Article
While there has long been concern about early death among the seriously mentally ill, this worry burst into prominence in 2006 with a report by the National Association of State Mental Health Program Directors in the USA that people diagnosed with schizophrenia and other serious psychiatric disorders were dying 25 years earlier than normal. While suicide and accidental deaths account for 35%–40% of this excess mortality, nearly two-thirds is attributable to somatic diseases—cardiovascular illnesses, diabetes, and respiratory ailments in particular (Parks, Svendsen, Singer, & Foti, Reference Parks, Svendsen, Singer and Foti2006).
The risks of developing such illnesses are known to be elevated due to the adverse effects of antipsychotics, which leads to a concern that these medications contribute to the mortality gap. However, in 2009, Finnish investigators concluded that over a 11-year period cumulative usage of antipsychotics reduced mortality (Tiihonen et al., Reference Tiihonen, Lönnqvist, Wahlbeck, Klaukka, Niskanen, Tanskanen and Haukka2009). Since then, the Finnish researchers and a handful of others have published papers that support this conclusion, which has produced headlines—at least in the USA—of this newly discovered benefit of antipsychotics.
Science Daily: ‘Use of antipsychotic drugs improves life expectancy for individuals with schizophrenia.’ (Johns Hopkins Medicine, 2012)
Psychiatry and Behavior Health Learning Network: ‘Antipsychotics appear to halve mortality risk in schizophrenia.’ (Tumolo, Reference Tumolo2018)
This claim has come at a time that other research has led to questions about the long-term use of antipsychotics. Harrow reported that the long-term recovery rate for schizophrenia patients off antipsychotic medication was eight times higher than for medicated patients and a handful of other studies have found that the drugs may hinder long-term functioning (Albert et al., Reference Albert, Randers, Allott, Jensen, Melau, Hjorthøj and Nordentoft2019; Harrow & Jobe, Reference Harrow and Jobe2007; Wunderink, Nieboer, Wiersma, Sytema, & Nienhuis, Reference Wunderink, Nieboer, Wiersma, Sytema and Nienhuis2013). In addition, the fact that antipsychotics appear to shrink brain volumes has led to questions about their long-term use (Murray, Reference Murray2017).
The claim that antipsychotics reduce mortality rates provides a counter to those concerns (Goff et al., Reference Goff, Falkai, Fleischhacker, Girgis, Kahn, Uchida and Lieberman2017). Thus, the question of the impact of antipsychotics on mortality rates among those diagnosed with schizophrenia becomes central to this larger question about their long-term use.
The mortality gap
The mortality gap between the seriously mentally ill and the general population, while it may be greater in the USA than in Finland and other Scandinavian countries, widened over the past 40 years. A systematic review of standardized mortality ratios (SMRs) of schizophrenia patients in 25 nations found that ‘all-cause mortality’ rose from 1.84 in the 1970s to 2.98 in the 1980s to 3.20 in the 1990s (Saha, Chant, & McGrath, Reference Saha, Chant and McGrath2007).
More recently, a UK study found that the SMR for bipolar patients, who today are often treated with second-generation antipsychotics, rose steadily from 2006 to 2014, increasing by 0.14 per year. The SMR for schizophrenia patients increased gradually from 2004 to 2010 (0.11 per year), and then more rapidly from 2010 to 2014 (0.34 per year.) (Hayes, Marston, Walters, King, & Osborn, Reference Hayes, Marston, Walters, King and Osborn2017).
The evidence that antipsychotics contribute to early death
Although it is common to categorize antipsychotics as either ‘first-generation’ or ‘second-generation’ drugs, the adverse-event profiles of individual antipsychotics vary greatly, depending on the neurotransmitter systems they disrupt and with what potency. As a class of drugs, antipsychotics may cause a long list of adverse effects, which increase the risk for a number of somatic ailments. In particular, the drugs are known to increase the risk for cardiovascular, respiratory, and endocrine diseases (Correll, Detraux, De Lepeleire, & De Hert, Reference Correll, Detraux, De Lepeleire and De Hert2015).
Excess mortality among the seriously mentally ill due to somatic illnesses
Mortality studies have found varying SMRs for people diagnosed with schizophrenia (or the seriously mentally ill), both for all-cause mortality and for specific diseases (Table 1).
Table 1. Excess mortality among seriously mentally ill: standardized mortality ratios
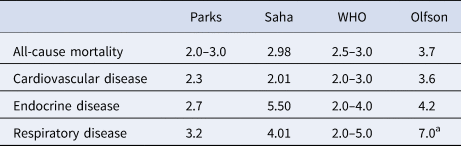
a SMR for pneumonia/influenza.
Two of the four studies in Table 1 charted SMRs among the seriously mentally ill in the USA (Olfson, Gerhard, Huang, Crystal, & Stroup, Reference Olfson, Gerhard, Huang, Crystal and Stroup2015; Parks et al., Reference Parks, Svendsen, Singer and Foti2006) and the other two charted global SMRs (Saha et al., Reference Saha, Chant and McGrath2007; World Health Organization, 2015). All four found that the seriously mentally ill, a large percentage of whom are prescribed antipsychotics, die from somatic illnesses at rates two to five times that of the general population.
The excess mortality due to somatic illnesses among the seriously mentally ill is often attributed to the ‘disease’ or to their unhealthy behaviors, as opposed to the adverse effects of antipsychotics. Yet, even if the seriously mentally ill, quite apart from any treatment effect, often suffer from poor physical health, the adverse effects of antipsychotics could still be expected to contribute to this excess mortality.
Excess mortality among all users of antipsychotics
In a study published in 2013, UK investigators assessed ‘mortality among antipsychotic users related to nonusers.’ They utilized a database of nearly 11 million patients treated in primary care from 1995 to 2010 to identify three cohorts of patients: all users of antipsychotics, regardless of whether they had a psychiatric diagnosis; non-users from the general population; and non-users who had a psychiatric diagnosis of schizophrenia, bipolar, or depression (Murray-Thomas et al., Reference Murray-Thomas, Jones, Patel, Brunner, Shatapathy, Motsko and Van Staa2013).
They reported ‘fully adjusted’ SMRs, meaning that sought to equalize risk factors in comparisons between any two groups, other than their use of antipsychotics. They made two important findings.
First, users of antipsychotics in the general population were almost three times as likely to die as non-users in the general population. All-cause mortality = 2.72; cardiac mortality = 1.83; sudden cardiac death = 4.03.
Second, users of antipsychotics in the general population were more likely to die than non-users with a psychiatric diagnosis. All-cause mortality = 1.75; cardiac mortality = 1.72; sudden cardiac death = 5.76.
The UK study provides evidence that antipsychotics elevate mortality in non-psychiatric patients and that non-psychiatric patients who take antipsychotics are at greater risk of dying than psychiatric patients who do not take them.
There are numerous other studies that have assessed the impact of antipsychotics on mortality rates in non-psychiatric patients, for various illnesses and in different age groups, and researchers regularly find that antipsychotics elevate SMRs for all-cause mortality and cardiac disease (Basciotta et al., Reference Basciotta, Zhou, Ngo, Donnino, Marcantanio and Herzig2020; Calsolaro, Antognoli, Okoye, & Monzani, Reference Calsolaro, Antognoli, Okoye and Monzani2019; Harrison et al., Reference Harrison, Sluggett, Lang, Whitehead, Crotty, Corlis and Inacio2020; Hoang, Stewart, & Goldacre, Reference Hoang, Stewart and Goldacre2011; Jayatilleke, Hayes, Chang, & Stewart, Reference Jayatilleke, Hayes, Chang and Stewart2018; Jennum, Baandrup, Ibsen, & Kjellberg, Reference Jennum, Baandrup, Ibsen and Kjellberg2015; Maust et al., Reference Maust, Kim, Seyfried, Chiang, Kavanagh, Schneider and Kales2015; Ralph & Espinet, Reference Ralph and Espinet2018; Ray et al., Reference Ray, Stein, Murray, Fuchs, Patrick, Daugherty and Cooper2019; Ray, Chung, Murray, Hall, & Stein, Reference Ray, Chung, Murray, Hall and Stein2009; Weintraub et al., Reference Weintraub, Chiang, Kim, Wilkinson, Marras, Stanislawski and Kales2016).
In a 2018 meta-analysis, Australian investigators concluded that ‘antipsychotic drugs precipitate excessive mortality across the spectrum,’ including in ‘general mental health care.’ They wrote that all-cause mortality of ‘patients prescribed antipsychotic drugs is close to two,’ and is dose-related (Ralph & Espinet, Reference Ralph and Espinet2018). (Their meta-analysis did not include studies of mortality rates in psychotic patients.)
Excess mortality in cohorts of psychotic patients
The studies cited above relied on large databases of medical records to calculate SMRs in patients grouped according to diagnosis or antipsychotic use. There have been a handful of studies of small cohorts of psychotic patients that have assessed whether variations in antipsychotic use affected their risk of dying.
In a study of chronic patients in Ireland, average age 62, 44% died within the next 10 years. Two-thirds died from either cardiovascular or respiratory illness. The researchers concluded that ‘the greater the number of antipsychotics given concurrently, the shorter was patient survival’ (Waddington, Youssef, & Kinsella, Reference Waddington, Youssef and Kinsella1998).
In a 17-year study of 99 schizophrenia patients in Finland, researchers identified four groups at study entry: 20 who were not taking an antipsychotic, 31 who were taking one antipsychotic, 34 who were taking two antipsychotics, and 14 who were taking three or more. During the study, 39 of the 99 died. SMRs for the four groups, compared with the general population (matched for age and gender), were 1.29 for no-antipsychotics, 2.97 for one antipsychotic, 3.21 for two antipsychotics, and 6.83 for three or more (Joukamaa et al., Reference Joukamaa, Heliövaara, Knekt, Aromaa, Raitasalo and Lehtinen2006). The researchers concluded: ‘The present study demonstrated a graded relationship between the number of neuroleptic drugs prescribed and mortality of those with schizophrenia. This relationship and the excess mortality among people with schizophrenia could not be explained by coexistent somatic diseases or other known risk factors for premature death.’
A third cohort study provides a comparison of mortality rates for first-episode psychotic patients treated either with Open Dialogue therapy in Western Lapland, Finland or conventional treatment elsewhere in the country. Open Dialogue limits both the immediate and long-term use of antipsychotics and thus this study provides a preliminary comparison between two different paradigms of care.
At the end of 19 years, only 55% of the 113 Open Dialogue group had ever been exposed to antipsychotics and only 36% were on the drugs. In contrast, 97% of the 1763 patients in the comparison group had been exposed and 81% were on antipsychotics at the end of the study. Eleven of the Open Dialogue cohort died (10%) during the lengthy follow-up, while 296 in the conventionally treated cohort died (17%.) While this mortality difference was not “statistically” significant (because the number treated with Open Dialogue was so small), it is still of note that the mortality rate was lower in the group with less exposure to antipsychotics (Bergström et al., Reference Bergström, Seikkula, Alakare, Mäki, Köngäs-Saviaro, Taskila and Aaltonen2018).
Suicide in the antipsychotic era
Suicide and accidents account for up to 40% of the early-death mortality among the seriously mentally ill and an even higher percentage of all deaths in the first year after diagnosis (Kasckow, Felmet, & Zisook, Reference Kasckow, Felmet and Zisook2011; Parks et al., Reference Parks, Svendsen, Singer and Foti2006). While studies have found that non-adherence to antipsychotics is associated with a higher risk of suicide, suicide rates are higher today than in the pre-antipsychotic era (before 1955), with drug side effects—and despair over their negative effects—a likely contributing cause.
Historical rates of suicide
Although estimates of the lifetime risk of suicide in schizophrenia range from 4% to 13%, with 10% a commonly cited figure, a 2007 review of 51 studies concluded that it was around 5% (Hor & Taylor, Reference Hor and Taylor2010). Even that lower number is higher than the suicide rate for schizophrenia patients in the asylum era.
A study of schizophrenia patients treated at a hospital in Northern Wales from 1875 to 1924 found their lifetime suicide rate was 0.5%. This finding, the researchers concluded, is in line with ‘estimates of a lifetime rate of 1%–2% or lower reported in the methodologically strong studies in the pre-community era’ (Healy et al., Reference Healy, Harris, Tranter, Gutting, Austin, Jones-Edwards and Roberts2006).
A 2002 report by SANE Australia similarly concluded that ‘the suicide rate has risen markedly since deinstitutionalization began—it is at least four times higher today than in studies from the period 1913 to 1960’ (SANE Australia, 2002).
The possible reasons for this increase are thought to be multifactorial. One thought is that asylum care was protective against suicide, and that the higher suicide rate today is a consequence of deinstitutionalization, with the seriously mentally ill poorly served by whatever community care is available. A second thought is that the arrival of antipsychotics in asylum medicine in 1955 is at least partly responsible for this increase.
An exhaustive study of suicides in US Veterans Administration hospitals provides correlative support for that second thought. From 1950 to 1954, the annual suicide rate in VA hospitals was the same for its neuropsychiatric patients as for its medical patients (around 50 per 100 000). Starting in 1955, the suicide rate for neuropsychiatric patients began to steadily climb, such that 20 years later it was eight times higher (400 per 100 000). Although the suicide rate for medical patients went up and down during this period, it stayed well below that of the neuropsychiatric patients and in 1974 it was the same as in 1954 (50 per 100 000) (Farberow, Ganzler, & Cuttler, Reference Farberow, Ganzler and Cuttler1998; as cited by Healy et al., Reference Healy, Harris, Tranter, Gutting, Austin, Jones-Edwards and Roberts2006). A 1962 study also found that there had been an increase in suicides after the introduction of chlorpromazine (Hussar, Reference Hussar1962).
There are three risk factors with antipsychotics that may impact suicide rates.
Drug side effects
Antipsychotics induce akathisia in a significant percentage of patients, which is known to be a risk factor for suicide and violence. Second-generation antipsychotics induce akathisia—an intense inner agitation—in 15%–35% of patients (Salem, Nagpal, PIgott, & Texeira, Reference Salem, Nagpal, PIgott and Texeira2017). The drugs may also induce dysphoric effects that lead to hopelessness and depression, which are risk factors for suicide (Atbaşoglu, Schultz, & Andreasen, Reference Atbaşoglu, Schultz and Andreasen2001).
A recent online survey of 832 antipsychotic users reported that 58% experienced ‘suicidality’ as a side effect of the medication, with 21% reporting it as ‘severe.’ There were a number of emotional and physical adverse effects— ‘feeling not like self’; ‘loss of motivation,’ ‘difficulty concentrating,’ ‘withdrawal effects,’ ‘emotional numbing,’ and ‘loss of sex drive’—that were strongly correlated with feelings of suicidality (Read & Williams, Reference Read and Williams2019).
Among those who thought ‘the drugs had made no difference or had made their problems worse,’ 74% said they experienced suicidality as an adverse effect of treatment. The researchers concluded: ‘Perhaps whatever degree of suicidality is generated by the adverse effects of antipsychotics, the discovery that the drugs do not work, or even make things worse, could further increase depression, hopelessness and suicidality.’
Withdrawal as a risk factor
A significant percentage of psychotic patients treated with antipsychotics in the hospital stopped taking the drug within 12 months after discharge. In some studies, the majority do (Schoenbaum et al., Reference Schoenbaum, Sutherland, Chappel, Azrin, Goldstein, Rupp and Heinssen2017). A common reason for stopping is ‘medication caused unpleasant side effects.’ (Read & Williams, Reference Read and Williams2019)
This exposes them to ‘neuroleptic discontinuation syndromes,’ which is not a risk natural to the disease. Symptoms include insomnia, restlessness, nausea, mood disturbances, severe psychotic relapse, and newly emergent akathisia that may persist for long periods of time. The psychotic symptoms are often seen as a return of the disease, but users tell of a psychosis that is different in kind—and often more severe—than their pre-drug psychosis (Gardos, Cole, & Tarsy, Reference Gardos, Cole and Tarsy1978; Larsen-Barr, Reference Larsen-Barr2016; Larsen-Barr, Seymour, Read, & Gibson, Reference Larsen-Barr, Seymour, Read and Gibson2018; Moncrieff, Reference Moncrieff2006; Moncrieff, Cohen, & Porter, Reference Moncrieff, Cohen and Porter2013; Moser et al., Reference Moser, Reese, Schultz, Benjamin, Arndt, Fleming and Andreasen2005; Read & Williams, Reference Read and Williams2019; Tranter & Healy, Reference Tranter and Healy1998).
This discontinuation syndrome is known to put patients at high risk for harm. A study of schizophrenia patients who stopped filling prescriptions for olanzapine or risperidone for 30 days found that their risk of attempting suicide rose four-fold in subsequent months (Herings & Erkens, Reference Herings and Erkens2003).
Therapeutic despair
First-episode psychotic patients enter into a therapeutic environment that many find profoundly depressing and isolating. They are often told they have a chronic illness and will need to forever take a drug that they find robs them of their ability to feel and emotionally interact with the world.
In one survey, 50% of patients reported they had a ‘wholly negative’ first reaction to antipsychotics, using such words as ‘scary, terrifying, horrifying, hell, a nightmare, traumatic and disempowering’ to describe the experience (Larsen-Barr, Reference Larsen-Barr2016). Yet, those who refuse to take an antipsychotic will likely find themselves in conflict with family and societal demands. They find themselves in a damned-if-they-do and damned-if-they-do not situation.
After hospital discharge, this first-episode cohort breaks into two groups: those who remain medication compliant and those who stop taking antipsychotics. The suicide rate during the first year soars for the cohort as a whole, and in particular, for those who stop taking medication.
A Danish study of 9156 schizophrenia patients hospitalized for the first episode of psychosis between 1970 and 1987 found that the SMR for suicide in the first year, among those under 30 years old, was more than 200 times higher than among the general public (Mortensen & Juel, Reference Mortensen and Juel1993).
Similarly, a US study of 5488 commercially insured first-episode psychotic patients determined that all-cause mortality in the first year was 24 times that of the general population, with nearly 2% dying during that period. More than 60% never filled a prescription for an antipsychotic in the first year following discharge (Schoenbaum et al., Reference Schoenbaum, Sutherland, Chappel, Azrin, Goldstein, Rupp and Heinssen2017).
Young males with good premorbid functioning—high intelligence, high level of education, good school performance, and insight into the illness ‘that leads to hopelessness’—have the highest risk of suicide (Carlborg, Winnerbäck, Jönsson, Jokinen, & Nordström, Reference Carlborg, Winnerbäck, Jönsson, Jokinen and Nordström2010). Having negative feelings about antipsychotics is also a risk factor for suicide (Sher & Kahn, Reference Sher and Kahn2019). These risk factors tell of higher-functioning first-episode patients who, having been exposed to antipsychotics, now view their future with despair.
Two perspectives
The impact of antipsychotics on suicide rates for first-episode patients may be interpreted in two ways. Researchers may compare suicide rates for those who stay on their antipsychotics to those who stop taking them, and if the suicide rate is higher in the latter group, conclude that the drugs are protective against suicide. The “disease” is seen as the risk factor for suicide.
A second way is to look at the suicide rate for the entire cohort during the first year following hospitalization, which provides information about the risk of suicide within a drug-based paradigm of care. Treatment nonadherence—and the associated risks that entails—is understood to be an outcome that occurs with antipsychotic-centered care.
The evidence that antipsychotics reduce mortality
The research most often cited as evidence that antipsychotics reduce mortality has come from a group of Finnish researchers led by Jari Tiihonen. Their studies rely on extracting information from three databases. The first is a national registry of hospitalized patients in Finland dating back to 1965, which gives a diagnosis for all patients. The second is a national database of all outpatient drug prescriptions since 1 January 1996, with each prescription linked to a specific individual by an ID number. The third is a national death registry (Taipale et al., Reference Taipale, Tanskanen, Mehtälä, Vattulainen, Correll and Tiihonen2020; Tiihonen et al., Reference Tiihonen, Wahlbeck, Lönnqvist, Klaukka, Ioannidis, Volavka and Haukka2006, Reference Tiihonen, Lönnqvist, Wahlbeck, Klaukka, Niskanen, Tanskanen and Haukka2009; Tiihonen, Mittendorfer-Rutz, Torniainen, Alexanderson, & Tanskanen, Reference Tiihonen, Mittendorfer-Rutz, Torniainen, Alexanderson and Tanskanen2016; Tiihonen, Tanskanen, & Taipale, Reference Tiihonen, Tanskanen and Taipale2018).
In these studies, outpatient prescriptions serve as a proxy for medication use. If a patient living in the community fills a prescription for an antipsychotic as scheduled, then the patient is deemed to be ‘on medication’ for that time. If a patient fails to fill a prescription, then that person is deemed to be off medication for that time.
There are several methodological issues with this research that need to be understood in order to assess its merits.
Medication usage
The outpatient prescriptions serve as a proxy for antipsychotic usage. However, since this national database did not exist before 1996, there is no assessment of antipsychotic exposure prior to that date. For instance, a person diagnosed in 1965 could have taken antipsychotics for up to 30 years and suffered adverse health effects from this usage, and yet if that person stopped taking the medication prior to 1996, he or she would be counted as a ‘non-user’ of antipsychotics in these studies. The usage of antipsychotics during hospitalization is also not known, which creates a second black hole in this research.
Survivorship bias
In several of the Finnish studies, the average age of patients at baseline is 40 and older. As a result, the studies are assessing mortality in a cohort that has ‘survived’ treatment for a number of years, and thus may not be representative of the larger population of patients so diagnosed and treated prior to 1996. The survivors are a subgroup that apparently tolerates treatment fairly well.
Person-year mortality rates
Tiihonen and colleagues regularly report mortality rates based on ‘person years’ of the collective time that patients spent on or off medication. In non-randomized studies, this is a method that can produce distorted results, particularly if one group can be expected to rack up many more person-years than the other.
For example, consider this scenario. A person diagnosed with schizophrenia during the first 5 years of follow-up is on an antipsychotic and alive at the end of that time. That is five ‘person-years’ of survival on an antipsychotic. Now that same person goes off the medication and dies 1-year later. That is one death in ‘one person year’ off medication. Thus, that one patient provides five ‘person years’ of survival on the drug to the total person-years equation and adds ‘one death per year’ to the off-medication total. Now imagine a second person who is on antipsychotics for 6 years and dies at the end of that 6th year. When the per-person mortality rate is tallied up for these two people, you end up with one death per 11 ‘person years’ on antipsychotics, v. one death per one ‘person year’ off medication.
Thus, in this calculation, the mortality rate is 11 times higher for the off-drug group, even though, during the 6 years, one person had died off medication and one had died on medication.
Reporting outcomes as relative risks
In the Finnish studies, the ‘relative risk’ of death is regularly reported as the primary outcome (instead of the absolute number of deaths.) However, for relative risks to be meaningful, it is necessary to compare outcomes in like populations (age, severity of illness, and so forth), and since these are not randomized studies, there may be notable differences between the ‘off med’ and ‘on med’ groups. Although Tiihonen and colleagues state, in their publications, that they have made statistical adjustments to account for inequalities in the groups being compared, they do not provide information about what the baseline inequalities are. As such, readers are left with a ‘trust us’ result (Tiihonen et al., Reference Tiihonen, Lönnqvist, Wahlbeck, Klaukka, Niskanen, Tanskanen and Haukka2009).
Mortality within a drug-centered paradigm of care
The biggest problem with the database studies is that these data come from patients treated within a drug-centered paradigm of care. To fairly assess the impact of antipsychotics on mortality rates, it would require assessing deaths among first-episode patients treated under differing paradigms of care, one that emphasized antipsychotic usage right from the outset, and one that avoided initial use and minimized long-term use. The Open Dialogue study provided the first hint of such a comparison.
However, except in the Western Lapland region, Finnish psychiatrist regularly prescribes antipsychotics to their psychotic patients. Of the total, 97% of Finnish patients with a schizophrenia diagnosis is exposed to antipsychotics, and the usual practice is to maintain patients so diagnosed on the drugs.
Given this paradigm, those who stop taking antipsychotics after discharge from the hospital continue to suffer a multitude of drug-related risks. They may continue to suffer from cardiovascular and other health problems that arose from their exposure to the drugs. Those stopping their medication likely will suffer withdrawal symptoms—physical, emotional, and psychiatric—that increase their risk of suicide. They will likely experience the social reproach and lack of social support that those diagnosed with schizophrenia regularly experience when they stop taking antipsychotics.
Yet, with the methodology employed in the Finnish research, these mortality risks, which arise within a drug-centered paradigm of care, are chalked up as due to being ‘off medication.’ The exercise rests on a faulty premise, which is that the minute a person does not fill a prescription, the risks due to prior exposure to the drugs vanish.
With those caveats in mind, here are summaries of their three most influential reports.
General population studies
(1) In a 2009 report, Tiihonen and colleagues identified 66 881 people who were admitted to a hospital with a diagnosis of schizophrenia from 1973 to 2004 and assessed their medication use, starting in 1996 based on the outpatient prescription register, for up to 11 years. They concluded that ‘long-term exposure to any antipsychotic treatment was associated with lower mortality than no drug’ (Tiihonen et al., Reference Tiihonen, Lönnqvist, Wahlbeck, Klaukka, Niskanen, Tanskanen and Haukka2009).
Their findings were summed up in a graphic that showed those who took antipsychotics for 2 years or longer were less likely to die than those who did not fill any prescriptions during the 11 years (Fig. 1).
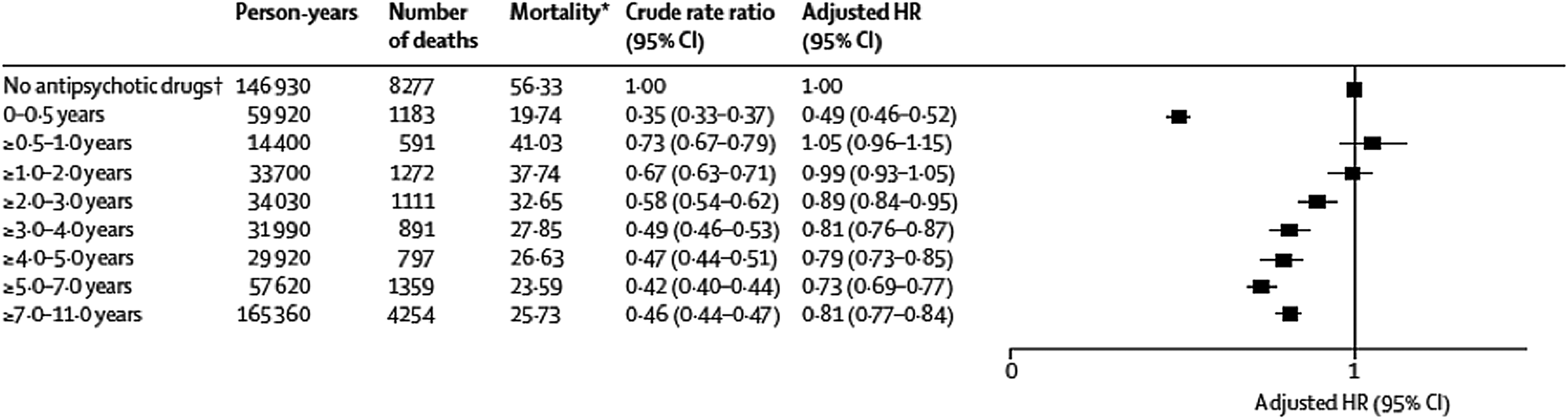
Fig. 1. This is the forest plot that Tiihonen et al. (Reference Tiihonen, Lönnqvist, Wahlbeck, Klaukka, Niskanen, Tanskanen and Haukka2009) used to present adjusted hazard ratios for death using ‘no antipsychotic drugs’ over 11 years as the reference group. With this reference, antipsychotic use is presented as lowering the risk of death.
The methodological issues discussed earlier are present in this study. There is no information about medication usage prior to 1996, even though the average age of the patients at study entry was 51. There is no information about medication usage in the hospital, even though 64% of all deaths occurred in hospitals (De Hert, Correll, & Cohen, Reference De Hert, Correll and Cohen2010). With a population this old, there is obvious survivorship bias. Person-years are used to calculate mortality rates. Outcomes are presented as relative risks. There is nothing about how the usage groups might have differed. All that readers can know is that the investigators sorted through the information in their three databases, performed any number of statistical adjustments, and out came a finding that told of how cumulative use of antipsychotics lowered mortality rates.
Since antipsychotics are regularly prescribed to schizophrenia patients, the first question is this: what is the makeup of the large group of patients who did not use any antipsychotics during the 11-year follow-up and yet died at high rates? There were 18 914 individuals in that no-use group, 8277 of whom died in the 11 years.
The report does not provide any descriptive information for this cohort. However, the ‘adjustments’ to the ‘crude rate ratio’ reveal that the non-users, at the start of the study, were at higher risk of dying than the other groups. This is almost certainly due to this cohort being much older than the others.
There is also a problem with the reporting of results. In their discussion, Tiihonen and colleagues state that ‘long-term use (of antipsychotics) is associated with lower mortality than is no use or short-term use.’ However, their own data reveal that this is not true.
The lowest mortality was among those who had 0–6 months of exposure to antipsychotics over an 11-year period, i.e. a group that hardly used any antipsychotic medication. Indeed, if this low-exposure group had been used as a reference for depicting relative risks, those with 7–11 years of cumulative exposure would have had a 65% greater mortality rate (Fig. 2).
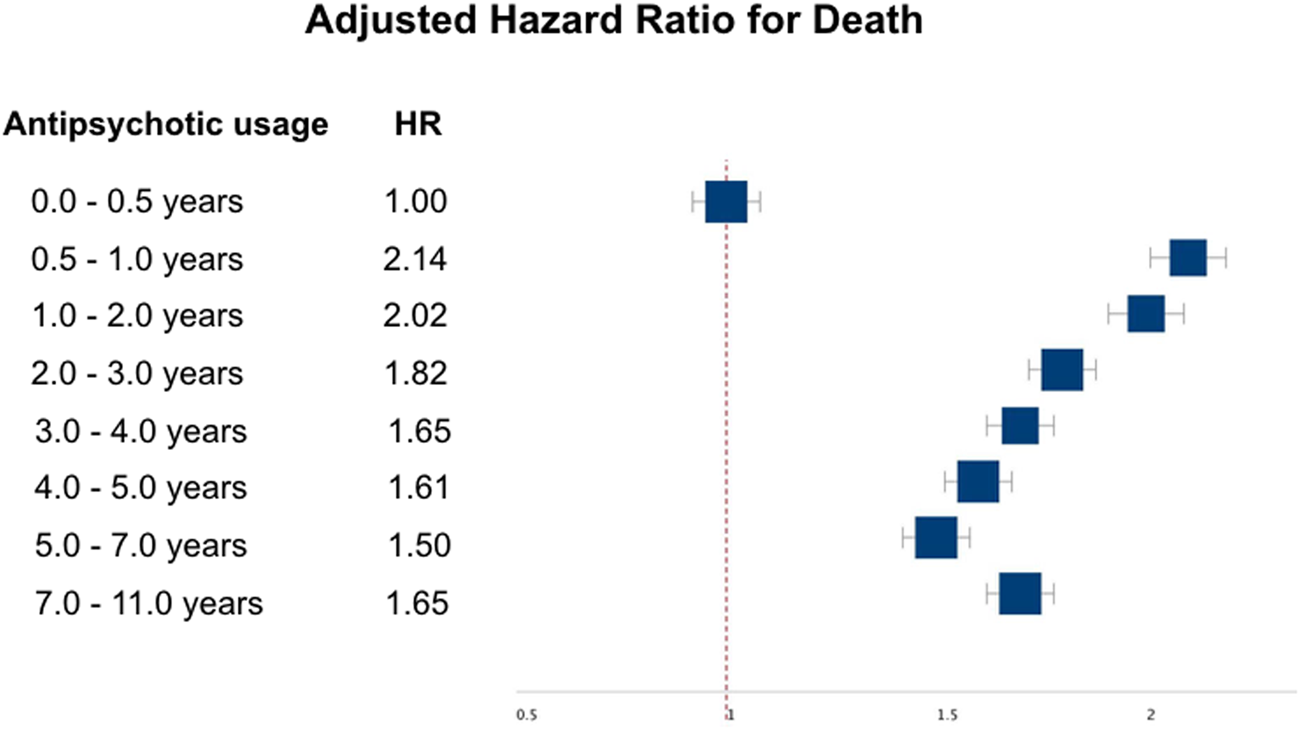
Fig. 2. This forest plot shows the relative risk of death in Tiihonen et al. (Reference Tiihonen, Lönnqvist, Wahlbeck, Klaukka, Niskanen, Tanskanen and Haukka2009) using 0–0.5 years of antipsychotic use as the reference group. When presented this way, it is evident that the group with minimal exposure to antipsychotics over 11 years had the lowest mortality rate.
With the data presented in this way, there is no clear-cut conclusion to be drawn about the impact of antipsychotics on mortality. Death rates are indeed high for those with only 6 months–2 years of exposure over the 11 years. Why might that be? At the same time, why would exposure of 0–6 months over an 11-year period produce the lowest mortality rate? Questions abound.
Given that the standard of care is to maintain schizophrenia patients on medication, here is the paradigm-challenging conclusion that Tiihonen and his colleagues could have written: ‘We found that the lowest mortality was in schizophrenia patients who, over an 11-year period, used antipsychotics for a very short time—six months or less.’
(1) In 2020, Tiihonen and colleagues provided an updated look at mortality drawn from the Finnish databases. However, rather than assess death rates based on cumulative antipsychotic usage, this study focuses on mortality related to on-off use of antipsychotics (Taipale et al., Reference Taipale, Tanskanen, Mehtälä, Vattulainen, Correll and Tiihonen2020).
The study examined antipsychotics usage from 1996 through 2015, based on the outpatient prescription register, for all Finnish adults diagnosed with schizophrenia and treated in a hospital between 1972 and 2014 (N = 62 250.) The researchers found that their ‘all-cause’ risk of dying more than doubled during periods when they were not filling their antipsychotic prescriptions and that cardiovascular mortality also increased during such periods.
To understand this bottom-line result, readers must dig into the data used to calculate the relative risks of death. The average age of the patients at entry into the study was 46. During a median follow-up 14.1 years, 13 899 of the 62 250 patients died (22%). There were 8264 who died while on antipsychotics and 5635 while off antipsychotics. Thus, 59% of the deaths occurred among people who were filling their prescriptions.
However, the researchers reported that the all-cause risk of dying while on medication was 0.48—less than half—that of the risk when patients were off medication. This is a conclusion made possible by the use of ‘person years’ to calculate mortality rates. Although readers need to do the math, there was one death for every 70 person years in the on-medication group (577 417 person years divided by 8264), and one death for every 33 person years in the off-medication group (187 773 person years divided by 5635.)
In their presentation of their results, Tiihonen and colleagues also published a graphic showing that antipsychotics improve survival rates at a steady pace, year after year. The graphic states that it depicts the survival rate for those who used ‘any antipsychotic v. those who used none.’ As such, readers could assume that there was a group in this study who never used antipsychotics for the 20 years and that 46% of these ‘non-users’ died, compared to 26% of those who used antipsychotics (Fig. 3).
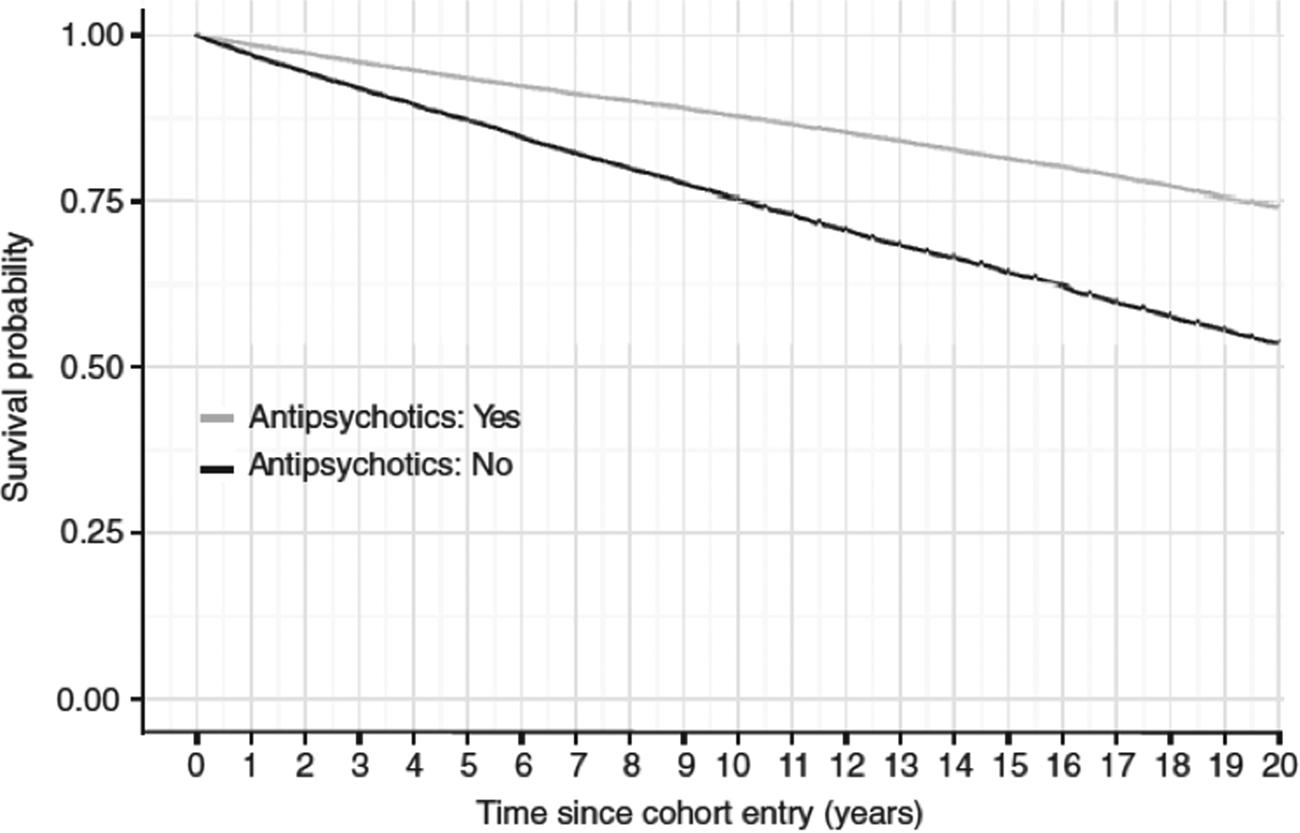
Fig. 3. This is the chart from Taipale et al. (Reference Taipale, Tanskanen, Mehtälä, Vattulainen, Correll and Tiihonen2020) that presented survival rates over the 20-year study.
Nothing like that actually happened in the study.
Here is how the graphic was created. If the mortality rate during off-antipsychotic periods was 1 in every 33 years, then, theoretically, if there were 100 patients at baseline there would be 97 alive at the end of 1 year. If you keep applying the 1-in-33 annual mortality rate for the next 19 years only 54 of the 100 would be alive at the end of 20 years (and 46 would be dead). Apply the same person-year calculations for the ‘on-medication’ group (one death in every 70 person years), then 74 of the 100 would be alive at the end of 20 years and 26 would be dead.
The published article, however, does not describe these calculations. Moreover, there is no group identified in the study that took antipsychotics continuously for 20 years. Nor is there any group identified as never having taken antipsychotics during that period.
The graphic is best described as a statistical mirage. But it is a powerful one. You see the graphic and you see that antipsychotics steadily improved survival rates for schizophrenia patients over two decades. It is a chart that, to the eye and mind, immediately tells of drug treatment that ‘works’ over the long term.
The researchers also reported that antipsychotics reduced cardiovascular mortality, with a relative risk of 0.62 compared to non-use periods. If this study is to be believed, the very drugs that in the general population double the risk of cardiovascular mortality are protective against that risk in people diagnosed with schizophrenia.
First-episode study
In 2006, Tiihonen and colleagues reported on deaths among 2230 adults hospitalized for a first episode of schizophrenia from 1995 through 2001, with their prescription use charted from the moment of their initial discharge (Tiihonen et al., Reference Tiihonen, Wahlbeck, Lönnqvist, Klaukka, Ioannidis, Volavka and Haukka2006).
The average age of the first-episode patients was 30.7 years and they were followed for an average of 3.6 years. As a cohort, these patients were ‘off medication’ 42% of the time. In total, 75 died while in off-medication status: 26 by suicide, 25 in accidents/violence, and 24 from natural causes. Only nine died while on medication: one by suicide, four in accidents/violence, and four from natural causes.
As noted earlier, suicide rates for people diagnosed with schizophrenia increased with the introduction of antipsychotics. One possible reason is that initial use of antipsychotics in the hospital sets up a period of high risk for those who do not like the medications and stop taking them after discharge. In this study, 36% of the discharged patients did not fill a prescription within 30 days, and as can be seen, death by suicide and accident was very high for those who entered this drug-withdrawal risk pool.
The mystery data in this study is that there were six times as many deaths due to natural causes—cardiovascular mortality and such—during ‘off antipsychotic’ periods than in ‘on antipsychotic’ periods. Why would that be? This is a fairly young cohort, and so why would patients who stopped taking the drugs die so frequently from diseases that are known to be elevated by the use of the drugs?
This is a mystery worth investigating, but it would appear to be a finding that tells of how risks from antipsychotic usage, in this on-medication/off-medication binary design, get transferred to the ‘off-medication’ column in one way or another.
SMRs in the database studies
Although Tiihonen did not calculate an SMR rate for the 2230 first-episode patients, a subsequent Finnish report on the 5-year outcomes of first-episode patients, which included this cohort, calculated an SMR of 4.5 (Kiviniemi, Reference Kiviniemi2014). Thus, the mortality rate for first-episode patients treated within this antipsychotic-centered paradigm of care was quite high, even though Tiihonen's study attributed it to being off the drugs.
There have been a handful of other studies that utilized prescription databases to assess mortality hazards-related antipsychotic use, and their findings mostly echo the Finnish findings. They tell of lower all-cause mortality associated with regular antipsychotic use, and yet, at the same time, if they report on SMR rates for the entire cohort, they tell of high mortality rates (Cullen et al., Reference Cullen, McGinty, Zhang, dosReis, Steinwachs, Guallar and Daumit2013; Khan, Faucett, Morrison, & Brown, Reference Khan, Faucett, Morrison and Brown2013).
This finding shows up in a Swedish study that assessed outpatient prescriptions from 2006 to 2010 in a population of 21 492 patients with a schizophrenia diagnosis (Torniainen et al., Reference Torniainen, Mittendorfer-Rutz, Tanskanen, Björkenstam, Suvisaari, Alexanderson and Tiihonen2015). The SMRs were as follows:
No exposure in 5 years: 6.3
Low exposure: 4.1
Moderate exposure: 4.0
High exposure: 5.7
Total cohort: 4.8.
This SMR of 4.8, like the SMR of 4.5 in the first-episode Finnish patients, is notably higher than the mortality ratios for schizophrenia patients in the 1970s–1990s. Saha and colleagues warned in their 2007 report that mortality rates would likely continue to rise in the era of second-generation antipsychotics because of their adverse metabolic effects, and at least in the case of these two studies, that is the case (Table 2). A 2010 review similarly concluded that ‘the disparity in mortality outcomes for people with mental illness is increasing’ (Lawrence, Kisely, & Pais, Reference Lawrence, Kisely and Pais2010).
Table 2. All-cause mortality among the seriously mentally ill: 1970s to 2010

There is one final SMR comparison that can be made. In the 2013 UK study, researchers reported that the adjusted SMR for schizophrenia patients who did not take antipsychotic mediation was 1.9 (Murray-Thomas et al., Reference Murray-Thomas, Jones, Patel, Brunner, Shatapathy, Motsko and Van Staa2013). That was less than half the SMR in the studies that are cited as providing evidence that these medications protect against early death.
Conclusion
As can be seen in this review, there is reason to worry that antipsychotics contribute to the mortality gap among the seriously mentally ill. The adverse effects of this class of drugs—weight gain, diabetes, lipid abnormalities, and so forth—are known to increase the risk of early death.
At the same time, the evident limitations of the database studies, including the way data were presented in the published articles, undercut the conclusion that is now being told to the public, which is that research has shown that antipsychotics ‘halve mortality rates.’
What can be concluded is that mortality rates for psychotic patients treated with the current paradigm of antipsychotic-centered care remain high, and are possibly growing worse. What is needed now are studies that compare mortality rates with different paradigms of care, one that emphasizes regular use of antipsychotics and one that minimizes their use. The Open Dialogue study was the first step toward such research.
The Finnish studies are being cited as evidence for maintaining patients diagnosed with schizophrenia on antipsychotics indefinitely. Such treatment, it is said, lowers mortality rates. But this review shows that there is reason to worry that an antipsychotic-centered paradigm of care is elevating mortality rates for those with psychotic disorders, and as such, provides evidence for rethinking paradigm of care.
Acknowledgements
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflict of interest
The author is president of Mad in America Foundation, a non-profit organization that publishes a webzine on psychiatry and its treatments, Madinamerica.com. He did not receive any financial grant or support to write this article.








