Total open thyroidectomy (TT) is one of the most frequently adopted surgical procedures. It is included in the list of Livelli Essenziali di Assistenza (Essential Assistance Levels-LEA). TT can be performed either with the conventional knot-tying technique (traditional) or using ultrasound activated shears (ultrasound scalpel). The ultrasound scalpel was developed in the 1990s and was initially used in laparoscopic surgery. It coagulates and simultaneously cuts tissue using mechanical energy with ultrasonic frequency at 55.5 kHz. This ultrasound vibration enhances blade-cutting ability and coagulates blood vessels, reducing operation time and producing less thermal damage to the surrounding vital structures (Reference Amaral1). The effectiveness and impact on the quality of life (QoL) of patients of the ultrasound scalpel in TT is widely investigated in literature (Reference Amaral and Chrostek2;Reference Bellantone, Lompardi and Bossola3;Reference Cordón, Fajardo, Ramirez and Herrera7;Reference Giddings11;Reference Karvounaris, Antonopoluos, Psarras and Sakadamis13;Reference Kilic, Keskek and Ertan14;Reference Miccoli, Berti and Raffaelli19–Reference Randolph and Donley21;Reference Siperstein, Berber and Morkoyun23). However, the associated costs for hospitals have only been partially investigated in a limited number of studies (Reference Hallgrimsson, Lovén and Westerdahl12;Reference Shemen22). So far, no published study has combined the clinical, economic, and QoL-related aspects. In this study, we present the results of the HARMONIC study, which represents the first cost-effectiveness analysis on the use of ultrasound scalpel in TT.
METHODS
Study Design
The HARMONIC study was carried out at the Department of Endocrine-surgery, in cooperation with the Health Technology Assessment Unit, University Hospital “A. Gemelli” and the Faculty of Economics, Catholic University of Rome. The study was designed as an economic evaluation of the use of such technology on the side of a Randomized Controlled Trial, in which economic data were expressly collected. The optimal sample size was estimated in 200 patients on the basis of the null hypothesis of a better performance of the ultrasound scalpel in terms of patient recovery at 3 months. Adult patients (>18 years), eligible for conventional total thyroidectomy (TT) with no previous cervical surgery intervention, were enrolled. Stratified randomization was performed according to age, sex, and size of thyroid nodules, after patients had signed an informed consent. A total of 203 patients were included and randomly assigned to one of these two treatment groups: (i) the Ultrasound group, in which patients were treated with the ultrasound scalpel; (ii) the Traditional group, in which patients were treated with the traditional scalpel.
After discharge, patients were contacted by telephone after 1 and 3 months to monitor their QoL, the changes in their vocal tone, their esthetic perception of the scar (Reference Miccoli, Berti and Raffaelli19), and their use of healthcare resources. Figure 1 reports the flow chart of the study according to CONSORT guidelines.

Figure 1. Flow chart of the study.
The study was approved by the Ethics Committee of the University Hospital “A. Gemelli.” Data were collected and stored at the Health Technology Assessment Unit.
Identification, Measurement, and Evaluation of Costs
The study considers simultaneously a hospital, a third party payer (TPP), and a social-perspective. The resources used during hospitalization—that is, type and number of diagnostic tests, drug consumption, medical and nursing care (expressed in minutes), operating theater usage (OT) (expressed in minutes), surgical team composition, and materials used in the OT—were observed for each patient during his/her hospital stay. Medical and nursing assistance were measured with the help of clinicians. During TT a trained member of staff, involved in the study (but not in the procedure), collected data in the OT. The duration of the TT was defined as the time interval between the first incision and the last suture (Reference Cordón, Fajardo, Ramirez and Herrera7), while duration of anesthesia was defined as the time between administration of the anesthesia and awakening of the patient. Data concerning the use of healthcare resources during the follow-up period, as well as productivity losses, were collected by telephone interview 1 and 3 months after discharge. Drug consumption was measured using prescribed daily dose (PDD). Finally, productivity loss was assessed in terms of missed working hours (as declared by patients in telephone interviews in the follow-up period).
To evaluate the usage of healthcare resources, we referred to the following: (i) the purchasing price applied to the Hospital for treatments during hospitalization and the National Pharmaceutical List for treatments in the follow-up period; (ii) standard cost of staff per year calculated on the basis of annual personnel working hours (including the surgical team) reported in the Hospital's management control data; (iii) the price published in the diagnostic and outpatient services list of the Lazio Region for diagnostic tests and consultations; (iv) management control data related to the daily costs of hospitalization in the Department of Endocrine Surgery for the mentioned expenses; (v) the human capital approach based on data provided by the Bank of Italy in 2007 for loss of productivity.
Identification, Estimation, and Evaluation of Effectiveness
After surgery, the patients’ perception of pain was monitored after 6–24–48 hours using a visual analogue scale ranging from zero (minimum pain) to ten (maximum pain) (Reference McMillan, Bradley, Razvi and Weaver16).
The frequency used to evaluate the postoperation pain, that is, after 6–24–48 hours, was based on the clinicians’ information and experience of a previous study conducted for TT using a video-assisted technique (Reference Hallgrimsson, Lovén and Westerdahl12). Patients’ quality of life (Reference McMillan, Bradley, Razvi and Weaver16) was assessed on admission, at discharge and 1–3 months after surgery with the EuroQoL 5D questionnaire (EQ-5D). Finally, to obtain the gain in quality-adjusted life-year (QALY), we assumed an improvement of QoL up to 3 months after discharge. We considered the 3-month QoL gain resulting from the EQ-5D score as the QALY gain over 1 year.
Cost-Effectiveness Analysis
The statistical differences between the results of the two groups of patients were tested with parametric tests (t-test, Chi-squared) and nonparametric tests (Wilcoxon-Mann-Whitney test, Fisher's exact test) based on the characteristics of the distribution. The presence of a normal distribution was assessed using the Shapiro-Wilks test. We referred to a 5 percent significance level. Regarding the timing of the operation and anesthesia, confidence intervals were assessed according to the normal distribution. The data processing was carried out using SPSS 12.0 statistical software. To test the consistency of the findings, we performed a one-way and a multi-way sensitivity analysis (Reference Briggs4–Reference Claxton, Sculpher and McCabe6).
We observed the impact on the incremental cost-effectiveness ratio (ICER) of the variability of each resource used with the one-way sensitivity analysis and, finally, we performed a nonparametric bootstrap simulation and the cost-effectiveness ratios were distributed on a cost-effectiveness acceptability curve (CEAC) (Reference Defechereux, Rinken, Maweja, Hamoir and Meurisse8–Reference Fenwick, O'Brien and Briggs10). Preliminary results were published in Lombardi et al. (Reference Lombardi, Raffaelli and Cicchetti15). The final results of the study, processed at the end of the admission and follow-up periods for all patients, are presented below.
RESULTS
Sample Analysis
At the end of March 2008, 202 patients were enrolled in the study, of whom 105 in the Ultrasound group and 97 in the Traditional one. Loss to follow-up 1 month (3 months) after surgery was 7 percent (8.5 percent), leaving 185 patients for final analysis. The randomization of the patients between the two groups was successful as confirmed by the absence of statistically significant differences in age (Traditional: 52.69 versus Ultrasound: 49.36 years, p-value = 0.122), sex and surgical diagnoses (Table 1). Women represented the majority of the sample, and the most frequent diagnoses were diffuse or multi-modular goiter, follicular nodule, and pre-toxic or hyper-functional goiter.
Table 1. Sample Characteristics of the Sample of Patients Enrolled

Note. HS, harmonic scalpel; nHS, nonharmonic scalpel; EQ-5D, EuroQoL 5D questionnaire.
There were no QoL differences between the two groups of patients on admission.
Cost Analysis
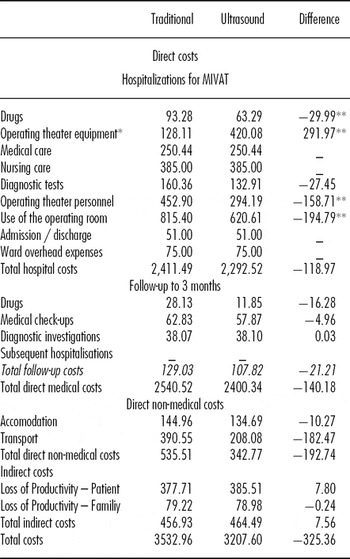
The cost analysis was performed on 199 patients, 102 in the Ultrasound group, and 97 in the Traditional group. The use of the ultrasound scalpel did not affect length of hospitalization that lasted 5 days, including the day before the operation. However, the Ultrasound group had a significantly lower average duration of TT. Appendix table shows the details regarding resources used, namely: OT usage (minutes), OT personnel (number of surgeons, nurses and others), quantity and duration of drainage, and duration of analgesic therapy. Further information about resources used (e.g., OT equipment in detail, OT and postoperation drug consumption in detail) as well as the form used to collect data are available for interested readers. In general, use of the ultrasound scalpel reduced OT occupation time and duration of anesthesia. Table 2 shows estimates of the average individual cost item per patient. The price of the ultrasound scalpel affects the cost of OT equipment but is compensated by shorter operation time. Overall, the use of the ultrasound scalpel allowed a reduction in hospitalization costs. Concerning the follow-up period, the sample with available data included 185 patients, 92 in the Ultrasound group and 93 in the Traditional one. In this period, there were no changes in direct medical costs: drugs, medical visits, and diagnostic exams. No further hospitalizations took place. Savings per patient, including the follow-up period, in terms of direct costs amounted 140.18 euros, whereas there was no significant statistical difference regarding nonmedical direct costs between the two groups of patients. The productivity loss was similar in both groups of patients as well as the household costs. Table 2 also shows the details of accommodation and transport costs related to hospitalization and examinations after discharge.
Table 2. Average Costs of Admission for TT 3 Months After Surgery (ί)

Note. *also includes the Ultrasound scalpel cost (291,97 euro)
** level of significance < 0.05
Including nonmedical direct costs, the Ultrasound group was less costly. In general, the use of the ultrasound scalpel showed a reduction of both direct and indirect costs.
Effectiveness Analysis
After the operation, the pain perception was registered after 6–24–48 hours by administering a visual analogue scale. There were no statistically remarkable differences between the two groups, although a different evolution over time was registered (Table 3). Six hours after surgery, the Ultrasound group tended to perceive less pain which was associated with better QoL on discharge. The QoL appeared to be higher for this group in the follow-up period as well, as shown in Table 3. The Ultrasound group also experienced better perception of the scar 1 and 3 months after discharge.
Table 3. Evolution of Quality of Life Following Total Open Thyroidectomy

Note. HS, harmonic scalpel; nHS, nonharmonic scalpel; EQ-5D, EuroQoL 5D questionnaire.
Low complication rate after 3 months confirmed the clinical validity of the ultrasound scalpel as well as the similar frequency and severity of changes in vocal tone between the two groups.
Base Case Analysis
In the base case, the Ultrasound group experienced cost reduction associated with an improvement in QoL which resulted in a QALY gain of 0.07.
Sensitivity Analysis
Supplementary Tables 1 and 2 (which can be viewed online at www.journals.cambridge.org/thc2012030 and www.journals.cambridge.org/thc2012031, respectively) show the results of the sensitivity analysis. Regarding variation of the resources used, the analysis shows that the most sensitive is OT use followed by OT personnel, nursing assistance, and OT equipment. In any case, the Ultrasound scalpel remains dominant if a one-way sensitivity analysis is conducted. In this case, ICER values are negative as the costs of the harmonic scalpel group are lower than those of the nonharmonic scalpel group. This suggests negative incremental cost due to positive incremental effectiveness. Concerning variation of total hospital costs, ICER can rise to 18,000 euros/QALY.
Supplementary Figure 1 (which can be viewed online at www.journals.cambridge.org/thc2012032) shows the cost-effectiveness acceptability curve (CEAC) resulting from the bootstrap-based multi-varied sensitivity analysis. The ultrasound scalpel is dominant in 65 percent of the simulations and ICER remains below 30,000 euros/QALY in 90 percent of cases.
DISCUSSION
From a clinical point of view, the HARMONIC study confirms the effectiveness of the ultrasound scalpel, given the encouraging results in the follow-up period in terms of postoperative pain, improved QoL, complications, and alterations of vocal tone. The use of the ultrasound scalpel does not affect duration of hospitalization and reduces operation time by more than 20 minutes, thus reducing the costs associated with the surgical team and OT use. This saving compensates the higher cost of OT equipment and ultrasound scalpel cost. The improvement in QoL associated with the reduction of hospital costs results in a QALY gain of 0.07. Cost-effectiveness ratio is dominant in 65 percent of the scenarios considered in the bootstrap simulation (see Supplementary Figure 1). Moreover, the threshold analysis shows 90 percent of the scenarios considered below an ICER of 30,000 euros per QALY. Given these results, we considered the impact of our results on the Diagnosis Related Groups (DRG) system. In 65 percent of cases, because technology is dominant, the hospital achieves greater efficiency. When technology is not dominant but below a threshold of 30,000 euros/QALY, the hospital experiences an extra cost, albeit lower than the DRG tariff, which is paid by the Italian National Health Service (SSN). This finding confirms that ultrasound technology is affordable for third party payers (TPP). Our results confirm the findings reported in other studies (Reference Lombardi, Raffaelli and Cicchetti15); however, certain strengths and limitations should be stressed. As far as the strengths are concerned, the HARMONIC study is the first cost-effectiveness analysis on the use of the ultrasound scalpel in TT performed in an Italian university hospital. A different study (Reference Ortega, Sala, Flor and Lledo20) on 200 patients presents the results only in terms of total costs, not providing any data in terms of QoL or ICER. The study follows a scientific protocol which may easily be applied in a different organizational context. Moreover, we conducted a nonsystematic literature review to compare our results with the previous existing (Reference Meurisse, Degechereux, Maweja, Degauque, Vandelaer and Hamoir17–Reference Ortega, Sala, Flor and Lledo20), which explains a reduction in OT use of 18–26 percent. Furthermore, Hallgrimsson et al. (Reference Hallgrimsson, Lovén and Westerdahl12) provide an estimate of TT costs for patients with Graves’ disease of 2,303 euros for the ultrasound scalpel and 2,511 euros for the traditional scalpel if the operation is performed in a university hospital. The data differ from the results presented here because of the different cost parameters used. Indeed, in Hallgrimsson et al. (Reference Hallgrimsson, Lovén and Westerdahl12), only OT occupation time and market prices of materials used, including sutures, clips, and gauzes, are considered while personnel costs are not mentioned. The data used in our study are particularly appropriate. The difficulty in obtaining data on the operating phase as discussed in literature (Reference Meurisse, Degechereux, Maweja, Degauque, Vandelaer and Hamoir17–Reference Miccoli, Berti and Raffaelli19;Reference Stojadinovic, Shaha and Orlikoff24–Reference Yildirim, Umit and Ebru27), was partly overcome by the “A. Gemelli” hospital using the OT information system. The HARMONIC study also highlights the costs of the surgical phase very precisely, including personnel costs. One of the limitations of this study is that the emphasis on organizational and operational reality refers only to one hospital. Furthermore, surgeons involved in the study have outstanding expertise in the use of the ultrasound scalpel. This could affect the transferability of the results to organizational contexts with different levels of expertise and quality. Moreover, we did not include training costs associated with the use of the ultrasound scalpel. This could have caused a bias in the “generalizability” of our findings for training costs could, indeed, be too onerous for small hospitals. Hence, the introduction of the ultrasound scalpel may not be efficient in organizational contexts with different and smaller volumes of activity than the “A. Gemelli” University hospital. Moreover, our study considered a differentiated sample of patients from a vast geographical area. However, this introduces a further limitation regarding the evaluation of the changes in vocal tone which we monitored through self-assessment. Finally, the one-way sensitivity analysis (see Supplementary Tables 1 and 2) allowed us to identify some implications for future research. In particular, OT use should be further investigated as it is the crucial parameter for sustainability of the cost-effectiveness ratio. Moreover, a multicenter study with cluster randomization should point out the opportunity to introduce complex technologies in different organizational settings.
CONCLUSIONS
In our study, we have shown that the ultrasound scalpel is a cost-effective technology, showing a cost per QALY below 30,000 euros in 90 percent of the scenarios considered. The widespread use of the ultrasound scalpel for TT would re-define OT use, enabling more operations in the same period of time. The lower variability also guarantees more precise planning and implementation of one-day surgery. In line with previous literature (Reference Lombardi, Raffaelli and Cicchetti15), we point out the possibility of reducing patient waiting lists for surgery.
SUPPLEMENTARY MATERIAL
Supplementary Table 1
www.journals.cambridge.org/thc2012030
Supplementary Table 2
www.journals.cambridge.org/thc2012031
Supplementary Figure 1
CONTACT INFORMATION
Matteo Ruggeri assistant Professor of Policy and Economics, Facoltà di Economia, Università Cattolica del Sacro Cuore, Francesco Vito 1, 00168 Rome, Italy
Rossella Dibidino senior research fellow at the HTA Unit, A Gemelli University Hospital, Università Cattolica del Sacro Cuore, Marco Marchetti Director of the HTA Unit of the A Gemelli University Hospital, Università Cattolica del Sacro Cuore, Celestino Pio Lombardi director of the endocrinosurgery unit at the A Gemelli University Hospital, Università Cattolica del Sacro Cuore, Marco Raffaelli Director of the HTA Unit of the A Gemelli University Hospital, Università Cattolica del Sacro Cuore, Policlinico Universitario “A. Gemelli,” Università Cattolica del Sacro Cuore, Rome, Italy
Americo Cicchetti Professor of Management, Facoltà di Economia, Università Cattolica del Sacro Cuore, Rome, Italy
CONFLICTS OF INTEREST
All authors report receiving an unrestricted grant to their institution from J& J Medical, payment for writing or reviewing the manuscript, and support in kind to themselves and their institute. Rossella Dibidino states no conflict of interest in the analysis, data collecting, and writing of this manuscript; Matteo Ruggeri states no conflict of interest in the analysis, data collecting, and writing of this manuscript; Americo Cicchetti states no conflict of interest in the analysis, data collecting, and writing of this manuscript; Marco Marchetti states no conflict of interest in the analysis, data collecting, and writing of this manuscript; Marco Raffaelli states no conflict of interest in the analysis, data collecting, and writing of this manuscript; Celestino Pio Lombardi states no conflict of interest in the analysis, data collecting, and writing of this manuscript.