The study of resilience has increased in recent times. One of the main difficulties in conducting research on resilience is that there are discrepancies in the way resilience is defined and conceptualized (Fletcher & Sarkar, Reference Fletcher and Sarkar2013).
Hu et al., (2015) showed that resilience can be understood as a trait, outcome, and process. The trait orientation (or trait resilience) suggests that resilience is a personal trait that helps individuals to cope with adversity and achieve good adjustment and development, namely, resilience as a personality trait (Ong et al., Reference Ong, Bergeman, Bisconti and Wallace2006). The outcome-oriented approach regards resilience as a function or behavioral outcome that can help individuals to overcome and recover from adversity. Finally, the process-oriented approach views resilience as a dynamic process that involves positive adaptation within the context of significant adversity, which implies that the person is exposed to a significant threat or severe adversity and displays positive adaptation despite the great adversities (Luthar et al., Reference Luthar, Cicchetti and Becker2000).
Focusing on resilience as a process, some authors, such as Windle (Reference Windle2011), have defined it as the process of negotiating, managing, and adapting to significant sources of stress or trauma. Assets and resources within individuals, their lives, and the environment facilitate this capacity for adaptation and ‘bouncing back’ in the face of adversity.
Taking this model into account, resilience could be the key to explaining risk resistance throughout life and the way people "recover" from and deal with the various challenges arising from childhood to more advanced ages, such as poor health (Windle et al., Reference Windle2011). It is also important to note that the role of resilience changes as adversity changes (Hu et al., Reference Hu, Zhang and Wang2015). Conceptual discrepancies hinder the evaluation and comparison of research findings and make it difficult to operationalize the construct for measurement purposes (Davydov et al., Reference Davydov, Stewart, Ritchie and Chaudieu2010). Resilience has been evaluated through various self-report measures. Specifically, in the present study, we focus on the development of short versions of these scales, given the need for scales that can be completed quickly and easily by respondents from certain populations, and/or research designs where time to complete the scales is limited.
The Brief Resilient Coping Scale
Sinclair and Wallston (Reference Sinclair and Wallston2004) developed the Brief Resilient Coping Scale (BRCS), based on an early 9-item version. The final version of the scale contains four items that measure a single dimension of resilient coping, which involves a form of confronting adversity that encourages the use of cognitive and behavioral strategies (Sinclair & Wallston, Reference Sinclair and Wallston2004). This scale describes an effective, active problem-solving, coping pattern that reflects resilient coping patterns, specifically the attributes described by Polk (Reference Polk1997) as situational patterns associated with resilience. Sinclair and Wallston (Reference Sinclair and Wallston2004) obtained a Cronbach’s alpha of .69 for the BRCS in a sample of 230 women and men diagnosed with rheumatoid arthritis. Likewise, the BRCS showed positive correlations with several measures of personal coping resources, pain coping behaviors, and psychological well-being (Sinclair & Wallston, Reference Sinclair and Wallston2004).
Several studies have analyzed the factorial structure and internal consistency of the BRCS in Spanish population, obtaining good psychometric results. In a sample of Spanish elderly people, Tomás et al., (2012) obtained a good fit for the BRCS and high internal consistency: χ2(2) = 5.20, p = .07, CFI = .95, GFI = .96, SRMR = .05, RMSEA = .19, and Conbach´s alpha = .83, confirming the unidimensionality of the scale. These data were even better than those obtained by Sinclair and Wallston (Reference Sinclair and Wallston2004). Tomás et al. (2012) obtained positive correlations between the BRCS and Ryff’s Scales of Psychological Well-Being and several measures of coping resources (problem-solving coping, negative self-focused coping, positive reappraisal, avoidance coping, social support seeking, and religious coping), as well as a negative correlation with overt emotional expression.
Limonero et al., (Reference Limonero, Tomás-Sábado, Gómez-Romero, Maté-Méndez, Sinclair, Wallston and Gómez-Benito2014) obtained an adequate fit for the BRCS, χ2(2) = 3.04, p =.21, CFI = .99, GFI = .99, NNFI = .98, SRMR = .01, and RMSEA = .04; 90% CI = [.00, .11], low internal consistency, Conbach´s alpha = .67, and a composite reliability index of .70. The BRCS showed negative, significant correlations with measures of depression, anxiety, and negative affect, and positive, significant correlations with personal perceived competence, optimism, life satisfaction, positive affect, problem solving, social support, cognitive restructuring, and problem avoidance.
Finally, López-Pina et al. (Reference López-Pina, Meseguer-Henarejos, Gascón-Cánovas, Navarro-Villalba, Sinclair and Wallston2016), using Principal Components Analysis of residuals after fitting a Rasch model in a sample of 232 patients diagnosed with systemic lupus erythematosus, reported that the BRCS was essentially a unidimensional scale and correlated positively with perceived health status.
Resilience and Mental Health
Recently, mental health research has shifted the focus from deficit-focused models to models that emphasize the recovery capacity of the person with a mental illness (Priebe et al., Reference Priebe, Omer, Giacco and Slade2014). In this new paradigm, resilience is considered an area of growth and interest (Thomas et al., Reference Thomas, Jenkins, Burch, Nasir, Fisher, Giotaki, Gnani, Hertel, Marks, Mather, Millington-Sanders, Morris, Ruprah-Shah, Stange, Thomas, White and Wright2016). Some authors characterize resilience as a protection factor against mental illness (Jääskeläinen et al., Reference Jääskeläinen, Juola, Hirvonen, McGrath, Saha, Isohanni, Veijola and Miettunen2013). to the extent that several studies indicate that a high level of resilience can prevent the development of a disease or minimize its seriousness (Shrivastava & Desousa, Reference Shrivastava and Desousa2016). Moreover, resilience can help a person to more successfully face future adversities (Meesters, Reference Meesters2014).
The measurement of the recovery experience has become a priority in the clinical mental health field (Shanks et al., Reference Shanks, Williams, Leamy, Bird, Le Boutillier and Slade2013). The results of the recovery, from a subjective perspective, have mainly been evaluated using qualitative methodology (Andresen et al., Reference Andresen, Oades and Caputi2003). Mak et al., (Reference Mak, Chan and Yau2018) identify resilience as one of the five significant factors in measuring attitudes to recovery in people with severe mental illness. The BRCS could be a useful tool for the quantitative assessment of resilience and, therefore, of the recovery experience, in people with severe mental illness.
As far as we know, there are no studies that analyze the psychometric properties of the BRCS in Spanish people diagnosed with chronic, stable severe mental disorders.
The Current Study
The main purpose of the present study was threefold: First, to confirm the factorial structure of the BRCS original model in a Spanish sample of stable severe mental disorder patients; second, to estimate the internal consistency of this scale; and third, to analyze the concurrent validity of the BRCS through its correlations with the WHOQOL-BREF scales.
Method
Participants
Participants were 57 Spanish stable severe mental disorder patients (42 men, 73.7%, and 15 women, 26.3%) with ages ranging between 23 and 64 years, M = 46.25; SD = 7.52. Most of the participants had a diagnosis of schizophrenic spectrum disorders, n = 47, 82.5%, whereas only a few had a diagnosis of affective disorders, n = 10, 17.5%. Almost all the participants were single, n = 52, 91.2%. We considered people with a stable mental disorder to be those who had not presented significant clinical changes and had not required any change in their pharmacological treatment in the previous month.
Instruments
Brief Resilience Coping Scale (BRCS; Sinclair & Wallston, Reference Sinclair and Wallston2004). The BRCS is a 4-item instrument with a 5-point Likert type response scale (1 = Does not describe you at all; 5 = Describes you very well), which was designed to identify highly adaptive tendencies to cope with stress, including aspects such as optimism, perseverance, creativity, and positive growth in the face of adversity. The total score can range from 4 to 20, with higher scores denoting greater resilient coping. The four items on the BRCS are grouped into a single dimension. In the present study, the Spanish adaptation (Tomás et al., Reference Tomás, Meléndez, Sancho and Mayordomo2012) was used, which showed acceptable internal consistency, as can be seen in the Results section.
World Health Organization Quality of Life Assessment (WHOQOL-BREF; WHOQOL Group, 1998). The WHOQOL-BREF is a 26-item Likert-type scale grouped into four subscales related to quality of life.
1. Physical health (PhH) subscale includes the next facets: Activities of daily living; dependence on medicinal substances and medical aids; energy and fatigue; mobility, pain and discomfort; sleep and rest; and work capacity.
2. Psychological health (PsH) subscale comprises items related to facets as bodily image and appearance; negative feelings; positive feelings; self-esteem; spirituality/religion/personal beliefs; and thinking, learning, memory and concentration.
3. Social relations (SR) subscale encompasses the next facets: Personal relationships, social support and sexual activity.
4. Environment (E) subscale includes items related to: Financial resources; freedom, physical safety and security; health and social care: Accessibility and quality; home environment; opportunities for acquiring new information and skills; participation in and opportunities for recreation/leisure activities; and physical environment (pollution/noise/traffic/climate); and transport.
This self-administered scale provides a profile of one’s perceived quality of life. The higher the scores on each of the subscales, the greater the perceived quality of life. In the present study, the Spanish adaptation (Lucas-Carrasco, Reference Lucas-Carrasco2012) was used. The WHOQOL subscales showed a Cronbach’s alpha higher than .70, and the whole scale showed a Cronbach’s alpha of .90.
Procedure
Participants were recruited from a rehabilitation and social integration resource located in the city of Valencia (Spain). They filled out both scales under the supervision of the authors of this study, who briefly explained its nature and objectives and emphasized the sincerity of the answers in order to maximize the validity of the data.
All the participants collaborated voluntarily, did not receive any compensation for their collaboration, and were informed that all the data gathered would remain anonymous and confidential. The procedure met the ethical standards of the Helsinki Declaration of 1975, as revised in 2013. Incomplete protocols were rejected, and the data from the selected protocols were entered into an SPSS file.
Statistical Analyses
First, a Confirmatory Factor Analysis (CFA) was performed for the BRCS, using the EQS version 6.1 software. Because it was possible to assume multivariate normality, the maximum likelihood method was used. Fit indexes included were the following: Comparative Fit Index (CFI), Incremental Fit Index (IFI), and Joreskog-Sorbom’s Fit Index (GFI) (where values between .90 and .95 indicate reasonable model fit), and the Standardized Root Mean-Square Residual (SRMR) and Root Mean Square Error of Approximation (RMSEA) (where values lower than .05 are optimal, values between .05 and .08 suggest an acceptable fit, values between .08 and .10 suggest a mediocre fit, and values higher than .10 indicate an unacceptable fit) (Hair et al., Reference Hair, Anderson, Tatham and Black2006). The ratio between observable variables (4 items) and sample size (N = 57) exceeded what has been suggested by some authors (5–10 subjects per observable variable), suggesting the viability of CFA (e.g. Jackson, Reference Jackson2003; Kline, Reference Kline2005).
Then, descriptive statistics (means and standard deviations) and the internal consistency and concurrent validity of the BRCS were calculated. Because Cronbach’s alpha tends to underestimate reliability when there are few items and ordinal scales (as in the current study), the Composite Reliability (CR) (e.g. Brown, Reference Brown2015) (according to Hair et al., Reference Hair, Anderson, Tatham and Black2006, the CR should be >.70) and the average inter-item correlation (according to Clark and Watson, Reference Clark and Watson1995, it should be between .15 and .50) of the BRCS were calculated. To report the concurrent validity of the BRCS, the correlation with the WHOQOL-BREF was analyzed. All these analyses were performed using the SPSS version 15.0 software.
Results
Structural Validity of the BRCS
A CFA for the original BRCS (Sinclair & Wallston, Reference Sinclair and Wallston2004) was specified. Mardia’s normalized estimated coefficient was 1.23. The model showed an excellent fit: χ2(2) = 1.20, p = .549, CFI = 1.00, IFI = 1.02, GFI = .99, SRMR = .032, RMSEA = .000, 90% CI [.000, .226] (Figure 1). All parameters were significant at the .05 level.

Figure 1. Model for the BRCS Obtained in the Current Study
Means and Standard Deviations of the BRCS
The means and standard deviations of the BRCS were the following: Item 1, M = 3.54, SD = 1.17; Item 2, M = 3.33, SD = 1.19; Item 3, M = 3.79, SD = 1.13; Item 4, M = 3.35, SD = 1.26, and total BRCS, M = 3.50, SD = .85.
Internal Consistency of the BRCS
The BRCS showed a Cronbach’s alpha of .69, a composite reliability of .64, and an average inter-item correlation of .35. Table 1 shows the scores obtained for the BRCS items.
Table 1. Properties of BRCS
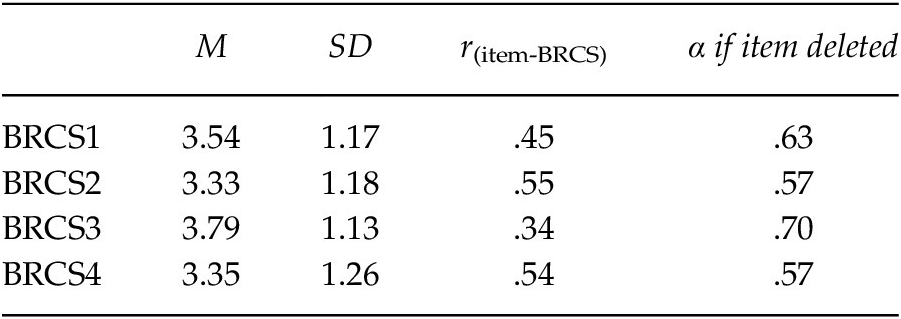
Note. N = 57.
Concurrent Validity of the BRCS
To report the concurrent validity of the BRCS, the correlation with the WHOQOL-BREF scales was calculated. The BRCS showed a positive, significant correlation, p < .01, with the WHOQOL-BREF scales in the expected direction, given what the scales are supposed to assess: r(PhH-R) = .42, r(PsH-R) = .40, r(SR-R) = .33, r(E-R) = .35.
Discussion
The purpose of the present study was to analyze the psychometric properties of the BRCS in a Spanish sample of stable severe mental disorder patients. We hypothesized (a) that the original structure of the BRCS would be confirmed, (b) that the BRCS would show good internal consistency and convergent validity, and (c) that the BRCS would show good concurrent validity based on its correlation with the WHOQOL-BREF scales. The results obtained in the present study confirm these hypotheses.
Factorial Structure of the BRCS
As in previous studies (Limonero et al., Reference Limonero, Tomás-Sábado, Gómez-Romero, Maté-Méndez, Sinclair, Wallston and Gómez-Benito2014; López-Pina et al., Reference López-Pina, Meseguer-Henarejos, Gascón-Cánovas, Navarro-Villalba, Sinclair and Wallston2016; Tomás et al., Reference Tomás, Meléndez, Sancho and Mayordomo2012) with a Spanish population, the BRCS showed an adequate fit as a unidimensional scale (Schumacker & Lomax, Reference Schumacker and Lomax2004). These results again support the situational pattern that gives rise to the resilience recognized by Polk (Reference Polk1997). This pattern shows the capacity of cognitive assessment, the ability to solve problems, and the ability to take action to deal with a situation. This pattern includes the possibility of making a realistic assessment of the ability to act and the expectations or consequences of that action, as well as an awareness of what can and cannot be done.
Internal Consistency and Convergent Validity of the BRCS
The Cronbach’s alpha obtained in the present study was equal to the one obtained by Sinclair and Wallston (Reference Sinclair and Wallston2004), lower than the one obtained by Tomás et al. (Reference Tomás, Meléndez, Sancho and Mayordomo2012), and higher than the one obtained by Limonero et al. (Reference Limonero, Tomás-Sábado, Gómez-Romero, Maté-Méndez, Sinclair, Wallston and Gómez-Benito2014).
Although the Cronbach’s alpha and composite reliability of the BRCS were slightly lower than the DeVellis (Reference DeVellis2003) and Hair et al. (Reference Hair, Anderson, Tatham and Black2006) criteria (α = .70 and CR > .70, respectively) for acceptable internal consistency, the average inter-item correlation supported the internal consistency of the scale (Clark & Watson, Reference Clark and Watson1995) and suggested that the items on the BRCS are well related to each other and might be suitable for measuring the same construct. These values are high for a scale composed by only 4 items, as is the case in this study, and the internal consistency would increase to .80 if the number of items were duplicated.
Validity of the BRCS
The positive significant correlations between the BRCS and WHOQOL-BREF scales, as expected, support the validity of the BRCS. As previous studies with very diverse health conditions showed, resilience is a strong predictor of quality of life. Robottom et al. (Reference Robottom, Gruber-Baldini, Anderson, Reich, Fishman, Weiner and Shulman2012), in a sample of people with Parkinson’s disease, reported correlations between resilience and Physical Health-related Quality of Life (r = .31) and between resilience and Mental Health-related Quality of Life (r = .29), both dimensions of the Short Form Health Survey (Ware et al., Reference Ware, Kosinski and Keller1998). Schumacher et al., (Reference Schumacher, Sauerland, Silling, Berdel and Stelljes2014), in a study with a sample of people suffering from hematological diseases, reported a high and significant correlation between resilience and quality of life (r = .59). López-Pina et al. (Reference López-Pina, Meseguer-Henarejos, Gascón-Cánovas, Navarro-Villalba, Sinclair and Wallston2016), with a sample of Spanish people diagnosed with Systemic Lupus Erythematosus, reported a significant correlation between resilience measured by the BRCS and perceived health status (quality of life).
Likewise, several studies with a Spanish population offered results suggesting that resilience is a strong predictor of well-being and coping (Tomás et al., Reference Tomás, Meléndez, Sancho and Mayordomo2012), positive affect, optimism, and life satisfaction, among other variables related to positive mental health (Limonero et al., Reference Limonero, Tomás-Sábado, Gómez-Romero, Maté-Méndez, Sinclair, Wallston and Gómez-Benito2014).
The recovery model in the field of mental illness attributes greater value to the continuous process of change in personal identity than to achieving results related to the disappearance of symptoms of the disease. According to Rosillo Herrero et al., (Reference Rosillo Herrero, Hernández Monsalve and Smith2013), this model emphasizes the construction of a life project despite suffering from a mental illness. Throughout this process, the individual assumes the proper management of the disease itself, in order to reduce the impact of persistent symptoms and disabilities and achieve socially valuable personal roles and goals beyond the role of the sick person. In other words, the person builds resilience, which is considered a component of the psychosocial adaptation associated with mental health.
As mentioned above, knowledge about the resilient coping process is of great interest to researchers, given its association with positive psychological results. Therefore, it is essential for clinicians to have valid and reliable instruments to measure resilience and its changes throughout the recovery process in patients with severe mental disorder.
The study of resilience in people with severe mental disorder can identify those characteristics that could be overcome in adverse situations and the most appropriate strategies to strengthen them. Thus, it could be identified predisposing or risk factors involved in the recovery process, develop new intervention strategies both preventive and therapeutic.
The literature recognizes that symptomatic remission is an insufficient goal in the treatment of serious mental disorders, and that the recovery of premorbid psychosocial functioning should be considered the target of the intervention. In this sense, promoting resilience can help take advantage of personal, family and social resources environment in patients diagnosed with severe mental disorder, which facilitate recovery and even personal growth in the face of adversity. Therefore, the use in the clinical setting of an instrument adapted with good psychometric properties, such as BRCS, is very useful throughout the entire therapeutic process.
The results of the present study should be interpreted taking into account certain limitations that are outlined below, along with suggestions for future research. The sampling method and the composition of the sample limit the generalizability of the results. The size of the men's group, n = 42, was significantly larger than the women’s, n = 15. Moreover, all the participants were in outpatient treatment, and so patients with more severe symptoms were not included, such as institutionalized people. Future studies should use randomized, size-balanced samples in order to ensure the statistical goodness of the comparisons and the generalizability of the results. Likewise, another limitation is the rather small size of the sample in the study. It would be useful to validate this version of the BRCS in a broader population of severe mental disorder patients.
It would have been interesting to test the test-retest reliability and inter-rater reliability. However, it was not possible due to the cross-sectional design of the present study and because the evaluations were carried out by a single evaluator. Future studies with a longitudinal design and several evaluators could provide additional insight into the scale’s reliability.
It would also be interesting to further examine the construct validity of the BRCS in different populations (such as people with disabilities, caregivers of dependents, people with chronic or terminal illnesses, among others). In future studies it would be interesting to verify the validity of BRCS to assess resilience in other diagnoses, for example in psychotic patients with other characteristics than those presented in the sample of the present study. In this sense, Bernardo et al., (Reference Bernardo, Bioque, Parellada, Ruiz, Cuesta, Llerena, Sanjuán, Castro-Fornieles, Arango and Cabrera2013) carried out a research on the clinical and neuropsychological characterization of patients with a first psychotic episode. It would be interesting to include in this type of studies measures such as BRCS to assess resilience from the early stages of psychosis.
Despite these limitations, the unique contributions of this study are worth highlighting. The BRCS is a brief, self-administered scale that has shown optimal psychometric properties, validity, and reliability. This scale could be particularly useful to assess people who have difficulties completing longer questionnaires and to carry out longitudinal studies. Another strength of the current study is its confirmatory nature. To our knowledge, this study is the only one that has analyzed the factor structure of the BRCS in severe mental disorder patients. Thus, the current study is original and might lead to future research on this scale and encourage cross-cultural studies on resilience.
It is important to study the mechanisms that contribute to the recovery of patients with severe mental disorders, including the use of instruments for the assessment of resilience with adequate psychometric properties. In this regard, the BRCS could be useful in clinical practice to better plan interventions. Likewise, the BRCS could be an indicator of the recovery process.




