Introduction
Cognitive behaviour therapy (CBT) represents the leading form of psychological treatment for bulimia nervosa (BN), and has recently been reformulated as a treatment for eating pathology regardless of diagnosis, known as enhanced CBT, or CBT-E (Fairburn, Reference Fairburn2008; Fairburn et al. Reference Fairburn, Cooper, Doll, O'Connor, Bohn, Hawker, Wales and Palmer2009). The efficacy of CBT-E has been demonstrated for both adults and adolescents with BN, anorexia nervosa (AN), and atypical variants of these disorders (e.g. see Fairburn et al. Reference Fairburn, Bailey-Straebler, Basden, Doll, Jones, Murphy, O'Connor and Cooper2015). Despite this growing evidence base, CBT-E fails to achieve symptom abstinence in many patients, a shortcoming that is likely to be further pronounced in AN given the significant resistance to treatment compliance seen with this disorder (e.g. Abbate-Daga et al. Reference Abbate-Daga, Amianto, Delsedime, De-Bacco and Fassino2013; Halmi et al. Reference Halmi, Agras, Crow, Mitchell, Wilson, Bryson and Kraemer2005; Vitousek et al. Reference Vitousek, Watson and Wilson1998). A common issue is the reluctance of many patients to ‘give up’ some of the symptoms of the disorder, such as the need to regain weight – an issue that is central to recovery (e.g. Guarda, Reference Guarda2008); as Vitousek et al. (Reference Vitousek, Watson and Wilson1998) point out, we, as clinicians, ‘are proposing to fix one of the few parts of their [patients’] lives that they do not consider broken’ (p. 399).
Despite some evidence that motivation – or readiness to change – predicts outcome, this has been difficult to define (Vansteenkiste et al. Reference Vansteenkiste, Soenens and Vandereycken2005). Low levels of motivation can be reflected in limited behavioural progress with patients often showing ‘a strong resistance to their therapists’ efforts towards improvement’ (Abbate-Daga et al. Reference Abbate-Daga, Amianto, Delsedime, De-Bacco and Fassino2013, p. 2). Despite recognition of this difficulty for many years (e.g. Amdur et al. Reference Amdur, Tucker, Detre and Markhus1969; Bruch, Reference Bruch1978), there has been ‘little in the way of addressing the treatment-resistance issue in AN’ (Abbate-Daga et al. Reference Abbate-Daga, Amianto, Delsedime, De-Bacco and Fassino2013, p. 13). In some cases, asking patients to leave, or suspend, treatment can represent a ‘last-resort opportunity’ (Masson and Sheeshka, Reference Masson and Sheeshka2009, p. 119), a decision that is individual to each patient but which can have positive side-effects (e.g. Tozman and DeJesus, Reference Tozman and DeJesus1981). Breaks have been suggested in treatment manuals for both eating disorders (EDs) and other psychological problems and are often considered when there is a pattern of limited behavioural change. Suspension of treatment has been proposed as a means for addressing low levels of motivation, borrowing from the concept of ‘therapy-interfering behaviours’ in dialectical behaviour therapy (e.g. Linehan, Reference Linehan1993). For example, Waller et al. (Reference Waller, Cordery, Corstorphine, Hinrichsen, Lawson, Mountford and Russell2007) suggest that a ‘brief session’ can be a powerful tool to ‘re-engage a patient who is undertaking therapy interfering behaviours’ (p. 117). A comprehensive review is held between patient and therapist, often culminating in a set of short-term goals that are aimed at fostering engagement in the therapeutic process and can often result in patients understanding that therapy ‘is contingent on their participation’ (Waller et al., Reference Waller, Cordery, Corstorphine, Hinrichsen, Lawson, Mountford and Russell2007, p. 118).
Masson and Sheeshka (Reference Masson and Sheeshka2009) explored premature termination of treatment through interviews with seven clinicians working on an in-patient unit, but as yet there has been little discussion of this within out-patients and also little detailed description using clinical information (e.g. case studies). Clinicians interviewed in the study of Masson and Sheeshka suggested that asking patients to suspend treatment is necessary to maintain a recovery-oriented atmosphere within ED treatment, with one noting that it can offer ‘a wake-up call to the patients to try something different or consider coming back at a later date when they feel better able to take what's offered’ (p. 119). Thus, there is some suggestion that clinicians view having ‘strong internal reasons to want to change’ (p. 116) as important in treatment completion. Other findings from the interviews suggested that suspension of treatment can maintain treatment integrity, and thus a strong focus on recovery, although clinicians were aware that there were rarely clear guidelines for this.
It is not yet known how suspension or premature termination of treatment can affect response and outcome, clearly important when considering decisions of this nature. The following case study describes the delivery of a CBT-based intervention to an individual presenting with AN where a break was taken after initial stages. Single-case designs may represent the optimal design for looking at specific factors of treatment that might be responsible for change (see Elliott, Reference Elliott2002), and allow for a more detailed analysis of motivational dynamics (Vansteenkiste et al. Reference Vansteenkiste, Soenens and Vandereycken2005) than large-scale designs, and therefore one objective of the study is to illustrate how consideration of a ‘therapeutic break’ can have positive side-effects, even when faced with significant risk (see Masson and Sheeshka, Reference Masson and Sheeshka2009).
Additional aims are to describe some of the difficulties encountered in the routine treatment of AN and propose factors to be considered in making a decision about discontinuing CBT. The case study will also illustrate how CBT for EDs can be delivered flexibly, whilst covering core elements such as achieving a healthy body weight, self-monitoring, and symptom reduction (NICE, 2017; see also Fairburn, Reference Fairburn2008; Waller et al., Reference Waller, Cordery, Corstorphine, Hinrichsen, Lawson, Mountford and Russell2007). Finally, this case study aims to build on the discussion around therapeutic breaks and to reflect on strategies for dealing with slow therapy progress (see also Geller, Reference Geller2002).
Method
Informed consent
For this study, the author retrospectively reviewed a case where a ‘therapeutic break’ was taken following initially limited progress. The individual concerned (‘Poppy’) provided consent to having her case submitted for publication in a peer-reviewed journal.
Presenting problem
Background
Poppy was an 18-year old student when she was referred to an adult ED service (EDS) for difficulties maintaining her weight at a healthy level. She had previously been seen within Child and Adolescent Mental Health Services (CAMHS) and received treatment as a day-patient (with a brief in-patient stay) for approximately three months. Her ‘weight for height’ at discharge from CAMHS was 88.5% (approximately BMI 18.1), where 100% is the median BMI relative to an individual's age. Poppy initially refused to be assessed by adult services but was reviewed by her general practitioner (GP) and, after approximately one month, consented to being seen for an initial assessment.
Assessment
Poppy reported concerns about her shape and weight, which were important in her self-evaluation (commonly known as ‘overvaluation’ of shape and weight). She described fear of fatness, perceived disturbance in body shape, and low body weight (BMI 17.0) and thus met DSM-5 criteria for anorexia nervosa – restricting subtype (APA, 2013) at a mild level of severity.
In her initial assessment, she engaged well and reported compulsive exercise and a history of purging (although not in the most recent year before her assessment). Poppy reported that her mood was generally ‘OK’, rating it as 7/10, although it could be affected by guilt related to eating, and she was prescribed an anti-depressant (the starter dose of a selective serotonin re-uptake inhibitor) which was maintained over the course of treatment. She had previously been noted to be suffering from osteopenia and was amenorrheic at the time of assessment. Poppy did not smoke, and drank alcohol occasionally (in a social capacity). She lived at home with her parents and younger sister and said that everything was fine apart from issues around her eating, which ‘sparks unnecessary arguments’. A developmental review suggested a family history of depression and no significant problems at birth or in early childhood. Her illness began around the age of 15 before a holiday abroad, and she reported becoming ‘paranoid’ about weight gain after returning home. She described a ‘rigid’ calorie limit and participated in athletics and other active hobbies.
Assessment measures
Alongside clinical interview, Poppy completed the Eating Disorder Examination questionnaire (EDE-Q; Fairburn and Beglin, Reference Fairburn and Beglin1994), Clinical Impairment Assessment questionnaire (CIA; Bohn and Fairburn, Reference Bohn, Fairburn and Fairburn2008), Rosenberg Self-Esteem Scale (RSES; Rosenberg, Reference Rosenberg1989), and Clinical Outcomes in Routine Evaluation – Outcome Measure (CORE-OM; Barkham et al. Reference Barkham, Margison, Leach, Lucock, Mellor-Clark, Evans, Benson, Connell, Audin and McGrath2001). The results suggested that she was experiencing significant symptoms of an ED and related impairment. They also suggested a mild level of psychological distress (above the suggested clinical cut-off of 10; see Connell et al. Reference Connell, Barkham, Stiles, Twigg, Singleton, Evans and Miles2006), and low self-esteem. A summary of these scores is provided in Table 1 (see below).
Table 1. Summary of scores on self-report measures at start-of-treatment, end-of-treatment, and five-month follow-up

Problem rating: ‘how much have your problems distressed you in the last 2 weeks?’; CIA: Clinical Impairment Assessment questionnaire; CORE-OM: Clinical Outcomes in Routine Evaluation – Outcome Measure; EDE-Q: Eating Disorder Examination – Questionnaire; RSES: Rosenberg Self-Esteem Scale; RCI Min.: minimum required value for reliable change (see text for details). n/a, not applicable; *exceeded RCI Min.; **below caseness and exceeded RCI Min.
In order to quantify the significance of any clinical changes during treatment, reliable change indices (RCI) were calculated according to the suggestions of Jacobson and Truax (Reference Jacobson and Truax1991), with a p < .05. Specifically, the difference in scores (from start of treatment) was divided by the standard errors of the difference of each test. The standard error of measurement for the tests was estimated, generally based on quoted test–retest reliabilities, for the EDE-Q from Mond et al. (Reference Mond, Hay, Rodgers, Owen and Beumont2004a), the CORE-OM from Evans et al. (Reference Evans, Connell, Barkham, Margison, McGrath, Mellor-Clark and Audin2002) from their non-clinical sample, the RSES from a US college sample (Robins et al. Reference Robins, Hendin and Trzesniewski2001), and the CIA from a sample of university females in Norway (Reas et al. Reference Reas, Ø, Kapstad and Lask2010). In addition, scores on the CIA and CORE-OM can be used to determine ‘caseness’, a cut-off for clinically significant change. For the EDE-Q, a score on the Global subscale ≥2.3 was taken (see Mond et al. Reference Mond, Hay, Rodgers, Owen and Beumont2004b). Results are therefore interpreted with relevance to RCI and caseness.
Treatment
Treatment rationale
Following assessment and discussion with the wider multidisciplinary team, a course of CBT was felt to be helpful – in part as previous reviews with CAMHS suggested that Poppy might benefit from an ‘adult model’ of care. Although some tenets of CBT-E were not strictly adhered to (e.g. twice weekly sessions were not possible due to service constraints), treatment followed this approach with the initial stage focusing on formulation, self-monitoring and regular eating. There was a focus on reaching a healthy body weight, as well as an overall goal of symptom reduction (see NICE, 2017). Later stages were to address the maintaining factors of Poppy's illness and preventing relapse (see Fairburn, Reference Fairburn2008, for details).
Case conceptualization
A provisional formulation based on the CBT-E model (Fairburn, Reference Fairburn2008) is shown in Fig. 1, and was developed collaboratively during stage 1 (which usually runs up to session 7) of treatment. Key maintaining factors of Poppy's eating problem included current low weight, dietary restraint and restriction, body image dissatisfaction, and experiencing feelings of ‘fatness’. Poppy engaged well with this, reiterating that her body shape and sense of control were important in her self-evaluation. She said that control over her eating was important so as to safeguard against overeating and thus excessive weight gain, and Poppy was fearful that she ‘won't stop’ gaining weight.
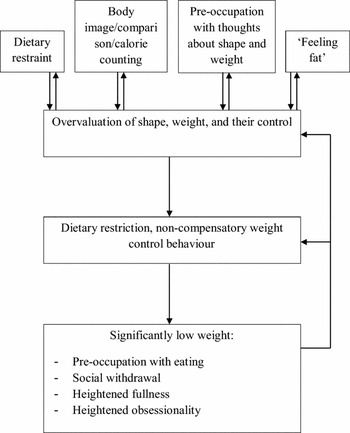
Fig. 1. Formulation
Goals of treatment
Poppy's goals at the start of treatment were to get to a healthy weight (e.g. restart menstruating) and be comfortable with it, be less rigid with her eating (to ‘eat what I fancy’), to stop comparison and body checking, to eliminate thoughts of calories and weight loss, and to be able to look forward to things other than weight loss. These goals were discussed and a treatment plan made, based on CBT-E and the provisional formulation (Fig. 1).
Course of therapy
Poppy's treatment consisted of two separate ‘courses’ of treatment, punctuated by a planned ‘therapeutic break’. For ease of understanding, the current article refers to the course of treatment based on one continuous timeframe (of 72 weeks from assessment to follow-up).
Initial course
Poppy initially engaged well with many elements of treatment. She consented to being weighed weekly, completed self-monitoring forms appropriately, and did not weigh herself between sessions. However, she was ambivalent about recovery and found it difficult to commit to making dietary change; as a result, she gradually lost weight, and her BMI had declined from 16.0 to 15.6 by session 3 (week 4; see Fig. 2). Poppy reiterated her goals, including being at a normal weight, but said that, in spite of having positive factors in her life (e.g. friends, family), lacking motivation was ‘the problem’, and often found that she couldn't ‘be bothered’ to change her eating. The therapist felt that these issues reflected limited internal motivation and struggling to see that ‘recovery is better than the disorder’ (Masson and Sheeshka, Reference Masson and Sheeshka2009, p. 118).
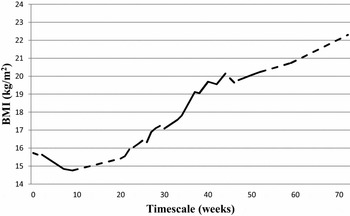
Fig. 2. Change in BMI over course of treatment
At session 3, the option of more intensive treatment (see below) was discussed as Poppy was continuing to make little progress (e.g. see Dalle Grave, 2013). She had made some changes to her dietary intake, but this had resulted in no significant weight regain. Poppy said that her family felt that more intensive treatment was a good idea, but that she was in ‘two minds’ about it, and thus some time was spent in the session reflecting on this ambivalence. Poppy raised the option of a break from treatment, stating that this would afford her time to reflect on her options. The therapist thought this was a good idea given the lack of progress, concerns about motivation, and continued weight loss, indicating a physical feature of concern that should prompt consideration of therapeutic ‘readiness’ (Fairburn, Reference Fairburn2008; Murphy et al. Reference Murphy, Straebler, Cooper and Fairburn2010). It was also considered that, while Poppy was making some dietary changes, these were of insufficient magnitude to effect weight regain. A review was therefore arranged after a break of one month, similar to the protocol of the ‘five-minute session’ described by Waller and colleagues (Reference Waller, Cordery, Corstorphine, Hinrichsen, Lawson, Mountford and Russell2007).
Over the intervening month, alternatives to taking a break were considered. In addition to hospital treatment, other alternatives included more frequent contact (such as daily e-mailing; Fairburn, Reference Fairburn2008, p. 176) and holding regular review sessions, although Poppy's reluctance to consider these suggested that they would not bring about any significant change. Reflecting on the break, she reported that it was difficult not having sessions and ‘someone to talk to’ but said that the longer gap between sessions gave her an opportunity to ‘take advantage’ (for example by going running). At this review meeting (week 8), Poppy's weight had decreased (BMI 14.8) and she stated that her eating didn't ‘seem like a big enough problem’, and it was discussed how this conflicted with the opinions of professionals and her family. The therapist suggested she spend some time at home evaluating her decision (e.g. pros and cons) before meeting again and also provided hand-outs on regular eating (see also Waller et al., Reference Waller, Cordery, Corstorphine, Hinrichsen, Lawson, Mountford and Russell2007).
At the next appointment one week later (week 9), Poppy had reflected on the hand-outs and noted some sequelae of her illness (e.g. cold hands and feet) and began to draw links between regaining weight and being able to do things she enjoyed. She and the therapist briefly discussed what she might be able to do to change her eating, although concerns about her ongoing weight loss were noted. Although the therapist and Poppy met for reviews during this time, CBT was suspended with the explicit understanding that any subsequent meetings did not constitute therapy per se but rather monitoring of risks (e.g. weight) – they did not follow a typical session structure (see Fairburn, Reference Fairburn2008, p. 62), and were briefer than formal CBT-E sessions.
It was also felt at this time that Poppy would benefit from being seen by a dietitian, which was arranged for the following week. The dietitian reiterated many of the therapist's suggestions, and also gave advice regarding nutritional requirements. Poppy was also seen by a doctor at the EDS, who strongly advised day-patient care and provided advice (although the therapist maintained regular contact with Poppy's GP, who took responsibility for physical monitoring). During the ‘therapeutic break’, Poppy was weighed at her GP surgery and also attended for regular blood tests and an ECG in light of some reported chest pains, a known symptom in AN (see Birmingham et al. Reference Birmingham, Stigant and Goldner1999). A positive aspect of this approach was that there was good communication and a unified approach (e.g. see Dalle Grave, 2013, pp. 44 – 49) between clinicians; the service benefits from having a multidisciplinary team based within one unit. Poppy was also closely supported by her family and the therapist was in regular contact with her GP. The general treatment plan was summarized in written communications, with a clear plan of monitoring in place to safeguard against the risks of rapid physical deterioration.
Second course
A planned review of Poppy's care was held in week 20, during which time Poppy had experienced a ‘change of heart’, and had reflected on the negative consequences of her illness. As a result, Poppy said that she had ‘upped’ her dietary intake and was positive about restarting CBT. Her weight had increased to a BMI of 15.4, having dropped to a nadir of 14.3 (falling within the ‘extreme’ range of AN; APA, 2013), and thus the therapist felt it was appropriate to recommence out-patient CBT-E.
In the first session (session 5, taking into account the first course of treatment), the therapist and Poppy returned to her formulation (see Fig. 1) and revisited her goals. Typically in CBT-E, a ‘transitional stage’ involving a review of progress would usually take place around this time; however, this was foregone given the most recent review and that barriers to change had been openly discussed and, to some extent, addressed. Self-monitoring was re-started, and the maintaining factors in Poppy's ED were highlighted. Treatment moved on to stage 3 of CBT-E, and thus two subsequent sessions covered overvaluation of weight and shape, identifying how Poppy's current self-perception was heavily influenced by her eating and that an ‘ideal’ evaluation was more balanced. Despite her low weight, Poppy maintained a number of pastimes; however, her ability to engage in them was poorer when she was at her most ill. In CBT-E, addressing ‘marginalization of other areas’ aims to help patients engage in areas of life that have been pushed aside (Fairburn, Reference Fairburn2008). In Poppy's case, this was addressed through improving other ED symptoms and reducing their impact on concurrent activities, thus increasing the subjective importance of these domains and developing their prominence in her self-esteem and self-perception.
Sessions also covered Poppy's eating style (i.e. behaviours around mealtimes; see Fairburn, Reference Fairburn2008, pp. 81–82); she was regaining weight more consistently at this point in treatment (BMI approximately 16.3; see Fig. 2), but continued to demonstrate ED behaviours, such as dietary restraint (i.e. attempts to restrict intake, such as leaving crumbs), which Poppy said ‘makes the thoughts easier’. A flexible approach was taken, with some sessions during this time looking at ‘rules’ around eating and dietary restraint, whilst also considering overvaluation of eating and using Poppy's weight graph to tackle negative predictions about making dietary changes (e.g. that her weight might increase beyond control). For example, Poppy began to introduce more ‘starchy’ foods (e.g. bread) and discussed the effects of such rule-breaking with the therapist (see Fairburn, Reference Fairburn2008, pp. 126–134). She worked to address avoiding other foods by completing a ‘feared foods’ worksheet, listing avoided foods and dividing them into groups based on how difficult Poppy would find it to eat themFootnote 1 .
Other elements of stage 3 included review of target weights and continued exposure to challenging events (for example, eating at a friend's birthday party). The treatment also covered the ‘overvaluation of control’, by addressing the different behaviours that maintain this aspect of the core psychopathology; self-monitoring forms were used to reflect on how certain behaviours (e.g. calorie-counting) maintained this overvaluation, and Poppy often reported similar themes to those observed in previous sessions. As noted in Fairburn (Reference Fairburn2008), dietary rules often remain an important maintaining mechanism and thus necessitated continued attention in sessions. At this stage in treatment, Poppy had begun to notice some positive aspects to weight regain; she had recommenced menstruation and also noted some other physical and psychological changes such as feeling more ‘alive’, and having thicker hair. Work in therapy continued by looking at dietary rules, and also set a ‘band’ for maintaining a healthy weight. Poppy expressed a wish to look at body image, and thus some sessions were spent discussing the nature of body image, body checking and mirror use (see Fairburn, Reference Fairburn2008). Analogy was drawn to the treatment of anxiety disorders (see Jenkins, Reference Jenkins2013) in terms of avoidance, attentional bias and reassurance-seeking (see also Fairburn, Reference Fairburn2008, pp. 106–107). As a final element to stage 3, two sessions were spent discussing ‘feeling fat’ (see Fairburn, Reference Fairburn2008, pp. 113–116) as well as homework between sessions, using self-monitoring forms to record such experiences.
At this stage, Poppy felt that it would be beneficial to meet less frequently (fortnightly); she was expanding her hobbies and interests and was also applying for jobs (cf. ‘marginalization of other areas’). She and the therapist thus began stage 4 and the construction of a ‘maintenance plan’ over two sessions. Sessions included discussion and completion of a long-term maintenance (relapse prevention) plan, looking at areas such as spotting setbacks early on and ensuring that progress is maintained. They also discussed phasing out certain treatment procedures, reducing reliance on self-monitoring, for example, and encouraging patients to start weighing themselves, often at home (see Fairburn, Reference Fairburn2008, pp. 187–188). However, Poppy said that she didn't really weigh herself before she was ill so would rather not monitor this at home. Poppy also completed end-of-treatment questionnaires and, as per standard practice in the service (and in line with the recommendations of Fairburn, Reference Fairburn2008), a further set at a longer follow-up (five months post-treatment).
Outcome
The results of key self-report measures are summarized in Table 1. Poppy's scores on the EDE-Q Global decreased from 4.74 at start-of-treatment to 0.41 at 5-month follow-up. By comparison, an Australian study (Mond et al. Reference Mond, Hay, Rodgers and Owen2006) reported a mean score of 1.59 for young adult women (aged 18–22 years), suggesting that Poppy experienced a significant reduction in symptoms of an ED with her scores falling low relative to individuals in her age group, and below a suggested cut-off of 2.3. Improvements on the CIA, a measure of psychosocial impairment, were also seen, with end-of-treatment and follow-up scores falling below the suggested clinical cut-off of 16 (Bohn et al. Reference Bohn, Doll, Cooper, O'Connor, Palmer and Fairburn2008). Improvements were also observed on a measure of psychological distress and in self-esteem (although this was less pronounced).
Anecdotally, at follow-up Poppy said that she felt happy with her eating and reflected that she now eats ‘what I want’, commensurate with the goals she identified at assessment. She was in paid employment as well as studying in higher education in preparation for university. Her weight was within the normal range (BMI 22.3) and Poppy reported feeling fine about this. She thought that some of the change would be due to an increase in muscle mass as she said that she was trying ‘to tone up’, although it is notable that her reported excessive exercise (as assessed by the EDE-Q) had ceased by end-of-treatment.
Discussion
This case study summarizes a course of CBT for AN, based on the model of Fairburn (Reference Fairburn2008), which necessitated a ‘therapeutic break’ following an initial lack of progress. It expands on the work of Masson and Sheeshka (Reference Masson and Sheeshka2009), who interviewed clinicians regarding treatment completion, by giving a clinical example of how a therapeutic break can contribute to positive outcomes. Although confirmation is not possible, it was the view of the treating clinician that this break effected changes that led ultimately to clinical improvement. Although the patient's stated goals changed little, she later reflected that her behaviours were not in harmony with how she wanted to live her life and it is possible that there was a shift in the locus of her motivation – from external to internal (see Geller, Reference Geller2002; Masson and Sheeshka, Reference Masson and Sheeshka2009). While it may have been possible to improve engagement through greater use of motivational interviewing techniques or more intensive treatment, there may be some patients who demonstrate a ‘persistent lack of motivation to change’ which is immune to this (Masson and Sheeshka, Reference Masson and Sheeshka2009, p. 122). Furthermore, judicious and appropriate use of a therapeutic break may be one way of addressing problems in collaboration, reducing therapy-interfering behaviours by focusing on the task in hand (Waller et al. Reference Waller, Cordery, Corstorphine, Hinrichsen, Lawson, Mountford and Russell2007; see also Linehan, Reference Linehan1993).
Poppy initially attended in the face of at least some external pressures (e.g. from her family). Over time, and perhaps influenced by the therapeutic break, she began to report greater acceptance of the target behaviours, such as weight regain (i.e. a shift towards intrinsic motivation). In spite of the challenges inherent to recovery, Poppy appeared to ‘accept the personal importance of changing behaviour’ in line with her own values (Vansteenkiste et al. Reference Vansteenkiste, Soenens and Vandereycken2005, p. 213), and thus her motivation appeared to change during treatment in terms of both its quantity and quality (Deci and Ryan, Reference Deci and Ryan2000), and she also ‘willingly enacted’ the decision to pause treatment, which may have promoted maintenance of change (Vansteenkiste et al. Reference Vansteenkiste, Soenens and Vandereycken2005).
It would be an oversimplification to attribute change in this case to a single intervention or decision and it is likely that the treatment, based on CBT principles, was delivered in line with motivational theory, applied throughout and in line with Poppy's readiness status (Geller, Reference Geller2002; see also Dalle Grave, 2013). Poppy was also prescribed an anti-depressant, which may have contributed to (although is unlikely to fully explain) her improvement. The prescribed dose remained constant throughout CBT and there is little evidence that medication alone is effective in the treatment of AN, although may have benefit in the treatment of related issues, such as depression (e.g. Lebow et al. Reference Lebow, Sim, Erwin and Murad2013). The assistance of colleagues in this case was also important – Poppy met with both a dietitian and a doctor in psychiatry within the EDS, who reinforced messages about the importance of treatment and did not contradict what was covered in therapy sessions. Poppy was in contact with her GP, who was updated regarding her progress and also monitored Poppy's physical and general mental health. The importance of having team members sharing similar philosophies in treatment has been previously emphasized in CBT for eating disorders (e.g. Dalle Grave et al. Reference Dalle Grave, Pasqualoni and Calugi2008; Dalle Grave, 2013) and may have been an important factor in the current case. Similarly, Poppy's parents were also significant in her recovery, and Poppy later recalled her Dad saying to her that being ill was ‘no way’ to spend her life. It may also be that ‘non-therapy processes’ brought about change in Poppy's behaviour (Elliott, Reference Elliott2002), such as life events or psychobiological factors outside of the treatment. However, there were few significant events noted, outside of those that are often seen in successful treatment such as greater engagement with social activities and improvements in general health.
Another issue noted by Masson and Sheeshka (Reference Masson and Sheeshka2009) relates to trust, which may also have been critical. Risks were taken by the clinician, patient, and her family – treatment was ceased when Poppy's BMI approached the cut-off for ‘extreme severity’ (APA, 2013) and the nadir was below this. Further deterioration may have caused greater medical complications (e.g. Mehler et al. Reference Mehler, Gray and Schulte1997) in addition to precipitating more intensive treatment. Her family, while understandably concerned, were supportive of the treatment plan and liaised closely with Poppy's care team.
It should be noted that, while CBT-E was the overarching treatment approach, some elements were not followed: treatment sessions were not held twice weekly during stage 1 (see also Knott et al. Reference Knott, Woodward, Hoefkens and Limbert2015), and only a limited amount of time was spent on addressing motivation. It has also been suggested that CBT-E should be continued for longer periods before considering more intensive treatment (Fairburn, Reference Fairburn2008; Dalle Grave, 2013). Conversely, many ‘core elements’ of CBT-E were followed (e.g. weekly weighing, self-monitoring, providing education, exposure). It has been demonstrated that amalgams of different CBT manuals can produce treatment effectiveness in ‘real world’ settings (e.g. Turner et al. Reference Turner, Marshall, Stopa and Waller2015), and therefore that a flexible approach to the delivery of CBT can be effective. Although measures were given at start-of-treatment, end-of-treatment, and follow-up, a significant shortcoming of the current study was the lack of questionnaires during the therapeutic break and a lack of session-by-session monitoring of cognitive symptoms, which may have given greater insights, for example into the timing of symptom change. However, regular monitoring of weight was conducted, indicating changes in a key symptom of AN (e.g. Accurso et al., Reference Accurso, Ciao, Fitzsimmons-Craft, Lock and Le Grange2014; see also NICE, 2017) that were observed over the course of treatment. Another obvious shortcoming is the absence of a measure assessing motivation, such as the Readiness and Motivation Interview (Geller and Drab, Reference Geller and Drab1999), and evaluation of change may have also benefited from a measure of helpful aspects of therapy (e.g. Llewelyn, Reference Llewelyn1988). In common with other case studies, it is difficult to determine causation in this case and it may be that non-therapy factors were responsible for change. However, evidence has been presented to challenge this hypothesis.
This case study describes treatment of AN using many core features of CBT-E. It is not intended to be used as a template for successful delivery of CBT-E but has illustrated use of responding to motivation within individual psychological therapy. The considered use of a ‘therapeutic break’ was hypothesized to have effected a change in Poppy's motivation, although it is possible that other approaches may have brought about a similar outcome. Most notably, little time was spent in the current case encouraging Poppy to learn more about the pros and cons of her illness, which is recommended as part of CBT-E for underweight patients (see Fairburn, Reference Fairburn2008).
Summary
Resistance to treatment in anorexia nervosa has been observed for decades but we are still relatively naïve in our understanding of how to address it. One option (e.g. Masson and Sheeshka, Reference Masson and Sheeshka2009) is to agree a break in treatment, which can afford time to reflect and evaluate options for moving forward. This case study describes such a ‘therapeutic break’ in a course of out-patient CBT and explored the possible impact of this choice. Positive outcomes were observed following treatment, and the relevance of taking a ‘therapeutic break’ is considered.
Main points
-
(1) CBT for eating disorders fails to achieve symptom abstinence in a number of patients.
-
(2) When progress is limited in active treatment, a therapeutic break offers one option to help foster engagement in the process of change.
-
(3) This case study describes CBT for anorexia nervosa, punctuated by a therapeutic break.
-
(4) Following the break, the individual was able to commit to core treatment strategies and engaged well with CBT, experiencing positive changes in a number of areas.
-
(5) Use of a therapeutic break can be helpful in CBT for anorexia nervosa, although clinicians should consider this option with adequate reflection and review.
Acknowledgements
The author would like to sincerely thank Poppy for her consent and input, and for having the courage not only to face her illness and recovery but also to permit publication of her treatment journey.
Ethical statement
The author asserts that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, and its most recent revision.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interest
Dr Jenkins has no conflict of interest with respect to this publication.
Learning objectives
-
(1) To gain an understanding of some of the difficulties in delivering outpatient CBT for anorexia nervosa.
-
(2) To illustrate treatment of anorexia nervosa through flexible use of evidence-based treatment.
-
(3) To consider use of therapeutic breaks in psychological therapy to enhance intrinsic motivation.






Comments
No Comments have been published for this article.