Introduction
Tympanosclerosis is an irreversible pathological process in the middle ear, usually resulting in conductive hearing loss. Histological changes are characterised by hyaline degeneration and calcification of the middle ear and mastoid mucosa.Reference Asiri, Hasham, al Anazy, Zakzouk and Banjar1–Reference Sheehy and House3 The pathogenesis of tympanosclerosis is not yet entirely clear. Severe acute otitis media sequelae, autoimmune causes, genetic factors, ventilation tube application sequelae and hypercalcaemia are some of the possible aetiologies discussed in the literature.Reference Forséni Flodin and Hultcrantz4–Reference da Costa, Paparella, Schachern, Yoon and Kimberley8
Tympanosclerotic calcareous plaques vary in terms of size and location, ranging from millimetric involvement to involvement of the entire tympanic cavity. Calcareous plaques often implicate the ossicular chain, and this usually results in conductive hearing loss. The most common way to restore hearing is surgical removal of the tympanosclerotic plaques, followed by reconstruction of the sound conduction mechanism.
Various surgical techniques have been described and utilised; however, the option of surgery and the choice of surgical technique remain controversial.Reference Stankovic9–Reference Martin, Timoshenko, Dumollard, Tringali, Peoc'h and Prades11 A variety of reconstruction materials have been used for ossiculoplasty, including homograft ossicles or cartilage, partial or total ossicular reconstruction prostheses, and, more recently, bone cements. The application of bone cement for ossicular reconstruction has shown promising results.
We describe an alternative technique for cases of malleus and incus fixation (caused by tympanosclerosis) that uses a glass ionomer cement for reconstruction of the sound conduction mechanism. This method involves removal of the malleus head and incus, and reconstruction of the ossicular chain from the manubrium mallei to the stapes, without the risk of refixation.
Materials and methods
Five patients with tympanosclerosis involving the malleus and incus underwent the manubrio-stapedioplasty with glass ionomer cement reconstruction technique at the Hacettepe University Faculty of Medicine (Department of Otorhinolaryngology – Head and Neck Surgery), between May 2010 and January 2012. The patients were categorised according to the tympanosclerosis classification reported by Wielinga and Kerr.Reference Wielinga and Kerr12 All cases were tympanosclerosis classification type 2; in other words, they had attic fixation of the malleus-incus complex with a mobile stapes. Patients were evaluated in terms of pre- and post-operative audiometric results. Follow-up time ranged from 14 to 30 months (mean of 22 months).
Surgical technique
All procedures were performed via an endaural approach under general anaesthesia. Endaural incision was made at the bony cartilaginous junction of the external ear canal. After elevation of the tympanomeatal flap and slight enlargement of the ear canal by drilling (for better exposure), the middle ear was inspected. For adequate exposure of the ossicles, we performed a limited atticotomy, which did not necessitate a reconstruction.
The following procedure was performed once all ossicles had been evaluated and the incudomalleolar attic fixation with mobile stapes had been identified. First, the incudostapedial joint was disarticulated to prevent inner-ear trauma associated with the inadvertent movement of ossicles (Figure 1). Tympanosclerotic plaques were then removed from the incus and malleus. The incudomalleolar joint was then separated with a 45° pick, and the incus was removed (Figure 1). The head of the malleus was cut with a malleus nipper, close to the neck, and removed (Figure 2). At this point, a mobile manubrium that has a very low possibility of fixation in the future by tympanosclerosis is obtained. As indicated before, a mobile stapes is necessary for this technique. Bone cement (Ketac-Cem (radiopaque); ESPE, Seedeld, Germany) was applied drop by drop to reduce the gap between the manubrium mallei and the head of stapes, until a complete bridge had been formed between the two structures (Figure 3). After obtaining a complete bone cement bridge, a 5-minute waiting period was necessary to enable stabilisation of the bridge.
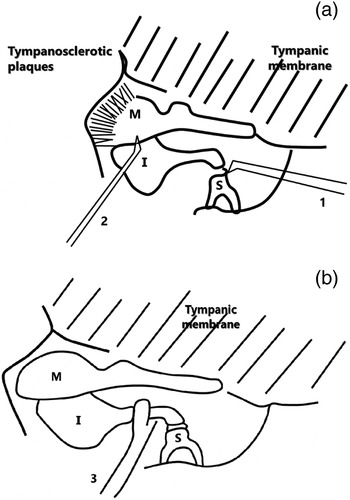
Fig. 1 (a and b) The illustrations show the malleus and incus fixed by tympanosclerosis. The incudostapedial joint is first separated with a 45° pick (1). The tympanosclerotic plaques surrounding the incus and malleus were then removed. The incudomalleolar articulation was separated with a 45° pick (2) and the incus was removed (3). (In order to illustrate the surgical method clearly, the outer attic wall is not shown in the drawings.) M = malleus; I = incus; S = stapes

Fig. 2 (a and b) The head of the malleus was cut with a malleus nipper (1), close to the neck, and removed (2). (In order to illustrate the surgical method clearly, the outer attic wall is not shown in the drawings.) M = malleus; S = stapes

Fig. 3 (a and b) Tiny drops of bone cement were applied between the manubrium mallei and head of the stapes (1) until a solid connection between the structures was achieved (2). (In order to illustrate the surgical method clearly, the outer attic wall is not shown in the drawings.) M = malleus; S = stapes
Results
The follow-up period of patients ranged from 14 to 30 months (mean of 22 months). Otoscopic examination was performed regularly during this period.
In all patients, the tympanic membrane healed satisfactorily, without any perforation or granulation tissue formation. None of the patients had facial nerve paralysis or any complications arising in the attic region post-operatively.
There were improvements in post-operative air pure tone average (PTA) values compared to pre-operative air PTA values for all patients. The mean pre-operative PTA was 55 dB (range, 28.75–82.5 dB) and the mean post-operative PTA was 18 dB (range, 11–30 dB). The mean pre-operative air–bone gap (ABG) was 42.75 dB (range, 23.75–60 dB) and the mean post-operative ABG was 6 dB (range, 2.50–12.50 dB). Hearing outcomes are shown in Table I and Figure 4. As indicated in Table I, four patients had post-operative ABG values of less than 10 dB; the remaining patient had an ABG of 12.50 dB.

Fig. 4 Hearing outcomes utilised according to the American Academy of Otolaryngology – Head and Neck Surgery minimal standard for reporting audiometric data, presented as scattergrams of pre-treatment (a) and post-treatment (b) hearing results for patients with manubrio-stapedioplasty. Data represent numbers of patients. *Indicates no change. PTA = pure tone average; ABG = air–bone gap
Table I Hearing outcomes

PTA = pure tone average; ABG = air–bone gap; pre-op = pre-operative; post-op = post-operative; FU = follow-up
Discussion
Fixation of the malleus and incus is the most common ossicular pathology encountered in tympanosclerotic ears during tympanoplasty.Reference Emmett and Shea13 Although several techniques have been described for reconstruction of the sound conduction mechanism, surgical management of tympanosclerosis in cases of incudomalleolar fixation remains controversial. There are also controversies regarding the choice of surgical technique.Reference Stankovic9–Reference Martin, Timoshenko, Dumollard, Tringali, Peoc'h and Prades11
The sound conduction mechanism can be restored by removing the tympanosclerotic plaques following a wide atticotomy, which mobilises the ossicular chain. The main problem of this method is refixation of the ossicles. Certain surgeons have advocated attic bypass procedures that utilise partial ossicular replacement prostheses (PORPs) or incus interposition grafts because of the considerable risk of ossicular refixation.Reference Emmett and Shea13–Reference Gibb and Pang17 Gel film insertion between potential contact areas and topical cortisone application are some other suggested methods to avoid ossicular refixation.Reference Joseph and Gordon18 The authors of the current study believe that the above-mentioned methods bear a risk of refixation.
Sensorineural hearing loss secondary to inadvertent drill contact with the ossicular chain, or instrumental manipulations during the removal of plaques on the ossicular chain with picks, might be expected in some cases. In the manubrio-stapedioplasty with glass ionomer cement technique, the incudostapedial joint is separated initially to avoid sensorineural hearing loss secondary to inadvertent movement of the ossicles during surgery.
Partial ossicular replacement prostheses and autografts can provide another solution. After removal of the incus and head of the malleus, incus interposition grafts, remodelled incus or malleus autografts, or PORPs can be used for reconstruction of the sound conduction mechanism.Reference Gibb and Pang17, Reference O'Reilly, Cass, Hirsch, Kamerer, Bernat and Poznanovic19 The disadvantages of PORPs are dislocation and extrusion after long-term use.Reference Roth, Pandit, Soma and Kertesz20–Reference Dalchow, Grun and Stupp22 Even with the use of a piece of cartilage between the PORP and tympanic membrane, there still may be extrusion. In addition, a PORP is a considerably more expensive alternative to other methods. In cases of incus or malleus interposition, stabilisation can be a problem, and may result in dislocation and failure.Reference Kartush23 The use of bone cement has again been advised by certain authors to avoid dislocation of the interposed ossicles.Reference Kalcioglu, Tan and Fleerakkers24
Recently, there has been an interest in using bone cements in otological surgery.Reference Bayazit, Ozer, Kanlikama, Durmaz and Yilmaz25–Reference Babu and Seidman27 Materials containing biocements have been used in mastoid obliteration, tegmen and ear canal wall reconstruction, and ossiculoplasty cases.Reference Kupperman and Tange28 Satisfactory hearing results have been reported with bone cement ossiculoplasty. Bayazit et al. reported on the bone cement repair of ossicular discontinuity between the incus and stapes, and between the malleus and stapes, with successful hearing restoration.Reference Bayazit, Ozer, Kanlikama, Durmaz and Yilmaz25
The manubrio-stapedioplasty with bone cement technique provides ideal closure of the ABG in patients with a fixed malleus and incus with a mobile stapes. The main advantages of this technique are a successful hearing result and cost effectiveness in comparison with PORPs. Application is easy, but care must be taken regarding the consistency of the cement. As the remaining manubrium has very little risk of being affected by further tympanosclerosis, the possibility of refixation is much lower with this technique. In addition, the possibility of dislocation is much greater with prostheses and homografts when compared to this technique.
It is important that the cement mixture is sticky, otherwise it may not be effective and revision may be necessary. Also, given the possible toxic effects of bone cement, care should be taken to avoid contact of the cement with the facial nerve and oval window.Reference Granstrom, Holmquist and Tjellstrom29 Aluminium toxicity can be encountered in patients who have undergone any cementoplasty surgery if the cement is in contact with cerebrospinal fluid or neural tissues.Reference Leveque, Soulie, Sarrazin, Hor, Desgeorges and Cordoliani30–Reference Renard, Felten and Bequet32 Glass ionomer cement has been used in our department since 2005, in over 100 patients so far (first author's personal experience). No such complication has been observed in these patients (in whom we adhered strictly to the principles of using a sticky mixture, and keeping the cement away from facial chorda tympani nerves and oval window).
One of the limitations of this study is the size of the patient population. This is because of the rarity of this special group of patients. The main aim of this paper was to report this novel technique in rare cases of malleus and incus fixation with mobile stapes. Although longer-term follow up is necessary, 3 patients with more than 20 months of follow up demonstrate the durability of the ossicular reconstruction technique. Longer-term results with an increased number of patients will be reported in the future.
No revision surgery has been performed in this patient population. Nevertheless, revision was required in three patients who received glass ionomer cement for ossicular reconstruction for other indications. In these patients, the cement did not adhere to the ossicles entirely (most probably because of its watery consistency); however, it was easily removed from ossicular surface with a 45° pick. Therefore, removal of the cement from bony surfaces is not difficult when required in revision cases.
In conclusion, the technique of manubrio-stapedioplasty using bone cement for cases of malleus and incus fixation (with mobile stapes) due to tympanosclerosis yields satisfactory hearing results. This cost-effective procedure can be performed safely in selected patients.