Introduction
Stapes surgery was introduced by Shea in 1956. Since then, the classical stapes operation has undergone numerous modifications.Reference Poe1 Most centres in the world are currently performing stapedotomies and stapedectomies under a microscope, with good surgical outcomes.
Surgical microscopes provide tunnel vision with a good quality magnified image. The tunnel vision limits visualisation of the tympanic membrane and middle-ear structures in an exclusive transcanal approach in the narrowest segment of external auditory canal. Limitations of the microscope increase in tortuous canals, often resulting in the requirement of an endaural or post-aural approach.
A transcanal approach performed under a microscope limits visualisation of the stapes supra-structure, particularly the anterior crus of the stapes. This often forces the surgeon to blindly fracture the anterior crus.Reference Nogueira Júnior, Martins, Aguiar and Pinheiro2
The advantages of using endoscopes in ear surgery are mainly related to providing clear, high quality images, and the visualisation of poorly seen structures such as the sinus tympani and hypotympanum. Additionally, use of an endoscope helps in bypassing a narrow isthmus in a transcanal approach, resulting in better visualisation of middle-ear structures.Reference Sarkar, Banerjee, Chakravarty, Singh, Sikder and Bera3
Many reports of endoscopic ear surgical procedures discuss the use of otological endoscopes that are less than or equal to 3 mm in diameter.Reference Poe1, Reference Yadav, Aggarwal, Julaha and Goel4–Reference Karhuketo and Puhakka6 A smaller diameter of otological endoscopes as compared to routinely used sinonasal endoscopes of 4 mm restricts the visual field.
Our study aimed to assess the advantages and disadvantages of using sinonasal 4 mm endoscopes for stapedotomy over a conventional microscopic procedure.
Materials and methods
The study was conducted at a tertiary care centre between 2014 and 2016, and included 40 patients with otosclerosis. Inclusion criteria were: patients diagnosed with otosclerosis based on clinical history; an intact tympanic membrane; audiometric tests showing conductive hearing loss with an air–bone gap larger than or equal to 30 dB, no stapedius reflex, and with normal bone conduction values at 0.5, 1, 2 and 4 kHz; no past history of middle-ear infectious diseases; and an intact ossicular chain with stapes footplate fixation intra-operatively. Exclusion criteria were: a past of middle-ear infectious disease; changes seen upon otoscopy, such as tympanic membrane perforation; and pure tone audiometry showing conductive hearing loss with an air–bone gap of less than 25 dB.
Patients were alternately distributed into the endoscopy and microscopy groups by a resident unaware of the study aims, to achieve a 20/20 distribution of cases in each group. Patients were first divided into two groups: one comprised patients with a narrow external auditory canal, and the other included patients with a normal or wide external auditory canal. The external auditory canal was labelled as narrow if all quadrants of the tympanic membrane were not visible in a single view while performing examination under a microscope in the out-patient department. Every alternate patient was then chosen to undergo an endoscopic or a microscopic approach. Randomisation and allocation were concealed from the operating surgeon. Written informed consent was obtained from all patients before surgery; the possibility of endaural incision was explained to each patient. All surgical procedures were performed by one operating surgeon with an assistant surgeon.
Intramuscular pre-medication in the form of injections of pentazocine (30 mg) and promethazine (25 mg) was given to patients half an hour before surgery. All the patients were operated on under local anaesthesia (xylocaine 2 per cent with 1:100 000 adrenaline). Transcanal injections were given in all four quadrants of the external auditory canal with a 26-gauge needle.
The variables recorded pre-operatively were: age and sex of the patient, the presence of bony overhangs obscuring a complete view of the tympanic membrane, and pure tone audiogram parameters. Intra-operative variables recorded were: canal incision, canalplasty performed to reduce overhangs, manipulation of the chorda tympani, curettage of the postero-superior canal wall for the assessment of ossicular status and adequate exposure, adequate visualisation to permit stapes footplate perforation before stapes supra-structure removal, and operative time. The post-operative variables recorded included pure tone audiogram parameters and pain.
Endoscopic stapedotomies were performed using 4 mm, sinonasal, wide-angle, 0-degree and 30-degree Hopkins telescopes that were 18 cm in length. Video equipment consisted of a video camera and a monitor. All procedures were performed directly off the monitor, which was placed opposite the surgeon and was positioned across the patient's head. The endoscope was held in hand; no stand was used to hold the endoscope. Microscopic stapedotomies were performed using a Zeiss microscope (Carl Zeiss Meditec, Jena, Germany). Magnification used was 6× for canal work and 10× for middle-ear work.
An endomeatal incision was made in the external auditory canal, comprising a circumferential incision between the 6-o'clock and 12-o'clock positions, about 6 mm lateral to the tympanic annulus. An endaural incision was required in four patients in the microscopy group. After raising the tympanomeatal flap, the middle ear was inspected for ossicular continuity and mobility. The postero-superior canal wall was curetted to achieve adequate exposure, with visualisation of the tympanic segment of the facial nerve and base of pyramid (Figure 1). Special attention was given to looking for prolapse of the facial nerve over the stapes footplate, dehiscent tympanic segment of facial nerve and persistent stapedial artery. The distance between the undersurface of the long process of the incus and stapes footplate was measured, and a Teflon stapes piston with an additional 0.25 mm length was cut. All pistons used were of 0.6 mm diameter.
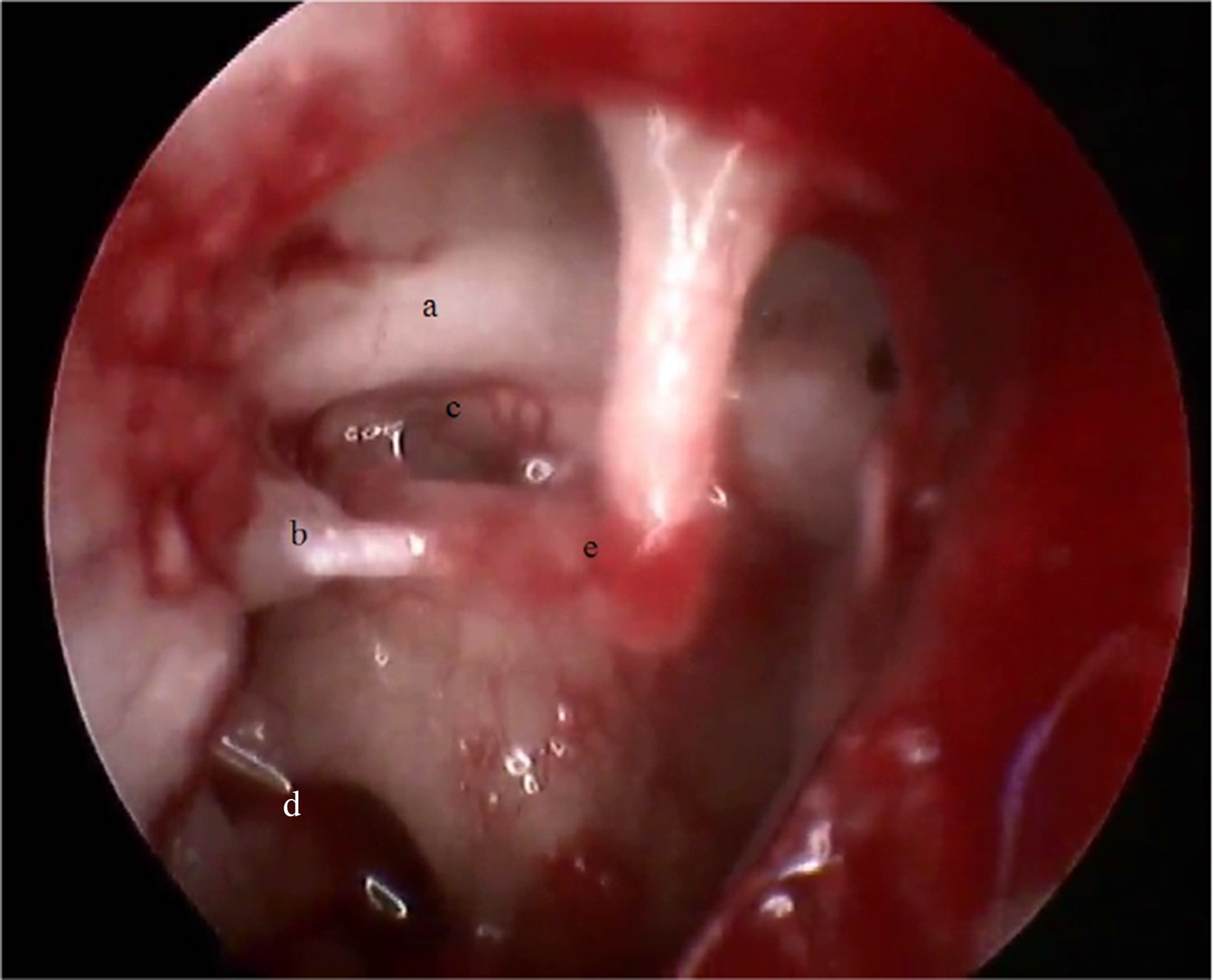
Fig. 1. Endoscopic image demonstrating exposure for endoscopic stapedotomy, with visualisation of tympanic segment of facial nerve (a), pyramid (b), stapes foot plate (c), round window niche (d) and incudostapedial joint (e).
An attempt was made to perforate the stapes footplate with an 0.8 mm perforator before removing the stapes supra-structure (Figure 2). In cases where this could not be done, the footplate was perforated after removing the stapes supra-structure. In these latter cases, the incudostapedial joint was dislocated using a 90-degree pick followed by crurotomy using crurotomy scissors or a 90-degree pick (Figure 3), and the stapes supra-structure was removed after cutting the stapedial tendon using micro scissors. The piston was inserted in the footplate perforation and hooked onto the long process of the incus (Figure 4). The perforation was sealed by a drop of blood.

Fig. 2. Endoscopic view of stapes footplate perforation with 0.8 mm perforator, with intact stapes supra-structure.

Fig. 3. Endoscopic image of crurotomy with 90-degree pick, with anterior (a) and posterior crus (b) under visualisation, with intact stapedius (c).
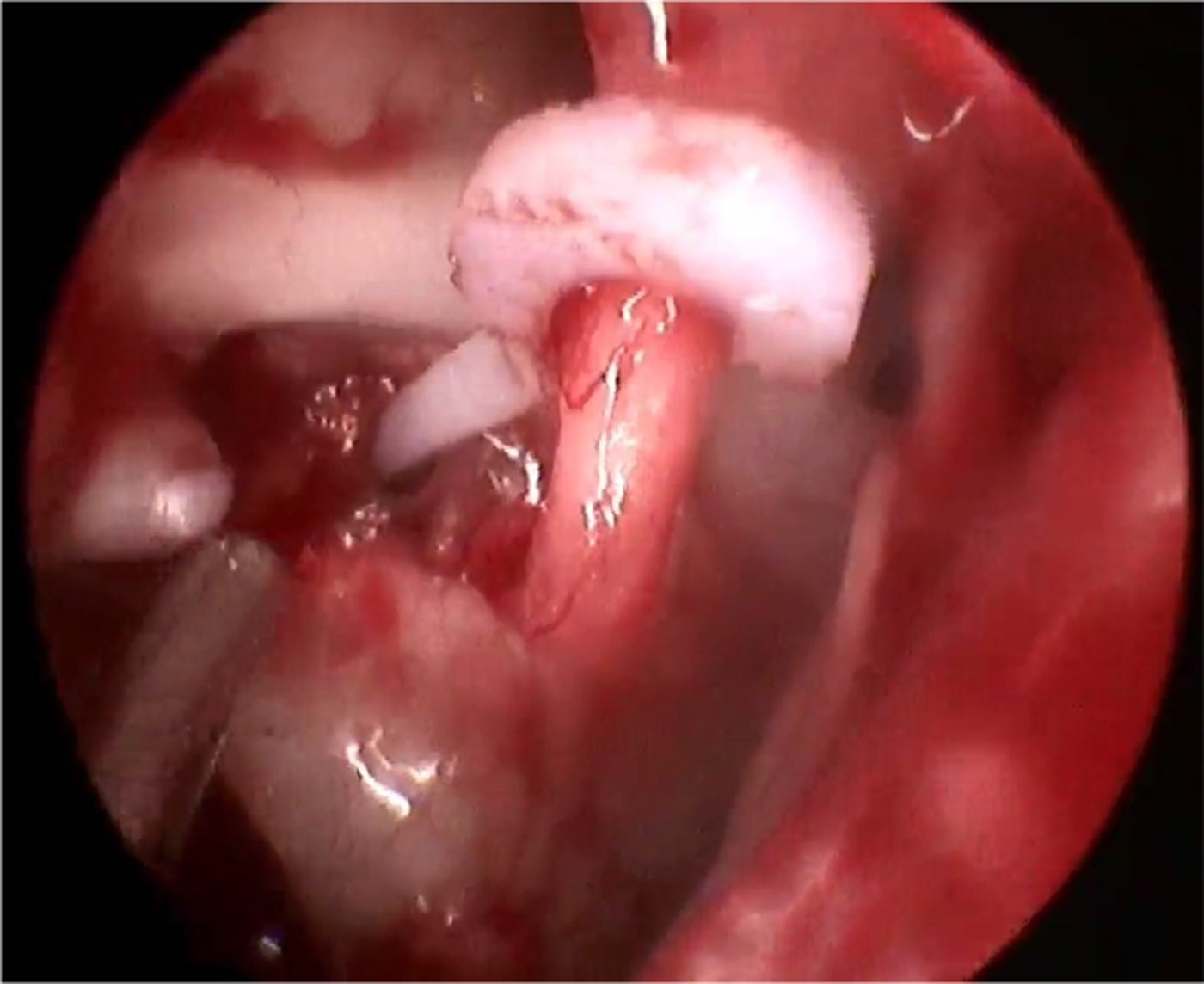
Fig. 4. Endoscopic view of Teflon piston in situ.
The tympanomeatal flap was reposited and the external auditory canal was packed with medicated Gelfoam. In cases with an endaural incision, the incision was sutured laterally using size 3-0 silk, and the canal was packed with medicated Gelfoam and umbilical tape.
Patients were discharged on the following day and recalled for serial post-operative visits at 1, 3, 12 and 24 weeks.
Data were analysed using SPSS® (version 16) statistical software with the student's t-test and Mann–Whitney U test.
Results
The youngest patient was 18 years old and the oldest was 48 years. Forty stapedotomies were performed in 37 patients; 34 of those individuals underwent unilateral surgery, and 3 underwent bilateral surgery with an interval of at least six months.
The mean age of patients was 33.10 years in the endoscopy group and was 32.9 years in the microscopy group, with no significant difference between groups. In the endoscopy group, 40 per cent of patients were female, compared with 45 per cent in the microscopy group, with no significant difference.
All patients had bilateral disease, except one, who was operated on endoscopically. Seven patients had a narrow external auditory canal, three in the endoscopy group and four in the microscopy group; those in the microscopy group needed endaural incision for adequate surgical access.
In the endoscopy and microscopy groups, three and four patients respectively had significant canal overhangs (p > 0.05). The overhangs were most commonly in the postero-superior and postero-inferior regions. No patient in the endoscopy group required canalplasty, and adequate exposure was obtained with the 0-degree endoscope. All four patients in the microscopy group underwent canalplasty for adequate exposure.
The 0-degree and 30-degree endoscopes provided an adequate view of the incudostapedial joint complex, and helped in assessing ossicular continuity and mobility without the need for any postero-superior canal wall curettage. In contrast, canal wall curettage was required in seven patients in the microscopy group (p = 0.008). One patient who satisfied the inclusion criteria pre-operatively was excluded from the study based on an intra-operative endoscopic finding of lenticular process erosion. A refashioned incus was used to restore ossicular chain continuity in this patient.
Equal curettage of the postero-superior canal wall was carried out in both groups of patients to enable further instrumentation in the middle ear. Curettage was conducted until adequate exposure was achieved (i.e. the facial nerve and pyramidal process were visible). For the endoscopy group, this was determined by keeping a 0-degree endoscope lateral to the tympanic annulus and then assessing the view on screen.
The chorda tympani was manipulated in 6 of the 20 patients in the endoscopy group (30 per cent) and in 13 of the 20 patients in the microscopy group (65 per cent) (p = 0.026). It was not transected in any of the cases.
Perforation of the stapes footplate before disturbing the stapes supra-structure was performed in 11 of the endoscopy group patients (70 per cent) and in 5 of the microscopy group patients (25 per cent) (p = 0.025).
A persistent stapedial artery, perilymph gusher and floating footplate were not seen in any of the patients.
Duration of endoscopic stapedotomy ranged from 50 to 102 minutes, with a mean of 76.05 minutes; duration of microscopic stapedotomy ranged from 40 to 60 minutes, with a mean of 50.25 minutes (p = 0.0001). Duration of endoscopic stapedotomies performed initially were higher as compared to those performed later. There was no iatrogenic facial injury.
Post-operative vertigo was encountered in three endoscopy group patients and in four of the microscopy group patients (p = 1). Vertigo resolved within 8 hours of surgery with conservative management in all except one patient in the microscopy group. This latter patient received tablet prochlorperazine 25 mg twice daily for one week for resolution of the post-operative vertigo.
None of the patients had a tear in the tympanomeatal flap intra-operatively. The tympanic membrane was intact in all patients post-operatively.
Air–bone gap closure after stapedotomy was seen in 18 and 17 patients in the endoscopy and microscopy groups respectively, with no significant difference between the two groups (p = 0.67). The mean post-operative air–bone gap was 10.73 dB in the endoscopy group and 13.81 dB in the microscopy group (Table 1).
Table 1. Comparison of pre- and post-operative air–bone gaps for each technique*

* p = 0.67. SD = standard deviation; SEM = standard error of mean; ABG = air–bone gap
None of the patients complained of taste change post-operatively. Four patients who required endaural incision complained of pain post-operatively; these patients were given tablet paracetamol (500 mg) twice daily for 10–14 days post-operatively for pain relief.
Discussion
The use of endoscopes in ear surgical procedures has increased in recent times. Endoscopes have revolutionised otitis media surgery, playing a significant role in the management of tympanic membrane perforation, cholesteatoma, sinus tympani disease and facial nerve surgery.Reference Lade, Choudhary and Vashishth7–Reference Marchioni, Alicandri-Ciufelli, Piccinini, Genovese, Monzani and Tarabichi13 However, there is still resistance to use of an endoscope in stapes surgery. Mandatory single-handed instrumentation in endoscopic ear surgery mostly forces otologists to use a microscope for stapedotomy.
The panoramic view provided by a 0-degree rigid endoscope, coupled with a 30-degree telescope, provides excellent visualisation of the ossicular chain, stapes crura, facial nerve and pyramid, even in the presence of bony overhangs.
Microscopic stapedotomy is a time-tested procedure, with good audiological outcomes. Disadvantages of the microscope, such as restricted visualisation in the narrow canal, the occasional requirement of endaural or post-aural incision, and non-visualisation of the anterior crus, has made otologists keen to explore the role of the endoscope in stapedotomy.
As happens with all surgical procedures, endoscopic ear surgery has a learning curve, but slightly longer. As in our study, performing endoscopic stapedotomy mandates previous experience in endoscopic tympanoplasties and endoscopic sinus surgical procedures.
In the current study, the mean operative times for endoscopic and microscopic stapedotomies were 76.05 and 50.25 minutes respectively. Operative time for endoscopic stapedotomy gradually decreased as surgeons gained experience, with the mean operative time of the last four cases falling in the same range as those of microscopic stapedotomies (Figure 5). This is in accordance with a study by Iannella and Magliulo, which mentions the learning curve and a higher mean operative time for endoscopic stapedotomies.Reference Iannella and Magliulo14 All the surgical procedures in our study were carried out by the same surgeon. While the surgeon was trained in microscopic ear surgery and endoscopic tympanoplasty, endoscopic stapes surgery was new to him. This is reflected in the operating times. This learning curve is present with most surgical skills, and is different for each individual. However, with the increasing use of endoscopes in nasal surgical procedures and in the out-patient department setting, surgeons are growing more comfortable with handling endoscopes. The findings in our study are an indicator of this, and they may vary from individual to individual.

Fig. 5. Line graph comparing operative time of the endoscopic and microscopic groups.
Canal overhang often requires canalplasty and conversion to an endaural approach. In the current study, four patients (20 per cent) with canal overhang required canalplasty and endaural incision in the microscopy group. None of the patients in the endoscopy group required canalplasty or an endaural incision, despite three patients having significant canal overhang, and the overhangs could be negotiated with the 0-degree endoscope without compromising exposure. In a study by Sproat et al., 34 per cent of patients required an endaural incision in the non-endoscopic stapedotomy group versus no patients in the endoscopic group.Reference Sproat, Yiannakis and Iyer15
Use of an endoscope helps in assessing ossicular chain continuity, without the need of postero-superior canal wall curetting. Seven patients in the microscopy group needed curettage of the postero-superior canal wall for assessment of ossicular continuity versus no patients in the endoscopy group, which is statistically significant (p = 0.008). An endoscope can help to rule out other possible causes of conductive hearing loss with a similar presentation without the need of curettage of the postero-superior canal wall.
Overstretching and trans-section of the chorda tympani during ear surgery has been reported to result in taste changes.Reference Michael and Raut16 The chorda tympani often obscures visualisation of the surgical field during stapedotomy, necessitating its manipulation many times and transection rarely. In the current study, the chorda tympani was manipulated in 6 and 13 patients in the endoscopy and microscopy groups respectively, which is statistically significant (p = 0.026). It is noteworthy that none of these cases developed a change in taste sensation post-operatively. This is in accordance with a study by Nogueira Júnior et al., who reported very little or no manipulation of the chorda tympani in endoscopic stapedotomy.Reference Nogueira Júnior, Martins, Aguiar and Pinheiro2
Adequate surgical exposure with visualisation of the tympanic segment of the facial nerve and base of pyramid necessitated significant curettage of the postero-superior canal wall in the microscopy group, but minimal curettage in the endoscopy group because of the wide-angle view of the endoscope. However, this visualisation did not translate into adequate access for stapes footplate work, requiring further curettage. A study by Tarabichi mentioned a similar finding of adequate visualisation but inadequate access by minimal curettage in the endoscopy group.Reference Tarabichi17 The study by Nogueira Júnior et al. reported no or minimal curettage requirements.Reference Nogueira Júnior, Martins, Aguiar and Pinheiro2
Stapes footplate perforation before its supra-structure removal could be performed in 11 patients in the endoscopy group and in 5 patients in the microscopy group, which is a statistically significant difference (p = 0.025). This can be attributed to the wide angle and close-up visualisation provided by the endoscope. Stapes supra-structure removal before its footplate perforation negates the complication of a floating footplate. A floating footplate was not encountered in any of the patients in the current study.
Facial nerve function was intact in all patients in this study. The endoscopy group patients did not complain of post-operative pain, but this was felt in four microscopy group patients. The difference was statistically insignificant (p = 0.10). The patients complaining of post-operative pain were those who underwent an endaural incision during the procedure. This highlights the advantage of using an endoscope for performing stapedotomy, with a minimal incision even in a narrow canal, resulting in fewer complaints of post-operative pain.
There was no statistically significant difference in post-operative air–bone gap closure between the two groups. In effect, hearing improvement after stapedotomy depends upon piston placement, piston length, perilymph leak, piston displacement and erosion of the long process of the incus, rather than the use of a microscope or endoscope. Endoscopes aid the visualisation of key structures, such as the ossicles and facial nerve, especially in narrow canals, they involve a minimal incision approach, and they improve exposure, footplate fenestration and piston placement.
• The hearing outcomes for microscopic or endoscopic stapedotomy approaches are comparable
• Operative time and canal wall curettage findings are variable
• The endoscopic approach has a learning curve
• A 4 mm sinonasal endoscope used with conventional instruments provides a good outcome in stapedotomy
• An endoscopic approach is better for: minimal incision, avoiding canalplasty, less chorda tympani mobilisation and stapes footplate perforation before supra-structure removal
• Minimal curettage of the canal wall provides adequate visualisation but inadequate access for an endoscopic approach
Limitations of the present study include the relatively small sample size, restricting generalisation of the findings.
Conclusion
Endoscopic stapedotomy is an effective and promising alternative to the traditional microscopic technique, and leads to comparable outcomes in terms of hearing. A sinonasal (4 mm) endoscope may serve as a better tool in terms of: a minimal incision approach and the avoidance of canalplasty (improving patients’ comfort post-operatively, especially in narrow canals), less chorda tympani mobilisation, and the ability to perform stapes footplate perforation before supra-structure removal. Minimal curettage of the postero-superior canal may provide adequate visualisation, but not adequate access for an endoscopic approach using traditional instruments. An endoscopic approach has a learning curve and any resistance to it is unwarranted.
Competing interests
None declared








