Introduction
The parapharyngeal space is a well-defined upper neck region located immediately lateral to the pharynx. Its ventral (prestyloid) compartment contains the parotid gland, fat and lymph nodes. The dorsal (retrostyloid) compartment corresponds to the carotid sheaths and the associated enclosed structures, including the internal carotid artery, internal jugular vein, IXth to XIIth cranial nerves and lymph nodes.Reference Presutti, Molteni, Malvè, Marchioni, Ghidini and Tassi1 This space harbours approximately 0.5 per cent of all head and neck neoplasms, and approximately 80 per cent of these tumours are benign lesions.Reference Servadei, Romano, Ferri, Magri and Sesenna2
Traditionally, different tumours should require different surgical methods based on the nature of the tumours.Reference Bradley, Bradley and Olsen3–Reference Khafif, Segev, Kaplan, Gil and Fliss5 Specifically, these procedures include transcervical, transparotid and transoral approaches, or a combination of the three.Reference Bradley, Bradley and Olsen3–Reference Khafif, Segev, Kaplan, Gil and Fliss5 However, benign tumours of the parapharyngeal space are located in the medial portion of the carotid sheaths, extending toward the skull base, and these tumours are not easy to detect by submandibular palpation. Given the evidence of exposure difficulties by the routing of the transcervical and transparotid approaches for tumours located in the superomedial parapharyngeal space, a more aggressive approach, such as mandibulotomy, may be taken. However, the transoral approach is often used.Reference Ducic, Oxford and Pontius6–Reference Chen, Wang, Zhang and Huang8
We chose a transoral or an endoscope-assisted transoral approach to resecting these tumours. This article describes our experience in surgically managing benign tumours in the superomedial portion of the parapharyngeal space over a five-year period, with special focus on the surgical approach, adequate mass exposure and structure safety.
Materials and methods
Patient selection
From January 2010 to September 2015, 32 patients with a mass in the medial portion of the parapharyngeal space were referred to the ENT Department of Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology. All these patients were diagnosed with benign tumours in the medial portion of the parapharyngeal space.
These patients underwent a transoral or an endoscope-assisted transoral surgical approach, and all were enrolled in this retrospective cohort study. The transoral approach was limited to benign tumours of the parapharyngeal space located in the medial portion of the carotid sheaths, extending toward the skull base. The tumours were not easy to feel by submandibular palpation.
Pre-operative imaging analysis consisted of computed tomography (CT) and/or magnetic resonance imaging (MRI). When necessary, pre-operative fine-needle aspiration cytology was performed.
Surgical approach
Transoral approach
Under general anaesthesia with orotracheal intubation, the mouth gag was inserted. If the tumour was larger than 6 cm in diameter, preventive tracheostomy was performed. The incision was made on the palatopharyngeal arch or the soft palate with the electric scalpel, according to the position of the tumour. The fascia and muscles were separated to the left or right, and blunt dissection was performed along the capsule (i.e. ‘extracapsular dissection’); fingers were sometimes used to remove the tumours. If the tumours were lobulated with an incomplete capsule, or were too hard, they were removed by en bloc resection.
Endoscope-assisted transoral approach
In some cases, we attempted endoscope-assisted resection. For instance, endoscope-assisted resection was utilised in cases of en bloc resection. Endoscope-assisted surgery was performed using a 4 mm, 0-degree nasal endoscope, to dissect parts of the tumour that could not be seen directly. The tumour's lateral, superior and deep margins were dissected with an endoscope. The 0-degree endoscope was adequate for the majority of procedures performed for relatively small tumours.
Drainage tube placement
When the tumour was larger than 5 cm in diameter, negative pressure drainage was required. A rubber drainage tube was led from the lower part of the surgical field to the contralateral posterior naris and anterior naris, to drain effusion in the surgical cavity.
Peri-operative complications
Peri-operative complications related to our surgical approach were limited to laryngeal nerve palsy.
Peri-operative management
Antibiotic therapy was administered intra-operatively and for 7 days after surgery. The drainage tube was placed in position and removed when the effusion had almost disappeared.
Follow up
Post-operative radiological assessment was performed using MRI or CT with contrast. Imaging was performed every year to monitor for local relapse.
Results
This study comprised 32 patients (20 females and 12 males), with an average age of 29.7 years (range, 12–56 years). All patients underwent complete resection of the lesions via a transoral approach or endoscope-assisted transoral approach.
Pathology findings included: neurilemmoma (n = 18), pleomorphic adenoma (n = 5), neurofibroma (n = 5), desmoid tumour (n = 2) and hyaline degeneration (n = 2). Tumour size varied from 2.2 cm to 7 cm (mean, 4.1 cm).
Preventive tracheostomy was performed in 5 cases, endoscope-assisted surgery was carried out in 11 cases and negative pressure drainage was conducted in 9 cases.
Post-operative deficits were limited to the expected laryngeal nerve palsy after resection of vagal schwannoma lesions. Two patients developed a light vocal fold paralysis and symptomatic dysphonia, but the paralysis and dysphonia resolved two months after the procedure. None of the patients developed airway compromise, post-operative infection or dehiscence of the mucosal incision.
None of the patients in this series demonstrated residual or recurrent neoplasms, either clinically or radiographically, during their follow-up period (average of 28 months; range, 12–60 months).
Representative cases are shown in Figures 1 and 2.

Fig. 1. A case of a pleomorphic adenoma. (a) Sagittal, (b) coronal and (c) axial magnetic resonance scans showed a large mass within the right parapharyngeal space (red arrows indicate the pleomorphic adenoma). (d) Intra-operative view of the right parapharyngeal space tumour (red arrow indicates the tumour). (e) The tumour was removed completely (red arrow indicates previous location of tumour shown in part d). H = head; F = feet; A = anterior; P = posterior
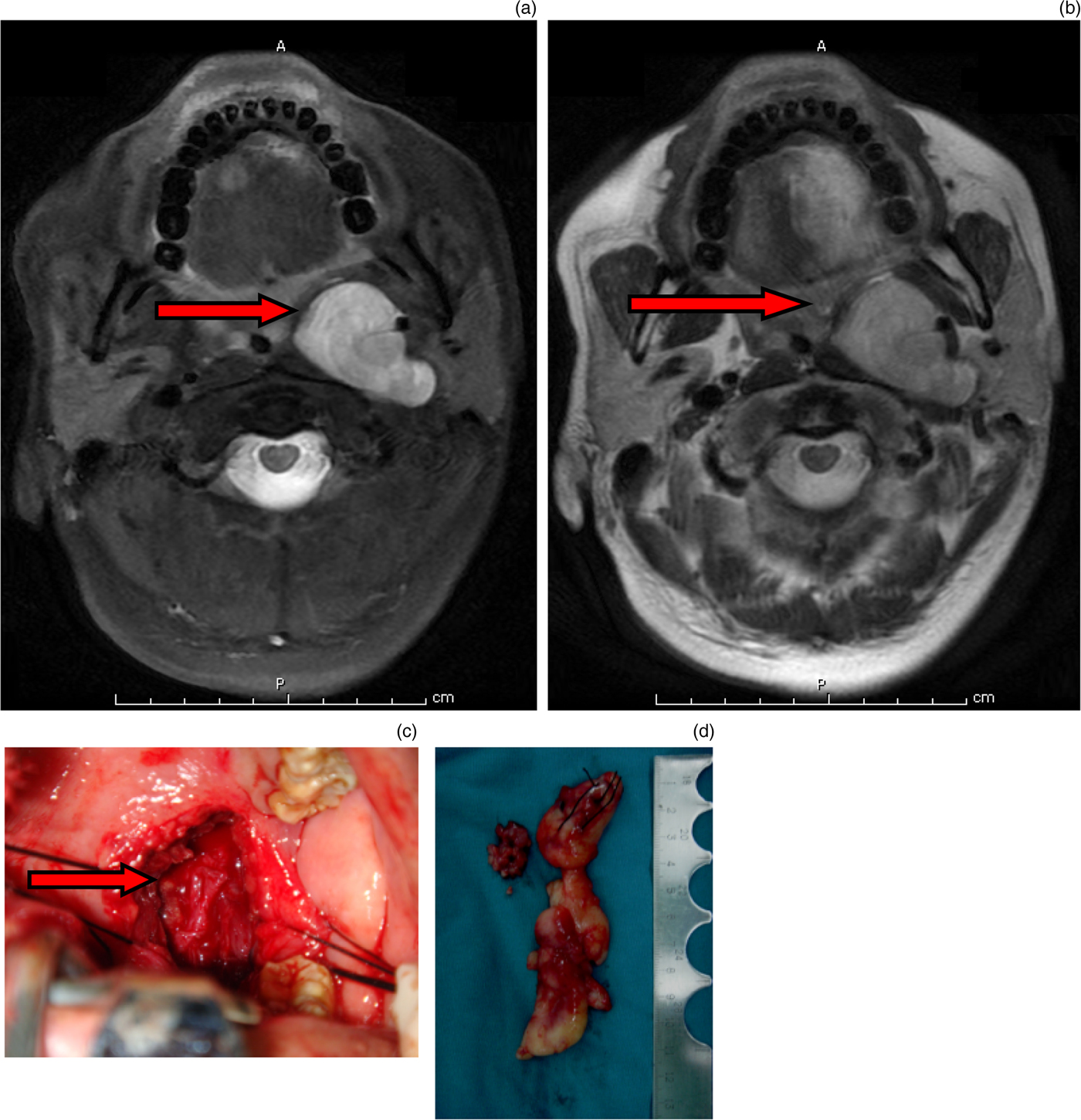
Fig. 2. A case of a neurofibroma. (a) A T2-weighted magnetic resonance imaging (MRI) scan showed a hyperintense, well-defined mass in the left parapharyngeal space (red arrow indicates the neurofibroma). (b) A T1-weighted MRI after the mass was excised (red arrow indicates former location of the mass). (c) Intra-operative view of the left parapharyngeal space (indicated by the red arrow). (d) The excised mass. A = anterior; P = posterior
Discussion
Benign tumours are the most common lesions found in the parapharyngeal space. Manifestations include a mass in the oropharynx and/or upper neck, pain, trismus, change in voice, and so on.Reference Khafif, Segev, Kaplan, Gil and Fliss5, Reference Som, Biller and Lawson9, Reference Morfit10 For masses in the oropharynx, physical intra-oral examination usually reveals a very large and smooth submucosal mass that anteromedially displaces the lateral pharyngeal wall, tonsil and soft palate. Sometimes the masses are palpable from the outside.Reference Bozza, Vigili, Ruscito, Marzetti and Marzetti11 Pre-operative assessment typically includes an MRI and/or CT scan.Reference Bradley, Bradley and Olsen3, Reference Douville and Bradford12 Angiography is required in cases of vascular lesions, such as haemangiomas or tumours of neuroectodermal origin.Reference Bradley, Bradley and Olsen3
• The transoral approach is suitable for most benign parapharyngeal space tumours in medial portion of carotid sheaths extending toward skull base
• Endoscope-assisted transoral resection of large benign parapharyngeal space tumours is simple and safe
• Transoral and endoscope-assisted transoral approaches lead to good surgical results with an acceptable complication rate
For parapharyngeal space masses of a benign nature, the surgeon must carefully consider the surgical approach most likely to enable convenient removal of the tumour and decrease the incidence of complications. The more commonly used methods include transcervical, transparotid and transoral approaches, or a combination of these;Reference Cohen, Burkey and Netterville4, Reference Khafif, Segev, Kaplan, Gil and Fliss5 each approach can be used with the addition of mandibulotomy if necessary.
Currently, transoral approaches are seldom performed. Traditionally, the transoral approach was considered only in very select cases, because of the risk of haemorrhage and/or cranial nerve damage and tumour spillage.Reference Ducic, Oxford and Pontius6 Practitioners have even suggested abandoning this approach for the surgical treatment of parapharyngeal space tumours.Reference Allison, Van der Waal and Snow13 However, in our practice we have used this approach for benign tumours in the superomedial portion of the parapharyngeal space. The transoral approach described herein safely allowed for en bloc resection of most benign tumours in the parapharyngeal space, with extracapsular dissection.
There is some controversy about en bloc resection, and even extracapsular dissection, for pleomorphic adenomas in the parapharyngeal space, which has been associated with a higher rate of tumour recurrence.Reference Guntinas-Lichius14 There were five cases of pleomorphic adenoma removed by extracapsular dissection and seven cases removed by en bloc resection in this cohort, but there were no cases of recurrence after up to five years of follow up. Moreover, this approach provides access to some benign parapharyngeal space tumours, with a low rate of complications, and provides benefits by decreasing cosmetic and functional disability. However, determining the long-term effects of the transoral approach will require a study with a large sample size and long follow-up times.
Here, we provide some tips for the transoral approach based on our own experience. In most cases, general anaesthesia with orotracheal intubation should be adopted. However, if the tumour is larger than 6 cm in diameter, with pharyngeal stenosis and limited operative space, a preventive tracheostomy should be carried out to prevent upper respiratory tract obstructive dyspnoea post-operatively. Depending on the state of the post-operative patients with pharyngeal oedema, the tracheal tube should be pulled out about 3 to 5 days after the operation. After exposing the tumour, blunt dissection can be performed along the capsule (that is, ‘extracapsular dissection’); gentle separation is advocated to avoid damage to the surrounding structures, including nerves and veins. When bleeding appears, a bipolar device can be used for coagulation. When the tumour is larger than 5 cm in diameter, negative pressure drainage is required; this is helpful for preventing a haematoma in the parapharyngeal space and for preventing secondary infections.
The applications of endoscopy in nasal and thyroid surgical procedures are wide. We applied this technique to transoral resection in the parapharyngeal space. Endoscopy enabled improved lighting and surgical field exposure, and important anatomical structures adjacent to the tumours were clearly visible. Especially in the case of en bloc resection, endoscopic assistance helped to distinguish tumour tissue from normal tissue. However, pure transoral endoscopic resection of parapharyngeal space tumours was not carried out in this research cohort. That technique may require improvement of the surgical instruments. Endoscope-assisted transoral resection of large benign tumours of the parapharyngeal space, in our own experience, is a simple and safe technique.
This study has several limitations. Each type of lesion (similar tumours regarding histopathology, dimensions and location) was treated with the same type of approach, without a control group treated with other methods. The other important limitation is that the mean period of follow up (28 months) is too short to obtain reliable oncological outcomes. The main aim of this study was to provide indications and short-term outcomes related to the transoral approach, not to establish the superiority of the approach in terms of oncological results.
Conclusion
Our experience suggests that, in the surgical management of benign parapharyngeal space tumours, most tumours can be treated by a transoral approach or an endoscope-assisted transoral approach, especially when the tumours are located in the superomedial portion of the carotid sheaths and extend toward the skull base. In most cases, the transoral approach is suitable for the safe removal of even large parapharyngeal space masses. The approach typically leads to a good surgical result, with an acceptable number of complications. Certainly, the methodological limitations and the small sample size of our study do not allow us to draw any final conclusions on how precisely valuable the presented surgical technique is. In this study, we emphasise that the transoral approach should be performed in clinical studies with a better study design and better definition of the surgical technique.
Acknowledgement
This study was supported by the National Natural Science Foundation of China (grant numbers 81300812 and 81770982, awarded to author LY).
Competing interests
None declared




