separate from the nasal cavity. The mean difference in time between the two scans was 1.25 ± 1.13 years.
The mean maximal width of the septal swell body across all scans was found to be 9.56 ± 1.96 mm, with a range of 5.9–14 mm. The height of the septal swell body was 17.47 ± 5.75 mm, with a range of 13.0–26.0 mm. Mean total turbinate width was noted to be 13.02 ± 3.51 mm, with range of 5.3–20.9 mm.
The mean difference in maximal septal swell body width between scans for the same patient was found to be 1.57 ± 1.00 mm. The mean difference between scans in the maximal width of the inferior turbinates was found to be 2.23 ± 2.52 mm.
There was a statistically significant correlation between the change in septal swell body width and total inferior turbinate width across scans, demonstrating a moderate strength correlation (r = 0.35, p = 0.04). However, the height of the septal swell body did not demonstrate a statistically significant correlation with total inferior turbinate width (r = −0.10, p = 0.67).
Discussion
The role of the septal swell body in nasal airflow remains poorly understood, with minimal research examining this topic in the published literature. The findings of this study, that the septal swell body changes in size over time and that this change is correlated to the size of the inferior turbinates, is novel and may have significant ramifications on our understanding of the structural causes of nasal obstruction and the interventions that can be offered to address this common problem.
Our results appear to confirm that the physiology of the septal swell body, at least in healthy patients, behaves similarly to other vasoerectile tissue such as the inferior turbinates. This finding appears consistent with histological studies in the literature that have demonstrated similarity between the mucosal surfaces in each of these anatomical regions.
A study performed by Wexler et al.Reference Wexler, Bravermann and Amar8 in 2006 of 14 mucosal biopsied specimens demonstrated that the septal swell body contained venous sinusoids and clusters of seromucinous glands, similar to that of the inferior turbinate. The epithelium of the septal swell body and inferior turbinate exhibited similar columnar ciliated cells and goblet cells. On the other hand, the inferior anterior septum consisted mainly of transitional type epithelium with few ciliated columnar cells. As a result, the authors concluded that the septal swell body should be considered as another expansile vascular tissue of the nose. Furthermore, although the proportion of sinusoids in the inferior turbinate was higher than that of the septal swell body, and therefore may exhibit less vasoactivity, the narrow distal segment in which the septal swell body lies may produce greater than expected changes in nasal resistance.
Another further study performed by Costa et al.Reference Costa, Sanford, Janney, Cooper and Sindwani6 identified different findings to Wexler et al.Reference Wexler, Bravermann and Amar8 Using 54 magnetic resonance imaging scans and 10 cadaveric nasal septa, the investigators found that the septal swell body was a consistent anatomical feature in all patients. Under histological section, they found that the septal swell body contained significantly more venous sinusoids and fewer glandular elements to the adjacent septal mucosa. Nevertheless, Costa et al.Reference Costa, Sanford, Janney, Cooper and Sindwani6 agreed that the septal swell body appears to be vasoerectile in nature and may be an area that could be surgically addressed in patients with nasal obstruction.
It is understood that chronic inflammatory changes, such as that of repeated allergen challenges causes structural changes to turbinate tissue leading to hypertrophy and subsequent nasal obstruction. Berger et al.Reference Berger, Gass and Ophir11 noted that hypertrophic inferior turbinates had a thicker mucosal layer with fibrosis, inflammation and engorged venous sinusoids. Given the similarities of septal swell body histology with turbinate tissue, it follows that the septal swell body may also undergo septal swell body changes in disease that can be addressed with surgery.
Gelera et al.Reference Gelera, Ojar, Lim, Wee, Kim and Rhee12 retrospectively compared the size of the septal swell body in 405 patients between those diagnosed with allergic rhinitis or chronic rhinosinusitis with disease free controls. They found that the mean septal swell body diameter was significantly larger among the diseased group compared to controls. The authors further suggested that the septal swell body should be considered as part of the internal nasal valve, and small changes in its width could have significant impact on nasal airflow.
A randomised controlled trial performed by Yu et al.Reference Yu, Kim, Kim, Kang and Lim13 compared outcomes between patients who underwent inferior turbinoplasty only with those who underwent inferior turbinoplasty and reduction of the septal swell body with a microdebrider for nasal obstruction. They found a statistically significant improvement in nasal obstruction visual analogue scale scores in the septal swell body reduction group compared to those who underwent inferior turbinoplasty only. A statistically significant increase in nasal volume was also found.
Catalano et al.Reference Catalano, Ashmead and Carlson14 also noted that patients who had intractable nasal obstruction despite septoplasty, turbinate reduction and internal nasal valve repair appeared to experience benefit from septal swell body coblation, with statistically significant improvements in nasal obstruction symptom evaluation scale scores at 3 and 6 months post-operatively in a cohort of 60 patients.
Nevertheless, our study appears to confirm that the septal swell body is a dynamic structure that appears to have a vasoerectile function in healthy individuals, with close association with that of the inferior turbinates. Therefore, the role of the septal swell body may also be in the facilitation of laminar airflow, humidification and thermal regulation as well as filtration of particles. Furthermore, the septal swell body may also become hypertrophied, losing its normal, physiological size fluctuation, causing nasal obstruction that may need surgical intervention.
The septal swell body appears to exhibit considerable variation over time, and these changes correlate with normal physiological changes in the size of the inferior turbinates. This variability implicates it in normal physiology of nasal airflow and potentially in pathophysiology of nasal obstruction. Further research into the septal swell body is required to determine its feasibility as a potential surgical structure to address for patients with nasal obstruction.
• The nasal septal swell body is a normal anatomical structure located in the superior nasal septum
• Previous histological studies have demonstrated histological similarity between the nasal swell body and turbinate tissue
• This study demonstrates significant correlation between the width of the nasal swell body and inferior turbinate at various points in time in the same patient
• This suggests that the nasal swell body is a dynamic structure that may play a role in laminar airflow, humidification and thermal regulation in a similar way to the inferior turbinate
Conclusion
The septal swell body appears to be a dynamic structure that varies in width over time in close correlation to the inferior turbinates. This is consistent with previous literature suggesting that these anatomical structures are histologically similar. Nevertheless, further research is required to quantify its feasibility as a surgical area of interest.
Competing interests
None declared