Introduction
Difficulties with psychosocial functioning, enduring emotional and cognitive disturbances and pervasive distress is often diagnosed as ‘personality disorder’, a contentious diagnostic term due to the stigmatised perception of the whole person (Department of Health, 2003; Lamb and Sibbald, Reference Lamb and Sibbald2018). The term is used here to aid clarity as it is without doubt that people meeting diagnostic criteria typically experience these idiosyncratic features. The most common personality disorder subtype in non-forensic healthcare settings is borderline personality disorder (BPD), characterised by emotional instability, feelings of abandonment, intense interpersonal relationships, suicidal behaviour, impulsivity and a negative self-image (National Institute for Health and Clinical Excellence, 2009). BPD is further related to a myriad of negative associations, such as increased use of healthcare services, higher risk of self-harm/suicide ideation, co-morbidity, substance and alcohol misuse, physical health problems, poor treatment outcomes, and shorter life expectancy, all of which contribute to the aforementioned stigma (Fok et al., Reference Fok, Hayes, Chang, Stewart, Callard and Moran2012; Goddard et al., Reference Goddard, Wingrove and Moran2015; Moran et al., Reference Moran, Romaniuk, Coffey, Chanen, Degenhardt, Borschmann and Patton2016a,b; Newton-Howes et al., Reference Newton-Howes, Tyrer and Johnson2006; Oldham, Reference Oldham2006; Quirk et al., Reference Quirk, Berk, Chanen, Koivumaa-Honkanen, Brennan-Olsen, Pasco and Williams2016; Soeteman et al., Reference Soeteman, Roijen, Verheul and Busschbach2008; Sansone et al., Reference Sansone, Farukhi and Wiederman2011; Tyrer et al., Reference Tyrer, Reed and Crawford2015).
How BPD develops continues to be debated within nosology, but it has become widely accepted that factors such as genetics, neurobiology, psychosocial factors, attachment and trauma contribute to the aetiology (National Institute for Health and Clinical Excellence, 2009; Stepp et al., Reference Stepp, Lazarus and Byrd2016). Symptoms usually present in childhood and adolescence with compounding evidence supporting long-term positive outcomes for patients who receive early diagnosis and intervention (Biskin, Reference Biskin2015). Despite this, GPs and clinicians are reluctant to diagnose the condition in ‘emerging adulthood’, based on suspected transient features and potential stigmatisation, which in reality lacks sufficient rationale to delay an evidence-based intervention (Biskin, Reference Biskin2015; Bozzatello et al., Reference Bozzatello, Bellino, Bosia and Rocca2019; Chanen, Reference Chanen2015; Laurenssen et al., Reference Laurenssen, Hutsebaut, Feenstra, van Busschbach and Luyten2013). As for adults, evidence suggests the clinical presentation of BPD is different to that of those in ‘emerging adulthood’ and therefore could be overlooked (Morgan et al., Reference Morgan, Chelminski, Young, Dalrymple and Zimmerman2013a). Overall, the trajectory for BPD is positive as longitudinal studies have found a decrease in symptomology over time and high remission rates (73–85%) after 6–10 years from diagnosis (Álvarez-Tomás et al., Reference Álvarez-Tomás, Ruiz, Guilera and Bados2019; Zanarini et al., Reference Zanarini, Frankenburg, Hennen and Silk2003a).
Subthreshold BPD
However, remission from BPD does not guarantee complete recovery from symptoms or traits. This pattern of symptom alleviation across the lifespan is common but rates of recovery are poor (Zanarini et al., Reference Zanarini, Frankenburg, Reich and Fitzmaurice2012). One study by Zanarini et al. (Reference Zanarini, Frankenburg, Hennen and Silk2003a) saw a significant reduction in 73.5% of participants’ symptoms and no longer met diagnostic criteria cut-off after 6 years, but the majority still experienced the typical BPD symptoms. This lack of diagnostic label is all but arbitrary and polythetic, which could deny individuals adequate treatment. Recent developments in the classification of BPD will see severity of personality diagnosed first, ranging from no personality disorder to severe personality disorder, with subtype domains a secondary diagnosis (Tyrer et al., Reference Tyrer, Crawford and Mulder2011; World Health Organisation, 2018). This dimensional approach to conceptualising personality disorder accounts for individuals who do not warrant a full diagnosis or meet clinical cut-off and present with subthreshold symptoms (Yang et al., Reference Yang, Coid and Tyrer2010; Zimmerman et al., Reference Zimmerman, Chelminski, Young, Dalrymple and Martinez2013).
Overall, subthreshold BPD remains an under-explored area in mental health research (Morgan et al., Reference Morgan, Chelminski, Young, Dalrymple and Zimmerman2013b). This presentation is not limited to those vulnerable to developing BPD but is also relevant for non-clinical populations experiencing symptoms (Johnson and Levy, Reference Johnson and Levy2020). Initial findings suggest that individuals with as little as one BPD trait still experience a degree of disability and distress that rivals the impairment of full-syndrome BPD (Bos et al., Reference Bos, Bas van Wel, Appelo and Verbraak2011; Kaess et al., Reference Kaess, Fischer-Waldschmidt, Resch and Koenig2017; Lu et al., Reference Lu, Wang, Ko, Hsiao, Liu and Yen2017; Zimmerman et al., Reference Zimmerman, Chelminski, Young, Dalrymple and Martinez2013). Furthermore, individuals experiencing subthreshold BPD traits possess higher rates of co-morbidity, in particular depression and anxiety, posing poorly for treatment outcomes and full-syndromes alike (French et al., Reference French, Turner, Dawson and Moran2017; Gorwood et al., Reference Gorwood, Rouillon, Even, Falissard, Corruble and Moran2010; Hepgul et al., Reference Hepgul, King, Amarasinghe, Breen, Grant, Grey and Cleare2016; Hill et al., Reference Hill, Geoghegan and Shawe-Taylor2016; Karukivi et al., Reference Karukivi, Vahlberg, Horjamo, Nevalainen and Korkeila2017; Newton-Howes et al., Reference Newton-Howes, Tyrer and Johnson2006).
Access to treatment and primary care
As subthreshold BPD does not meet clinical cut-off, individuals with these symptoms do not receive an adequate, evidence-based treatment. This creates the need for an intervention which supports people experiencing subthreshold BPD symptoms and improved accessibility of treatment for individuals unable to access specialist secondary care (Chanen and McCutcheon, Reference Chanen and McCutcheon2013; Chanen and Thompson, Reference Chanen and Thompson2018; Thompson et al., Reference Thompson, Jackson, Cavelti, Betts, McCutcheon, Jovev and Chanen2018). This is not to be confused with early intervention, which would be a treatment seeking to prevent the exacerbation or development of symptoms leading to full-syndrome BPD (best targeted in emerging adulthood). A treatment for subthreshold BPD would aim to bridge the gap between specialist, evidence-based treatment and those who may experience persistent BPD symptoms throughout their lifetime but may never develop the full disorder. Without addressing these needs, individuals may not benefit from standard interventions, resulting in a higher cost for services and latent co-morbidity.
This presentation has been explicitly observed within primary care Improving Access to Psychological Therapies (IAPT) services, a UK government initiative to address common mental health concerns in the UK population (French et al., Reference French, Moran, Wiles, Kessler and Turner2019; Goddard et al., Reference Goddard, Wingrove and Moran2015; Hepgul et al., Reference Hepgul, King, Amarasinghe, Breen, Grant, Grey and Cleare2016). With an initial focus on treatment anxiety and depression, 2016 saw a new emphasis on treating people meeting criteria for personality disorder in primary care services following the publication of the Five Year Forward View for Mental Health (NHS England, Reference England2016). However, the presentation of patients within primary care is a complicated issue. Individuals meeting diagnostic criteria for personality disorder had already been utilising IAPT services, which have adversely affected and been identified as a prognosis risk factor to treatment outcomes (French et al., Reference French, Turner, Dawson and Moran2017; Goddard et al., Reference Goddard, Wingrove and Moran2015; Hepgul et al., Reference Hepgul, King, Amarasinghe, Breen, Grant, Grey and Cleare2016). The presence of subthreshold BPD difficulties has led to possible misclassification between conditions and an increased risk of developing depression and anxiety in later life (Moran et al., Reference Moran, Romaniuk, Coffey, Chanen, Degenhardt, Borschmann and Patton2016a,b). By treating anxiety and depression, whilst ignoring subthreshold BPD symptoms, interventions in IAPT are less effective with the need to address these concerns. Two primary care services in the South East of England have attempted to address this by offering a cognitive behavioural therapy group intervention devised for people experiencing subthreshold BPD traits: Systems Training for Emotional Predictability and Problem Solving – Early Intervention (STEPPS-EI; Blum et al., Reference Blum, Bartels, St. John, Pfohl and Harvey2016).
STEPPS-EI was adapted from STEPPS for BPD (Blum et al., Reference Blum, Pfohl, St John, Monahan and Black2002b; Blum et al., Reference Blum, Bartels, St. John, Pfohl and Harvey2016), following pilot studies run within primary care services in Sussex and Essex (Harvey, Reference Harvey, Black and Blum2016). The full-programme STEPPS is a manualised, psychoeducational treatment, which aims to train individuals to become more aware of their emotions, and to provide them with skills on how to challenge and effectively manage their emotional intensity difficulties (EID). Individuals are then further reinforced by the facilitators and other group members to develop a system of support with significant others (Blum et al., Reference Blum, Bartels, St. John and Pfohl2002a). STEPPS is currently supported by three randomised controlled trials which have found that it can reduce the severity of BPD symptoms and symptoms of depression, and improve global functioning and quality of life (Blum et al., Reference Blum, St. John, Pfohl, Stuart, McCormick, Allen and Black2008; Bos et al., Reference Bos, Bas van Wel, Appelo and Verbraak2011; van Wel et al., Reference van Wel, Bos, Appelo, Berendsen, Willgeroth and Verbraak2009). In addition, the evidence base for STEPPS is further supported by numerous uncontrolled studies, and it is recognised by the National Institute for Health and Clinical Excellence (NICE) as an effective treatment method that improves general functioning and reduces self-harm and suicide ideation (Black et al., Reference Black, Blum and St John2009; Harvey, Reference Harvey, Black and Blum2016; Hill et al., Reference Hill, Geoghegan and Shawe-Taylor2016; National Institute for Health and Clinical Excellence, 2009).
STEPPS-EI was established to address the absence of early intervention for subthreshold BPD (Blum et al., Reference Blum, Bartels, St. John, Pfohl and Harvey2016). As it is directed at individuals without a formal diagnosis, the term subthreshold BPD will be used to describe participants. The adapted version is a 13-week programme, as opposed to 20 weeks, and consists of three modules: (1) Awareness of EID, (2) Emotion Management and (3) Behaviour Management Training (see Supplementary material for full module and session breakdown). Each session is 2 hours long and is delivered within the community after an initial primary care referral to STEPPS-EI. The intervention is then delivered using the STEPPS-EI manual, with additional homework and materials.
The present study
STEPPS-EI is yet to be clinically evaluated, and it is important to assess whether the NHS is providing an effective yet feasible treatment service for a population in which research is limited. The emerging literature has so far outlined the difficulty with identifying subthreshold BPD and the dysfunction and distress encountered by BPD symptoms, such as EID (Harvey, Reference Harvey, Black and Blum2016; Kaess et al., Reference Kaess, Fischer-Waldschmidt, Resch and Koenig2017; Tyrer, Reference Tyrer2017; Zimmerman et al., Reference Zimmerman, Chelminski, Young, Dalrymple and Martinez2013). Although initial evidence suggests that individuals meeting criteria for full-syndrome personality disorder can make significant progress over the course of short-term treatment, more research is needed in relation to subthreshold BPD (Laporte et al., Reference Laporte, Paris, Bergevin, Fraser and Cardin2018). It has therefore become a clinical priority to investigate the indicated prevention of BPD by treating individuals presenting with subthreshold symptoms (Chanen et al., Reference Chanen, Sharp and Hoffman2017). However, this is further complicated by the complex presentation of subthreshold BPD. The co-morbidity of personality difficulties with depression and anxiety has affected treatment outcomes and created a need to address associated difficulties individually (French et al., Reference French, Turner, Dawson and Moran2017; Goddard et al., Reference Goddard, Wingrove and Moran2015; Hepgul et al., Reference Hepgul, King, Amarasinghe, Breen, Grant, Grey and Cleare2016). By evaluating STEPPS-EI within primary care, the impact of intervention on subthreshold BPD symptoms can be further assessed and begin to formulate a profile of individuals with subthreshold BPD.
The present article seeks to expand on the initial pilot evaluation of STEPPS-EI. As preliminary effectiveness has been established, this evaluation sought to draw on further aspects of an uncontrolled feasibility study (Medical Research Council, 2000; Medical Research Council, 2019), with the intention to explore whether STEPPS-EI is feasible to be delivered in NHS primary care mental health settings. The primary aims were to assess:
(1) Recruitment. Is it possible to recruit participants into STEPPS-EI groups? This was operationalised as recruiting at least 30 participants within each service each year and running at least three groups.
(2) Retention. Is it possible to retain participants in STEPPS-EI groups? This was operationalised as having at least 70% of participants offered a group attending 10 or more sessions and completing treatment.
(3) Potential effectiveness. Is there preliminary evidence that STEPPS-EI groups are effective at improving symptoms of emotional intensity, depression and anxiety? This is operationalised as pre–post effect sizes on measures of emotional intensity, depression and anxiety being in the direction of benefit, and that the 95% confidence interval for the pre–post effect size includes a medium-sized effect.
(4) Group appraisal. How did participants experience the STEPPS-EI groups? This is determined through open-ended feedback from intervention completers.
Method
Participants
All individuals were referred to one of two NHS primary care mental health services in the South of England and screened for STEPPS-EI at assessment. Inclusion criteria were: scoring 7 or more (out of a possible 10) on the STEPPS-EI screening tool (see Supplementary material) adapted from the McLean Instrument for BPD (Zanarini et al., Reference Zanarini, Vujanovic, Parachini, Boulanger, Frankenburg and Hennen2003b), aged 18 and over, tolerance of group settings, motivation to complete work outside of sessions, and reading/writing skills necessary to complete intervention exercises.
Exclusion criteria were: having a formal diagnosis of personality disorder (n = 10), as identified by a psychiatrist or GP; completing an alternative STEPPS intervention; antisocial, avoidant or narcissistic traits; ongoing co-morbidity which would prevent engagement, such as persistent physical health problems; history of long-term severe mental health problems, e.g. schizophrenia; use of illicit substances which create instability; or a history of multiple psychological treatments. See Fig. 1 for flow of participants within the evaluation.
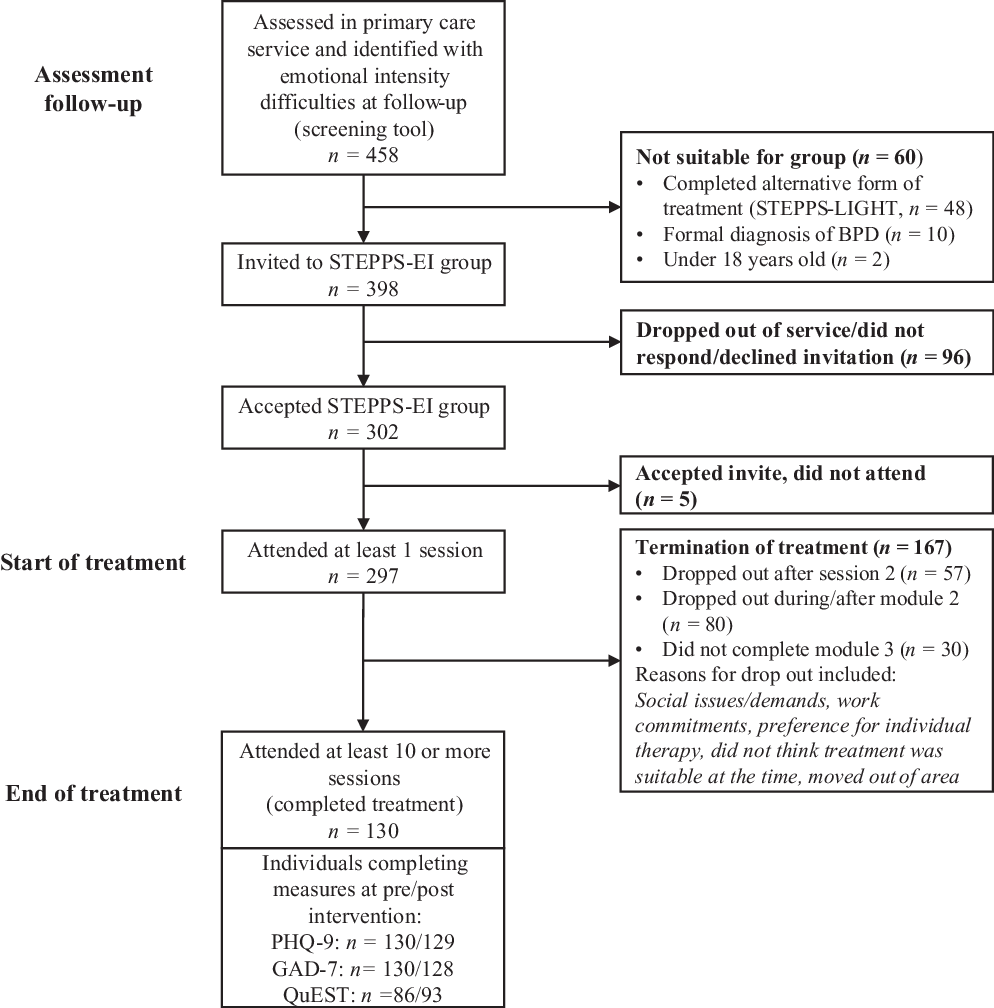
Figure 1. The flow of participants through primary care attending STEPPS-EI groups.
A priori analysis was run using G*Power 3.1 to determine the sufficient number of participants needed to test the study hypotheses with a pre–post effect size of d = .95, 95% power, two-tailed hypotheses and p < .05 (Faul et al., Reference Faul, Erdfelder, Lang and Buchner2007). The estimated effect size was based on Harvey et al. (Reference Harvey, Black and Blum2010) due to the shared similarities with regard to a UK clinical population, uncontrolled STEPPS study, study design and location. The total sample size required was 80 participants, which was sufficiently achieved.
The sample was recruited from two NHS patient database systems, PC-MIS and SystmOne (University of York, 2006; tpp, 2018). Four hundred and fifty-eight individuals were screened by primary care mental health workers and invited to participate in STEPPS-EI. If invited individuals declined the group, they would be offered an alternative intervention within the stepped care model with consideration of subthreshold BPD symptoms. Of the sample, 12 participants were excluded after not meeting inclusion criteria. In addition, 48 individuals completed an alternative form of STEPPS-EI (STEPPS-Light; an earlier version of STEPPS shortened to 16 sessions) during 2013–2014 and were further excluded from the final sample. Of the remaining 398 participants, 321 were female (81%) with an age range of 18 to 62 years (mean = 31.05, SD = 9.39). Full sample demographics are presented in Table 1, with individual differences between groups based on the number of completed sessions. Incidentally, some patient data were incomplete, resulting in missing data for some individuals at pre- and post-periods (see Table 2).
Table 1. STEPPS-EI demographics with individual grouping based on number of sessions completed
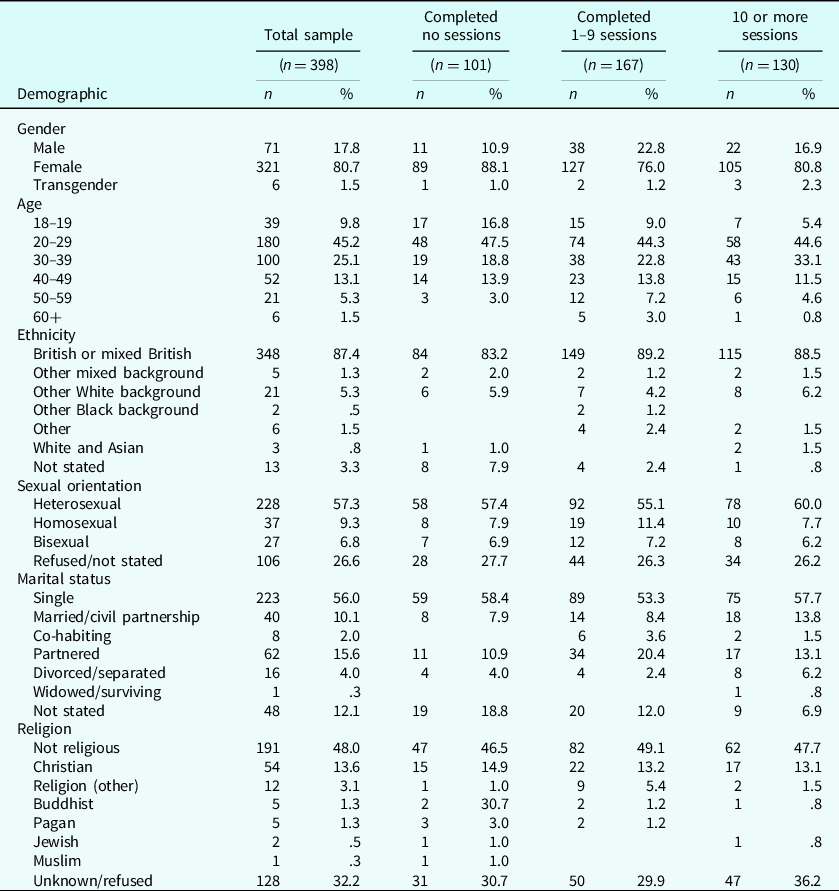
Table 2. Missing data for each outcome measure

Procedure
This evaluation draws on aspects of an uncontrolled feasibility study of STEPPS-EI. STEPPS-EI is a psychoeducational, group intervention for individuals with subthreshold BPD. Based on cognitive behavioural principles, the programme aims to teach individuals skills to identify and manage emotional intensity with the additional help of a social support network. The programme consists of 13 weekly sessions, divided into three modules, with the introductory module being 1 week and the following two modules 6 weeks accordingly. Module 1 introduces EID as a problem with emotion regulation rather than an illness or diagnosis. Following on, module 2 teaches individuals emotion management skills (such as distancing and challenging) to help identify and address factors that perpetuate their EID. These difficulties are identified as cognitive factors, expressed by negative coping strategies and maladaptive schema (‘filters’). Module 3 elaborates on module 2 by developing behavioural management skills (such as distraction and self-soothing techniques) to improve competent coping strategies in their day-to-day environment. Both emotional and behavioural management skills are consolidated in weekly homework assignments, as group members are actively encouraged to practise STEPPS-EI during their daily routine.
The intervention is set up to imitate a ‘classroom experience’, with group members and two facilitators. STEPPS-EI facilitators possess significant experience with cognitive behavioural principles before being trained across a 2-day workshop and participating in a STEPPS group as an observer. Facilitators were from a range of professional backgrounds (psychologists, primary care mental health workers, psychological wellbeing practitioners and nurses). Facilitators were also provided with regular clinical supervision to discuss group delivery, dynamics and any reflections they may have.
Twenty-five STEPPS-EI groups were implemented during the designated collection period (February 2015 to July 2018). Service-users were screened for suitability at assessment follow-up (see Supplementary material) and invited to treatment. If a service-user declined treatment, they would be offered treatment as usual depending on presentation, or signposted elsewhere. Invited participants would consent to start treatment and complete baseline measures at the first session as part of routine service evaluation. At each following session, primary care staff collected and recorded outcome measures on specified patient databases (PC-MIS and SystmOne). Data were then extracted from these platforms and hard copy questionnaires, with post-intervention classed as the last attended session. Participants who completed 10 or more of the 13 sessions were regarded as completing treatment and included in the analysis. The researchers were not involved in facilitation or consultation of any STEPPS-EI groups and have independently examined the data.
Measures
Within the current study, feasibility measures are outlined below with preliminary effectiveness assessed using a repeated-measures design at pre- and post-intervention variables (symptoms of BPD, depression and anxiety).
Recruitment
This is the number of individuals who were invited to treatment and participated. Recruitment is reported as percentage rates of the total population who attended at least one group session and average enrolment per year, per site. Recruitment was deemed feasible if each service recruited at least 30 participants and ran at least three groups in total since September 2014.
Retention
This is the rate at which participants completed treatment. Retention was deemed feasible if 70% of participants offered the group would attend 10 or more sessions. Participants were considered to have ‘completed’ treatment if they had attended 10 or more sessions. This threshold was taken from the full-programme of STEPPS which allows for three missed sessions (Blum et al., Reference Blum, Pfohl, St John, Monahan and Black2002b).
Group appraisal
Feedback on participant experiences of the group was collected using evaluation forms that were distributed to the participants in the final STEPPS-EI session. A total of 56 participants responded to these questionnaires (43% of those attending 10 sessions or more). Evaluation questions consisted of open and closed questions with the addition of rating scales (see Supplementary material).
Effectiveness
The outcome measures of interest were the QuEST (symptoms of BPD), PHQ-9 (symptoms of depression) and GAD-7 (symptoms of anxiety).
Quick Evaluation of Severity Over Time (QuEST) – Pfohl et al., Reference Pfohl, Blum and Zimmerman1997; Pfohl et al., Reference Pfohl, Blum, St John, McCormick, Allen and Black2009; Blum et al., Reference Blum, Bartels, St. John, Pfohl and Harvey2016
This is a 15-item psychometric test designed specifically for STEPPS-EI as a measure of emotional intensity severity over time. Participants track their progress weekly during the programme on a 5-point Likert scale with responses ranging from none/slight to extreme. The scale consists of three subsections: (A) Thoughts and Feelings, (B) Behaviour (negative) and (C) Behaviour (positive). An example question is: ‘Going to extremes to try and keep someone from leaving you’. The scale was originally adapted from the full STEPPS programme instrument, Borderline Evaluation of Severity over Time (BEST), and is found to possess good sensitivity to clinical change, moderate test–re-test reliability and a high internal consistency in the current study (α = .78).
Patient Health Questionnaire 9 (PHQ-9) – Kroenke et al. (Reference Kroenke, Spitzer and Williams2001)
This is a brief 9-item instrument used within the NHS to assess symptoms of depression. The questionnaire is based on the DSM-IV criteria for depression as individuals rate their experience on a 4-point Likert scale (not at all; several days; more than half the days; nearly every day). Scoring can range from 0 to 27, with cut-off points of 10, 15 and 20 signifying mild, moderate and severe depression, respectively, and possesses high internal consistency (α = .83). The scale is frequently used within IAPT services with scores ≥10 indicative of an episode of major depression, and an improvement or deterioration of ≥6 indicating reliable change (NHS Digital, Reference Digital2019). An example statement is: ‘Little interest or pleasure in doing things?’.
Generalised Anxiety Disorder Questionnaire (GAD7) – Spitzer et al. (Reference Spitzer, Kroenke, Williams and Löwe2006)
This is a brief 7-item instrument also used within the NHS, to measure symptoms of anxiety. Individuals rate their experience on a 4-point Likert scale (not at all; several days; more than half the days; nearly every day). Scoring can range from 0 to 21, with cut-off points for mild (5), moderate (10) and severe anxiety (15) accordingly, with high internal consistency (α = .84). This scale is frequently used with IAPT services with scores ≥8 indicative of clinically significant anxiety symptoms, and an improvement or deterioration of ≥4 indicative of reliable change (NHS Digital, Reference Digital2019). An example statement is: ‘Feeling nervous, anxious, or on edge’.
Data analysis
All data were analysed using Statistical Package for the Social Sciences (SPSS), version 24 (IBM Corporation, 2016). Differences in demographics were compared across participants based on the number of sessions completed (no sessions; 1–9 sessions; 10 or more sessions) using the Kruskall–Wallis H test as all demographic data were not normally distributed. Substance misuse was classed as any reported current drug use which is listed on the UK government ‘controlled drug list’ or exceeding the recommended weekly alcohol intake, excluding any drugs for medical purposes. Furthermore, post hoc Dunn tests were conducted, with adjusted Bonferroni correction to account for a potential higher risk of Type I error. To test the change between pre- and post-outcome measure data, individuals who completed treatment (10 or more sessions) were analysed using a per-protocol (PP) analysis. Both t-test and the Wilcoxon test were employed for significance testing with Pearson’s r correlation coefficients calculated for effect sizes (ES).
As mentioned previously, there was a lack of complete data for the full sample. For individuals who did not attend any sessions, screening data were carried forward to baseline for the PHQ-9 and GAD-7 only. Percentage recovery, reliable improvement and deterioration were also calculated using criteria for these used in IAPT as follows: (1) recovery is deemed to have occurred when PHQ-9 and GAD-7 scores are below clinical cut-offs at post-intervention when at least one of these scores was in the clinical range at baseline; (2) reliable improvement/deterioration is deemed to have occurred when PHQ-9 scores decrease/increase by 6 or more points and GAD-7 scores increase/decrease by 4 or more points, respectively (NHS Digital, Reference Digital2019).
Group appraisal was analysed following the six stages for thematic analysis by Braun and Clarke (Reference Braun and Clarke2006). To begin with, the data were transcribed verbatim from the paper questionnaires and assessed to identify codes. These codes encapsulated units relating to the evaluation of the STEPPS-EI course. The list of codes was analysed to derive themes and sub-themes, with a thematic map used to formulate how the themes and codes relate to each other. The analysis was conducted by one of the authors (F.A.) under supervision of three of the other authors (C.S., J.C. and H.S.).
Results
Feasibility of STEPPS-EI
Recruitment
Three hundred and ninety-eight participants out of 458 referrals were invited to take part in a STEPPS-EI group. Of those 398 participants invited, 75% attended at least one STEPPS-EI session (see Table 3). The average recruitment rate across both sites per year was 110 individuals (SD = 49.66). Site 1 conducted 14 STEPPS-EI groups between May 2015 and July 2018 (mean = 3.50, SD = 1.00) and Site 2 conducted 11 STEPPS-EI groups between September 2014 and July 2018 (mean = 3.67, SD = 2.08). Reasons recorded by group facilitators for not attending any sessions included time of session, location, work commitments, childcare commitments, fear/anxiety of working in a group, social issues/demands, bereavement and medical appointments.
Table 3. Overall recruitment for STEPPS-EI at Site 1 and Site 2; total number of groups, sign-ups and attrition per year

At time of analysis, 2018 had not been completed (July 2018), reflecting a lower number of groups and recruitment. *Only Site 1 registered a group for 2015 which met the inclusion criteria.
Retention
One hundred and thirty participants attended 10 or more sessions (43% of those who accepted the group invitation). The overall sample also completed a mean of 5.59 sessions (SD = 4.85), with 26 individuals completing the full program of 13 sessions (6.5%).
Group appraisal
Two over-arching themes emerged from the thematic analysis: Aspects and Evaluation of STEPPS-EI and Psychological Changes. As displayed in Table 4, these two themes are interdependent; as the participants experience aspects of STEPPS-EI, they undergo psychological changes which then influence their evaluation of the course. Aspects and Evaluation of STEPPS-EI consisted of four themes: Interpersonal Sensitivities, the Length of the Course, Paperwork and Reinforcement team cards, and Responses to Diagnostic Ambiguity. The second over-arching theme encompassed four themes: Emotional Changes, Interpersonal Changes, Behavioural Changes and Cognitive Changes. The theme Emotional Changes breaks down further into two subordinate themes: Changes in Everyday Emotions and Changes in EID.
Table 4. Over-arching themes, themes, subordinate themes and illustrative quotes from qualitative STEPPS-EI feedback forms

Effectiveness
A per protocol (PP) analysis was conducted to evaluate change between measures at baseline and post-intervention for individuals who attended at least 10 sessions. There were 130 participants with complete data at both baseline and post-intervention.
Table 5. Comparisons of pre- and demographic variables between samples, grouped by number of completed sessions with Dunn–Bonferroni correction post hoc and effect sizes

* p < .05.
Table 6. Paired samples t-test between outcome measures

* p < .001.
Table 7. Wilcoxon signed-rank test between outcome measures

* p < .001.
PP paired-samples t-test was conducted on pre- and post-data from the QuEST and PHQ for individuals attending at least 10 sessions (Table 6). QuEST scores, assessing BPD symptoms, decreased significantly from baseline (mean = 44.65, SD = 9.71) to post-intervention (mean = 33.39, SD = 11.43); t 83 = 8.96, p < .001, with a large effect size; r = .70.
PHQ scores significantly decreased from baseline (mean = 16.46, SD = 5.38) to post-intervention (mean = 13.78, SD = 6.25) scores; t 128 = 4.74, p < .001, with a medium–large effect size; r = .39. At baseline 89% (n = 116) of individuals scored at caseness for clinical significance on the PHQ; following the intervention, 32 of these individuals scored below the caseness threshold (23.2%). In addition, 37 of these individuals showed reliable improvement on the PHQ-9, with an improvement in score of at least 6 points (29%). Eleven individuals (8.46%) showed reliable deterioration in their PHQ-9 score of at least 6 points.
GAD data violated the assumption of normality which was reinforced by a significant Shapiro–Wilk test (p < .001). A Wilcoxon signed-rank test was employed to assess change in GAD scores (Table 7). GAD scores significantly decreased from baseline (Mdn = 15, SD = 4.67) to post-intervention (Mdn = 11, SD = 5.59); Z = –5.04, p < .001, with a medium effect size, r = –.31. At baseline 88% (n = 114) were at caseness for clinical significance on the GAD; following the intervention, 30 individuals scored below the threshold to non-caseness (23.1%). In addition, 52 individuals made reliable improvement (40%) and six individuals (4.62%) showed reliable deterioration. Overall, 16 (13%) individuals showed recovery on both PHQ-9 and GAD-7 measures. See Table 8 for full primary care recovery, improvement and deterioration calculations.
Table 8. Primary care measures of caseness, reliable improvement and deterioration, recovery and reliable recovery

*p < .001.
Demographic differences
Further analysis compared differences between the number of sessions attended (grouped by no sessions, attended 1–9 sessions, and 10 or more sessions) and participant demographics (see Table 5 for full analysis). Groups significantly differed between pre-intervention PHQ-9 scores, H (2) = 8.99, p < .02. Dunn post hoc tests revealed a significant difference between overall scores for participants who attended no sessions (Mdn = 20, IQR = 7) and those who attended 10 or more sessions (Mdn = 17, IQR = 8) with a small effect size, p < .02, r = .20. In addition, there were significant differences between sessions attended and psychotropic medication use, H (2) = 7.36, p < .03.
In addition, observations revealed significant differences between number of sessions attended and age, H (2) = 8.26, p < .02. Pairwise comparisons found significant differences between individuals who attended no sessions (Mdn = 26, IQR = 14) and both 1–9 sessions (Mdn=29, IQR=14), p = .024, r = –.16, or 10 or more sessions (Mdn = 29.50, IQR = 13), p < .05, r = –.13. There were no statistically significant differences between session attendance and gender, ethnicity, sexual orientation, marital status, religion, drug misuse, history of overdose, deliberate self-harm, previous therapy, and referrer; p > .05.
Discussion
The present evaluation sought to investigate the feasibility of STEPPS-EI as an intervention for individuals presenting with subthreshold BPD traits within primary care services. Results partially supported STEPPS-EI as a feasible treatment, meeting three out of four study aims of recruitment, effectiveness and group appraisal, but narrowly falling short due to issues with retention. This evaluation did not allow for follow-up data for those who dropped out, but we can speculate on this low retention rate based on the present findings.
One explanation for this could be that there are specific engagement issues with the overall STEPPS programme model and shortened STEPPS-EI course itself. STEPPS programmes have been found to possess higher rates of drop-outs in comparison with other group BPD treatments, although overall rates are inconclusive due to large confidence intervals and variation between studies (Barnicot et al., Reference Barnicot, Katsakou, Marougka and Priebe2011; Droscher et al., Reference Droscher, Startup, Petfield, Horsman and Cartwright-Hatton2014; Martino et al., Reference Martino, Menchetti, Pozzi and Berardi2012). In this evaluation, observed drop-out rates for STEPPS-EI (57%) were higher in comparison with other STEPPS studies (26–50%) and general primary care services (42–48%), regardless of specified disorder (Byng et al., Reference Byng, Newbold, Qureshi, Weyer-Brown, Bannon, Pooler and Anderson2011; Murphy et al., Reference Murphy, Mansell, Craven, Menary and McEvoy2013; Richards and Borglin, Reference Richards and Borglin2011). One key difference, besides the shortened number of sessions, is the lack of routine ‘reinforcement’ sessions. Reinforcement sessions are usually conducted weekly alongside the full programme as a means to consolidate knowledge and further practise STEPPS outside of the group environment. Marshall et al. (Reference Marshall, Quinn, Child, Shenton, Pooler, Forber and Byng2016) outlined ways in which primary care services can reduce drop-out, which included being more flexible as a service and developing stronger therapeutic relationships between clinicians and participants. By integrating reinforcement sessions more proactively into primary care treatment, we can elicit a stronger therapeutic alliance and model a secure base for those with subthreshold BPD. With such a high drop-out rate in primary care and STEPPS programmes alike, it is possible that in practice the feasibility threshold set in this evaluation is unobtainable.
Alternatively, this higher rate could be accounted for by some demographic risk factors that increase the likelihood of drop-out and which overlap with people diagnosed with symptoms of BPD, e.g. unstable relationships, alcohol use and suicide attempts (Buckman et al., Reference Buckman, Naismith, Saunders, Morrison, Linke, Leibowitz and Pilling2018; Wnuk et al., Reference Wnuk, McMain, Links, Habinski, Murray and Guimond2013). Our findings suggest that younger participants, those who use psychotropic medication and those with higher scores of depressive symptomatology are more likely to drop out of the programme completely. It is quite possible that these more complex participants would meet a formal diagnosis for BPD, but due to clinician ambivalence to diagnose, they do not receive appropriate care. On the other hand, by not possessing a full profile of BPD symptoms, some parts of the course may not feel relevant or these traits may not be as severe/problematic to warrant a full treatment programme. Positively, the overall retention rate has increased each year since 2016.
Despite this, the course itself is attractive enough to recruit a substantial number of participants and those who complete the course find it broadly acceptable. Participants were able to learn from each other, validate their symptoms and experience a shared group identity. This was further benefited from the lack of formal diagnosis by identifying problematic traits/symptoms, but without being labelled with a stigmatising ‘personality disorder’. This was confirmed by the second over-arching theme, Psychological Changes, which found that some of the participants objectified their EID. Perhaps more can be done before the initial session to inform participants of what is expected of them within the group, whilst also gauging their motivation to engage.
The findings for the effectiveness of the course for those who complete the course are very promising. The large effect sizes of pre–post treatment for symptoms of EID/BPD (QuEST) and medium effect sizes for depressive (PHQ-9) and anxiety symptomology (GAD) indicate a meaningful decrease in symptoms related to distress. These findings are also in line with the original STEPPS programme (moderate to large) and stepped care short-term treatment for BPD in reducing the symptoms of EID within participants (Blum et al., Reference Blum, St. John, Pfohl, Stuart, McCormick, Allen and Black2008; Bos et al., Reference Bos, Bas van Wel, Appelo and Verbraak2011; Harvey et al., Reference Harvey, Black and Blum2010; Hill et al., Reference Hill, Geoghegan and Shawe-Taylor2016; Laporte et al., Reference Laporte, Paris, Bergevin, Fraser and Cardin2018). However, effect sizes remain lower than in an evaluation of IAPT more broadly with pre–post PHQ-9 (r = .67) and GAD-7 (r = .73) scores showing large improvements following treatment (Clark et al., Reference Clark, Layard, Smithies, Richards, Suckling and Wright2009). Only 13% of the participants who completed treatment could be considered recovered in line with IAPT criteria. Still, the aim of STEPPS-EI is not primarily to address symptoms of depression or anxiety but rather emotional intensity, hence it would be misguided to evaluate the feasibility of STEPPS-EI based solely on these recovery rates (McCusker et al., Reference McCusker, Turner, Pike and Startup2018).
Limitations
First, this was an uncontrolled feasibility evaluation. There was no control group to establish the efficacy of STEPPS-EI. Second, there was a considerable amount of missing data, reducing ecological validity. Although the data reflect a real-world setting, the analyses do not take full account of those who dropped out. Third, there was no follow-up to the study. The longevity of symptom/trait improvement and whether individuals re-present to the service or other services is unknown. Fourth, the screening tool to assess for subthreshold BPD has not been psychometrically validated. Fifth, due to the nature of a dimensional scoring for BPD, there is uncertainty whether the sample is truly subthreshold. Individuals may have undiagnosed, full-syndrome BPD or temporary emotional difficulties without pervasive distress which would not constitute subthreshold. Moreover, there is controversy over what constitutes subthreshold BPD in relation to core behaviours, such as impulsivity, and how can STEPPS-EI measure and capture these different traits.
Future research
Despite the limitations, the findings from this evaluation create scope for further study. Future research should focus on understanding the reasons why participants decline treatment and drop out, and how this can inform future groups to improve the overall feasibility. Once this has been established and rates improved, the next step would be to conduct a randomised controlled trial to test the efficacy of STEPPS-EI with long-term follow-up. This could also be supplemented with a cost-effectiveness analysis to assess the potential economic benefits of the intervention.
Currently, ethnic minority groups and males are under-researched within STEPPS research, so further study into different socio-demographic groups would be beneficial. In addition, as outlined in the study limitations, validating a screening tool for subthreshold BPD would be advantageous. Contemporary research by Johnson and Levy (Reference Johnson and Levy2020) found that subtypes of subthreshold BPD may exist, suggesting that further adaptations to the STEPPS-EI programme may be needed in an effort to personalise treatment based on presentation phenotype.
In summary, this evaluation has presented the preliminary evidence of STEPPS-EI in primary care. The promising results of recruitment, acceptability and overall effectiveness indicate that STEPPS-EI is a possible treatment to address the current gap in treatment provision for patients presenting in primary care settings with subthreshold BPD. However, more needs to be done to further understand this client group and how treatments can be adapted to meet their needs and therefore improve the overall retention rate. Future research is crucial to understanding this.
Acknowledgements
We recognise that without the assistance of some key individuals we would not have been able to run this evaluation: Hilary Martin and Juliet Couche facilitated the data access to respective services, and Amy Dunn for additional consultation on the current direction and nature of PD research. We also thank clinicians past and present at Lighthouse Recovery Support and Bluebell House for insight into STEPPS and methodological issues.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interest
None.
Ethical statement
This evaluation was part of a wider service evaluation of STEPPS-EI within primary care, approved by the Clinical Audit Team for Sussex Partnership NHS Foundation Trust. Data analysed and collected were a part of routine data collection, with participants consenting for their anonymised data to be used for evaluation purposes.
Data availability
Anonymised data are available from the corresponding author upon reasonable request.
Supplementary material
To view supplementary material for this article, please visit: https://doi.org/10.1017/S1754470X2100009X
Key practice points
(1) Screening for subthreshold BPD traits in primary care is essential to identify greater clinical need.
(2) STEPPS-EI has potential to be a feasible treatment modality for individuals presenting with subthreshold BPD traits if issues with retaining participants are addressed.
(3) Despite this, STEPPS-EI can significantly reduce symptoms of emotional intensity, depression and anxiety.
(4) Prospective therapists may wish to focus on ways to increase the therapeutic alliance when forming a group to increase overall group retention.












Comments
No Comments have been published for this article.