Between 1998 and 2016, the suicide rate in the USA increased by 32% (Curtin, Warner, & Hedegaard, Reference Curtin, Warner and Hedegaard2016) and between 2004–2005 and 2012–2013 the recent suicide attempt rate increased by 27% (Olfson et al., Reference Olfson, Blanco, Wall, Liu, Saha, Pickering and Grant2017). Some literature suggests that the prescription opioid crisis has contributed to the increase in suicidal behavior (Bohnert & Ilgen, Reference Bohnert and Ilgen2019; Kegler, Stone, & Holland, Reference Kegler, Stone and Holland2017). The opioid crisis in the USA started around 1997 and was characterized by a two-fold increase in the rate of long-term use of opioids to treat non-cancer pain from 1997 to 2005 (Boudreau et al., Reference Boudreau, Von Korff, Rutter, Saunders, Ray, Sullivan and Weisner2009). From 1999 to 2016 the nation experienced a 340% increase in prescription opioids fatal overdoses (Hedegaard, Warner, & Miniño, Reference Hedegaard, Warner and Miniño2017).
The prescription opioid crisis may have influenced suicidal behavior by increasing the number of individuals with suicidal ideation/behavior, through the effects that the continuous use opioids and opioid use disorder have on the reward system (Garland, Froeliger, Zeidan, Partin, & Howard, Reference Garland, Froeliger, Zeidan, Partin and Howard2013; Hyman, Malenka, & Nestler, Reference Hyman, Malenka and Nestler2006). As the reward system is altered by external opioids, individuals may become gradually insensitive to rewarding experiences with a need for higher opioid doses to achieve prior levels of psychological well-being (Garland, Hanley, Thomas, Knoll, & Ferraro, Reference Garland, Hanley, Thomas, Knoll and Ferraro2015; Hyman et al., Reference Hyman, Malenka and Nestler2006). Continuous use of opioids can result in loss of control over opioid use despite the social and health problems it causes, and social and occupational activities being neglected, all central characteristics of opioid use disorder (APA, 2013). Emotional pain and distress experienced during withdrawal periods can also result in a cascade of events that increases the levels of neuropeptides involved in maintaining negative mood states (Koob & Le Moal, Reference Koob and Le Moal2001; Striebel & Kalapatapu, Reference Striebel and Kalapatapu2014). Opioid withdrawal has been characterized by states of severe dysphoria (Hyman et al., Reference Hyman, Malenka and Nestler2006), and continuous use of a prescription opioid is associated with a high risk of depression (Scherrer et al., Reference Scherrer, Svrakic, Freedland, Chrusciel, Balasubramanian, Bucholz and Lustman2013). Further, disinhibition effects of opioids could increase the risk of individuals with suicidal thoughts, whether or not linked to depressive states, acting on these impulses (Ilgen et al., Reference Ilgen, Bohnert, Ganoczy, Bair, McCarthy and Blow2016). Moreover, those with opioid use disorder may face social discrimination and financial challenges that can trigger feelings of failure and despair and eventually suicidal behavior.
The link between the use of prescription opioids and suicidal symptoms in non-clinical settings is supported by evidence from epidemiologic surveys (Ford & Perna, Reference Ford and Perna2015; Kuramoto, Chilcoat, Ko, & Martins, Reference Kuramoto, Chilcoat, Ko and Martins2012; Zullig, Divin, Weiler, Haddox, & Pealer, Reference Zullig, Divin, Weiler, Haddox and Pealer2015). Cross-sectional studies indicate that nonmedical use of prescription opioids is associated with a two-fold increased risk of suicidal thoughts among adolescents (Zullig et al., Reference Zullig, Divin, Weiler, Haddox and Pealer2015) and a 1.4-to two-fold risk of suicidal thoughts in adults (Ford & Perna, Reference Ford and Perna2015; Kuramoto et al., Reference Kuramoto, Chilcoat, Ko and Martins2012). Although these studies controlled for the effects of some important factors that could explain the association between opioid use and suicidal outcomes, lack of control for psychiatric disorders or adverse childhood experiences could partially explain their findings. In addition, because measures of opioid use and suicidal outcomes are usually obtained for the same period (e.g. past year), it is difficult to assess the temporal relationship between opioid use and suicidal behavior in these studies. Further research attending to temporality and improved control for important covariates would provide a more robust test of the hypothesis that nonmedical opioid use contributes to the risk of suicidal symptoms.
The objective of this study was to test whether the nonmedical use of prescription opioids, the heavy/frequent use of prescription opioids, and related disorder were associated with subsequent suicidal ideation and attempts. We tested these associations in a national longitudinal representative sample of the US population. The results of this study can shed light on one of the potential factors contributing to the recent increase in the rate of suicide deaths. This information can be used in harm reduction and substance use disorder treatment programs with the goal of treating opioid use disorder and preventing suicidal behavior.
Methods
Participants and procedures
We used data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), a nationally representative sample of US adults ages 18 years and older, residing in households and non-institutional group quarters (e.g. college quarters and boarding houses). In wave 1 (2001–2002), interviews were conducted with 43 093 participants by experienced lay interviewers with extensive training and supervision (Grant et al., Reference Grant, Stinson, Dawson, Chou, Ruan and Pickering2004b; Grant, Kaplan, Shepard, & Moore, Reference Grant, Kaplan, Shepard and Moore2003). The response rate in wave 1 was 81%. Wave 2 was conducted approximately 3 years after wave 1 (mean interval, 36.6 months). After exclusion of wave 1 respondents who were institutionalized, were deported or who had died, 34 653 participants were re-interviewed (86.7%) (Hasin & Grant, Reference Hasin and Grant2015). The US Census Bureau and US Office of Management and Budget approved all protocols and study consent procedures. Participants gave written informed consent and were compensated for participation.
Measures
Figure 1 describes the wave of measure assessments and the period they cover. The outcome is any suicidal event since the last interview measured at wave 2; the exposure is any nonmedical prescription opioid use in the 12 months prior to the interview at wave 1, and the confounders are events occurring before the exposure period.

Fig. 1. Study design using NESARC wave 1 and wave 2 data.
Exposure variables
Nonmedical use of prescription opioids was assessed with the Alcohol Use Disorder and Associated Disabilities Schedule (AUDADIS-IV) (Grant, Harford, Dawson, Chou, & Pickering, Reference Grant, Harford, Dawson, Chou and Pickering1995; Ruan et al., Reference Ruan, Goldstein, Chou, Smith, Saha, Pickering and Grant2008). The test-retest reliability of the opioid use measure in AUDADIS achieved a κ of 0.66 (Grant et al., Reference Grant, Harford, Dawson, Chou and Pickering1995). Respondents were queried regarding use of prescription opioids either without a doctor's prescription, in greater amounts, more often, or longer than prescribed, or for a reason other than a doctor said the person should use them. Participants were also asked whether they used prescription opioids in this manner in the last 12 months.
We evaluated dose-response using a measure of past-year heavy/frequent nonmedical prescription opioid use based on the number of days they used prescription opioids in the past year, categorized as (1) heavy/frequent users (2–3 times a month or more); (2) infrequent (⩽1/month) and 3) non-users (0 in the past year).
We also used a measure of prescription opioid use disorder (POUD) in the past year based on AUDADIS-IV module (Grant et al., Reference Grant, Harford, Dawson, Chou and Pickering1995; Ruan et al., Reference Ruan, Goldstein, Chou, Smith, Saha, Pickering and Grant2008). The test-retest reliabilities of AUDADIS-IV drug abuse and dependence measures have been shown to be excellent (Kappa coefficients above 0.79) (Grant et al., Reference Grant, Stinson, Dawson, Chou, Dufour, Compton and Kaplan2004a).
Outcomes
We examined the prevalence and incidence of suicidal ideation and attempt. Based on prevalence, we evaluated whether exposure at wave 1 was associated with persistence/recurrence and onset of suicidal ideation/attempts at wave 2. Based on incidence, we evaluated whether the exposure was associated with the onset of suicidal ideation/attempts (i.e. developing these outcomes). Note that incidence is based on participants who had not experienced suicidal outcomes before the wave 1 assessment.
Prevalence of suicidal ideation and suicide attempts
In wave 2, respondents were asked about suicidal ideation and suicide attempts since the last interview; however, this was restricted to those screened into the depression module in the NESARC by answering ‘yes’ to either the depressed mood or anhedonia items. Participants screened into the depression module were asked: ‘During that time since your last interview when (your mood was at its lowest/you enjoyed or cared the least about things), did you think about committing suicide? Did you attempt suicide?’ Respondents were coded as having suicidal ideation if they responded ‘yes’ to the first question. Respondents were also coded as making a suicide attempt if saying ‘yes’ to the second question.
Incidence of suicidal ideation and suicide attempts
We used measures of lifetime suicidal ideation and suicide attempts from wave 1 to restrict additional analyses to those without a history of suicidal ideation (91.1%) and suicide attempts (97.3%) in wave 1. Suicidal items from waves 1 and 2 were similar.
To evaluate how the nesting of the suicide ideation item within the depression module might bias results, in sensitivity analyses we used information from additional questions on ‘ever attempt suicide’ and also the ‘age at the most recent attempt’ that were asked to all participants at wave 2.
Other covariates
Models were adjusted for covariates (potential confounders) that could explain the association between prescription opioids and suicidal outcomes. All measures, except where noted, are from NESARC wave 1 and correspond to events or problems experienced 12 months prior to the wave 1 interview. A detailed description of covariates is shown in online Supplemental Table S1.
The AUDADIS-IV module (Grant et al., Reference Grant, Harford, Dawson, Chou and Pickering1995; Ruan et al., Reference Ruan, Goldstein, Chou, Smith, Saha, Pickering and Grant2008) was used to classify participants by DSM-IV criteria for mood and personality disorders; social deviance before and after age 15 (based on number of symptoms of conduct or antisocial personality); and substance use and substance use disorder prior to the last 12 months. We also used a measure of low self-esteem (online Supplemental Table S1).
Childhood adversity included the following binary measures: lifetime history of depressive events and drug disorder in blood/natural parents; drug disorder in any full brothers/sisters; behavior problems in blood/natural parents; parental divorce/separation or death of at least one parent before age 18 years; and history of suicide attempts among parents/adults living in the home before age 18 years.
Socio-demographic variables included: age, sex, and race/ethnic group and history of the end of marriage (first marriage separation, divorce, or death of a partner). We also included measures of current total family income, health insurance coverage, and marital status at wave 1. In addition, we included measures of past/current use of medicine/drugs to improve mood. Because these are measures occurring in the exposure period, it is possible that they represent pathways through which opioid use could lead to suicidal outcomes (e.g. opioid use can lead to divorce, which can lead to suicidal ideation). Adjusting for these covariates could result in removing some of the effects that prescription opioid use and POUD had on suicidal ideation/attempts through these mechanisms. Therefore, we present results from models with (Table 1b) and without these covariates (online Supplemental Table S4).
Table 1. Past-year nonmedical use of prescription opioids, heavy/frequent use of nonmedical prescription opioids and related disorder at wave 1 and their association with prevalence and incidence of suicidal ideation and suicide attempts since last interview (wave 2) in adjusted and unadjusted modelsa
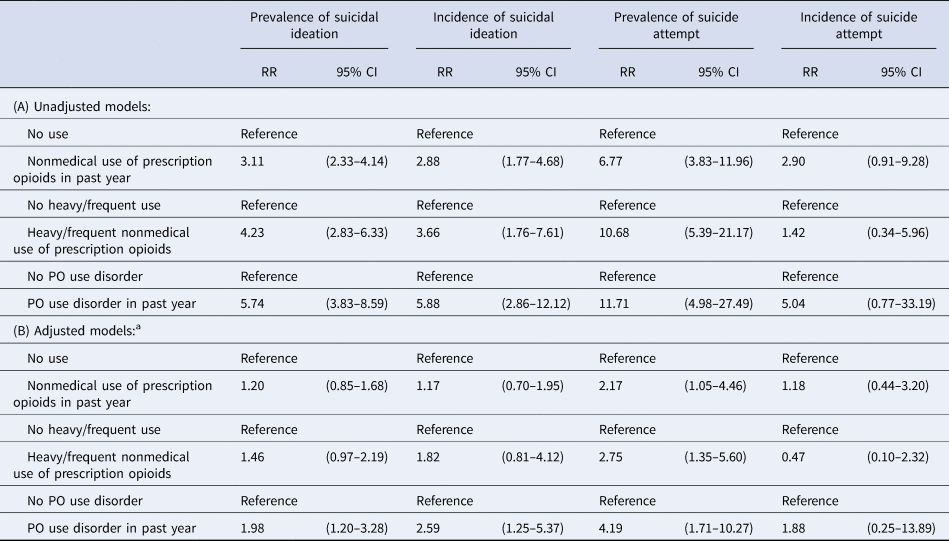
a Models were adjusted by the log transformed propensity score that included the following variables: Marital status, family income, type of insurance, having used medication as directed by physician to improve mood (ever in life), having used medication not as directed by physician to improve mood, respondent's age, sex, and race/ethnic group; history of marriage ending (separated/divorced/widowed); mood and personality disorders experienced before age 18; low self-esteem; other substance use prior to past year before interview; substance use disorder prior to past year before interview; social deviance before and after age 15; lifetime history of depressive events among blood/natural parents; lifetime history of drug use disorders in blood/natural parents; lifetime history of drug use disorders in any full brothers/sisters; parental divorce/separation or death of at least one parent before the participant was 18 years old; family history of behavior problems in blood/natural parents; history of suicide attempts among parents or other adults living in home before the participant was 18 years old.
Analyses
To estimate the association between prescription opioid use and POUD on suicidal ideation/attempts, we used generalized linear models with a logarithm link function and a Poisson distribution. First, we calculated the crude and then the adjusted estimates of these associations. We calculated the population Average Treatment Effect on the Treated (ATT) (Dugoff, Schuler, & Stuart, Reference Dugoff, Schuler and Stuart2014; Williamson, Morley, Lucas, & Carpenter, Reference Williamson, Morley, Lucas and Carpenter2012) for each exposure. The ATT was estimated by including the log-transformed propensity score centered at the mean of the exposed (e.g. those with POUD), plus adding an interaction term between the exposure and the log-transformed propensity score (Williamson et al., Reference Williamson, Morley, Lucas and Carpenter2012).
For each exposure of interest, we calculated a propensity score predicting the probability of being exposed in logit models with each exposure as the dependent variable and a set of covariates as independent variables (D'Agostino, Reference D'Agostino1998; Oakes & Johnson, Reference Oakes, Johnson, Oakes and Kaufman2006; Rosenbaum & Rubin, Reference Rosenbaum and Rubin1983; Williamson et al., Reference Williamson, Morley, Lucas and Carpenter2012). For the propensity score prediction, we included only variables that were associated, in univariate analyses, with the exposures and the outcomes at a p value of ⩽0.2 (Greenland & Mickey, Reference Greenland and Mickey1989). Because the distribution of the propensity score was skewed to the right, we log-transformed the propensity score (Rosenbaum & Rubin, Reference Rosenbaum and Rubin1985). The balance of covariates among exposed and unexposed individuals was checked in separate logit models with the exposure as the independent variable and each covariate and the log-transformed propensity score as independent variables. There was no remaining significant association between any of the covariates and the exposures (online Supplemental Table S2).
To handle missing data, all analyses were conducted using 5 sets of imputed data. Imputation was conducted using switching regression, an iterative multivariable regression technique, in STATA 14. Percentages missing were 0.5% for any nonmedical use of prescription opioids, 0.04% for heavy/frequency of use of opioids, and 0.5% for both suicidal ideations and for suicidal attempt since last interview measures. Most variables had <1% missing data. The variables with maximum missing were those used to create measures of history of family drug use, family history of depression and of antisocial personality disorder (range: 2.7–15.0%). All analyses were conducted in STATA 14 (StataCorp, 2015) accounting for the complex survey design features of the NESARC survey and combining results from the 5 imputed datasets.
Results
The prevalence of past-year nonmedical use of prescription opioids was 1.78%; 0.62% of participants were heavy/frequent opioid users, and 0.33% meet criteria for past-year POUD at wave 1. Also, 8.51% had a history of lifetime suicidal ideation at wave 1, and 2.38% a history of suicide attempts at wave 1; 3.56% of participants endorsed having suicidal thoughts at wave 2, and 0.64% endorsed having attempted suicide since last interview at wave 2.
Prescription opioid use and suicidal outcomes
Individuals with past-year nonmedical use of prescription opioids, compared to those without such use, had a higher prevalence of suicidal ideation (10.66% v. 3.43%) and suicide attempts (3.91% v. 0.58%) since last interview (online Supplemental Table S3). Prevalence of suicidal outcomes at wave 2 among those with heavy/frequent use of opioids and POUD was higher than among those with any past-year nonmedical use of prescription opioids (online Supplemental Table S3).
Unadjusted association between prescription opioid use and suicidal outcomes
Nonmedical use of prescription opioids and POUD were associated with greater prevalence and onset of suicidal ideation and a greater prevalence of suicide attempt (Table 1a). There was a dose-response pattern with a higher risk for POUD followed by heavy/frequent use of prescription opioids. In all associations between each exposure and the outcome onset of suicide attempts the 95% CI were wide and included the null value.
Adjusted associations between prescription opioid use and suicidal outcomes
We found a reduction in the magnitude of crude risk ratios after adjusting for the propensity score (Table 1b). The largest reduction was for the association between heavy/frequent use of prescription opioids and prevalence of suicide attempts, with the change in the magnitude of the risk ratio from 10.68 to 2.75. Despite this reduction, strong associations remained between each exposure and prevalence of suicide attempts.
POUD was associated with prevalence (ARR = 1.98, 95% CI 1.20–3.28) and onset (ARR = 2.59, 95% CI 1.25–5.37) of suicidal ideation. Although not significant, the range of effects sizes suggested that heavy/frequent use of opioids was linked to the prevalence of suicidal ideation (ARR = 1.46, 95% CI 0.97–2.19). In associations between any past-year nonmedical use of prescription opioids and prevalence of suicidal ideation and onset of suicidal ideation the 95% confidence intervals included the null value. This was also the case for all associations between each exposure and incidence of suicide attempts.
Sensitivity analyses
Results were robust in models not adjusted by current family income, marital status, medical insurance at wave 1, and past/current use of medicine/drugs to improve mood (online Supplemental Table S4). Also, no major changes were observed in sensitivity analyses after recoding individuals who were not screened into the depression module but who had endorsed attempting suicide in questions asked to all participants at wave 2 (Table 2). Fifty-seven individuals who were not screened into the depression module endorsed attempting suicide since the last interview in these questions (two were exposed to any past-year prescription opioid use, and two to POUD).
Table 2. Sensitivity analyses after recoding participants who were not screened into the depression module but endorsed having attempting suicide in additional questions asked to all participantsa
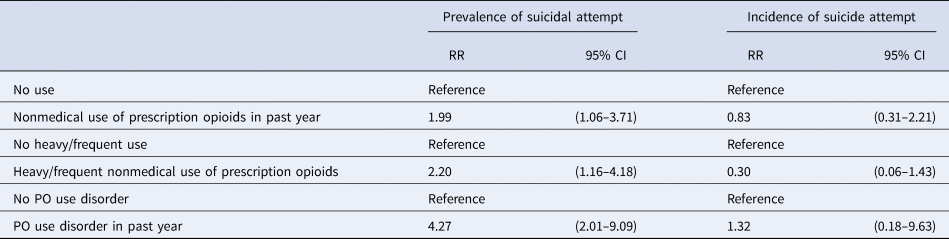
a Models were adjusted by the log transformed propensity score that included the following variables: Marital status, family income, type of insurance, having used medication as directed by physician to improve mood (ever in life), having used medication not as directed by physician to improve mood, respondent's age, sex, and race/ethnic group; history of marriage ending (separated/divorced/widowed); mood and personality disorders experienced before age 18; low self-esteem; other substance use prior to past year before interview; substance use disorder prior to past year before interview; social deviance before and after age 15; lifetime history of depressive events among blood/natural parents; lifetime history of drug use disorders in blood/natural parents; lifetime history of drug use disorders in any full brothers/sisters; parental divorce/separation or death of at least one parent before the participant was 18 years old; family history of behavior problems in blood/natural parents; history of suicide attempts among parents or other adults living in home before the participant was 18 years old.
Discussion
In a longitudinal representative sample of the US adult population, POUD was associated with increased prevalence and onset of suicidal ideation and prevalence, but not onset, of non-fatal suicide attempts. Heavy/frequent use of prescription opioids was also associated with the prevalence of suicidal ideation and of suicidal attempts. Controlling for covariates considerably reduced the magnitude of the crude associations. Even after extensive adjustment, however, most of these associations remained significant. To our knowledge, this is the first large-scale longitudinal study investigating the associations between prescription opioid use/POUD and suicidal outcomes.
A dose-response pattern was observed in the risk of suicidal ideation and attempts. Those with POUD are by definition experiencing symptoms (including problems at work, or with family or friends) related to their drug use and are more likely to use opioids at a higher frequency and in higher doses than occasional users (Gardner, Reference Gardner2011). POUD was associated with a 2.59-fold increase in the risk of the onset of suicidal ideation. Because incidence measures are less likely affected by reverse causation, this finding provides support for the hypothesis of a causal connection between POUD and suicidal ideation. In contrast, there was no evidence for associations with the onset of a suicide attempt. This could be due to the fact that the nonmedical use of opioids may contribute more to persistence/recurrence of suicidal behavior rather than the new onset of attempts. Also, because very few participants had suicide attempts between waves 1 and 2, there was less available power to detect these associations (despite the large sample size in NESARC, only seven and eight participants with prescription opioid use disorder and heavy/frequent use, respectively, endorsed new onset of suicide attempts at wave 2).
Results were robust in models not adjusted by current measures of marital status, family income, health insurance, and use of medicine/drugs to improve mood, with only a slight increase in association estimates. Given that opioid use/POUD can influence some of these measures [e.g. POUD can lead to financial distress and family problems (Center for Substance Abuse Treatment, 2004)], it is possible that in models adjusted by these covariates some of the association between opioid use/POUD and suicidal outcomes through these measures was removed. We believe results from these models are conservative, with the true association likely resting between the results from the two models adjusting/not adjusting by these current measures.
Our findings are more modest than those previously reported between adults with heroin use disorder and suicide deaths (Wilcox, Conner, & Caine, Reference Wilcox, Conner and Caine2004), which could be explained by our focus on a population that used prescription opioids rather than heroin, suicidal ideation/attempts rather than death due to suicide, and our strategy to control for the effects of multiple factors that influence suicidal outcomes.
Our results are in line with other studies showing that those with nonmedical prescription opioid use and PUOD, in addition to being at risk of numerous adverse outcomes, are also at risk for suicidal ideation/behavior (Ford & Perna, Reference Ford and Perna2015; Guo et al., Reference Guo, Xu, Den, Huang, Huang, Gao and Lu2016; Kuramoto et al., Reference Kuramoto, Chilcoat, Ko and Martins2012; Zullig et al., Reference Zullig, Divin, Weiler, Haddox and Pealer2015). They are also in line with clinical research showing that high-dose medical use of these drugs is linked to a higher risk of suicide (Ilgen et al., Reference Ilgen, Bohnert, Ganoczy, Bair, McCarthy and Blow2016). However, recent data (2015–2016) shows that medical use (i.e. opioid use without misuse) has not been found to be strongly related to suicidal ideation (Samples et al., Reference Samples, Stuart and Olfson2019). Whether or not physicians' adherence to recent prescription opioid guidelines (including lower opioids doses) has contributed to reductions in suicidal outcomes among medical opioid users remains unknown.
Overall, our findings support the hypothesis that frequent/heavy use of prescription opioids and POUD contribute to the risk of suicidal ideation/attempts. This is important as it is estimated that in the USA in 2016 around 1.6 million adults met criteria for prescription opioid use disorder (SAMHSA, 2017). If the risk of suicidal ideation and attempts in these exposed groups remain similar to date and assuming there are similar to our estimates from the 2004–2005 period, we estimate that annually approximately 322 000 individuals with POUD would experience suicidal ideation and 115 000 suicide attempts nationwide.
These findings have implications for suicide prevention efforts. The results revealed that both heavy opioid use and POUD were associated with suicidal ideation and suicide attempts. Therefore, providing access to evidence-supported treatments, such as opioid agonist treatments, that reduce opioid use among people with heavy opioid use and POUD (Mattick, Breen, Kimber, & Davoli, Reference Mattick, Breen, Kimber and Davoli2014; Volkow, Frieden, Hyde, & Cha, Reference Volkow, Frieden, Hyde and Cha2014; Yovell et al., Reference Yovell, Bar, Mashiah, Baruch, Briskman, Asherov and Panksepp2016), might help prevent future suicidal events and reduce suicidal ideation. Screening for suicide risk and continuous monitoring of those with heavy or frequent medical or nonmedical use of opioids and POUD might help to identify and provide appropriate treatment to a high-risk group. These findings also align with previous work indicating that associations between POUD and suicidal outcomes are related to mental health problems, adverse life experiences and use of other medicine/drugs, elements that should also be addressed in therapy with the goal of preventing suicidal behaviors.
Limitations are noted. Although we controlled analyses for several important covariates, it is possible that residual confounding (e.g. other traumatic experiences or psychiatric conditions) explains our findings. A single item assessed suicidal ideation and another item suicide attempts, which can cause misclassification of the outcome (Hom, Joiner, & Bernert, Reference Hom, Joiner and Bernert2016; Millner, Lee, & Nock, Reference Millner, Lee and Nock2015). These questions are part of the depression module of a fully structured interview, which likely improved their validity. Self-report of exposure, outcome and confounders may have led to misclassification with correlated errors, likely inflating the magnitude of associations. Fatal suicide attempts in the sample, and also the fact that NESARC excludes inmate populations that have high rates of opioid use and suicidal behavior (Stoliker, Reference Stoliker2018) could have introduced bias. Censoring of participants interview at wave 1 who died by suicide could introduce bias if these participants were more likely to be non-opioid users and died by means unrelated to opioids. Assuming that 20 participants, based on a national suicide rate of 14 per 100 000 people, were censored, we find that adding these 20 participants to the cell of non-opioid users who attempt suicide (13 out of 202 of heavy prescription opioid users attempted suicide at wave 2, and 222 out of 33 894 non-opioid users attempted) would have slightly reduced the association from an unadjusted RR = 9.2 to RR = 8.5. Also, the absence of information on adolescents prevented us from analyzing these associations in young people. Suicidal ideation/attempts questions were only asked to participants screened into the depression module, which can result in false negatives. However, results from sensitivity analyses were overall robust after recoding participants not screened into the depression module. The fact that there was a slight reduction in the magnitude of associations in sensitivity analyses suggest that some people, mostly non-opioid users at wave 1, may develop suicidal outcomes through alternative mechanisms that do not include depression (e.g. suicide among those with impulsive traits). Future research examining these associations should measure suicidal outcomes in all participants. Although we used prospective data, the assessments were 3 years apart precluding assessment of longer- and shorter-term associations. Because NESARC data used in this study are from 2001–2002 to 2004–2005 further assessment with data reflecting the most recent nonmedical use of prescription opioids, POUD and suicidal ideation/behavior would be important to evaluate whether these associations have remained constant over time. Despite this limitation, NESARC data allowed us to examine the link between nonmedical prescription opioid use and suicidal outcomes during a period when the USA was already 5 years into the opioid epidemic.
Conclusions
We found evidence supporting the hypothesis of the influence of POUD on prevalent suicidal ideation and attempts, and also the subsequent onset of suicidal ideation. The range of effect sizes also shows evidence that heavy/frequent prescription opioids use may influence prevalent suicidal ideation. Given increases in non-medical use of prescription opioids and related disorder in the USA, the prescription opioid crisis may have contributed to increases in suicidal ideation, and potentially behavior, during the last two decades.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291720002160.
Acknowledgements
We thank Dr Sharon Schwartz for guidance and for providing insightful and constructive comments on previous versions of the manuscript. Support is acknowledged from NIDA R01DA 037866 (Dr Martins) and 1R01DA039962-01 (Dr Cerdá). Dr Santaella-Tenorio was funded by the J. William Fulbright and the Colciencias doctoral scholarships. K. Keyes has received compensation for expert witness consultation in product litigation.
Conflict of interest
K. Keyes has received compensation for expert witness consultation in product litigation.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional guides on the care and use of laboratory animals.






