Introduction
In recent years, there has been increased focus on mental health services providing more timely and cost-effective psychological interventions (e.g. NHS England, 2015). During this time, the percentage of adults accessing mental health services has also increased (NICE, 2017), and these pressures have led to services needing to find creative ways to meet the increasing demand. One of the biggest advancements in adult mental health care provision in England has been the development of Improving Access to Psychological Therapies (IAPT) in primary care. IAPT was developed as part of the roll-out of a stepped-care model to mental health in 2008, with a view to ensuring timely access to evidence-based psychological interventions for common mental health problems, thought to be better for both individuals and the economy, through facilitating return to work (Wakefield et al., Reference Wakefield, Kellett, Simmonds-Buckley, Stockton, Bradbury and Delgadillo2020). Since the national roll-out of IAPT services, there has been increased research into, and evidence for, brief psychological interventions (BPIs).
BPIs are typically interventions that have the following key characteristics: (1) they include some of the key components of longer-term evidence-based psychological interventions, (2) they are brief in nature in that they are delivered over fewer sessions, and (3) they are designed to be delivered by staff with less specialised training (paraprofessionals). However, it should be noted that in the literature the phrase ‘brief psychological interventions’ has also been used when the intervention is delivered by professionals and not paraprofessionals (e.g. Sprong et al., Reference Sprong, Clare, Galante, Crawford and Jones2021).
In terms of delivery intensity, Shafran et al. (Reference Shafran, Myles-Hooton, Bennett and Öst2021) proposed that brief cognitive behavioural therapy (CBT) could be defined as either low intensity (utilising self-help materials, totalling ≤6 hours of contact time, being ≤30 minutes per session, and delivered by trained practitioners or supporters) or brief high intensity (based on the standard evidence-based intervention, ≤50% contact time of the full intervention and delivered by a qualified mental health professional).
The BPI approach has been naturally evolving within clinical services in order to meet the high demand, therefore it is crucial to establish an evidence base for the effectiveness (e.g. Wright et al., Reference Wright, Travers-Hill, Gracey, Troup, Parkin, Casey and Kim2020), and develop relevant guidance for services to follow. BPIs are most commonly found in primary care services (e.g. Wakefield et al., Reference Wakefield, Kellett, Simmonds-Buckley, Stockton, Bradbury and Delgadillo2020), some school settings (e.g. Michelson et al., Reference Michelson, Malik, Krishna, Sharma, Mathur, Bhat, Parikh, Roy, Joshi, Sahu, Chilhate, Boustani, Cuijpers, Chorpita, Fairburn and Patel2020) or tailored to specific populations such as refugees (e.g. Graaff et al., Reference Graaff, Cuijpers, Acarturk, Bryant, Burchert, Fuhr, Huizink, Jong, Kieft, Knaevelsrud, McDaid, Morina, Park, Uppendahl, Ventevogel, Whitney, Wiedemann, Woodward and Sijbrandij2020). However, recent studies have shown that BPIs can be effective in reducing symptomatology in secondary care services (e.g. Wright et al., Reference Wright, Travers-Hill, Gracey, Troup, Parkin, Casey and Kim2020), in reducing suicide risk in emergency departments (see synthesis by McCabe et al., Reference McCabe, Garside, Backhouse and Xanthopoulou2018), and for the treatment of eating disorders in non-underweight adult patients (Waller et al., Reference Waller, Tatham, Turner, Mountford, Bennetts, Bramwell, Dodd and Ingram2018). During the global pandemic of COVID-19, BPIs were also delivered to health care staff (Morina, Reference Morina2020) and an ultra-BPI (15–20 minute sessions) designed to be delivered to front-line nurses and the public (Ping et al., Reference Ping, Shoesmith, James, Nor Hadi, Yau and Lin2020).
BPIs are most frequently targeted at common mental health problems, notably anxiety and depression. The NICE guidelines for both anxiety (NICE, 2011) and depression (NICE, 2018) recommend CBT. CBT-based BPIs typically focus on behavioural change, for example behavioural activation for depression and graded exposure for anxiety.
Current research shows promising results for CBT-based BPIs. For example, the COBRA trial (Richards et al., Reference Richards, Ekers, McMillan, Taylor, Byford, Warren and O’Mahen2016) indicated that behavioural activation delivered by junior mental health workers was no less effective than CBT delivered by psychological therapists, where both interventions were offered for 8–20 sessions. A meta-analysis (Cape et al., Reference Cape, Whittington, Buszewicz, Wallace and Underwood2010) also found large effect sizes for brief CBT for anxiety (d = –1.06), comparable to the effect sizes for longer-term treatment. Effect sizes for depression (d = –0.32) and mixed anxiety and depression (d = –0.21) were much smaller, although still showed an improvement compared with treatment as usual.
Research also indicates that relatively brief training (15 hours) can significantly improve competence and confidence in non-psychologists delivering brief CBT interventions (Armstrong et al., Reference Armstrong, Blashki, Lynette, Gunn, Moulding, Bland and Naccarella2009). These findings make CBT-based BPIs an appealing option for improving access to psychological treatment in a cost-effective manner. However, this research has mostly been conducted in primary care settings, usually excluding clients with more complex mental health problems (e.g. bipolar disorder, psychosis) or co-morbidities. Despite this, initial research investigating CBT-based BPIs for depression and/or anxious avoidance in individuals with psychosis has found improvements in both depressive symptoms and negative symptoms of psychosis (Turkington et al., Reference Turkington, Kingdon, Rathod, Hammond, Pelton and Mehta2006; Waller et al., Reference Waller, Garety, Jolley, Fornells-Ambrojo, Kuipers, Onwumere and Craig2013), suggesting the potential for BPIs in more complex client groups.
This paper aims to evaluate BPIs for anxiety and depression delivered in a secondary care adult mental health team, to clients with a range of moderate to severe mental health difficulties (including both anxiety and depression as the primary difficulty, and secondary to more complex mental health problems). Specifically, the evaluation will focus on two BPIs entitled ‘anxiety management’ and ‘behavioural activation’. These two BPIs included components of CBT, were delivered by paraprofessionals (supervised by clinical psychologists) and were brief in nature (six to eight 1-hour sessions). These BPIs do not fit neatly into the proposed definitions of brief CBT by Shafran et al. (Reference Shafran, Myles-Hooton, Bennett and Öst2021); however, the BPIs align more closely with their definition of ‘low intensity CBT’, but with duration and length of sessions more flexible to reflect the complexity of the patient population. As a service evaluation, this project provides a more realistic representation of both the client group seen by community mental health teams and a possible approach to service delivery.
The primary aim of this study is to evaluate whether anxiety and depression BPIs are effective in reducing their target symptoms, as well as improving wellbeing, functioning, and co-morbid symptoms of depression (anxiety BPI) or anxiety (depression BPI). The secondary aim is to evaluate whether there was a difference in demographics or baseline scores between those who do and do not complete treatment, to provide suggestions for improving practice.
Method
Design
The study reports on the clients offered anxiety or depression BPIs over a 24-month period (March 2017 to March 2019) in two secondary care adult mental health community teams (hereafter referred to as ‘the service’). A within-group design was used to compare outcome measures pre- and post-engaging in a BPI, with between-group comparisons to explore (non-)completion.
The study used anonymised outcome data collected as part of routine clinical practice, and as such the NHS Trust’s Research and Development Department considered this to be a service evaluation project, and no additional NHS ethical approval was required. As an educational project, additional ethical approval was sought and granted by the University of East Anglia Faculty of Medicine and Health Sciences Research Ethics Commitee.
Service setting
The service consisted of two adult community mental health teams covering one English county. The service included pathways for affective disorders and psychosis, with BPIs offered across both of these pathways. Service inclusion criteria was guided in part by the mental health care clustering system (NHS England, 2016/17), a system designed to broadly categorise an individual’s mental health presentation based on severity and level of service input likely to be needed. Diagnoses were based on ICD10 criteria (World Health Organization, 2016). For the affective pathway, service criteria included a primary diagnosis of major depressive disorder, bipolar disorder without current psychosis, anxiety disorder, obsessive compulsive disorder (OCD), or post-traumatic stress disorder (PTSD) at the level of severity described in care clusters 4 (severe non-psychotic mental health problems) to 7 (enduring non-psychotic disorders with high disability), or 15 (severe psychotic depression). For the psychosis pathway, inclusion criteria included a primary diagnosis of: schizophrenia; schizoaffective disorder; psychosis not otherwise specified (NOS); dual diagnosis/psychotic illness; bipolar disorder with psychosis; and covering clusters 10–14, 16 and 17. Within the locality, individuals with needs falling within care clusters 1 (common mental health problems, low severity) to 3 (non-psychotic mental health problems, moderate severity) were typically seen by the local IAPT service.
Procedure
BPI overview
The service developed three BPIs: anxiety management, behavioural activation (for depressive symptoms) and distress tolerance. The outcomes for the distress tolerance BPI have been reported elsewhere (Wright et al., Reference Wright, Travers-Hill, Gracey, Troup, Parkin, Casey and Kim2020). The anxiety and depression BPIs were bespoke to reflect the client group, but were informed by previous research and low intensity guided self-help manuals including: Richards et al. (Reference Richards, Ekers, McMillan, Taylor, Byford, Warren and O’Mahen2016), Farrand et al. (Reference Farrand, Taylor, Greaves and Pentecost2013), Lovell and Richards (Reference Lovell and Richards2012), and Richards and Whyte (Reference Richards and Whyte2011). Table 1 outlines the contents of both BPIs.
Table 1. Summary of BPI content

The service offered a half-day training session introducing BPIs, followed by an additional half-day training for each BPI. The training was delivered by clinical psychologists and trainee clinical psychologists within the service and was open to all clinical staff, including both those with a core profession (community psychiatric nurses, occupational therapists, social workers) and without (support workers, peer support workers, and assistant psychologists). Training materials and BPI resources were made available following this training, and around 6 months into the project these were consolidated into a manual for each BPI. This allowed staff feedback from trialling the BPIs to be incorporated into the design of the manuals, to improve ease of use. In addition to this, staff who would be delivering BPIs were offered shadowing opportunities with either psychologists using the interventions (although these data are not reported in the present study), or a member of staff who already had significant experience delivering BPIs. Later in the implementation of this model of working, additional ‘top-up’ training sessions were provided, which were less didactic and more focused on reflecting on the implementation of BPIs with different client groups.
Possible referrals for BPIs were made internally and discussed at weekly psychology meetings for suitability. Exclusion criteria included currently engaging in psychological therapy, presenting with high levels of risk requiring crisis management, and current drug or alcohol misuse (following current Public Health England guidelines). All staff delivering BPIs were offered fortnightly group supervision with a clinical psychologist. Supervision was held separately for staff working on the affective disorder and psychosis pathways.
The BPIs were designed to be contracted for six to eight sessions, but there was flexibility for this to be extended if deemed appropriate following discussion with BPI supervisors.
Anxiety BPI
The anxiety management BPI focused on psycho-education, relaxation techniques, graded exposure, and relapse prevention. There were additional optional modules in the anxiety BPI manual for worry management, problem solving, and sleep hygiene for use when relevant to a particular client. The decision to use the additional modules was made collaboratively with the client, and through supervision discussions with psychologists in the team.
Depression BPI
The depression BPI was focused on behavioural activation. The manual was developed drawing on components of the interventions used in the COBRA (Richards et al., Reference Richards, Ekers, McMillan, Taylor, Byford, Warren and O’Mahen2016) and CADET (Richards et al., Reference Richards, Hill, Gask, Lovell, Chew-Graham, Bower, Cape, Pilling, Araya, Kessler, Bland, Green, Gilbody, Lewis, Manning, Hughes-Morley and Barkham2013) trials, but also the wider literature and clinical experience of psychologists within the team, with the view to improving engagement and suitability for the client group. The main content of the intervention was most similar to Farrand et al.’s (Reference Farrand, Taylor, Greaves and Pentecost2013) ‘Get Active Feel Good!’ guide. The manual included psycho-education, behavioural activation, overcoming obstacles, attention training, and relapse prevention (see Table 1 for full content summary).
Measures
Four routine service outcome measures are completed at the start and end of a BPI (outlined below).
Generalized Anxiety Disorder-7 (GAD-7; Spitzer et al., Reference Spitzer, Kroenke, Williams and Löwe2006)
The GAD-7 is a 7-item measure of anxiety symptoms, scored on a 4-point Likert scale with total scores ranging from 0 to 21 (a higher score indicating greater symptomology). Within a primary care population, the GAD-7 has been found to have good internal consistency (Cronbach’s alpha = .92) and test–retest reliability (0.83; Spitzer et al., Reference Spitzer, Kroenke, Williams and Löwe2006). The GAD-7 also correlated well with diagnostic interviews conducted by mental health professionals (0.83), and with the Beck Anxiety Inventory (0.72), indicating good convergent validity. The GAD-7 was the primary outcome measure for the anxiety BPI.
Patient Health Questionnaire-9 (PHQ-9; Kroenke et al., Reference Kroenke, Spitzer and Williams2001)
The PHQ-9 is a 9-item measure of depressive symptoms, scored on a 4-point Likert scale with total scores ranging from 0 to 27 (a higher score indicating greater symptomology). Within a primary care population, the PHQ-9 has been found to have good internal reliability (Cronbach’s alpha = .89; Kroenke et al., Reference Kroenke, Spitzer and Williams2001), responsiveness to change, and convergent validity with the Hospital Anxiety and Depression Scale’s depression subscale (0.68; Cameron et al., Reference Cameron, Crawford, Lawton and Reid2008). The PHQ-9 was the primary outcome measure for the depression BPI.
Short Warwick-Edinburgh Mental Wellbeing Scale (SWEMWBS; Stewart-Brown et al., Reference Stewart-Brown, Tennant, Tennant, Platt, Parkinson and Weich2009)
The SWEMWBS is a 7-item measure of general mental wellbeing, scored on a 5-point Likert scale with total scores ranging from 7 to 35 (a higher score indicating better wellbeing). Within a population of out-patients experiencing anxiety, depression and/or schizophrenia, the SWEMWBS has shown good internal reliability (Cronbach’s alpha = .90) and convergent validity with the Satisfaction with Life Scale and a previously validated measure of positive mental health (Vaingankar et al., Reference Vaingankar, Abdin, Chong, Sambasivam, Seow, Jeyagurunathan and Subramaniam2017).
Work and Social Adjustment Scale (WSAS; Mundt et al., Reference Mundt, Marks, Shear and Greist2002)
The WSAS is a 5-item measure of functioning in different areas of daily life. Each item is scored from 0 to 8, with the total score ranging from 0 to 40 (a higher score indicating greater impairment). The WSAS was found to have good internal reliability in individuals with OCD and depression (Cronbach’s alpha between .79 and .94), and test–retest reliability (0.73). Convergent validity was also found with the Hamilton Rating Scale for Depression in the depression sample, and the Yale-Brown Obsessive Compulsive Scale in the OCD sample (Mundt et al., Reference Mundt, Marks, Shear and Greist2002).
Participants
Participants were 136 adults (aged 17–64 years) accessing a secondary care mental health service, who were accepted for anxiety or depression BPIs over a 2-year period (March 2017 to March 2019). Figure 1 shows the number of people that were accepted for and completed BPIs over this time period.
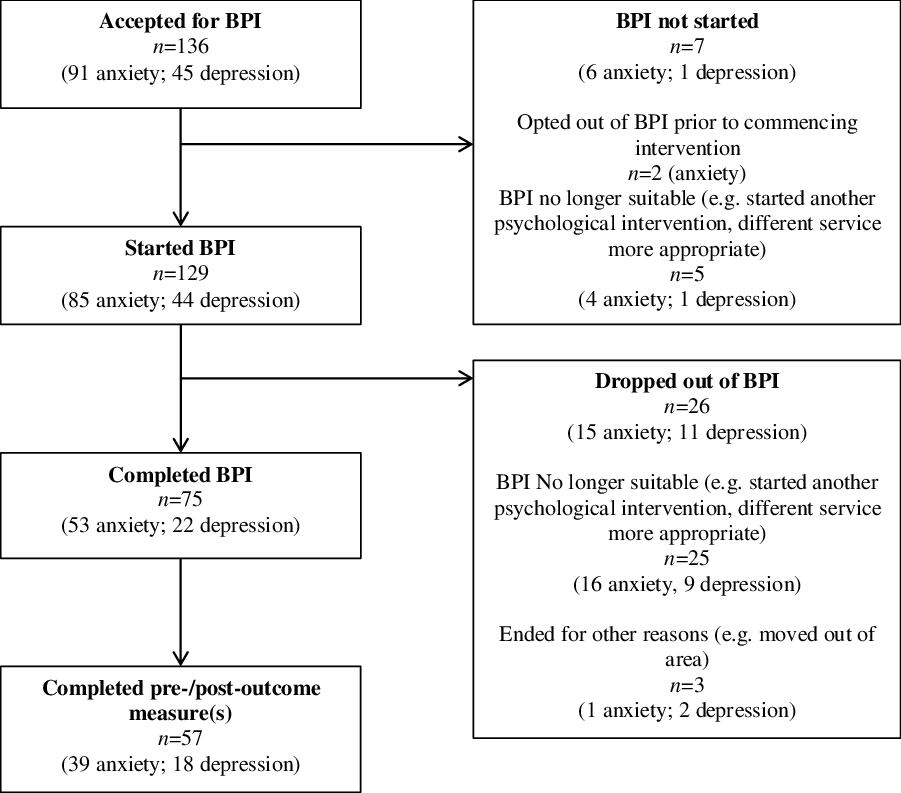
Figure 1. Number of participants accepted for BPI and attrition.
The majority of BPIs were conducted by staff without a core profession, primarily support workers (85.2% anxiety BPI; 86.7% depression BPI) and peer support workers (6.8% anxiety BPI; 6.7% depression BPI), but also assistant psychologists (5.7% anxiety BPI; 4.4% depression BPI), and social work students (0% anxiety BPI, 2.2% depression BPI). However, two anxiety management cases (2.2%) were completed by staff with a core profession (occupational therapist and community psychiatric nurse).
Participants presented with a range of moderate to severe anxiety and/or depression (71.1%) and more severe and enduring mental health problems (e.g. bipolar disorder, psychosis; 28.9%), typical of the secondary care population.
Table 2 shows demographic information for all participants accepted for BPIs, and those with at least one outcome measure completed at both the start and end of the BPI.
Table 2. Characteristics of all participants, and those with completed outcome measure(s) for anxiety and depression BPIs

Primary diagnosis was recorded on the basis of ICD-10 (World Health Organization, 2016) criteria, with the exception of ‘Mixed anxiety and depression’ which refers both to the ICD-10 criteria and also any patient who met criteria for both an anxiety disorder and depressive disorder without a clear primary difficulty.
Data analysis
Primary analysis
Data analysis was conducted using IBM SPSS Statistics v25. Initially, group level change was assessed using t-tests, with the effect size Cohen’s d also reported. Power analysis indicated that a sample size of 15 would be needed to detect a large effect and 34 to detect a large effect, at power level 0.8 and alpha .05.
Individual change was subsequently assessed through calculation of reliable change and clinically significant change (CSC), to provide a more clinically meaningful evaluation of the effectiveness of BPIs. Reliable change assesses whether an individual’s score has changed by more than would be expected from natural retest variability. CSC indicates improvement to the extent that the measured problem would no longer be considered clinically significant.
For the GAD-7 and PHQ-9, individual change was assessed by the criteria used by IAPT services (Clark and Oates, Reference Clark and Oates2014). While this client group would typically have milder difficulties than those included in the current report, the BPIs were similar to interventions used in IAPT settings, and using these standards aids comparison with the large amount of data publicly available from IAPT services.
For the SWEMWBS and WSAS, the reliable change index (RCI) and CSC (criterion ‘c’) were manually calculated using equations outlined by Jacobson and Truax (Reference Jacobson and Truax1991). Where more than one set of norms were available, selection was on the basis of being larger samples, and closer matched to the population included in the current study. For the SWEMWBS, clinical norms were taken from Vaingankar et al.’s (Reference Vaingankar, Abdin, Chong, Sambasivam, Seow, Jeyagurunathan and Subramaniam2017) study of adults experiencing anxiety, depression, and/or schizophrenia under the care of an out-patient service in Singapore. Healthy norms were taken for Bartram et al.’s (Reference Bartram, Sinclair and Baldwin2013) study of UK veterinary professionals, and reliability was from Fat et al.’s (Reference Fat, Scholes, Boniface, Mindell and Stewart-Brown2017) evaluation of the SWEMWBS. Using these figures, the RCI was calculated as 5.88 and CSC as 22.42.
For the WSAS, clinical norms were taken from Zahra et al. (Reference Zahra, Qureshi, Henley, Taylor, Quinn, Pooler and Byng2014), including data from IAPT services within 14 healthcare trusts. Healthy norms were taken from Dell’Osso et al. (Reference Dell’Osso, Carmassi, Corsi, Pergentini, Socci, Maremmani and Perugi2011), which included a sample from an Italian population who had experienced the loss of a friend or family member at least 6 months previously, but were not showing signs of complicated grief, and had no current or lifetime DSM-IV Axis I disorders. Test–retest reliability was as reported in the development of the measure (Mundt et al., Reference Mundt, Marks, Shear and Greist2002). Using these figures, the RCI was calculated as 13.21, and the CSC as 9.25.
Secondary analysis
For the secondary analyses, Mann–Whitney U-test and Fisher’s exact test were used to compare demographic information and start of treatment scores between those who did and did not complete treatment. To improve power and reduce potential issues associated with multiple testing, data for anxiety and depression BPIs were pooled for these analyses. Due to the small sample size, those who dropped out of treatment were pooled with those who did not complete the intervention for other reasons. However, on the basis of assessing descriptive statistics, no additional patterns were apparent when the three different groups were compared.
Results
Primary analysis: change on GAD-7, PHQ-9, SWEMWBS and WSAS
Group level change
Table 3 shows mean scores on the four outcome measures pre- and post-BPI; all mean scores for both anxiety and depression BPIs moved in the direction of improvement following BPIs.
Table 3. Mean pre- and post-treatment scores with standard deviations
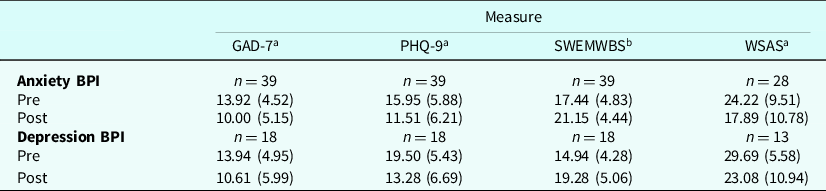
a Decreased score indicates positive change.
b Increased score indicates positive change.
GAD-7, Generalized Anxiety Disorder-7; PHQ-9, Patient Health Questionnaire-9; SWEMWBS, Short Warwick-Edinburgh Mental Wellbeing Scale; WSAS, Work and Social Adjustment Scale.
For the anxiety BPI, the primary outcome measure was the GAD-7, for which a significant decrease in scores and medium to large effect size was found (t 38 = 4.95, p<.001, d = –0.79). This indicates a reduction in anxiety symptoms, as per the focus of the intervention. A significant decrease was also found for the PHQ-9 (t 38 = 5.71, p<.001), which represents a large effect size (d = –0.91), and indicates a significant improvement in depressive symptoms. Significant differences were also found for the SWEMWBS (t 38 = –4.52, p<.001, d = 0.72) and WSAS (t 27 = 4.02, p<.001, d = –0.77).
For the depression BPI, the primary outcome measure was the PHQ-9, for which a significant decrease and large effect size was found (t 17 = 4.16, p = .001, d = –0.98). This indicates a significant improvement in depressive symptoms, as per the focus of the intervention. Significant differences and medium to large effect sizes were also found for both the GAD-7 (t 17 = 2.62, p = .018, d = –0.62) and SWEMWBS (t 17 = –5.28, p<.001, d = 1.24), indicating significant improvements in anxiety and wellbeing. No significant difference was found for the WSAS (t 12 = 2.02, p = .066); however, a medium effect size was calculated (d = .56), indicating a potential moderate improvement in functioning.
Individual level change
For the anxiety BPI, 52.6% of participants showed a reliable improvement on the GAD-7, with one participant (2.6%) showing a reliable deterioration; 21.1% of participants also reached CSC on the GAD-7, with a further 7.9% below clinical cut-off at the start and end of treatment. On the PHQ-9, 36.8% of participants showed reliable improvement, with one participant (2.6%) showing a reliable deterioration, with 23.1% reaching CSC (10.3% below clinical cut-off at the start and end of treatment). However, only four participants (10.5%) showed CSC on both the GAD-7 and PHQ-9, and would therefore meet the IAPT criteria for overall recovery (Clark and Oates, Reference Clark and Oates2014). On the SWEMWBS, 39.5% showed reliable improvement, and 28.9% reached CSC (13.2% below CSC at start and end of treatment). On the WSAS, 23.1% showed reliable improvement, with three participants (10.7%) reaching CSC (14.3% below CSC at the start and end of treatment).
For the depression BPI, 50.0% showed a reliable improvement on the PHQ-9, with 21.1% of participants also showing a CSC (5.3% below clinical cut-off at the start and end of treatment). On the GAD-7, 55.6% of participants showed a reliable improvement, with one participant (5.6%) showing a reliable deterioration; 26.3% reached CSC on the GAD-7 (5.3% below CSC at the start and end of treatment), and 21.1% also showed overall recovery (that is below CSC threshold on both PHQ-9 and GAD-7 at the end of treatment). On the SWEMWBS, 33.3% showed reliable improvement, and 11.1% reached CSC (11.1% below CSC at the start and end of treatment). On the WSAS, 30.8% showed reliable improvement, with one participant (7.1%) reaching CSC.
Clark and Oates (Reference Clark and Oates2014) provide additional criteria for overall reliable improvement, defined as a reliable improvement on the PHQ-9 and/or GAD-7 with no reliable deterioration on any other measures. On the basis of these criteria, 57.9% who received the anxiety BPI and 66.7% who received the depression BPI showed overall reliable improvement. Two participants (5.3%) who engaged in the anxiety BPI showed an overall reliable deterioration, with no overall reliable deteriorations observed for the depression BPI.
Secondary analysis: comparisons of completers and non-completers
There were no significant differences (p>.05) between those who did and did not complete treatment for the following: age, gender, primary diagnosis (anxiety/depression compared with severe and enduring mental health difficulties), BPI type (anxiety/depression), whether the primary diagnosis matched the focus of BPI, and start of treatment scores on the PHQ-9, GAD-7, SWEMWBS and WSAS.
Discussion
There is increasing interest in the use of BPIs within mental health services; however, the majority of research has been conducted in primary care settings, typically with individuals experiencing mild to moderate mental health difficulties. This study evaluated BPIs for anxiety and depression within a secondary care adult mental health service including clients with a range of moderate to severe mental health problems. Both the anxiety and depression BPIs were found to lead to significant improvements in the target symptoms with medium to large effect sizes (anxiety d = –0.79; depression d = –0.98). Improvements following both BPIs were also seen in wellbeing, functioning, and co-morbid anxiety or depressive symptoms with medium and large effect sizes. At an individual level, reliable improvement was observed in 57.9% of participants who completed anxiety BPI and 66.7% of those that completed depression BPI, clinically significant change in anxiety (anxiety BPI) and depression (depression BPI) symptoms was also observed in 21.1% of participants.
The effect sizes found in the present study are broadly similar to the pooled effect sizes reported in Wakefield et al.’s (Reference Wakefield, Kellett, Simmonds-Buckley, Stockton, Bradbury and Delgadillo2020) meta-analysis of practice-based IAPT studies. Within this meta-analysis, pooled effect sizes for those who completed interventions varied from 0.44 to 1.06 for the PHQ-9, GAD-7 and WSAS. Comparatively, the present study found somewhat larger effects for functioning (WSAS), similar results for depression (PHQ-9), and somewhat smaller effect sizes for anxiety (GAD-7). These are encouraging results, particularly given that the current study included a client group typically experiencing more severe difficulties, and the training for staff was generally much briefer (with most IAPT studies including interventions conducted by psychological wellbeing practitioners as opposed to paraprofessionals used in this study). However, it is important to note that both the present study and Wakefield et al.’s meta-analysis found high rates of non-completion. It is well documented that studies including outcomes only for those that complete an intervention generally find superior effects (for example Clark et al., Reference Clark, Layard, Smithies, Richards, Suckling and Wright2009; McCoy, Reference McCoy2017). This was also reflected in Wakefield et al.’s meta-analysis where smaller effect sizes were found for intention to treat studies. This highlights an important limitation of the present study.
As a service evaluation, the current study was not able to make changes to routine care, which introduces several limitations. Firstly, participants who dropped out of treatment were not asked to complete outcome measures, and unlike typical IAPT service protocol, measures were completed only at the start and end of intervention and not on a session-to-session basis. Exploration of demographic and start of intervention measures did not show significant differences between those who did and did not complete BPIs, suggesting that those who completed the intervention were broadly representative of the sample population. However, it will be important for future research to focus on the acceptability of the BPIs, and the effectiveness of BPIs when using an intention to treat approach. Furthermore, as the present study was unable to include a control group, it was unable to consider how BPIs compare with treatment as usual in terms of clinical- or cost-effectiveness. Additionally, the primary outcome measure for the anxiety used within the service was the GAD-7 (Spitzer et al., Reference Spitzer, Kroenke, Williams and Löwe2006), a measure of generalised anxiety disorder symptoms. In contrast, the main active intervention in the anxiety BPI manual was graded exposure, more typically used for those experiencing panic symptoms. It may be that this contributed to smaller effect size found for anxiety BPI compared with depression BPI, a finding that is contrary to previous BPI research (e.g. Cape et al., Reference Cape, Whittington, Buszewicz, Wallace and Underwood2010) and the wider CBT literature (e.g. Cuijpers et al., Reference Cuijpers, Cristea, Karyotaki, Reijnders and Huibers2016), where effect sizes have typically been found to be greater for anxiety interventions.
A further limitation of the present study is that treatment fidelity was not assessed, and therefore it was not possible to comment on how closely the interventions received by participants matched the content of the BPI manuals. This may be particularly pertinent for anxiety management due to a wider range of techniques being included in the manual, which may mean there was greater variability in the interventions received by participants. Finally, the demographic information available for the present study was limited, and did not include information such as ethnicity, sexual orientation and socioeconomic status. These may be important factors to consider in future studies of acceptability and effectiveness of BPIs, both in ensuring the representativeness of samples and to be able to assess any potential impact of social inequalities on treatment outcomes.
Despite the limitations of the current study, to the best of the authors’ knowledge this is the first evaluation of BPIs within a general adult secondary care mental health service. As a service evaluation, the study offers good ecological validity as participants were representative of the client group seen by community mental health teams, and the model of delivery was feasible within the constraints of an NHS service. In particular, the present study used a model where training was offered by and to staff already employed within the service, and was relatively brief in duration. This is positive for both the speed of potential roll-out and cost-effectiveness as a model to improve access to low intensity psychological interventions in secondary care. The positive initial findings highlight the need for much further research in this field, to address the limitations of the current evaluation and build on the evidence base to understand if wider roll-out of this novel model of working would be warranted.
Firstly, it would be beneficial for future research to gain participant feedback to help understand perception of BPIs and the reasons for drop-out, with a view to understanding and improving the acceptability of the interventions. It would also be beneficial to consider both staff and client perception of outcome measures, to understand if any changes could be made to improve completion and therefore the representativeness of results. Secondly, it may be beneficial to evaluate a small number of cases using a single case series approach, including session-by-session monitoring and an end of treatment interview to understand the participant’s perception of change. This may aid the refinement of BPIs by understanding whether observed improvements appear to be associated with specific treatment components, which would aid understanding of the importance of fidelity to different treatment components. The results of this work could subsequently contribute to the development of a protocol for a future randomized controlled trial to assess the effectiveness of BPIs in a secondary care setting on a larger scale, and with greater control than was possible within the scope of a service evaluation. It will be important for any future trials in this area to consider both the immediate outcomes of BPIs, but also whether they are effective in reducing the duration and intensity of future interventions required for clients to reach recovery, as well as whether the improvements observed during BPIs are maintained. This will be important for evaluating both the clinical- and cost-effectiveness of BPIs in this client group.
In summary, the initial results for BPIs in this client group are positive. However, there is scope for much further research and evaluation before drawing firm conclusions. If found to be effective, BPIs could offer a cost-effective way to improve access to psychological therapies within secondary care. While BPIs may not be sufficient to lead to recovery for most individuals in this client group, BPIs may offer a quicker way to see significant improvements in wellbeing and functioning, which are important for an individual’s quality of life. If BPIs were found to reduce the length and intensity of subsequent psychological intervention needed, they could also help alleviate some of the pressure on waitlists, allowing those with the greatest need to access more intensive psychological support more quickly. The introduction of BPIs also leads to a new role for psychologists and/or CBT therapists working in these settings to train and supervise staff in using BPIs, hopefully leading to a more integrated way of working and embedding psychologically informed care within mental health services.
Overall, given the promising findings of this initial evaluation, and the potential benefits of BPIs, further investigation of BPIs within secondary care is clearly warranted.
Key practice points
-
(1) CBT-based brief psychological interventions for anxiety and depression have been found to be helpful for mild to moderate anxiety and depression.
-
(2) The present study proposes a new model for introducing BPIs in a secondary care setting with patients with moderate to severe mental health difficulties. This included adapting interventions and using a model of BPIs being delivered by staff without core therapeutic training under the supervision of clinical psychologists.
-
(3) The current study provides preliminary evidence that brief psychological interventions for anxiety and depression may be helpful within secondary mental health care for adults experiencing more severe difficulties.
-
(4) Given the potential benefits of brief psychological interventions for improving access to psychological treatment and for cost-effectiveness, larger scale evaluations in secondary mental health care are warranted.
Data availability statement
Data and further information of the role out of this model of service delivery is available from corresponding author in response to reasonable requests.
Acknowledgements
The authors would like to thank the service managers Kim Masson and Maggie Page for their support of this project, and the service users and staff who participated in this project.
Author contributions
Conceptualization: K.R., E.T.-H., Y.K.; Data curation: J.T., S. Casey, K.P.; Formal analysis: K.R.; Investigation: E.T.-H., J.T., S. Casey, K.P., Y.K.; Methodology: K.R., E.T.-H., J.T., Y.K.; Project administration: E.T.-H., J.T., S. Casey, K.P., Y.K.; Resources: E.T.-H., J.T.; Supervision: E.T.-H., S. Coker, Y.K.; Writing-original draft: K.R., E.T.-H., S. Coker, S. Casey, K.P., Y.K.; Writing-review & editing: K.R., E.T.-H., Y.K.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interest
None.
Ethics statements
Authors have abided by the Ethical Principles of Psychologists and Code of Conduct as set out by the BABCP and BPS. Approval for this project as a service evaluation was granted by Cambridgeshire and Peterborough NHS Foundation Trust’s Research and Development Department, as an educational project additional ethical approval was granted by the University of East Anglia Faculty of Medicine and Health Sciences Research Ethics Commitee.







Comments
No Comments have been published for this article.