Introduction
Hereditary haemorrhagic telangiectasia is an autosomal dominant disease characterised by angiodysplasia of the skin, mucous membranes and viscera. Fragility of the blood vessels results in bleeding following minimal trauma. This is caused by mutations that downregulate genes in the transforming growth factor beta signalling pathway.
Epistaxis is the most common manifestation of bleeding in hereditary haemorrhagic telangiectasia patients, with 96 per cent of patients suffering from recurrent epistaxes at some point in their lives.Reference Plauchu, de Chadarévian, Bideau and Robert1 Recurrent persistent epistaxis from hereditary haemorrhagic telangiectasia is associated with iron deficiency anaemia, admission to hospital for blood transfusion and chronic nasal crusting. Studies have shown significantly reduced quality of life scores for patients suffering from hereditary haemorrhagic telangiectasia.Reference Geirdal, Dheyauldeen, Bachmann-Harildstad and Heimdal2
Initial assessment
History and examination
A medical history should be taken covering the frequency and duration of epistaxis. It is important to document the natural history of epistaxis up to the present because a progressive increase in frequency and severity occurs in some patients. Other key points include the number of hospital admissions with severe epistaxis, number of blood transfusions and interval between blood transfusions. We recommend the use of the epistaxis severity score questionnaire, which is specifically validated for assessing epistaxis in hereditary haemorrhagic telangiectasia and helps to categorise symptoms as mild, moderate or severe (Figure 1, Table I).Reference Hoag, Terry, Mitchell, Reh and Merlo3 A careful non-traumatic examination of the nasal airway for areas of treatment should be carried out in the out-patient setting. A combination of anterior rhinoscopy and cautious use of a 0–30° rigid endoscope can provide information on which areas are amenable to treatment. There is some evidence that telangiectasiae occupying multiple nasal subsites predispose to more severe epistaxis and that larger prominent telangiectasiae are associated with more frequent bleeding.Reference Pagella, Colombo, Matti, Giourgos, Tinelli and Olivieri4
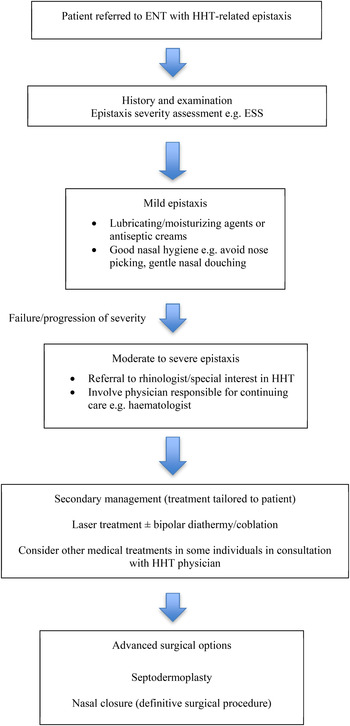
Fig. 1 Flow chart illustrating the epistaxis severity score system for grading epistaxis in HHT.3 ESS = epistaxis severity score; HHT = hereditary haemorrhagic telangiectasia.
Table I Epistaxis severity score*

* Answer the following questions as they pertain to your typical symptoms within the last three months for nose bleeding. The total = raw epistaxis severity score. Normalised epistaxis severity score = (Raw epistaxis severity score / 2.81) × 10. 1–4 = mild epistaxis; 4–7 = moderate epistaxis; 7–10 = severe epistaxis.
Although epistaxis may be the only manifestation of hereditary haemorrhagic telangiectasia, it is important to ensure close collaboration with other clinicians involved in the care of the patient, such as haematologists.
Medical treatments
Nasal packing
The traditional role of packing is to provide tamponade to bleeding vessels and reduce dead space in the nasal cavity to allow haemostasis. However, epistaxis in hereditary haemorrhagic telangiectasia is caused by multiple bleeding telangiectasiae which are not compressible in the same way as blood vessels. The use of nasal packing to treat hereditary haemorrhagic telangiectasia related epistaxis has traditionally been discouraged if avoidable because of the risk of exacerbating bleeding from local trauma when packing and from bleeding to the trauma when removing packing.
No clinical trials have investigated the efficacy of packing in hereditary haemorrhagic telangiectasia. Anecdotal evidence supports the use of alginate dressing as an atraumatic haemostatic plug for treating minor recurrent epistaxis. In cases of acute bleeding, we advocate the use of minimal atraumatic packing such as alginate dressings to provide a haemostatic plug for bleeding telangiectasiae. If standard nasal packing is required, we suggest using a lubricated low-pressure pneumatic packing to reduce the likelihood of rebleeding on removal.Reference Faughnan, Palda, Garcia-Tsao, Geisthoff, McDonald and Proctor5
Moisturising and anti-microbial agents
No trials have investigated the use of simple moisturising agents or antiseptic creams to treat epistaxis in hereditary haemorrhagic telangiectasia. The use of vaseline or mupirocin ointment may moisturise the nose interior, thus reducing the propensity to bleed from a dry telangiectatic nasal airway.Reference Faughnan, Palda, Garcia-Tsao, Geisthoff, McDonald and Proctor5 Gentle saline douching may help to clear clots, and forceful nose blowing, which can easily precipitate epistaxis, should be avoided.
Silver nitrate cautery
The use of silver nitrate sticks for chemical cauterisation of vessels to treat recurrent epistaxis is well established. No randomised trials have investigated the use of silver nitrate cautery in the treatment of hereditary haemorrhagic telangiectasia specific epistaxis. There is low-level evidence that silver nitrate cautery provides a poorer outcome in hereditary haemorrhagic telangiectasia related epistaxis, with higher rates of intra-operative bleeding.Reference Faughnan, Palda, Garcia-Tsao, Geisthoff, McDonald and Proctor5
Silver nitrate cautery is likely to be associated with increased crusting and may be more traumatic than other methods of endonasal coagulation. The long-term risk of septal perforation may also be a concern with repeated bilateral cautery. There should be a low threshold for considering other less traumatic methods of endonasal coagulation when there is a failure to respond to treatment.
Topical oestrogen
One prospective, uncontrolled trial has described the reduced frequency and severity of epistaxis following the use of topical oestriol combined with argon plasma coagulation to treat hereditary haemorrhagic telangiectasia related epistaxis. No articles have compared topical oestrogen therapy with controls or any other treatment modality.Reference Sadick, Naim, Oulmi, Hörmann and Bergler6
There is currently insufficient evidence to support a role for topical oestrogen therapy to treat hereditary haemorrhagic telangiectasia related epistaxis.
Tranexamic acid
There is evidence of local hyperfibrinolysis in hereditary haemorrhagic telangiectasia lesions mediated by an increased level of tissue plasminogen activator.Reference Kwaan and Silverman7 This provides a partial rationale for using tranexamic acid to treat hereditary haemorrhagic telangiectasia lesions.
Two case reports have described a beneficial role for topical tranexamic acid in treating hereditary haemorrhagic telangiectasia related epistaxis.Reference Klepfish, Berrebi and Schattner8, Reference Flanagan, Collins and Parra9 A small case series showed control of epistaxis in three patients treated with up to 4.5 g tranexamic acid in divided doses.Reference Sabbà, Gallitelli and Palasciano10
There is low-level evidence for a role for topical and oral tranexamic acid in treating hereditary haemorrhagic telangiectasia epistaxis.
Bevacizumab
Bevacizumab is a monoclonal antibody inhibitor of vascular endothelial growth factor. Intranasal bevacizumab via submucosal injection and topical therapy can significantly reduce the epistaxis severity score for up to 12 months.Reference Karnezis and Davidson11 The use of low-dose intranasal bevacizumab in addition to laser treatment is superior to laser treatment alone.Reference Karnezis and Davidson12, Reference Rohrmeier, Sachs and Kuehnel13 Injection of the cartilaginous septum was found to increase the risk of septal perforation. Therefore, a modified strategy of a four-point injection in the sphenopalatine area, upper part of the bony septum, upper part of the lateral nasal wall and the anterior part of nasal floor has been successfully adopted.Reference Chen, Karnezis and Davidson14, Reference Dheyauldeen, Østertun Geirdal, Osnes, Vartdal and Dollner15
In the UK, off-label treatment of 3 patients with intranasal bevacizumab was associated with a reduction in the epistaxis severity score from 8.8 to 4.3 and a reduction in the duration of epistaxis from 35 to 4 minutes within 3 months of starting treatment.Reference Alderman, Corlett and Cullis16
The North American Study of Epistaxis in Hereditary Haemorrhagic Telangiectasia (the ‘NOSE’ study; NCT01408030) is a randomised, placebo-controlled, double-blinded, trial evaluating the treatment efficacy of bevacizumab versus topical oestrogen versus topical tranexamic acid versus saline spray. There is growing evidence suggesting a role for bevacizumab in the treatment of hereditary haemorrhagic telangiectasia epistaxis. The results of the North American Study of Epistaxis in Hereditary Haemorrhagic Telangiectasia study will be useful for making more reliable conclusions about the benefits of these treatments.
Systemic oestrogen and anti-oestrogen treatments
Oestrogen therapy has been proposed for treating North American Study of Epistaxis in Hereditary Haemorrhagic Telangiectasia epistaxis because it is hypothesised that the ability of oestrogen to promote squamous epithelial metaplasia protects against telangiectasia breakdown and bleeding.
There has been only one randomised, double-blinded, controlled trial of single agent oestrogen (estradiol valerate), and no difference was seen between treatment group and placebo.Reference Vase17 Oral contraceptive combinations of estrogen and progesterone and single agent progesterone have been shown in small, uncontrolled trials to reduce epistaxis frequency.Reference Flessa and Glueck18, Reference Richtsmeier, Weaver, Streck, Jacobson, Dewell and Olson19 A randomised, double-blinded, placebo-controlled trial showed improved quality of life scores, reduced bleeding time and higher haemoglobin concentration following treatment with 20 mg/day tamoxifen for six months.Reference Yaniv, Preis, Hadar, Shvero and Haddad20 A follow-up study by the same group with an additional 25 patients also showed an improved quality of life and reduced epistaxis severity and frequency.Reference Yaniv, Preis, Shevro, Nageris and Hadar21
In cases of severe epistaxis refractory to other treatments, it would seem reasonable to suggest the combined oral contraceptive pill for fertile women. This decision should be made in consultation with the North American Study of Epistaxis in Hereditary Haemorrhagic telangiectasia physician responsible and preferably also with a gynaecologist and primary care physician. There is some evidence that tamoxifen (level Ib) and the oral contraceptive pill (level IV) have a role in the treatment of hereditary haemorrhagic telangiectasia epistaxis.
Local sclerotherapy
A recent non-randomised uncontrolled retrospective study examined 45 patients treated with monthly 0.5 per cent polidocanol injections infiltrated into the septum or telangiectasia area until a significant reduction in epistaxis had been achieved. All patients had grade 2–3 for frequency (several times per week, more than once per day) and 2–3 for intensity (soaked handkerchief or requiring bowl) on the Bergler–Sadick epistaxis scale. Epistaxis was reduced to grade1–2 (less than once a week, soaked handkerchief) in 73 per cent of cases, with an average of five to six infiltrations in each nasal cavity.Reference Morais, Millás, Zarrabeitia, Botella and Almaraz22 A small pilot study using intralesional sodium tetradecyl sulphate in an office-based setting reported a reduction in epistaxis frequency and the requirement of nasal packing.Reference Boyer, Fernandes, Duran, Hunter and Goding23
There is currently no consensus regarding treatment of hereditary haemorrhagic telangiectasia with any particular sclerosing agent. Evidence for the wide number of agents that have been investigated is limited to a few case series.
Surgical treatments
Diathermy
One case series has evaluated the use of bipolar diathermy for treating hereditary haemorrhagic telangiectasia related epistaxis. This was predominantly used as an adjunct to laser treatment or in the presence of larger conglomerate telangiectasia (level IV).Reference Ghaheri, Fong and Hwang24
There is limited evidence to support investigating the use of bipolar diathermy for treating hereditary haemorrhagic telangiectasia. However, there may be a role for bipolar diathermy as an adjunct to laser treatment to treat larger telangiectasiae not amenable to laser treatment alone.
Argon plasma coagulation
Argon plasma coagulation uses argon gas to deliver plasma of evenly distributed thermal energy to a field of tissue adjacent to a probe. A spark is delivered at the tip of the probe, which ionises the argon gas as it is sprayed from the probe tip towards the tissue. This ionised gas or plasma delivers the thermal energy with a penetration depth of a few millimetres.
A retrospective questionnaire study of 26 patients with severe epistaxis requiring blood transfusion who were treated with argon plasma coagulation suggested that this treatment reduced the number of blood transfusions required post procedure.Reference Pagella, Matti, Chu, Pusateri, Tinelli and Olivieri25 At the same institution, a retrospective analysis of 43 patients diagnosed with hereditary haemorrhagic telangiectasia reported substantially reduced bleeding in 36 patients after treatment. Of the 18 patients who had previously needed blood transfusions, 13 reported a substantial reduction in bleeding after treatment, with no blood transfusions necessary.Reference Pagella, Semino, Olivieri, Corno, Dore and Draghi26
The potential advantages of argon plasma coagulation include a reduced thermal energy and penetration depth or trauma compared with other electrocautery techniques. However, more studies are required before the use of argon plasma coagulation can be advocated as a first-line treatment for nasal telengiectasiae.
Coblation or radiofrequency
In a prospective pilot study of 16 patients using submucosal radiofrequency ablation under local anaesthesia, there was a reduction from 57.3 to 14.1 epistaxis events per month.Reference Mortuaire, Boute, Hatron and Chevalier27 In another small case series of five patients, epistaxis control was achieved by the elective treatment of nasal lesions in those with mild to moderate severity hereditary haemorrhagic telangiectasia (level IV).Reference Joshi, Woodworth and Carney28 It has been suggested that the lower operating temperatures of coblation compared with diathermy would reduce thermal injury and the resultant crusting and scarring.
Coblation treatment appears to be a feasible, less traumatic alternative to bipolar diathermy for treating mild to moderate hereditary haemorrhagic telangiectasia (level IV) epistaxis, particularly where laser treatment is not available. However, much more research is required to establish the long-term efficacy of coblation treatment.
Laser
Various laser therapy modalities have been used to treat hereditary haemorrhagic telangiectasia lesions in the nasal airway. Most reports involve the use of the potassium titanyl phosphate laser. The largest case series, including 268 potassium titanyl phosphate treatments on 131 patients, reported a reduction in epistaxis frequency following treatment, but the benefit was time limited.Reference Harvey, Kanagalingam and Lund29 A smaller study investigating the use of potassium titanyl phosphate laser with submucosal bevacizumab showed a significant reduction in the epistaxis severity score; unfortunately, there was no laser-alone arm to the trial.Reference Chen, Karnezis and Davidson14
A retrospective study using a non-validated questionnaire of 24 patients treated with a diode laser reported a decreased severity and frequency of epistaxis and an improved quality of life.Reference Fiorella, Lillo and Fiorella30 A case series of 27 patients treated with a neodymium-doped yttrium aluminium garnet (‘ND-YAG’) laser reported improved epistaxis control and an improved quality of life. Over a two-year period 30 per cent of patients required a single treatment, 56 per cent required two and 14 per cent required three.Reference Karapantzos, Tsimpiris, Goulis, Van Hoecke, Van Cauwenberge and Danielides31 The largest study examining the use of an argon laser showed reduced epistaxis in patients with mild to moderate severity hereditary haemorrhagic telangiectasia but little benefit to those with severe disease.Reference Lund and Howard32 A few smaller studies have cited similar benefits.Reference Haye and Austad33, Reference Bergler, Riedel, Baker-Schreyer, Juncker and Hörmann34 The pulsed dye laser has also been shown to be of some benefit for treating lesions in several small studies in both surgical and out-patient settings.Reference Harries, Brockbank, Shakespeare and Carruth35, Reference Hartnick, Dailey, Franco and Zeitels36
There is evidence supporting the use of laser treatment for telangiectatic lesions in the nose to reduce the severity and incidence of epistaxis (level IV). However, there is insufficient evidence to support a particular modality of laser therapy.
Septodermoplasty
Septodermoplasty involves removal of the mucosa from the anterior half of the septum, floor and lateral wall of the nasal airway with perichondrial preservation, followed by the placement of a tissue graft (usually a split-thickness skin graft).
A retrospective study of 29 patients showed no significant improvement in quality of life scores following septodermoplasty.Reference Hitchings, Lennox, Lund and Howard37 In a smaller study of nine hereditary haemorrhagic telangiectasia patients with severe transfusion-dependent epistaxis and septal perforations caused by other treatment modalities, combined septectomy and septodermoplasty did provide a long-lasting improvement in quality of life scores.Reference Lesnik, Ross, Henderson, Joe, Leder and White38
Septodermoplasty provides a time-limited reduction in epistaxis in hereditary haemorrhagic telangiectasia, but contributes to a significant reduction in the frequency of potassium titanyl phosphate laser treatments. There is some evidence that septodermoplasty is an effective treatment for moderate to severe epistaxis in hereditary haemorrhagic telangiectasia (level IV).
Nasal closure
Closure of the anterior nares (Young's procedure) is reported to best control severe hereditary haemorrhagic telangiectasia related epistaxis refractory to other treatments. In the largest case review, complete cessation of bleeding occurred in 30 out of 36 cases. This was associated with a mean increase in haemoglobin levels of 4.68 g/dL after the procedure.Reference Richer, Geisthoff, Livada, Ward, Johnson and Mainka39 Nasal closure was the only treatment for which the quality of life improvement was greater than that of argon laser and septodermoplasty.Reference Lund and Howard40 A modified Young's procedure using an alotomy incision for better exposure has also been shown to successfully treat severe hereditary haemorrhagic telangiectasia related epistaxis in a few short case series.Reference Gluckman and Portugal41, Reference Hosni and A Innes42
There is some evidence that nasal closure is the definitive surgical procedure for epistaxis control in hereditary haemorrhagic telangiectasia (level IV).
Interventional radiology
The role of selective endovascular embolisation in epistaxis treatment is limited to a number of small case series. Temporary relief was obtained in three out of five cases of hereditary haemorrhagic telangiectasia related epistaxis treated by superselective sphenopalatine artery ligation.Reference Strach, Schröck, Wilhelm, Greschus, Tschampa and Möhlenbruch43 Nasal tip necrosis and transient hemiparesis was reported in 2 cases out of 53 embolisations carried out to treat epistaxis of varying aetiology. Fourteen cases of severe hereditary haemorrhagic telangiectasia epistaxis unresponsive to nasal cautery and packing were treated by selective embolisation of branches of the external carotid artery. Recurrent bleeding occurred in 6 cases between 6 and 24 months post procedure.Reference Trojanowski, Jargiello, Trojanowska and Klatka44
There is insufficient evidence to advocate the role of selective embolisation over other treatment modalities.
Nasal obturators
The effectiveness of nasal closure in treating epistaxis has led to the investigation of reversible methods of nasal closure. Two small case series suggest a reduction in epistaxis frequency after the use of a silastic obturator.Reference Woolford, Loke and Bateman45, Reference Lobo, Hartley and Farrington46
There is insufficient evidence to advocate the routine use of a nasal obturator for the treatment of hereditary haemorrhagic telangiectasia related epistaxis. However, it would be reasonable to offer patients a trial of nasal obturator prior to nasal closure because it is a reversible, well-tolerated treatment modality with no adverse effects reported to date.
Conclusion
There is a lack of high-level evidence for the use of many of the available treatments for the specific management of epistaxis in hereditary haemorrhagic telangiectasia. Current management should be based on a multidisciplinary team approach involving both an hereditary haemorrhagic telangiectasia physician and an ENT surgeon, especially when systemic therapy is being considered. The suggested treatment algorithm considers that the degree of epistaxis severity merits intervention at different levels of the treatment ladder. Patients should be assessed using a reproducible validated assessment tool such as the epistaxis severity score to guide treatment.
More research is required, particularly into the use of topical agents targeting the development and fragility of telengiectasiae in hereditary haemorrhagic telangiectasia.




