Introduction
Paralysis of the facial nerve causes lagophthalmos and leaves the eye exposed. Lack of blinking and incomplete eyelid closure prevent the tear film from spreading evenly over the surface of the cornea, which subsequently becomes dry. This causes irritation and congestion of the eye, which can lead to corneal keratitis, ulceration, perforation or, in severe cases, even blindness.
Eyedrops and eye ointments are simple measures but are inconsistent in providing long term relief. Taping the eyelid at bedtime is also a temporary measure which offers unreliable results and hampers vision if used during the day.
Tarsorrhaphy has been one of the standard surgical procedures for management of the exposed eye. However, tarsorrhaphy restricts the field of vision, offers incomplete corneal protection and is cosmetically disfiguring. In addition, it can cause trichiasis or permanent adhesions. Reversal of tarsorrhaphy can result in persistent lid deformity.
Tantalum gauze mesh was used by SheehanReference Sheehan1 as early as 1950. Wire spring implantsReference Morel-Faio and Lalardrie2, Reference Levine, Tse and Wright3 were used to oppose the action of the levator muscle. However, comparison of the complications and failures of wire spring implants (including extrusions requiring removal) with the superior performance of gold eyelid implants suggest the latter as the preferred technique.Reference May4
Gold weight implantation in the upper eyelid was first described by Smellie,Reference Smellie5 and it is the most widely accepted and useful procedure to reanimate the paralysed eyelid.Reference Jobe6–Reference Linder, Pike and Linstrom9 The action of the orbicularis oculi on the affected side is substituted by a gold weight implanted in the affected eyelid; combined with the effect of gravity, this helps to shut the eye when the levator palpebrae relaxes. This procedure offers excellent protection to the eye and also very good cosmesis. It can be used as a temporary or permanent procedure.
From 1997 to 2005, we prospectively analysed 50 patients for whom a customised technique of gold eyelid implant preparation was employed.
Patients and methods
Following the granting of approval by the relevant institutional review board, a prospective study was conducted from January 1997 to December 2005. Fifty patients underwent upper lid gold weight implantation as treatment of lagophthalmos caused by facial palsy. Forty-eight of the patients were followed up for at least one year, and these patients form the main basis of this study. The aetiologies of patients' facial palsies are summarised in Table I.
Table I Aetiologies of patients' facial paralysis

Ca = cancer; CP = cerebellopontine
The patients ranged in age from 17 to 76 years, with a mean of 41 years. The male to female ratio was approximately 2:1. The time of implantation varied from four days to six years after onset of facial palsy. The indications for surgery were: established cases of facial palsy (recent or longstanding); a facial nerve weakness of House–Brackmann grade III or worse, with corneal exposure; patients in whom facial nerve recovery was expected to take substantial time; and those in whom end-to-end suturing of the facial nerve or facial–hypoglossal nerve anastomosis had been unsuccessfully attempted. In all cases, patients presenting with facial palsy were informed of the pressing need for early implantation. Also included in the study group were four subjects in whom tarsorrhaphy had been performed but in whom symptoms had persisted.
Patients underwent ophthalmological evaluation, during which their corneal condition and visual acuity were determined. Patients were then divided into categories according to the severity of corneal involvement, as shown in Table II.
Table II Severity of patients' corneal involvement

Pre-operatively, the necessary implant weight was determined by taping the affected eye with chemistry laboratory microweights. The correct weight was that which enabled complete closure of the eye. The length of the eyelid was measured from medial to lateral canthus; two-thirds of this length was determined to be the optimum implant length. In adults, the medial end of the implant measured 5 mm and the lateral end 4 mm; this was proportionately decreased in children. The greater breadth at the medial end was based on our finding that a fractionally greater implant weight was required to close the medial end of the upper eyelid, compared with the lateral end. A thin, flexometallic strip was placed over the eyeball to determine its curvature. These measurements were then conveyed to a trained, licensed goldsmith, who prepared the implant from 24 carat gold (i.e. 99.5 per cent purity).
The goldsmith's technique was as follows. A 24 carat gold bar was melted and a sheet prepared of the required gauge. The necessary sheet gauge was calculated by taking into account the loss of gold in making and polishing the sheet and adding three holes for fixation to the tarsal plate, while still retaining the requisite weight. A paper drawing of the implant was prepared, using the dimensions provided, and the gold sheet cut and shaped as required. The implant edges were smoothed to reduce the risk of extrusion due to sharp edges. High buff polishing was applied until the implant weight exactly matched that required to close the eye. On average, two days were required to prepare each implant. The implant was then autoclaved for 20 minutes at 121–132°C and made ready for use (Figure 1).

Fig. 1 Customised gold eyelid implant. Note that the medial end is broader than the lateral end.
Such locally made implants were of the desired dimensions, and were also far more economical than commercially available implants. In addition, they had the advantage of being easily available at short notice, even in remote areas.
Two of the 50 patients also underwent a lower lid tightening procedure, in addition to the upper eyelid gold implant insertion.
Surgical technique
The procedure was performed under local anaesthesia. Three to four drops of 4 per cent xylocaine solution were instilled into the affected eye. A corneal guard was placed between the inner surface of the upper eyelid and the cornea, and the eyelid margin was sutured to the fixation holes in the guard. This helped to stretch the upper eyelid, in addition to protecting the cornea.
The incision site was determined, being approximately 6 mm from the lid margin and involving the middle third of the upper eyelid, preferably along a supratarsal skin fold if possible. The incision site was infiltrated with 2 cc of 1:200 000 xylocaine with adrenaline. The incision was extended to involve the skin and the orbicularis oculi. A pocket was created in the space between the orbicularis oculi and the tarsal plate for placement of the implant. It is important to note that the pocket was created inferior to the insertion of the levator palpebrae fibres on the tarsal plate.
The implant was then placed in this pocket, with the broader end medially. The implant was then sutured to the partial thickness of the tarsal plate with 6-0 monofilament sutures passed through the fixation holes in the implant. The orbicularis oculi was sutured with 5-0 vicryl and the skin with 6-0 ethilon. Subjects were followed up on day 7, 1 month, 3 months, 6 months and 1 year where symptoms, eye closure, corneal status and visual acuity were recorded.
Results
The mean weight of implants used in our series was 1.7 g. This contrasts with a mean weight of 1.2 g described for Western populations. The exact reason for this difference between Asian and Western populations requires further research.
Only patients with a mimimum of one year's follow up were included in the study. The mean palpebral aperture in 50 patients was 5.9 mm pre-operatively. Post-operatively, the upper and lower eyelids approximated completely in 34 patients (Figure 2). In 14 patients, a post-operative palpebral aperture of less than 1 mm persisted, exposing a thin margin of sclera. However, the cornea was covered in all cases.
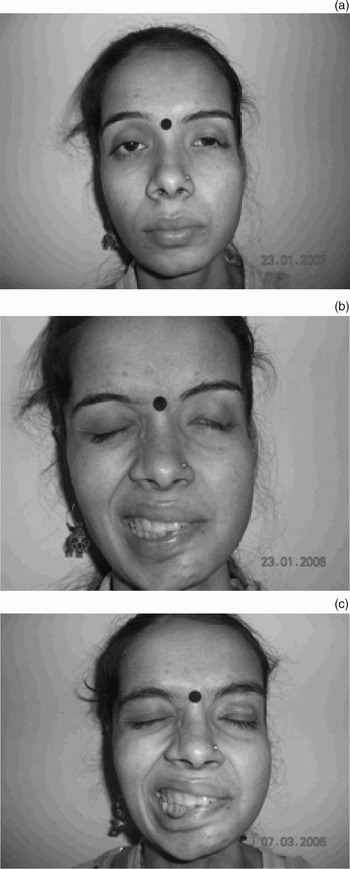
Fig. 2 (a) Pre-operative photograph showing lateral tarsorrhaphy of left eyelid, obscuring the patient's vision. (b) Incomplete eye closure. (c) Reversal of tarsorrhaphy with gold eyelid implantation. Published with patient's permission.
In two patients, the initial corneal coverage was complete, but the implant extruded within a month of surgery and was removed. During implant removal in one of these cases, the implant was found to be not securely fixed to the tarsal plate, resulting in displacement of the implant and subsequent extrusion. In the other case, a frail, 72-year-old patient, the orbicularis oculi was atrophic; hence, improper apposition of the orbicularis oculi following implant placement, combined with lax skin on the upper eyelid, were judged to be the causes of extrusion. These two patients were amongst the earliest cases treated; subsequently, no further extrusions occurred.
Forty-eight of the 50 patients underwent only upper eyelid gold implantation, whereas two patients required lower eyelid shortening in addition. Both these latter subjects were in their fifth decade of life. We observed that younger subjects did not appear to have lower eyelid lag, despite a reasonable duration of facial palsy.
Complete resolution of keratitis occurred in 46 of the 50 subjects (92 per cent), enabling these patients to dispense with eyedrops and ointments. In two subjects, deep corneal ulceration resolved, leaving corneal scarring which partially obscured vision. The two subjects whose implants extruded subsequently refused any further intervention, and resumed use of eyedrops and eyelid taping. Visual acuity improved in 46 of the 50 patients (92 per cent). None of the patients reported astigmatism following the procedure, after a minimum post-operative follow-up period of one year.
Discussion
Although eyedrops, ointments, eyelid taping, tarsorrhaphy, muscle transfers and spring wire implants have been used, gold eyelid implantation is the most favoured procedure for the treatment of paralytic lagophthalmos. In 1999, Tucker and SantosReference Tucker and Santos10 conducted a survey of North American otolaryngologists and ophthalmologists, and found that gold upper lid implantation was the procedure of choice for management of paralytic lagophthalmos. The procedure gives immediate results, is cosmetically pleasing, and can be used as a temporary or permanent treatment.
• Gold upper eyelid implantation is the procedure of choice for management of paralytic lagophthalmos
• Commercially produced gold implants are expensive and not widely available
• The authors describe a method in which gold upper eyelid implants were custom-made according to individual patient dimensions, enabling a more accurate weight than that possible with commercial implants
• This method was successfully used in 48 of 50 patients with facial paralysis (2 extrusions)
The advantage of customised gold implants lies in their easy availability within the local area, even in remote places. Considering the time required to despatch gold implants to the many regions around the world in which they are not readily available, a method of creating customised gold implants offers significant benefits. Locally prepared implants are also far more cost-effective than imported ones. Autoclaving the implant ensures its sterilisation.
Our results are comparable to those of most published studies.Reference Kartush, Linstrom, McCann and Graham8, Reference Linder, Pike and Linstrom9, Reference Chepeha, Yoo, Birt, Gilbert and Chen11, Reference Harrisberg, Singh, Croxson, Taylor and McCluskey12 Hence, we conclude that customised gold eyelid implants offer an alternative to commercially produced implants.






