Introduction
Cognitive behaviour therapy (CBT) is the first-line treatment for a range of different psychological problems including depression, generalized anxiety disorder, panic and agoraphobia, schizophrenia and eating disorders (NICE, 2004, 2009, 2011, 2013). There is growing evidence that this may be due, in part, to common cognitive-behavioural processes such as selective attention, rumination, avoidance, reassurance seeking and thought suppression that maintain psychological distress across disorders (Mansell et al. Reference Mansell, Harvey, Watkins and Shafran2008; Clark, Reference Clark2009).
Transdiagnostic theory exploring these commonalities has been the focus of a growing body of research. Mansell et al. (Reference Mansell, Harvey, Watkins and Shafran2008) outlined the advantages of a transdiagnostic approach stating that it can help to explain comorbidity of problems through the generalization of theories and understanding of specific problems to other disorders. It can also inform transdiagnostic interventions, of which there are several practical benefits. For example, interventions that are less disorder-specific and instead focus on common processes allow treatments to be offered in a group format, thus potentially reducing both costs and waiting times (Clark, Reference Clark2009).
There is now substantial evidence demonstrating the effectiveness of transdiagnostic interventions, in both group and individual format. Norton & Paulus (in press) recently reviewed the evidence of transdiagnostic interventions, namely transdiagnostic group CBT and the ‘Unified Protocol’, an individual intervention for emotional disorders based upon cognitive-behavioural approaches developed by Barlow et al. (Reference Barlow, Allen and Choate2004). They reported positive results of open trials and two randomized controlled trials (RCTs) of transdiagnostic group CBT which showed non-inferiority to diagnosis-specific group CBT and transdiagnostic group relaxation. Furthermore, data collapsed across open studies and RCTs suggested that transdiagnostic group CBT may be associated with superior results for comorbid anxiety symptoms when compared to disorder-specific CBT. The unified protocol intervention was also associated with positive results for emotional disorders, although it was noted that the number of studies of this approach was very small. Newby et al. (Reference Newby, McKinnon, Kuyken, Gilbody and Dalgleish2015) conducted a meta-analysis of transdiagnostic clinician-guided computerized or face-to-face psychological interventions for anxiety and depression in group or individual format. Using this broad criteria for interventions they included 50 studies, predominately exploring transdiagnostic CBT or CBT-informed interventions (n=40) with the remaining studies examining mindfulness or acceptance-based interventions or psychodynamic therapy. Overall, there were large, significant effects for anxiety and depression (g=0.87 and g=0.91, respectively).
In light of these positive findings for anxiety and depression, consideration has been given to the utility of transdiagnostic interventions for other diagnoses. For example, Larsen-Barr & Glynn Owens (Reference Larsen-Barr and Glynn Owens2013) conducted a study of transdiagnostic psychological intervention for participants with self-identified comorbid schizophrenia spectrum disorders and problematic anxiety. Despite a very small sample size (n=9) and no statistically significant conclusions being drawn, the authors suggested that the group had potential benefits for individuals experiencing psychosis. Another study that explored the utility of patient-led appointment scheduling also provided some information about the effectiveness of a transdiagnostic intervention for individuals in a community mental health team (Carey et al. Reference Carey, Tai and Stiles2013). Participants were patients referred to a psychology clinic irrespective of diagnosis, who received ‘Method of Levels’ therapy; a transdiagnostic cognitive therapy. The results showed an effect size of 1.45 that the authors concluded was similar to effect sizes in studies of disorder-specific interventions. Furthermore, this effect was produced with a low mean number of sessions (3.6), suggesting that the intervention was also more efficient than some other types of therapy that the study cited. However, the main focus of the study was patient-led appointment scheduling where patients selected the frequency and duration of their intervention. It is therefore difficult to attribute these results solely to the content of the intervention.
The findings and conclusions of these studies and reviews suggest that transdiagnostic interventions are effective and have the potential to be more efficient than some disorder-specific interventions. This study aims to follow on from this research by evaluating the effectiveness of a transdiagnostic CBT group intervention, plus three individual sessions, held within a secondary-care mental health setting. The intervention was open to anyone under the care of this service irrespective of diagnosis and, as such, this study used a real-world sample of individuals and problems typically seen by clinicians in community mental health services.
Method
Participants
Participants were adults under the care of a secondary-care mental health team and were, therefore, experiencing significant mental health difficulties requiring multi-disciplinary professional support. Participants were referred to the group by a clinician in the team and were then assessed by a group facilitator. Inclusion criteria were that the group facilitator judged that the individual was motivated to engage and would be able to commit to regular attendance. There were no exclusion criteria relating to diagnosis and the group accepted participants with a range of difficulties typical of this population including anxiety, depression, bipolar disorder, substance use difficulties, psychosis and personality disorders.
A total of 56 participants in five cohorts started the group between 2010 and 2013 and group facilitators routinely collected outcome data. Unfortunately no data are available regarding referral and acceptance rates for this period. Participants’ characteristics are displayed in Table 1. Data were missing for five participants who were therefore excluded from analysis, leaving a total sample of 51 participants, 31 of whom were female. No data on age or ethnicity were collected. Participants were categorized into diagnosis type based on their primary diagnosis which was obtained from a detailed clinical assessment prior to the group, but this was not based upon a clearly identified or validated diagnostic tool. Some participants had more than one diagnosis listed in the group records. In such cases the first diagnosis listed was considered to be the primary diagnosis. Diagnoses were divided into two groups; common mental health problems (anxiety disorders and depression) or severe mental illness (psychotic disorders, bipolar disorder and personality disorders) and represented 70.6% and 29.4% of the sample, respectively. Comorbidities were recorded in 19.6% of participants.
Table 1. Participants’ characteristics
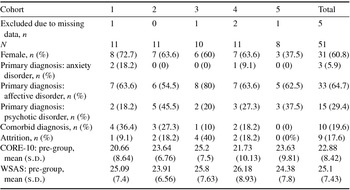
CORE-10, Clinical Outcomes in Routine Evaluation-10; WSAS, Work and Social Adjustment Scale.
Measures
Outcome measures were administered at pre-group individual sessions and during the final group sessions.
Clinical Outcomes in Routine Evaluation-10 (CORE-10; Connell & Barkham, Reference Connell and Barkham2007)
The CORE-10 is a short self-report measure of general subjective clinical outcome and distress. Connell & Barkham (Reference Connell and Barkham2007) reported that the CORE-10 has good discriminate validity between clinical and non-clinical samples (t=37.3, p<0.001), to show good internal consistency (Cronbach's α=0.81 and 0.82 for women and men, respectively) and to be sensitive to change post-therapy (t=38.1, p<0.001). The CORE-10 also demonstrated good convergent validity with the original 34-item CORE-OM in a clinical sample (r=0.94, 95% confidence interval 0.93-0.95) and to be acceptable for use with patients in primary care (Barkham et al. Reference Barkham, Bewick, Mullin, Gilbody, Connell, Cahill, Mellor-Clark, Richards, Unsworth and Evans2013).
Work and Social Adjustment Scale (WSAS; Mundt et al. Reference Mundt, Marks, Shear and Greist2002)
The WSAS is a five-item self-report measure of general functional impairment. In a study of participants with either obsessive compulsive disorder (OCD) or depression the WSAS was demonstrated to be reliable, with a test–retest correlation coefficient of 0.73 in a sample with OCD, internally consistent (Cronbach's α=0.942 and 0.882 at week 30 in participants with depression and OCD, respectively) and to have convergent validity with other validated outcome measures (Mundt et al. Reference Mundt, Marks, Shear and Greist2002).
Procedure
A CBT therapist and a clinical psychologist designed the group structure and content. The intervention was not based on a specific transdiagnostic model, but rather was an amalgamation of aspects of CBT that are transdiagnostic in nature. The content was identified based upon the current evidence-based interventions for specific disorders, namely CBT protocols for anxiety and depression, as well as the clinical experience of those involved in developing the group (see Table 2). Sessions included psychoeducation, behavioural activation, identifying negative automatic thoughts and considering productive and unproductive worry. Treatment consisted of 12 weekly 1½-h sessions, with a booster session delivered 4 weeks after session 12. In addition, each participant was also offered three 1-h individual sessions. The group and individual sessions were facilitated by clinical psychologists, nurses, social workers and occupational therapists who received group supervision from a clinical psychologist on a monthly basis.
Table 2. CBT group plan

The first individual session was held before the start of the group and provided participants with information about the group and individual requirements such as homework. Pre-group outcome measures were completed at this point. Two further individual sessions were held between sessions 3 and 4, and 6 and 9, and offered support in developing and applying the skills introduced in the group, as well as problem-solving any difficulties that arose. The content of these two sessions was guided by what the individual participant wanted to discuss.
Results
Attrition
Nine (17.6%) participants did not complete the group programme. Rates of attrition did not differ for gender (Fisher's exact test yields p=0.223 indicating no difference) or diagnosis type [χ²(1, n=51)=0.272, p=0.602].
Further analysis of pre-group outcome measure scores indicated no significant differences between those who completed the group (CORE-10: mean=22.45, s.d.=8.45; WSAS: mean=24.60, s.d.=7.51) and those who did not (CORE-10: mean=24.89, s.d.=8.43; WSAS: mean=27.44, s.d.=6.98; CORE-10: t 49=0.79, p=0.436; WSAS: t 49=1.05, p=0.301). This was also reflected in the descriptive statistics of clinical cut-offs for these measures (clinical cut-off for the CORE-10 and WSAS was a score of ≥10). One hundred per cent of participants who did not complete the group met the clinical cut-off for both the CORE-10 and WSAS while in completers these figures were 92.5% and 100%, respectively.
Baseline characteristics of completers
One-way between-subjects ANOVAs were conducted to explore the baseline CORE-10 and WSAS scores of participants who completed the group (n=42). Using the significance level p<0.05 there was not a significant difference between groups on baseline CORE-10 scores (F 2,39=1.36, p=0.270) or WSAS scores (F 2,39=0.21, p=0.814).
Primary analysis: CORE-10 and WSAS outcomes
The pre- and post-group scores for outcome measures are shown in Figure 1. A paired-samples t test was conducted on CORE-10 scores of completers (n=42) at pre-group (mean=22.45, s.d.=8.45) and post-group (mean=14.92, s.d.=7.68) and found a significant decrease at the end of the group (mean=7.52, s.d.=9.96; t 41=4.9, p<0.001). This represents a large effect size (Cohen's d=0.93), indicating that, over the course of the intervention, distress experienced by participants significantly reduced.
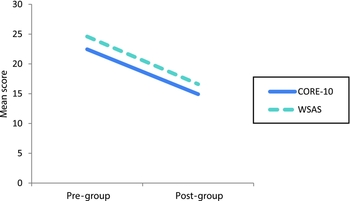
Fig. 1. Mean pre- and post-group outcome measure scores. CORE-10, Clinical Outcomes in Routine Evaluation-10; WSAS, Work and Social Adjustment Scale.
A significant decrease (mean=8.0, s.d.=6.92) was also found between WSAS scores at pre-group (mean=24.6, s.d.=7.51) and post-group (mean=16.6, s.d.=7.4; t 41=7.49, p<0.001), with a large effect size (Cohen's d=1.07). This indicates that the general functioning of participants was significantly improved at the end of the intervention.
An intention-to-treat analysis was also conducted with pre-group scores carried forward for participants who did not complete the group. A paired-samples t test found the significant decrease in CORE-10 scores remained with the inclusion of these participants (pre-group: mean=22.88, s.d.=8.42: post-group: mean=16.69, s.d.=8.6; difference: mean=6.20, s.d.=9.47; t 50=4.68, p<0.001, d=0.73), as well as for WSAS scores (pre-group: mean=25.10, s.d.=7.43; post-group: mean=18.51, s.d.=8.37; difference: mean=6.59, s.d.=6.99; t 50=6.74, p<0.001, d=0.83).
Secondary analysis: effect of intervention on different diagnostic groups
As per the analysis protocol, statistical analysis showed a significant improvement in scores on the CORE-10 and WSAS at post-treatment compared to baseline scores. Further ANOVAs were conducted to explore effects of the intervention across the two diagnostic groups whilst controlling for baseline scores (see Table 3). An ANCOVA was conducted with diagnostic group as the between-group factor and post-group CORE-10 and WSAS scores as dependent variables. Pre-group scores were included as covariates. This analysis showed no significant difference between the groups on post-group CORE-10 scores (F 1=0.001, p=0.98) or WSAS scores (F 1=0.09, p=0.77), indicating that participants benefited from the intervention irrespective of their diagnostic group.
Table 3. Mean pre- and post-group outcome scores
CORE-10, Clinical Outcomes in Routine Evaluation-10; WSAS, Work and Social Adjustment Scale.
Internal validity
Correlations were conducted to explore the relationship between CORE-10 and WSAS scores at pre-treatment and at post-treatment. The pre-treatment scores were moderately correlated (r=0.742, p<0.01) but at post-treatment the association was weaker (r=0.469, p<0.01). These results suggest that symptoms and general functioning were somewhat related before the intervention, but at post-treatment the two measures were assessing different outcomes.
Discussion
Evidence is increasingly being gained for the use of transdiagnostic group CBT interventions for mental health problems, with positive outcomes demonstrated in a range of diagnoses with a particular focus on anxiety disorders. This study evaluated a transdiagnostic intervention within a secondary-care mental health service that accepted participants irrespective of their diagnosis. The data from five cohorts show that the intervention was associated with significant improvements in subjective distress and functioning, irrespective of broad diagnosis type. Although the effect sizes of the mean decrease in symptom severity and functional impairment are smaller than the pre- to post-treatment effect size of d=1.58 reported in a previous meta-analysis by Norton & Philipp (Reference Norton and Philipp2008), they still indicate large effects.
The study was conducted in routine clinical practice and as such provides an ecologically valid account of the effect of this intervention. The study also demonstrates internal validity, as measured by correlations of the CORE-10 and WSAS at pre- and post-intervention. The moderate positive correlation at pre-treatment is to be expected when considering the symptoms and general functioning of participants under secondary-care mental health services, whereas the weak positive correlation at post-treatment suggests that the intervention was associated with positive outcomes on two different measures that assessed separate indices of improvement.
However, there are a number of limitations that should be considered. First, the lack of information about the referral and acceptance rates of the group is a significant weakness of the study, although it nevertheless represents the clinical reality. Furthermore, the data available regarding diagnosis of participants was unfortunately very limited and it was not possible to collect data retrospectively. Consequently, although the results show no difference in outcomes between the broad diagnostic groups employed, the validity of these groups is unknown. Ideally all participants would have undergone a diagnostic screening process to determine their primary and comorbid diagnoses. Instead diagnosis was determined by a clinician who used information gained at the pre-group interview, through review of patient records or from referral information. This variance in diagnostic procedure undermines the validity of the diagnostic groups and the conclusions about the effect of the intervention across diagnoses. This limitation is further highlighted by the unusually low rates of anxiety disorders and comorbidities reported here, as well as the unequal numbers of participants in the two diagnostic groups. It is therefore not possible to conclude whether the intervention is particularly beneficial to any specific diagnosis. Additionally, limited demographic information for the participants was collected, preventing statistical analysis of potential confounding effects of variables such as age, employment status, adjunctive medication, and previous or current additional psychological therapy.
Second, the effects of the group intervention must be interpreted with caution due to the lack of a control condition. The findings suggest that the group contributed to an improvement in symptom severity and general functioning, but without a control condition it is not possible to determine the processes involved. For example, the group in itself may have served to normalize the experience of participants, leading to an improvement in distress and functioning. Wolfensberger & Tullman (Reference Wolfensberger and Tullman1982) discussed the ways in which normalizing can minimize the effect of feeling different to others in society. For the participants, being in a group setting with a number of other individuals experiencing similar difficulties might well have served this function and reduced psychological distress associated with feeling different and ‘abnormal’. The effect of this and other potential confounding variables are unknown due to the lack of control condition.
Although the pre- and post-group outcome measures provide information on the effect of the group as a whole, no session-by-session outcome data was collected. This prevented an analysis of the change associated with individual sessions and the identification of specific transdiagnostic processes that the group targeted. It is therefore not possible to determine the components of the group that affected the positive changes observed. We can, however, hypothesize about the factors that may have been involved. For example, the group may have acted on the presenting problem of participants while also affecting comorbid difficulties and symptoms below the clinical threshold that may have served to exacerbate the presenting problem. Rather than addressing one particular problem through a psychological intervention, a broader approach as employed in the group might allow skills to be generalised and applied to lower level difficulties. For example, the thought challenging skills developed by an individual with depression may also be applied to anxious cognitions and result in a decrease in comorbid anxiety.
Despite the limitations of the study and the lack of clarity regarding the important processes involved, the results arguably offer good ecological validity. The real-world sample of participants with the diagnoses, comorbidities and complexities typical of a secondary-care mental health service suggests that transdiagnostic CBT groups are a promising treatment option. In addition, these groups were run by clinicians from a range of disciplines within the service and the group facilitators followed a protocol devised by the clinicians based on their experience of a substantial range of diagnoses. Feedback from the facilitators suggests that the group represents a good first-line treatment that is cost-effective due to it being delivered by a small number of staff. The potential for more cost-effective and efficacious services in which patients can more rapidly access evidence-based treatment is an exciting prospect for the NHS and patients alike and further research into transdiagnostic CBT group interventions in secondary-care services is clearly justified.
Summary of main points
This study evaluated the effectiveness of a 13-session transdiagnostic CBT-based group intervention, with three individual sessions. Unlike much of the literature on transdiagnostic groups that has focused on anxiety disorders, the current study included participants with a range of diagnoses typical of a secondary-care mental health service and the results therefore have good ecological validity.
The group was associated with reductions in subjective distress, as measured by the CORE-10, and increases in general functioning, as measured by the WSAS. Significant differences were found between pre- and post-group outcomes and these remained in an intention-to-treat analysis.
These positive initial findings highlight the need for more rigorous research into the clinical utility of transdiagnostic groups for individuals with any mental health diagnosis in order to explore the potential cost and time benefits, both to patients and to the NHS.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Acknowledgments
The authors thank Jennie Boland, Joel Conrad and Steve Marrett for developing and facilitating the group, and their support with this project.
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Declaration of Interest
None.
Learning objectives
-
(1) To outline the available literature on transdiagnostic group interventions.
-
(2) To outline features of a transdiagnostic CBT-based intervention.
-
(3) To highlight the flexible application of transdiagnostic group intervention across diagnoses.
-
(4) To illustrate the potential of a transdiagnostic CBT-based intervention approach to produce positive results for less cost and with reduced waiting times.







Comments
No Comments have been published for this article.