At the end of April, 2020, an alert was sent out about severe paediatric cases presenting with shock that were possibly related to SARS-CoV-2.Reference Whittaker, Bamford and Kenny1 Clinical features of Kawasaki disease were noted from the first reported cases.Reference Whittaker, Bamford and Kenny1 This was considered to be a new syndrome and was named as multisystem inflammatory syndrome in children. In contrast to pre-COVID-19 habitual KD, this systemic inflammation syndrome predominantly affects older children, particularly of African descendants and Hispanic ethnicities. MIS-C frequently presents with gastrointestinal manifestations and myocardial involvement and requires aggressive treatment.Reference Whittaker, Bamford and Kenny1 There is no clear distinction between MIS-C and pre-pandemic KD shock syndrome. The following is a representative case that supports this statement.
Case report
A 5-year-old boy presented with a high fever and abdominal pain accompanied by a skin rash. He had COVID-19 contact within his family in the previous month. On physical examination, he was febrile and hypotensive and presented with bilateral conjunctival injection, urticarial exanthema of the trunk and extremities, redness of the lips, and left cervical lymphadenopathy. Laboratory tests revealed haemoglobin 10.51 g/dl, leukocytes 5290 cells/µl, lymphocytes 2200 cells/µl, albumin 3.3 g/dl, platelet count 582 × 109/L, elevated CRP 168 mg/L, elevated D-dimer 2590 ng/ml, elevated CK-MB (20.6 U/L) and NT-proBNP (1550 pg/ml and 3950 pg/ml), TGO 117 IU/L, TGP 163 IU/L, and interleukin-6 79.6 pg/ml. SARS-CoV-2 immunoglobulin G testing was positive. The echocardiographic evaluation showed normal biventricular systolic function but identified left coronary artery dilation of 4.5 mm (z score: 4.36). He was admitted to the ICU and was treated with intravenous immunoglobulin 2 g/kg, methylprednisolone 2 mg/kg/day, low-dose aspirin, and enoxaparin.
Discussion
KD presents more commonly in children with Asian ancestry, and surprisingly, MIS-C is rare in Asians, the latter more is commonly reported in children of African ancestry and Hispanic.Reference Whittaker, Bamford and Kenny1,Reference Gardner-Medwin, Dolezalova, Cummins and Southwood2 In the seminal paper of KDSS by Kaneyage et al. in San Diego, Hispanic patients were overrepresented with no Asians.Reference Kanegaye, Wilder and Molkara3 Before the COVID-19 pandemic, KDSS was considered to be a distinct and unique form of KD.Reference Gamez-Gonzalez, Moribe-Quintero and Cisneros-Castolo4 KDSS is defined as an episode during acute KD of hypotension and shock requiring volume expanders, infusion of vasoactive agents, or transfer to the ICU. KDSS differs from haemodynamically stable KD in terms of older age, frequent gastrointestinal manifestations, neurological manifestations, severe cardiac dysfunction, pericarditis, hypoalbuminemia, hyponatremia, and thrombocytopenia, with higher levels of CRP and troponin, all features are encountered in MIS-C.Reference Noval Rivas, Porritt, Cheng, Bahar and Arditi5 In PP-KDSS, gastrointestinal manifestations were present in 74.6% of the patients. Patients with MIS-C often present with an acute abdomen mimicking appendicitis.Reference Whittaker, Bamford and Kenny1 Coronary artery dilation or aneurysms have been described in 6–24% of patients with MIS-C. Echocardiographic include valve regurgitation, pericardial effusion, and marked LV dysfunction, again paralleling the course of PP-KDSS.Reference Whittaker, Bamford and Kenny1 Hypercoagulability with abnormalities in the coagulation cascade has been noted with elevated levels of D-dimers and fibrinogen. Notwithstanding, these laboratory findings are non-specific and are altered in PP-KDSS. Whittaker et al. compared MIS-C patients with PP-KDSS patients and found the former tended to be older, present with higher white blood cell count, CRP, and more lymphopenia, while alanine aminotransferase and D-dimer levels were similar.Reference Whittaker, Bamford and Kenny1 Remarkably, patients with MIS-C often present with thrombocytosis in the convalescent phase. Recently, superantigen activity of SARS-CoV2 have been implicated in the pathogenesis of MIS-C, similar to toxic shock syndrome.Reference Noval Rivas, Porritt, Cheng, Bahar and Arditi5 In PP-KDSS, TSS-1 was the most frequent diagnosis at the time of admission.Reference Gardner-Medwin, Dolezalova, Cummins and Southwood2 Superantigens have long been implicated in KD pathophysiology. In PP-KDSS, superantigens were implicated contrasting to hemodynamically normal-KD, and have been thought to have a role in this presentation of KD.Reference Iglesias-Amaya, Quezada-Ortega and Godinez-Victoria6 SARS-CoV2 has been shown to infect endothelial cells leading to endotheliitis.Reference Calcaterra, Mehta, Fanos and Bassareo7,Reference Varga, Flammer and Steiger8 MIS-C share more features with PP-KDSS than with TSS-1, particularly with TSS-1 lacking coronary arteries abnormalities (Table 1). Treatment of MIS-C is analogous to KDSS with IVIG, steroids, and biologics.Reference Whittaker, Bamford and Kenny1 Recently, the presence of SARS-CoV2 in the gastrointestinal tract with a breakdown of intestinal permeability and subsequent trafficking of the virus antigens into the bloodstream has been found.Reference Yonker, Gilboa and Ogata9 Importantly, treatment with larazotide, a tight junction regulator that improves intestinal permeability, was associated with clinical response in MIS-C.Reference Yonker, Gilboa and Ogata9 The clinical similarities and response to similar therapy support the notion that MIS-C is part of the KD spectrum, and with all these arguments, authorities in the field have concluded that MIS-C may be a new presentation of KD triggered by a single virus.Reference Sancho-Shimizu, Brodin and Cobat10 The parallelism of MIS-C with PP-KDSS reflects the racial predisposition, possible similar pathophysiology (superantigens in both), and infectious aetiology of KD located in the GI tract. These cases open research questions such as the genetic susceptibility of MIS-C (as an inborn error of immunity or superantigen and HLA-related) and the presence of an infectious gastrointestinal trigger, the role of superantigens, and the possible efficacy of larazotide in non-SARS-CoV2-KDSS.
Table 1. Demographic and clinical characteristics of patients with MIS-C and KDSS.
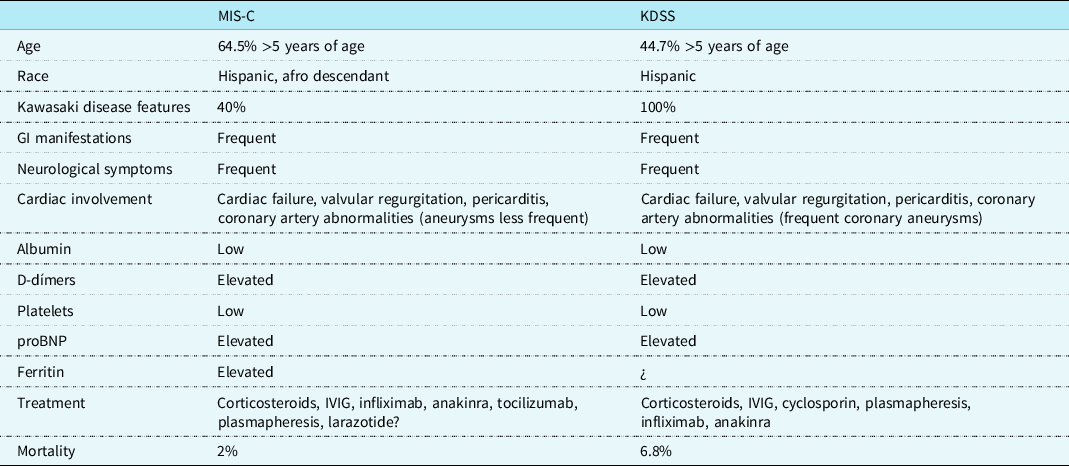
KDSS = Kawasaki disease shock syndrome, data are from references 2 and 3; MIS-C = Multisystemic inflammatory syndrome in children.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of interest
None.




