An elevated number of people are facing the burden of obesity, which is defined as a Body Mass Index (BMI) of ≥ 30 kg/m2 (Haslam & James, Reference Haslam and James2005). Previous research has showed that decreases in weight after bariatric surgery improve clinical parameters of health and enhance health related quality of life of patients with obesity (see for a meta-analysis, Magallares & Schomerus, Reference Magallares and Schomerus2015). In addition, depression and anxiety are usually correlated with obesity (Strine et al., Reference Strine, Mokdad, Dube, Balluz, Gonzalez and Kroenke2008). Recent meta-analyses have found that obesity increases the risk of depression and that depression was found to be predictive of developing obesity (Luppino et al., Reference Luppino, de Wit, Bouvy, Stijnen, Cuijpers, Penninx and Zitman2010) and that a positive association between obesity and anxiety disorders exists (Gariepy, Nitka, & Schmitz, Reference Gariepy, Nitka and Schmitz2010). In Spain, the country where this study has been carried out, obesity reaches currently a prevalence rate of 21.6 % (Aracenta-Bartrina, Pérez-Rodrigo, Alberdi-Aresti, Ramos-Carrera, & Lázaro-Masedo, Reference Aracenta-Bartrina, Pérez-Rodrigo, Alberdi-Aresti, Ramos-Carrera and Lázaro-Masedo2016).
Obesity can be considered a social stigma (Puhl, Heuer, & Brownell, Reference Puhl, Heuer, Brownell, Kopelman, Caterson and Dietz2010). Individuals with obesity have to face discrimination in many social areas, like in employment, healthcare settings, educational contexts, and at every day activities (see for a review, Puhl & Heuer, Reference Puhl and Heuer2009). A recent meta-analysis shows the strong link between perceived discrimination and health related quality of life in several stigmatized groups (Schmitt, Branscombe, Postmes, & Garcia, Reference Schmitt, Branscombe, Postmes and Garcia2014).
It is important to make a distinction between two types of discrimination that people with obesity suffer. Blatant or overt discrimination refers to discrimination which is open and is not hidden in any given way (Magallares, Luna, Garriga, Botella-Carretero, & Morales, Reference Magallares, Luna, Garriga, Botella-Carretero and Morales2016). On the other hand, subtle discrimination is a broad range of behaviors and events that perpetuate inequities for members of stigmatized groups but because of their nature are difficult to identify (King, Shapiro, Hebl, Singletary, & Turner, Reference King, Shapiro, Hebl, Singletary and Turner2006). For example, it has been shown that individuals who are overweight face weight bias at every stage of the employment cycle, but this discrimination may be related to the wage a person with obesity receive (more blatant) or to the way they are treated in the workplace by their colleagues (more subtle; see for a review, Nowrouzi et al., Reference Nowrouzi, McDougall, Gohar, Nowrouz-Kia, Casole and Ali2015). Recently, it has been shown that both types of discrimination are negatively related to health related quality of life in patients with obesity (Magallares, Benito de Valle, Irles, & Jauregui-Lobera, Reference Magallares, Benito de Valle, Irles and Jauregui-Lobera2014). In addition, it was found that greater stigmatizing experiences were significantly related to depression in individuals with obesity (Koball & Carels, Reference Koball and Carels2011) and that perceived weight discrimination was associated with anxiety disorders (Hatzenbuehler, Keyes, & Hasin, Reference Hatzenbuehler, Keyes and Hasin2009).
Besides the mentioned weight bias that people with obesity suffer, individuals with overweight are frequently aware of stigma directed at others who have a similar weight and come to think stigmatized thoughts about themselves (Ratcliffe & Ellison, Reference Ratcliffe and Ellison2015). In other words, weight self-stigma or internalized weight stigma emerges when individuals with overweight internalize the stereotypes that exist about people with obesity and, then, show negative emotional reactions, and discriminate themselves (Hilbert et al., Reference Hilbert, Braehler, Schmidt, Löwe, Häuser and Zenger2015). Weight self-stigma is positively associated to depression (Durso et al., Reference Durso, Latner, White, Masheb, Blomquist, Morgan and Grilo2012) and related to more anxiety (Hilbert, Braehler, Haeuser, & Zenger, Reference Hilbert, Braehler, Haeuser and Zenger2014). In addition, it has been shown that the association between higher BMI and poorer quality of life was found only in individuals with obesity reporting high levels of internalized weight stigma (Latner, Barile, Durso, & O’Brien, Reference Latner, Barile, Durso and O’Brien2014). This last result suggests the mediational effect that weight self-stigma may be having in the relationship between discrimination experiences and quality of life of individuals with obesity. In this line of thinking, it has been said recently that internalized weight stigma may be a mediator between perceived discrimination and different psychopathological outcomes (see for a review, Sikorski, Luppa, Luck, & Riedel-Heller, Reference Sikorski, Luppa, Luck and Riedel-Heller2015).
According to the reviewed literature, it is expected a positive relationship between blatant and subtle discrimination (Magallares et al., Reference Magallares, Benito de Valle, Irles and Jauregui-Lobera2014) and internalized weight stigma (Latner et al., Reference Latner, Barile, Durso and O’Brien2014). In addition, it is expected a positive relationship between blatant and subtle discrimination and depression (Koball & Carels, Reference Koball and Carels2011) and anxiety (Hatzenbuehler et al., Reference Hatzenbuehler, Keyes and Hasin2009). In the third place, it is expected that weight self-stigma will be positively related to depression (Durso et al., Reference Durso, Latner, White, Masheb, Blomquist, Morgan and Grilo2012) and anxiety (Hilbert et al., Reference Hilbert, Braehler, Haeuser and Zenger2014), and that these two variables will be related to each other (Strine et al., Reference Strine, Mokdad, Dube, Balluz, Gonzalez and Kroenke2008). Finally, it will be tested if internalized weight stigma is mediating the relationship between perceived discrimination, both blatant and subtle, and depression and anxiety (Sikorski et al., Reference Sikorski, Luppa, Luck and Riedel-Heller2015).
Method
Sample
The sample comprised 170 participants with obesity from the Clinical Nutrition Unit (CNU) of the “Hospital de Valme” (Seville, Spain) with a mean age of 46.96 (SD = 13.21) and an age range between 20 and 76. 111 were males and 59 were females. These participants attended the CNU in order to receive treatment meanly focused on a weight loss program. The mean BMI was 42.75 (SD = 8.32). 55.9 % of our participants had primary studies, 35.9 % secondary studies and 8.2% university studies. 67.6% of our participants were unemployed. All of them voluntarily agreed to participate in the study.
Procedure
All participants received treatment in the CNU of the “Hospital de Valme” as outpatients. After having obtained the CNU Headmaster’s permission and the patients’ informed consent, participants fulfilled the questionnaires and scales individually and without time limits. The procedure was supervised by a nutritionist, instructing the participants about how to fill in the questionnaires and scales until they were completely sure about their fully understanding of the instructions. The participants developed their task in a suitable setting. As we noted above, all the participants volunteered to take part in the study and none of them received any kind of reward after fulfilling the task. The anthropometric measures (weight, height) were taken by some members of the CNU (nurses and dieticians) who treated the patients, so with enough experience of working in this type of studies. All participants who were invited attended regularly the CNU and none of them refused to participate in this study. With respect to the inclusion/exclusion criteria, all patients who were attending the CNU regularly and with a good adherence were invited to participate. Patients with other diagnostics (for example eating disorders or other mental illnesses) were excluded as well as those who were not able to follow the treatment as outpatients due to medical complications or difficulties to go on a diet (it should be noted that the treatment was based on a dietetic program aimed to lose weight).
Instruments
To measure internalized weight stigma, the Weight SelfStigma Questionnaire (WSSQ; Lillis, Luoma, Levin, & Hayes, Reference Lillis, Luoma, Levin and Hayes2010; Spanish version: Magallares et al., Reference Magallares, Bolaño-Rios, Ruiz-Prieto, Benito de Valle, Irles and Jauregui-Loberain press) was used. The WSSQ contains 12 items (Example: “Others will think I lack self-control because of my weight problems”). The participants filled in a Likert scale ranging from 1 (“strongly disagree”) to 5 (“strongly agree”). The WSSQ had a Cronbach’s α of .77. A score was computed by averaging the corresponding items for the WSSQ. Higher scores on the WSSQ reflect more internalized weight stigma.
To measure blatant and subtle discrimination, the Multidimensional Perceived Discrimination Scale (English and Spanish version: Molero, Recio, García-Ael, Fuster, & Sanjuan, Reference Molero, Recio, García-Ael, Fuster and Sanjuán2013) was used. This scale consists of 10 items that measure, in a 5-point Likert scale, two aspects of perceived discrimination: blatant (7 items) and subtle (3 items). An example of the blatant subscale (α = .83) is “I have been treated unfairly for being obese” and in the case of the subtle subscale (α = .91) “Even though there is no express rejection, people treat me differently when they see I am obese”. Two scores were computed, one for each dimension, by averaging the corresponding items for each of these subscales. Higher scores on blatant discrimination reflect more overt rejection. Higher scores on subtle discrimination reflect more subtle rejection.
To measure depression and anxiety, the Hospital Anxiety and Depression Scale (HAD; Zigmond & Snaith, Reference Zigmond and Snaith1983; Spanish version: Terol-Cantero, Cabrera-Perona, & Martín-Aragón, Reference Terol-Cantero, Cabrera-Perona and Martín-Aragón2015) was used. This scale consists of 14 items that measure, in a 5-point Likert scale, depression (7 items) and anxiety (7 items). An example of depression (α = .80) is “I have lost interest in my appearance” and in the case of anxiety (α = .86) “Worrying thoughts go through my mind”. Two scores were computed, one for each dimension, by averaging the corresponding items for each of these subscales. Higher scores on depression reflect a lower mood. Higher scores on anxiety reflect more nervous behavior.
BMI was calculated as the relationship between weight (kg) and height squared (m2). Weight and height were taken in individual sessions, with the participants in the standing position, barefoot, and in light garments. A stadiometer (Atlántida S13; Básculas y Balanzas Añó-Sayol, Barcelona, Spain) was used.
Finally, sociodemographic questions (age, sex, level of studies, employment situation) of the participants were requested.
Data analysis
First of all, descriptive analyses were conducted. Means and standard deviations in all the variables of the study were estimated. In addition, it was analyzed whether our data matched a normal distribution. To do so, it was decided to measure the asymmetry and kurtosis of the variables used in the study.
The next step was to conduct Student’s t with all the variables of our study to check if there were sex differences.
After that, Pearson’s correlations were calculated among all the variables of the study.
Then, a path analysis with blatant and subtle discrimination as the independent variables, weight self-stigma as the mediator variable, and depression and anxiety as the dependent variables, was conducted. We decided to introduce the manifest variables in the model following the recommendations of experts in the field (Kline, Reference Kline2011). This approach is quite common in the weight stigma field (see for example recently, Himmelstein & Tomiyama, Reference Himmelstein and Tomiyama2015). To determine goodness of fit, the following indexes were employed: the chi square, the Normal Fit Index (NFI), the Comparative Fit Index (CFI) and the Standardized Root Mean Square Residual (RMSEA).
The AMOS program (Arbuckle, Reference Arbuckle2011) for the path analysis, and SPSS program (v. 22.0, SPSS Inc, Chicago, IL) for the rest of the analyses were used.
Results
Exploratory analysis
First of all, means, standard deviations, asymmetry and kurtosis of all the variables of the study were calculated. According to the analyses performed (see Table 1), the variables of the current study matched a normal distribution (values of between -2 and +2; George & Mallery, Reference George and Mallery2010).
Table 1. Descriptives of the variables of the study

Note: Scales from 1 to 5, except BMI
WSS: Weight Self-Stigma; BMI: Body Mass Index; SD: Standard deviation
Sex differences
Sex differences were checked with Student’s t. As it can be seen in Table 2, the differences between men and women were not very high in the variables of the study. According to the obtained results, these differences were not significant (all ps > .05).
Table 2. Mean (Standard Deviations) in males and female participants of the study

Note: Scales from 1 to 5, except BMI
WSS: Weight Self-Stigma; BMI: Body Mass Index
Correlational analysis
Once the means and standard deviations were estimated and sex differences were checked, Pearson’s correlations of all the variables of the study were calculated. As it can be seen in Table 3, it has been found a positive relationship between weight self-stigma and depression, anxiety, BMI, blatant and subtle discrimination. In addition, blatant and subtle discrimination were positively related to depression and anxiety. BMI was only related to subtle discrimination but not to blatant discrimination, and depression and anxiety were positively related to each other. Finally, blatant and subtle discrimination were correlated to each other.
Table 3. Correlations between the variables of the study
** p < .01
WSS: Weight Self-Stigma; BMI: Body Mass Index
Path analysis
A path analysis was conducted with blatant and subtle discrimination, weight self-stigma and depression and anxiety as the main variables. The direct relationships between blatant discrimination and depression (p = .94) and anxiety (p = .70), and between subtle discrimination and depression (p = .18) and anxiety (p = .22) were removed from the final model because there were not significant. The final model obtained can be seen in Figure 1. The goodness of fit indices obtained for the model without the direct relationships between the independent and dependent variables were satisfactory: χ2(4) = 3.71, p = .44; CFI = .99; NFI = .98; RMSEA = .01. According to experts, if the chi-square is not significant, the model is regarded as acceptable (Kline, Reference Kline2011). In addition, values higher than .95 on the NFI and CFI indicate good fit (Kline, Reference Kline2011). Finally, values lower than .05 on the RMSEA indicate good fit (Kline, Reference Kline2011).
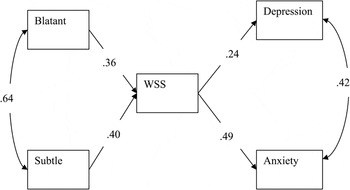
Figure 1. Path analysis.
Note: Standardized estimations of the model. The values of the arrows are the standardized regression coefficients (β).
WSS: Weight Self-Stigma.
According to the model, blatant and subtle discrimination had a positive and direct effect on weight self-stigma. Blatant and subtle discrimination had an indirect effect on depression and anxiety trough weight self-stigma. Finally, it is showed a positive and direct effect of weight self -stigma on depression and anxiety.
Discussion
According to the obtained results, it can be said that all the hypotheses of the study can be maintained. We have found positive and significant correlations between the variables of the study, such as blatant and subtle discrimination, weight self-stigma and depression and anxiety, as expected. Finally, the proposed model with weight self-stigma as a mediator variable has been tested with a path analysis and has been confirmed attending to the goodness of fit indices obtained.
In the first place, as expected, a positive relationship between blatant and subtle discrimination (Magallares et al., Reference Magallares, Benito de Valle, Irles and Jauregui-Lobera2014) and internalized weight stigma (Latner et al., Reference Latner, Barile, Durso and O’Brien2014) was found. These results confirm what have been showed in the reviewed literature. In the second place, as it was hypothesized, a positive relationship between blatant and subtle discrimination and depression (Koball & Carels, Reference Koball and Carels2011) and anxiety (Hatzenbuehler et al., Reference Hatzenbuehler, Keyes and Hasin2009) was found. Again, this result is congruent with the previous research about this topic. In the third place, weight self-stigma was positively related to depression (Durso et al., Reference Durso, Latner, White, Masheb, Blomquist, Morgan and Grilo2012) and anxiety (Hilbert et al., Reference Hilbert, Braehler, Haeuser and Zenger2014) as the reviewed literature had found previously. In addition, depression and anxiety were related to each other (Strine et al., Reference Strine, Mokdad, Dube, Balluz, Gonzalez and Kroenke2008). Finally, is has been shown that internalized weight stigma was a mediator in the relationship between perceived discrimination, both blatant and subtle, and depression and anxiety (Sikorski et al., Reference Sikorski, Luppa, Luck and Riedel-Heller2015) as the path analysis has demonstrated. In this case, it can be said that this result is a novelty in the field on the study of the social stigma of obesity. It is important to remark, that according to the results of the current study, the relationship between the independent and dependent variables were fully mediated by the mediator variable because it has been found that the inclusion of the weight self-stigma made non-significant the relationships between blatant and subtle discrimination and depression and anxiety (Shrout & Bolger, Reference Shrout and Bolger2002). This last result suggests that discrimination experiences, both blatant and subtle, are positively related to weight self-stigma in people with obesity, and that these negative beliefs about themselves increase the possibility to develop depression and anxiety problems.
In addition, results of the current study show that BMI was not significantly correlated to depression and anxiety. This is an unexpected result given previous meta-analyses showed that depression (Luppino et al., Reference Luppino, de Wit, Bouvy, Stijnen, Cuijpers, Penninx and Zitman2010) and anxiety (Gariepy et al., Reference Gariepy, Nitka and Schmitz2010) were positively related to body weight. This finding may be explained by the fact that our sample was entirely composed by individuals with obesity. Probably, with a population-based sample, BMI would be significantly related to the variables we measured. In addition, we believe that these results may be also suggesting that it is not body weight itself causing less quality of life in patients with obesity but that there are other social variables that may influence the health related quality of life of people with obesity as it has been showed in this study. In this line of thinking, a recent meta-analysis showed that patients with obesity do not necessarily report less health related quality of life compared to normal weight individuals (Magallares & Pais-Ribeiro, Reference Magallares and Pais-Ribeiro2014).
We believe that the current results have potential clinical implications. We suggest that it may be important for clinicians to assess and treat not just patients’ body weight, but also the social consequences that their weight may be having in their lives (Puhl & Heuer, Reference Puhl and Heuer2010). The reviewed literature indicates that individuals with obesity may engage in a variety of self-protective coping strategies in order to enhance their health related quality of life (Puhl & Brownell, Reference Puhl and Brownell2006). These authors suggest that what contributes more strongly to depression or anxiety in people with obesity is not the stigmatizing situation itself but the ways in which an individual copes with these experiences (see for a review, Puhl & Brownell, Reference Puhl and Brownell2003). Future studies should address which variables may help individuals with obesity to cope better with weight self-stigma and discrimination experiences (Myers & Rothblum, Reference Myers, Rothblum and Chin2010).
The current study is subject to at least three limitations that deserves mention. The cross-sectional nature of our study is limited and longitudinal (see for example, Sutin & Terracciano, Reference Sutin and Terracciano2013) or experimental studies (see for example, Magallares, Rubio, & Morales, Reference Magallares, Rubio and Morales2011) are needed. However, it is important to remark that this problem may be partially solved using AMOS software. According to experts, structural equations procedures help to understand the causal relationships between the variables of the study (Arbuckle, Reference Arbuckle2011). On the second place, the ratio of women/men of our sample (111 men and 59 women) should be more similar to the one in the general population. This limitation may be an important issue because there are more female patients than men in the treatment for obesity (Kulie et al., Reference Kulie, Slattengren, Redmer, Counts, Eglash and Schrager2011). However, it is important to remark that in Spain the prevalence of obesity in men (22.8%) is higher than in women (20.5%; Aranceta-Bartrina et al., Reference Aracenta-Bartrina, Pérez-Rodrigo, Alberdi-Aresti, Ramos-Carrera and Lázaro-Masedo2016). Finally, the study is only based on self-report measures. According to experts, new measures need to be developed in the next years to provide a more direct assessment of experiences related to weight stigma (DePierre & Puhl, Reference DePierre and Puhl2012).
These limitations considered, the current study offers new directions for the study of the relationship between perceived discrimination, weight self-stigma, depression, and anxiety in individuals with obesity. With the growing prevalence of obesity (Ng et al., Reference Ng, Fleming, Robinson, Thomsom, Greatz, Morgono and Gakidou2014), it is becoming increasingly important to understand the ways in which some of the social variables that we have analyzed in this studio may be having an influence on health related quality of life of people with obesity. For example, recent systematic reviews show that weight stigma leads to less support of prevention and intervention measures in people with weight problems (Sikorski et al., Reference Sikorski, Luppa, Kaiser, Glaesmer, Schomerus and Riedel-Heller2011), that weight stigmatization is an important contributor to negative health outcomes and behaviors that can promote and exacerbate obesity (Puhl & Suh, Reference Puhl and Suh2015), and that stigma can reduce the quality of care for patients with obesity (Phelan et al., Reference Phelan, Burgess, Yeazel, Hellerstedt, Griffin and van Ryn2015). Thus, future studies should continue analyzing this important topic both for improving the life conditions of individuals with obesity, and also as part of efforts to denounce weight discrimination.
This study presents some contributions with respect to the previous literature. First of all, to our knowledge, no other study has investigated the relationship between blatant and subtle discrimination, weight self-stigma, depression, and anxiety in individuals with obesity at the same time. In addition, in this study a path analysis has been conducted that helps to give an integrative view of the variables that are related to the social stigma of obesity. We believe that this article enriches and extends the field of the stigma of obesity, as it provides a series of approaches that have not been taken into account before.






