Introduction
Autism spectrum disorders (ASD) are diagnosed when there is a triad of impairments in social communication, interaction and imagination, including restricted repetitive patterns of behaviours, interests, or activities (DSM-V; APA, 2013). People with ASD with more advanced social functioning and normal range intelligence can be referred to as high functioning (HF). When diagnosing an adult with an ASD, a retrospective assessment of impairments with an informant referring back to the patient's early developmental years is included to assess lifetime history of the triad of impairments. However, according to ICD-10 classification, people with HF ASD and no known history of language delay are diagnosed as having Asperger's syndrome (AS; ICD-10, WHO, 1993). The relevance of this diagnostic difference, however, appears to lessen with age (Gilchrist et al. Reference Gilchrist, Green, Cox, Burton, Rutter and Couteur2001) especially by adulthood where outcome in social and linguistic functioning is generally low (Howlin, Reference Howlin2003). The DSM-V diagnostic criterion for ASD therefore refers to a single and dimensional entity for ASD despite the DSM-IV having included AS (APA, 2013). It is noteworthy that this recent diagnostic change to ASD has been reported to have particularly poor sensitivity to those at the more cognitively able end of the spectrum that includes AS (e.g. McPartland et al. Reference McPartland, Reichow and Volkmar2012).
Research has shown that people with HF ASD have a number of deficits in both their social and non-social abilities. These deficits include theory of mind (Baron-Cohen et al. Reference Baron-Cohen, Leslie and Frith1985) and empathy (Baron-Cohen & Wheelwright, Reference Baron-Cohen and Wheelwright2004), facial expression processing (Humphreys et al. Reference Humphreys, Minshew, Leonard and Behrmann2007), linguistic pragmatics (Colle et al. Reference Colle, Baron-Cohen, Wheelwright and van der Lely2007), executive functioning (Ambery et al. Reference Ambery, Russell, Perry, Morris and Murphy2006), and central coherence (Jolliffe & Baron-Cohen, Reference Jolliffe and Baron-Cohen1999).
Despite the recent developments in ASD diagnostic criteria, and persistent attempts to research people on the autism spectrum experimentally, there is a very small evidence base guiding clinicians on how to treat this group of disorders. In particular, there is a paucity of evidence with respect to social skills training in adults with HF ASD. Social skills group interventions for adolescents and adults with AS and related disorders have found some positive outcomes using mixtures of modelling, coaching, role-playing and reinforcement through feedback (Mesibov, Reference Mesibov1984; Barnhill et al. Reference Barnhill, Tapscott Cook, Tebbenkamp and Smith Myles2002). In addition, another social skills group training programme found improvements in social skills and self-confidence according to family informants (Howlin & Yates, Reference Howlin and Yates1999). The evidence-based guidance that exists suggests increasing social skills in adults with AS by improving ‘instrumental skills’ such as eye contact as well as ‘fund of knowledge about social norms’ (or the unwritten rules of social interaction; Gaus, Reference Gaus2007). Gaus (Reference Gaus2007) also asserts that social cognition including abilities such as theory of mind should be targeted in social skills training.
Co-existing mental health difficulties are common in HF ASD (Ghaziuddin et al. Reference Ghaziuddin, Weidmer-Mikhail and Ghaziuddin1998). Depression is common although anxiety disorders are the most frequently found co-existing mental health difficulties in people on the autism spectrum (Skokauskas & Gallagher, Reference Skokauskas and Gallagher2010), possibly related, in part, to symptom overlap (Cath et al. Reference Cath, Ran, Smit, van Balkom and Comijs2008). For example, there is some research which shows that social anxiety in particular is related to certain social skill difficulties in people with HF ASD, although a fuller explanation of this relationship is lacking (Bellini, Reference Bellini2004). Nonetheless, there is therefore a need to develop treatment packages that address co-existing mental health difficulties, such as social anxiety and depression, in addition to social skills deficits within the context of HF ASD.
Most of the cognitive behavioural therapy (CBT) evidence base for the treatment of anxiety in HF ASD has been studied in children (Reaven & Hepburn, Reference Reaven and Hepburn2003; Sofronoff et al. Reference Sofronoff, Attwood and Hinton2005; Chalfant et al. Reference Chalfant, Rapee and Carroll2007; Sze & Wood, Reference Sze and Wood2007; Wood et al. Reference Wood, Drahota, Sze, Har, Chiu and Langer2009; Lang et al. Reference Lang, Regester, Lauderdale, Ashbaugh and Haring2010). There is, however, an emerging literature on CBT for anxiety and depression in adults with HF ASD.
CBT with innovative adaptations for the idiosyncrasies of people with AS of all ages has been suggested for the treatment of co-existing anxiety and depression (Anderson & Morris, Reference Anderson and Morris2006). More recently a detailed nomothetic model of vulnerability factors was published to inform cognitive behavioural practice with adults with AS (Gaus, Reference Gaus2011). In terms of treatment outcome there are results showing that a 14-week course of CBT was successful in reducing symptoms of both social anxiety and co-existing depression in a 23-year-old adult with AS (Cardaciotto & Herbert, Reference Cardaciotto and Herbert2004). Hare (Reference Hare1997) also demonstrated that 15 sessions of CBT led to clinically significant reductions in depression and a considerable although not entire attainment of therapy goals in a 26-year-old man with AS. A recent case series has also found group CBT to be helpful in the treatment of mood and anxiety difficulties in adults with AS (Weiss & Lunsky, Reference Weiss and Lunsky2010). A non-randomized controlled trial comparing CBT to treatment as usual for adults with HF ASD and obsessive compulsive disorder has also shown some success (Russell et al. Reference Russell, Mataix-Cols, Anson and Murphy2009).
In keeping with the high co-existence of anxiety and HF ASD, and with the paucity of a treatment evidence base in mind, the present single-case study aimed to investigate the use of CBT in the treatment of social skills deficits and social anxiety disorder in a man with AS.
Presenting problem
Diagnostic assessment
Luke (client's name and identifying details have been changed to preserve anonymity) was a 47-year-old man who had had a diagnostic assessment for ASD in the National Health Service. At the assessment interview there was reported evidence of difficulties in reciprocal social interaction, such as difficulties forming and maintaining friendships. His father's reports of Luke's childhood also suggested a lack of spontaneous seeking to share enjoyment, interest or achievements with other people. During the assessment interview a poorly modulated eye gaze was also observed and he had a tendency to close his eyes when talking.
There was no evidence of language delay although Luke's father recalled that there was very limited make-believe or social imitative play in childhood. There was also evidence of preoccupation with an interest in computers and computer languages. Luke reported that as a child he liked to copy tables and ‘data’, particularly from books on space and the solar system. Luke was assessed as having met his motor milestones on time despite being a little clumsy. Luke met criteria for AS according to ICD-10 criteria (WHO, 1993).
Neuropsychological testing at the time of Luke's diagnostic assessment showed that he had some difficulties with executive functioning in the areas of impulsivity and mild difficulties in selective attention over and above what would be expected in individuals with ASD diagnoses. He was also found to have some difficulties with visual recognition (possibly due to his poor eyesight), recall memory and theory-of-mind tasks.
Following his diagnostic assessment Luke was referred to psychology services for CBT due to difficulties with recurrent depression, social anxiety and social skills within the context of his AS.
Psychology assessment
Luke was assessed for treatment with CBT. During the assessment Luke was, at first, anxious and was concerned that he would not have enough to talk about. His eye contact was variable and he had some difficulties in turn-taking during conversation. It was important that, with some assistance, he was able to identify behaviours, thoughts and emotions that were preventing him from reaching his goals.
Luke described himself as ‘shy’ and as being constantly worried about what he would say in conversation with this reportedly making it difficult for him to initiate, maintain, and end conversations. Indeed he reported difficulties with socializing and accepted his diagnosis of AS in this context. Luke also reported difficulties with non-verbal communication. Luke described a number of social interaction/communication difficulties, including: literal interpretation, difficulties reading indirect intentions/requests, difficulties reading body language, talking at length about certain topics, lack of awareness of the listener's perspective and of subtle social rules such as how much eye contact to give. In addition, Luke said that he struggled with facial expressions and with remembering names and faces and that this made things difficult at work especially when meeting new people. He also reported a preference for one-to-one as opposed to group conversations owing to it being easier for him to keep track of what was going on. Luke also mentioned some difficulty with the use of humour and in figuring out whether people were being serious or joking in conversation, suggesting difficulties with language pragmatics such as sarcasm.
More generally, Luke spoke about situations at home and at work that lead to his experience of anxious apprehension and tension that he described as ‘freezing’ in conversations. Indeed Luke identified current symptoms of anxiety including tightness of chest, increased perspiration and heartbeat, feelings of restlessness and racing thoughts in reaction to the anticipation of social events. Furthermore, he reported a persistent concern about saying something that would invoke a negative judgement from other people. Luke's apparent fear of negative social evaluation was associated with avoidance and safety-seeking behaviours (SSBs) such as keeping what he said to a minimum and being careful to monitor what he said. Despite having minimal current symptoms of depression Luke linked his fear of negative evaluation to a low self-esteem.
Other difficulties that emerged in Luke's assessment were reports of difficulties in planning and organization and he related this to his difficulties in memory, and indeed problems in recall had been found in his neuropsychological assessment. Luke's strong interests in computers were also elicited during his psychology assessment.
Relevant history
Luke reported having one friend at primary school and was considered shy, nervous and slow yet determined by his teachers. He reported having been bullied at secondary school although he achieved a number of A–C GCSEs. He went on to Sixth Form but after 3 years dropped out without A-levels and completed a more vocational college course instead. Luke reported that he then worked as a labourer for a number of years. At the time of the present treatment Luke was working regular night shifts as a security guard.
Luke lived alone although he had a lot of support from his parents with finances and other activities of daily living including phone calls as prompts to go to work, for example. Luke expressed a desire to be more independent from his parents with his decision-making. In terms of his social life Luke reported having a small social network made up of two good friends without ASD that he met up with weekly and several online friends from an AS group whom he had occasionally met up with.
Standard measures
The use of standard measures supported the present psychology assessment.
Liebowitz Social Anxiety Scale (LSAS). The LSAS is a 24-item self-report measure of social anxiety. It consists of 11 items relating to social interaction and 13 items relating to public performance. Each item is rated on 4-point likert scales for both fear/anxiety and avoidance of social situations over the past week. It has been found to have a high internal consistency (Cronbach's α = 0.95) and it also correlated highly (0.85) with the clinician-administered version of the scale in a social anxiety group (Fresco et al. Reference Fresco, Coles, Heimberg, Liebowitz, Hami, Stein and Goetz2001).
Social Phobia Weekly Summary Scale (SPWSS). The six-item SPWSS measures social anxiety, social avoidance, self-focused vs. external attention, anticipatory processing, and post-event rumination using ratings on a scale from 0 to 8 for each item. It has been found to have a high internal consistency (Cronbach's α = 0.81) and it also correlated highly with the LSAS (Clark et al. Reference Clark, Ehlers, Hackmann, McManus, Fennell, Grey, Waddington and Wild2006).
Clinical Outcomes in Routine Evaluation – Outcome Measure (CORE-OM). The CORE-OM is a 34-item self-report measure designed to assess the efficacy and effectiveness of psychological therapies. It has been reported to have good sensitivity to therapeutic change, good internal and test–retest reliability, and good convergent validity (Evans et al. Reference Evans, Mellor-Clark, Margison, Barkham, Audin, Connell and McGrath2000, Reference Evans, Connell, Barkham, Margison, McGrath and Mellor-Clark2002).
Rosenberg Self-Esteem Scale (RSES). The RSES is a well-known and well-used 10-item measure of global self-esteem with each item using a 4-point likert scale (Rosenberg, Reference Rosenberg1965). There is recent evidence supporting the scale's item convergent (r = 0.57–0.79) and discriminant validity (r = 0.27–0.52) and its internal consistency reliability (α = 0.91) in a large sample of US adults (Sinclair et al. Reference Sinclair, Blais, Gansler, Sandberg, Bistis and LoCicero2010).
Beck Depression Inventory – II (BDI-II). The BDI-II is a well-known and well used 21-item measure of the severity of depression with each item using a 4-point likert scale. Its scores have shown good convergent validity (r = 0.71) with the Hamilton Depression Rating Scale and a high 1-week test–retest reliability (r = 0.93, Beck et al. Reference Beck, Steer and Brown1996a ). The measure has also shown a high internal consistency (α = 0.91, Beck et al. Reference Beck, Steer, Ball and Ranieri1996b ).
Treatment
Goals of treatment
Session 1 (goal setting)
Luke decided upon two main goals for his therapy. His first goal was to improve his social skills to help with life at work and home. To make this goal more specific and concrete he was given a checklist of potential areas of social skills that he could work on. Luke chose opening, maintaining, joining and closing conversations, and the non-verbal parts of conversations such as facial expressions and eye contact, which were all in keeping with his need for social skills training. He also chose talking positively about himself to others from this list, which was indicative of a need for some work on self-esteem. Luke's second goal was to manage his social anxiety to help with life at work and home and in this context he was aiming to make more friends. CBT was deemed an appropriate mode of treatment to address Luke's goals. A therapy contract adapted from Gaus (Reference Gaus2007) covering therapy boundaries/therapist accessibility, confidentiality, and appointment attendance and cancellation was then completed.
Conceptualization
Session 2 (individualized formulation)
An individualized cognitive behavioural formulation was formed collaboratively with Luke to direct treatment. This formulation included how earlier experiences of attempting to make friends and of living with AS had shaped his beliefs about the self (‘I'm different’), others and the future following Beck (1976). Evident in the dysfunctional assumptions elicited was a pattern of marked rigidity and extremes of all or nothing thinking about making friends (‘If I try hard and still can't make friends, then there's no point in trying’). Another dysfunctional assumption elicited was ‘If I enter a social situation then I will get something wrong and they'll know I'm different or they'll feel awkward’). Inherent in this assumption was Luke's awareness of his own social skills deficits and its perceived impact on others.
The longitudinal section of Luke's formulation was linked up with his day-to-day experiences of social anxiety at work based on Padesky's well-known format (Padesky & Mooney, Reference Padesky and Mooney1990). This covered links between thoughts (‘they might socially exclude me’), bodily sensations (e.g. increased heart rate), emotions (i.e. anxiety) and behaviours including those that appeared to be inadvertently giving others the impression that Luke was unapproachable (e.g. forcing a smile and closing his eyes) (Clark & Wells, Reference Clark, Wells, Heimburg, Liebowitz, Hope and Schneier1995). A more comprehensive and nomothetic formulation of Luke's difficulties based on Gaus (Reference Gaus2007) was held within the mind of the clinician and his supervisor who was an experienced clinical psychologist working as a specialist with clients with HF ASD. Indeed, the more comprehensive formulation highlighted that some unhelpful behaviours that Luke used were related to the social and communication difficulties inherent to his AS as opposed to SSBs, hence the need for social skills training. Luke's formulation was also written as a therapeutic letter focusing on empathic language covering his presenting problem as well as precipitating, predisposing, perpetuating, and protective factors. Also incorporated in the letter were the positive and negative meanings of AS to Luke, which had been elicited using a mindmap to promote a predominantly visual style of thinking (Anderson & Morris, Reference Anderson and Morris2006).
Course of therapy
A detailed treatment plan was written as a source of guidance for Luke's therapy. The plan was initially developed from a published social phobia protocol (Wells, Reference Wells1997) although many innovations for AS based on ASD literature were made. These innovations are noted and referenced in the session outlines. A substantial social skills training component was also added based on Gaus (Reference Gaus2007) and on treatment resources used in the service. The phases of treatment decided on were:
-
1. Goal setting, and conceptualization (sessions 1–2; as above).
-
2. Building a rationale for intervention (sessions 3–4).
-
3. Social skills training and planning and organizing (sessions 5–7).
-
4. Working with social anxiety (sessions 8–10).
-
5. Self-esteem and core-belief work (sessions 11–13).
-
6. Review and follow-up (sessions 14–15).
Sessions 3–4 (rationale for intervention)
To increase Luke's motivation for social skills training and exposure to anxiety-provoking social situations his formulation along with psychoeducation about the nature of anxiety was discussed. Thought bubbles were also used to make concrete the process of thinking about thoughts (Wellman et al. Reference Wellman, Baron-Cohen, Caswell, Gomez, Swettenham, Toye and Lagattuta2002). More specifically, they were used to illustrate how beliefs can change with duration of exposure to anxiety-provoking situations. The influence of Luke's SSBs, such as keeping to using short sentences, on the maintenance of anxious beliefs and anxiety was also explained in this context (Salkovskis, 1991). A decision matrix consisting of Luke's immediate and long-term advantages and disadvantages of ‘dropping’ his SSBs was used to help his motivation for treatment.
Sessions 5–7 (social skills training)
A hierarchy of conversation role-plays, graded by difficulty, was built using a manipulation of the form (i.e. problem-focused or social chat) and content (Luke's interests or general everyday things) of conversation and the level of input from each person holding the conversation. A variety of conversation cards and worksheets guided the role-plays and ensured that Luke practised opening, maintaining, closing and joining (with help from a volunteer) conversations. Luke also wanted to know more about eye contact and facial expressions in conversations. Informative handouts and modelling by the therapist to promote learning was used (Bandura, Reference Bandura1977). Social skills training was continually coordinated with subsequent social anxiety work as required (Gaus, Reference Gaus2007).
Planning and organizing. To target Luke's reported procrastination and organization difficulties a simple activity diary was introduced. Luke completed the diary for homework and in therapy he was assisted to integrate other activities into his week by adding them to the diary in advance. The diary also allowed him to record changes in his mood.
Sessions 8–10 (working with social anxiety)
In these sessions Luke's social skills training was reviewed before a shift in emphasis to understanding his social anxiety. During these sessions he was further socialized to the relevant processes found in Clark & Wells (Reference Clark, Wells, Heimburg, Liebowitz, Hope and Schneier1995) and his social skills training was distinguished from SSBs to be dropped. Luke's tendency to focus inwards on his own body tension when anxious in social situations was discussed. This self-focus was heightened by his tendency to close his eyes during social situations in which he also dwelled on what the feelings of tension meant to him making potential disconfirmatory evidence inaccessible to him. Luke saw his tension as an indication that his social interaction was going wrong, for example. The influence of this process on post-event rumination was also covered. Alongside this discussion some attention training techniques were used in session to help Luke experience that attention could be devoted to different things (Wells, Reference Wells1990). This training was then applied with exposure to social settings in session time and for homework. For example, Luke was given the task of noting everything he could about the people he was focusing on while interacting with them to promote an outward focus of attention.
To help Luke approach social situations cue cards and coping statements were used. These included reminders about social skills and phrases drawing on his work on looking for more helpful perspectives to negative automatic thoughts and mindfulness principles (e.g. thoughts are not facts) to help him be distanced from his anxious apprehension. This work allowed Luke to build adaptive strategies for coping with his AS, as opposed to promoting any SSBs which would have functioned as avoidance and prevented the disconfirmation of unhelpful beliefs (Thwaites & Freeston, Reference Thwaites and Freeston2005). Another key piece of work was a behavioural experiment where Luke's anxious predictions about how he came across during social interactions were falsified by contrasting his beliefs with the feedback of a volunteer who met Luke under controlled conditions.
Sessions 11–13 (self-esteem and core-belief work)
In Luke's later sessions time was devoted to building his self-esteem and collecting evidence against his core belief that he was different. Self-esteem was discussed and his strengths and positive qualities were elicited. Luke's proven drawing ability was positively reinforced with compliments and thought challenging led to the conclusion that there were more similarities than differences between him and colleagues at work hence working against his core belief about being different to others. Information from these sessions was listed visually for Luke.
Sessions 14–15 (review and follow-up)
Luke's review was spent reflecting on his therapy using an individually tailored CBT blueprint booklet created with his comprehensive therapy handouts. Luke felt sad that his therapy was ending as he explained that he thought that he had got on well with his therapist. This was reflected back to Luke as evidence that he could build meaningful relationships with people and that he could take the experience forward and do it again outside of therapy.
At his follow-up Luke said he was aware of improvement in certain areas of his life such as feeling more relaxed with people at work. He added, however, that it was difficult to see change outside of work such as in his number of friends.
Outcome
Figure 1 shows Luke's scores on the SPWSS. The scores illustrate a gradual reduction in variables specific to the model of social phobia that Luke's formulation was based on with some session-by-session variability (Clark & Wells, Reference Clark, Wells, Heimburg, Liebowitz, Hope and Schneier1995).

Fig. 1. Luke's session-by-session social anxiety as measured by the Social Phobia Weekly Summary Scale (SPWSS). Lower scores indicate less social anxiety.
Figure 2 shows Luke's scores on the LSAS. His total score of 70 at the start of therapy was similar to published means for people with social phobia (69.1, Baker et al. Reference Baker, Heinrichs, Kim and Hofmann2002; 74.5, Fresco et al. Reference Fresco, Coles, Heimberg, Liebowitz, Hami, Stein and Goetz2001). At the middle and end of therapy this score had reduced to 52 and 45, respectively, and was 26 at 1-month follow-up suggesting a continued improvement. This improvement was evident in both the fear or anxiety and avoidance subscales of the LSAS.
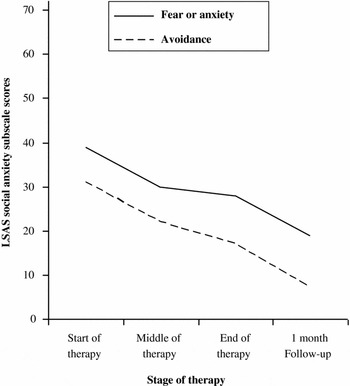
Fig. 2. Luke's social anxiety as measured by the subscales of the Liebowitz Social Anxiety Scale (LSAS) at the start, middle, and end of therapy and at 1-month follow-up. Lower scores indicate less social anxiety.
Figure 3 shows Luke's scores on the CORE-OM. His mean item score of 1.38 for level of global distress was above the clinical cut-off mean score for males (1.36) indicating clinically significant distress at the start of therapy. At the middle and end of therapy this score had reduced to 1.12 and 0.94, respectively, and was 0.44 at 1-month follow-up suggesting a continued improvement.

Fig. 3. Luke's level of global distress as measured by the Clinical Outcomes in Routine Evaluation – Outcome Measure (CORE-OM) at the start, middle, and end of therapy and at 1-month follow-up. Lower scores indicate less global distress.
The BDI-II showed a change from 10 at the start of therapy to 3 at both the middle and end of therapy and 1 at 1-month follow-up. These scores all suggested a clinically notable reduction in depression from the start of therapy and minimal depression at the end of therapy.
On the RSES Luke scored 12 at the start of therapy indicating low self-esteem. At both the middle and end of therapy however he scored 18 and at 1-month follow-up he scored 25. This latter score, at the least, is suggestive of normal self-esteem based on a mean from Luke's age-matched peers (23.17, Sinclair et al. Reference Sinclair, Blais, Gansler, Sandberg, Bistis and LoCicero2010). In addition to these formal outcome measures Luke had continued to maintain his working life, efforts to meet friends and hobbies in meditation.
Discussion
This single-case study reports results suggesting the successful use of CBT for social skills deficits and social anxiety disorder in an adult who received a late diagnosis of AS. The successful outcome is in keeping with the extant literature (Cardaciotto & Herbert, Reference Cardaciotto and Herbert2004; Weiss & Lunsky, Reference Weiss and Lunsky2010). There was a continued improvement in social anxiety from clinically significant levels at the start of therapy to scores well into the normal range at 1-month follow-up. This improvement appeared to be reflected in both levels of fear/anxiety, avoidance, and variables specific to the model of social anxiety guiding treatment (Clark & Wells, Reference Clark, Wells, Heimburg, Liebowitz, Hope and Schneier1995).
In summary, Luke showed continued improvements in social anxiety, depression, self-esteem and global distress all the way to 1-month follow-up suggesting the beginning of an enduring treatment effect. It is interesting that despite social skills and social anxiety being the main focus of the work a concomitant reduction in depressive symptoms was also observed. Reductions in depressive symptoms may have been due to Luke becoming behaviourally activated by collaborative efforts to improve his organization and activity levels (Hopko et al. Reference Hopko, Lejuez, Ruggiero and Eifert2003). However, more specific to Luke's formulation, his improved mood may have been due to a combination of real or perceived improvements in his social skills and/or an improved self-esteem.
It was helpful for Luke that his expectations were not unrealistic probably partly owing to the regular acknowledgement of how aspects of AS create real vulnerabilities and barriers to social relationships (Gaus, Reference Gaus2011). This therapeutic validation may well have assisted engagement. Highlighting Luke's interests and strengths, elicited and formulated in a visual manner following Anderson & Morris (Reference Anderson and Morris2006), may also have assisted engagement and contributed to his improved self-esteem. In terms of Luke's social skills practice in sessions it was helpful to draw from known sources of self-efficacy (Bandura, Reference Bandura1977). In formulating Luke's social anxiety, and in devising a course of therapy, consideration was given to if his behaviours were solely safety-seeking or sometimes more adaptive methods of coping (Thwaites & Freeston, Reference Thwaites and Freeston2005) in the context of his AS. His tendency to close his eyes during social interaction appeared to function as a way for him to briefly regulate his anxiety and stay in social situations. However, this behaviour made him appear less friendly and warm to the observer, as can be the case in safety-seeking according to the authors of the social anxiety model followed (Clark & Wells, Reference Clark, Wells, Heimburg, Liebowitz, Hope and Schneier1995). There was therefore a collaborative decision made to work on changing this behaviour, as his confidence in his social skills improved, and this went hand in hand with the intervention aim of changing Luke's processing priorities to a more external focus. Luke reported finding the behavioural experiment involving a volunteer particularly useful. In addition to the experiment targeting a thinking error of mindreading it may well have also been helpful in the broader context of the theory-of-mind difficulties found in those with ASD (Baron-Cohen et al. Reference Baron-Cohen, Leslie and Frith1985).
A main barrier to Luke making further improvement in therapy appeared to have been his difficulties with planning and organization. This barrier appeared in keeping with the executive dysfunction often found in people with ASD (Hill, Reference Hill2004). At follow-up his father attended and commented that he and his wife often tried to provide a daily timetable for Luke. Collaborative working with Luke's immediate family network may have been useful. It is noteworthy that Luke initially presented with marked all-or-none thinking (which is often present in depression and anxiety) about making friends and that this can often be compounded by rigid and repetitive behaviour patterns in those with ASD. However, this did not appear to create a barrier to his engagement with graded hierarchies of role-plays in social skills training. This was perhaps due to a clear conceptualization of Luke's all-or-none thinking at the dysfunctional assumptions level, early on in therapy.
A limitation of this clinical work, however, was that it could not directly address Luke's goal to make more friends. He nonetheless wished to be referred to a forthcoming social skills group for people with HF ASD. This way Luke would have opportunities to continue social skills training in a supportive environment where he could have positive peer-related experiences similar to models used in the literature (Mesibov, Reference Mesibov1984). Such group work may provide an avenue to help compensate for the known difficulties with generalizing learned behaviours found in this population (Ozonoff & Miller, Reference Ozonoff and Miller1995).
The design of the study also prevents more definitive statements about what had contributed to the apparent improvements in Luke's social anxiety, self-esteem, depression and more global wellbeing while he was in therapy and similarly up until his 1-month follow-up. The reliance on self-report also limits what conclusions can be made about the effectiveness of his therapy. Nonetheless, a comprehensive battery of these measures was regularly administered and consistent improvement appeared on them all.
Summary
In conclusion, this single-case study suggests that CBT with relevant innovative adaptations can be effective in treating social skills deficits and social anxiety disorder in the context of HF ASD. The recommended follow-up reading includes the social phobia protocol found in Wells (Reference Wells1997) and social skills training for adults with HF ASD found in Gaus (Reference Gaus2007) as these were drawn from in the present intervention.
Declaration of Interest
None.
Learning objectives
-
• To gain a basic understanding of higher-functioning autism spectrum disorders such as Asperger's syndrome (which is still a diagnostic condition using ICD-10 criteria).
-
• To gain knowledge of the existing evidence base with respect to social skills training and the treatment of anxiety and depression in high-functioning autism spectrum disorders.
-
• To understand better how the innovative adaptations required for the cognitive behavioural treatment of social skills deficits and social anxiety in Asperger's syndrome in the context of a single-case study link to positive outcome on several standard measures.






Comments
No Comments have been published for this article.