Introduction
Worldwide, post-traumatic stress disorder (PTSD) has a lifetime prevalence of 3.9% in the general population, and 5.6% among those exposed to trauma (Koenen et al., Reference Koenen, Ratanatharathorn, Ng, McLaughlin, Bromet, Stein and Kessler2017). PTSD is associated with substantial levels of disability, poor quality of life and functional impairment (Alonso et al., Reference Alonso, Angermeyer, Bernert, Bruffaerts, Brugha, Bryson and Vollebergh2004). It is often comorbid with other mental disorders such as depression, anxiety, substance abuse (Kessler, Sonnega, Bromet, Hughes, & Nelson, Reference Kessler, Sonnega, Bromet, Hughes and Nelson1995), and has been associated with numerous physical health difficulties, including cardiovascular and metabolic diseases (Ahmadi et al., Reference Ahmadi, Hajsadeghi, Mirshkarlo, Budoff, Yehuda and Ebrahimi2011).
Several psychological treatments are available for the management of PTSD in adults. Trauma-focused cognitive behavioural therapy (TF-CBT) is a broad class of psychological interventions that predominantly use trauma-focused cognitive, behavioural or cognitive-behavioural techniques and exposure approaches to treatment. Although some interventions place their main emphasis on exposure and others on cognitive techniques, most use a combination. There is considerable overlap in the proposed mechanisms underlying the effectiveness of the various versions of TF-CBT. TF-CBT includes therapies such as cognitive therapy (CT), cognitive processing therapy (CPT), exposure therapy/prolonged exposure, virtual reality exposure therapy, mindfulness-based CT and narrative exposure therapy. Other available treatments for PTSD include eye movement desensitisation and reprocessing (EMDR), interpersonal psychotherapy, present-centred therapy, self-help therapies such as internet-based TF-CBT and expressive writing, counselling, non-TF-CBT, which focuses on current symptoms of PTSD without re-visiting the trauma experience, and combined somatic/cognitive therapies such as emotional freedom techniques and thought field therapy; these are exposure-based therapies with both cognitive and somatic components that utilise the tapping of points on the body (Church et al., Reference Church, Hawk, Brooks, Toukolehto, Wren, Dinter and Stein2013; Robson, Robson, Ludwig, Mitabu, & Phillips, Reference Robson, Robson, Ludwig, Mitabu and Phillips2016).
A number of systematic reviews and meta-analyses have evaluated the effectiveness of psychological treatments for adults with PTSD (Bisson, Roberts, Andrew, Cooper, & Lewis, Reference Bisson, Roberts, Andrew, Cooper and Lewis2013; Cusack et al., Reference Cusack, Jonas, Forneris, Wines, Sonis, Middleton and Gaynes2016; Forman-Hoffman et al., Reference Forman-Hoffman, Middleton, Feltner, Gaynes, Weber, Bann and Green2018; Frost, Laska, & Wampold, Reference Frost, Laska and Wampold2014; Gerger et al., Reference Gerger, Munder, Gemperli, Nüesch, Trelle, Juni and Barth2014; Khan et al., Reference Khan, Dar, Ahmed, Bachu, Adnan and Kotapati2018; Kuester, Niemeyer, & Knaevelsrud, Reference Kuester, Niemeyer and Knaevelsrud2016; Seidler & Wagner, Reference Seidler and Wagner2006; Sijbrandij, Kunovski, & Cuijpers, Reference Sijbrandij, Kunovski and Cuijpers2016; van Emmerik, Reijntjes, & Kamphuis, Reference van Emmerik, Reijntjes and Kamphuis2013). Commonly they find most robust evidence for the efficacy of individual TF-CBT and EMDR, and some evidence for non-TF-CBT, present-centred therapy and self-help. For other interventions (such as combined somatic/cognitive therapies) there has been more limited high quality research that did not always meet the inclusion criteria for these reviews, and therefore no robust conclusions on their effectiveness could be drawn. One review suggested that individual TF-CBT, EMDR and non-TF-CBT are more effective than other therapies for PTSD (Bisson et al., Reference Bisson, Roberts, Andrew, Cooper and Lewis2013). Moreover, there was evidence to suggest superiority of EMDR over TF-CBT (Khan et al., Reference Khan, Dar, Ahmed, Bachu, Adnan and Kotapati2018). However, these findings were not confirmed in another review (Gerger et al., Reference Gerger, Munder, Gemperli, Nüesch, Trelle, Juni and Barth2014). With the exception of one review (Gerger et al., Reference Gerger, Munder, Gemperli, Nüesch, Trelle, Juni and Barth2014), these analyses have made limited comparisons across a narrow range of treatments using standard pairwise meta-analysis to synthesise evidence from randomised controlled trials (RCTs). This approach does not allow for the relative effectiveness across all treatments to be assessed, unless all possible comparisons have been evaluated in head-to-head trials.
Network meta-analysis (NMA) is a generalisation of pairwise meta-analysis to data structures that include, for example, A v. B, B v. C and A v. C trials (Lu & Ades, Reference Lu and Ades2004). NMA strengthens inferences concerning the relative effect of two treatments by including both direct and indirect treatment comparisons. This means that NMA allows estimation of the relative effects of treatments that may not have been directly compared in RCTs. Simultaneous estimation of all relative effects for any number of treatments is possible provided that treatments are connected in a single ‘network of evidence’ – that is, every treatment is linked to at least one of the other treatments under assessment through direct comparisons (Caldwell, Ades, & Higgins, Reference Caldwell, Ades and Higgins2005; Mavridis, Giannatsi, Cipriani, & Salanti, Reference Mavridis, Giannatsi, Cipriani and Salanti2015).
The objective of this study was to examine the relative effectiveness of psychological treatments for PTSD in adults using NMA techniques. The analyses presented here supported the updating of national guidance for PTSD in England (National Institute for Health and Care Excellence, 2018a). The guideline was developed by a guideline committee, an independent multi-disciplinary group of clinical academics, health professionals and service user and carer representatives with expertise and experience in the field of PTSD.
Methods
Search strategy
A search for RCTs of treatments for people with clinically important post-traumatic stress symptoms was conducted in the following databases: MEDLINE, Embase, PsycINFO, CINAHL and The Cochrane Library. Databases were searched using relevant medical subject headings, free-text terms and a study design filter. The aim of the search was to update evidence included in the previous National Institute for Health and Care Excellence (NICE) PTSD guideline, published in 2005. The search was undertaken in January/February 2017 with re-runs performed in January 2018. Online Supplementary Appendix 1 provides full details of the databases and search terms used. The reference lists of all relevant systematic reviews were hand-searched for any additional eligible studies. Clinical trial registries (ISRCTN and ClinicalTrials.gov) were also searched to identify any relevant unpublished trials and authors were contacted to request study reports (where these were not available online). Primary authors of published included studies were also contacted to request outcome data where these could not be extracted.
Selection criteria for the systematic review and the network meta-analysis
A systematic review of psychological, psychosocial and other non-pharmacological interventions targeted at clinically important post-traumatic stress symptoms in adults more than 1 month after a traumatic event was carried out in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines (Moher, Liberati, Tetzlaff, & Altman, Reference Moher, Liberati, Tetzlaff and Altman2009). Eligible populations included adults with either a diagnosis of PTSD according to the Diagnostic and Statistical Manual of Mental Disorders (DSM), the World Health Organization (WHO) International Classification of Diseases (ICD) or similar criteria, or with the presence of clinically significant PTSD symptoms, as indicated by baseline scores above a pre-defined threshold on a validated PTSD symptom scale. If some, but not all, of a study's participants had clinically important PTSD symptoms, the study was included if at least 80% of participants had clinically important PTSD symptoms or if disaggregated data only for those with PTSD could be extracted from the paper. If less than 80% of the participants had clinically important PTSD symptoms, or if disaggregated data only for those with PTSD were not available, then the mean baseline PTSD symptom score was used and a study was included in the review if this mean was above a pre-defined clinical threshold. Primary outcomes for the review included PTSD symptom endpoint or change scores on a validated PTSD scale; response to treatment; and recovery or remission defined either as the number of people no longer meeting diagnostic criteria for PTSD, or with PTSD symptom scores below the threshold on a validated scale.
For quality assurance of study identification, and in accordance with NICE guidance (National Institute for Health and Care Excellence, 2014), the titles and abstracts of identified studies were screened by two reviewers against inclusion criteria specified in the guideline review protocols until a good inter-rater reliability was observed (percentage agreement ⩾90%). Initially, a random 10% of references were double-screened and inter-rater agreement was good; therefore, the remaining references were screened by one reviewer. All primary-level studies included after the first citation scan were acquired in full and re-evaluated for eligibility at the time of being entered into a study database (standardised template created in Microsoft Excel). At least 10% of data extraction (including data informing the risk of bias assessment) was double-coded. Discrepancies or difficulties with coding were resolved through discussion between reviewers or the opinion of a third reviewer was sought. Data were extracted on study characteristics, intervention details, outcome data and risk of bias.
For the NMA, we considered only first-line psychological treatments offered to adults with a diagnosis of PTSD or clinically important post-traumatic stress symptoms more than 3 months after trauma. Pharmacological and combined psychological and pharmacological treatments that were linked in the treatment network were also considered. Hypnotherapy, psychosocial interventions (meditation, mindfulness-based stress reduction, supported employment, peer and practical support) and physical interventions (exercise, yoga, acupuncture, bio-neuro-feedback and repetitive transcranial magnetic stimulation) were not included in the analysis as they were not considered to be alternative, first-line treatments for the management of PTSD in adults. Relaxation was included as a control intervention that provided additional indirect comparisons across interventions of interest.
Interventions in the TF-CBT class were not considered separately according to their type. Although the specific interventions that make up a class do not include exactly the same content or follow the same manual, they use the same broad approach and there is a considerable overlap in the proposed mechanisms; the efficacy of interventions within the class was therefore considered to be equivalent. Hence, in the analyses presented here, TF-CBT is considered as an umbrella term and forms one node in the network. For the analyses that informed the NICE clinical guideline on PTSD, we divided the TF-CBT class by number of sessions and format of delivery and created different nodes in the network according to the intensity of TF-CBT, as these differences in resource use comprised practical considerations that informed the guideline economic analysis, and, subsequently, practice recommendations.
The guideline systematic review included two categories of RCTs: those that compared interventions or their combinations delivered as the sole treatment in a trial arm v. waitlist or another inactive control or active intervention; and those comparing interventions added to treatment as usual (TAU) v. TAU alone or v. an inactive control added to TAU or v. another active intervention added to TAU. The definition of TAU varied widely across studies, including minimum contact comparison, a mixture of psychoeducation and supportive counselling, medication, substance misuse treatment, any treatment outside the research setting or any treatment except the intervention assessed in the study. To reduce heterogeneity attributable to the diversity of TAU across RCTs, comparisons involving TAU alone or combined with a control or with an intervention of interest were not included in the NMA even if they provided links in the network.
The NMA considered two outcomes: PTSD symptom change scores and remission. Data on these outcomes were mostly reported at treatment endpoint. Moreover, a number of studies reported data on one or both of these outcomes at 1–4-month follow-up. PTSD symptom change scores between baseline and 1–4-month follow-up were adequate to inform an NMA; in contrast, remission data at 1–4-month follow-up were very sparse (the network only included 10 studies, 7 interventions and 572 participants; the only active intervention that had been tested on more than 100 participants was TF-CBT). Beyond 1–4 months of follow-up, available data were very sparse for both outcomes. Based on the availability of data for the two outcomes of interest, three separate NMAs were conducted on the following outcomes and time points:
• PTSD symptom change scores between baseline and treatment endpoint
• PTSD symptom change scores between baseline and 1–4-month follow-up
• Remission at treatment endpoint
If both were available in the same study, PTSD symptom change scores derived from self-rated symptom scales were prioritised over those derived from clinician-rated symptom scales, because the former were deemed to better capture symptoms experienced by adults with PTSD, according to the NICE guideline committee. Similarly, intention-to-treat (ITT) data, obtained after imputation of missing data, were prioritised over completer data, if both were available in the same study.
The guideline study protocol was published on the NICE website during consultation of the draft guidance with registered stakeholders (https://www.nice.org.uk/guidance/ng116/history). The systematic review protocol and the additional inclusion criteria applied for the NMA are provided in online Supplementary Appendix 2.
Statistical analysis
NMAs were conducted within a Bayesian framework using a generalised linear model approach (Dias, Sutton, Ades, & Welton, Reference Dias, Sutton, Ades and Welton2013a), estimated using Markov Chain Monte Carlo simulation techniques implemented in WinBUGS 1.4.3 (Lunn, Thomas, Best, & Spiegelhalter, Reference Lunn, Thomas, Best and Spiegelhalter2000; Spiegelhalter, Thomas, Best, & Lunn, Reference Spiegelhalter, Thomas, Best and Lunn2003). An overview of the approach and methods adopted is provided below. Details of the statistical analysis and WinBUGS codes used to synthesise changes in PTSD symptom scores and dichotomous remission data are reported in online Supplementary Appendix 3.
For the synthesis of continuous data (changes in PTSD symptom scores), a linear model with a normal likelihood and identity link was used (Dias, Ades, Welton, Jansen, & Sutton, Reference Dias, Ades, Welton, Jansen and Sutton2018). Because the RCTs included in the NMAs used different continuous scales to report change in PTSD symptoms, relative effects were expressed in the form of the standardised mean difference (SMD) between pairs of interventions. For the synthesis of dichotomous data (remission), a linear model with binomial likelihood and logit link was used (Dias et al., Reference Dias, Sutton, Ades and Welton2013a, Reference Dias, Ades, Welton, Jansen and Sutton2018). The output of this analysis was the set of log-odds ratios (LORs) between all pairs of interventions. The suitability of fixed and random effects models in terms of model fit was assessed and compared, and the most suitable model (fixed or random effects) was then selected for the analysis of each outcome.
For each analysis we report posterior mean relative effects (either SMD or LOR) with 95% credible intervals (CrI). We also report posterior mean ranks with 95% CrI for every treatment tested on at least 100 individuals in each analysis, where a rank of 1 indicates highest effectiveness. We only included interventions tested on at least 100 people in the ranking, as this was deemed the minimum adequate evidence to draw conclusions on effectiveness. Results were interpreted in terms of ‘evidence of effect’, rather than ‘statistical significance’ (Pike, Reference Pike2019), and this was determined based on whether the 95% CrI crossed the line of no effect. Although no cut-off points were used in order to judge the magnitude of effect, in general a SMD value of 0.2–0.3 was deemed to indicate a small effect, a value around 0.5 a medium effect, and a value of 0.8 and above a large effect (Cohen, Reference Cohen1969).
Inconsistency checks
A basic assumption of NMA methods is that direct and indirect evidence estimate the same parameter, that is, the relative effect between A and B measured directly from an A v. B trial is the same as the relative effect between A and B estimated indirectly from A v. C and B v. C trials. In other words, it is assumed that there is agreement between the direct and indirect evidence informing the treatment contrasts [this has also been termed the similarity or transitivity assumption (Mavridis et al., Reference Mavridis, Giannatsi, Cipriani and Salanti2015)]. Inconsistency arises when there is a conflict between direct evidence (from an A v. B trial) and indirect evidence (gained from A v. C and B v. C trials) and can only be statistically assessed when there are closed loops of evidence on three treatments that are informed by at least three distinct trials (van Valkenhoef, Dias, Ades, & Welton, Reference van Valkenhoef, Dias, Ades and Welton2016). The assumption of consistency between indirect and direct evidence was explored by undertaking global inconsistency tests (Dias et al., Reference Dias, Welton, Sutton, Caldwell, Lu and Ades2013b; Dias, Welton, Caldwell, & Ades, Reference Dias, Welton, Caldwell and Ades2010) and local tests through node-splitting (Dias et al., Reference Dias, Welton, Sutton, Caldwell, Lu and Ades2013b; van Valkenhoef & Kuiper, Reference van Valkenhoef and Kuiper2016). When evidence of inconsistency was found, studies contributing to loops of evidence where there might be inconsistency were checked for data accuracy. Analyses were repeated if corrections in the data extraction were made. If evidence of inconsistency was still present following data corrections, no studies were excluded from the analysis, as their results could not be considered to be less valid than those of other studies solely because of the inconsistency findings; nevertheless, the presence of inconsistency in the NMA was highlighted and results were interpreted accordingly.
Details of the methods used to test inconsistency and the WinBUGS codes of the inconsistency models are provided in online Supplementary Appendix 4.
Pairwise sub-analyses
For the purposes of the NICE clinical guideline, a number of sub-analyses of the pairwise meta-analyses were considered, including sub-analysis by specific intervention type for the TF-CBT comparisons, and sub-analyses by trauma type and multiplicity of index trauma for all interventions. It is beyond the scope of this paper to explore all sub-analyses but for illustrative purposes, exploratory sub-analyses have been conducted by specific TF-CBT intervention, method of analysis (ITT v. modified ITT v. completer) and multiplicity of index trauma (single or multiple) for the TF-CBT v. waitlist comparison for the PTSD symptom change scores between baseline and treatment endpoint outcome. This comparison and outcome were selected as it was the only pairwise meta-analysis with sufficient studies to enable meaningful comparison between subgroups. A sub-analysis by trauma type was not included because there were almost as many trauma types as studies and as such the analysis was not interpretable.
Results
Studies and treatments
The systematic literature search identified 715 studies potentially eligible for the systematic review, 529 of which were excluded. Ninety-six more studies were excluded as they did not meet criteria for the NMA, leaving 90 eligible studies on 22 interventions (including two inactive controls) that reported one or more outcomes of interest (Fig. 1). In 64% of the included studies, the study population comprised adults with a diagnosis of PTSD; in the remaining 36% of the included studies, the study population consisted of adults with clinically significant PTSD symptoms, as indicated by baseline scores above a pre-defined threshold on a validated PTSD symptom scale. The characteristics of included studies are reported in online Supplementary Appendix 5. A list of excluded studies, with reasons for exclusion, is provided in online Supplementary Appendix 6. Online Supplementary Appendix 7 shows the full data included in each NMA.

Fig. 1. Flow diagram of study selection for the systematic review and the NMA.
Risk of bias assessment
All 90 included trials were assessed for risk of bias using the Cochrane risk of bias tool (Higgins et al., Reference Higgins, Alman, Sterne, Higgins and Green2011). Sequence generation and allocation concealment were adequately described in 36 and 29 trials, respectively. All trials were regarded as at high risk of bias for lack of participant and provider masking. In 20 studies, a clinician-rated scale was used, with assessors being unaware of treatment assignment. In seven trials, it was unclear if the assessors were blinded, and in 63 studies a self-rated scale was used meaning that raters were non-blinded but were less likely to have a conflict of interest in terms of detection bias. Attrition was high in 11 trials and unclear in 35 studies. However, we favoured ITT analysis and, for the remission outcome, we conservatively treated drop-outs as failing to remit. Of the studies that reported PTSD symptom change scores, approximately 60% reported ITT data, or ITT data were possible to estimate, with the remaining providing completer data only. Included trials reported a variety of outcomes. Only nine trials were registered on a trials database and reported all listed outcomes. Consequently, most studies were judged as being at high or unclear risk of reporting bias. Other potential biases were identified in seven studies; these included high risk of bias due to potential conflicts of interest or due to methodological limitations not otherwise captured. An overview of the trials' risk of bias assessment is provided in online Supplementary Appendix 8.
NMA model fit statistics
In all NMAs, the random effects model provided a better fit over the fixed effect model and fit the data well. However, the between-trial standard deviation (s.d.), which measures the heterogeneity of treatment effects estimated by trials within contrasts, was high when compared with the size of the intervention effect estimates across all three analyses (posterior median s.d.: 0.93 in the NMA of PTSD changes between baseline and treatment endpoint; 0.59 in the NMA of changes in PTSD symptom scores between baseline and 1–4-month follow-up; 1.05 in the NMA of remission at treatment endpoint).
Details of model fit statistics are provided in online Supplementary Appendix 9.
Inconsistency checks
No evidence of inconsistency between direct and indirect evidence was found in the NMAs of changes in PTSD symptom scores at treatment endpoint and at follow-up. The NMA of remission at endpoint showed evidence of inconsistency between pooled direct and indirect estimates comparing TF-CBT, EMDR and self-help without support. Direct effects in these comparisons were implausibly large and with very wide 95% CrI (e.g. mean LOR of EMDR v. TF-CBT −2.01, 95% CrI −4.01 to −0.01), a finding likely attributable to the small number and size of RCTs involved in these comparisons; indirect/NMA estimates for these comparisons are therefore likely to be more trustworthy.
Results of inconsistency checks are provided in online Supplementary Appendix 10.
Treatment outcomes
Results of the three analyses are presented in Tables 1–3, as posterior mean effects with 95% CrI of each intervention v. waitlist, which served as the reference. In each analysis, interventions have been ordered from the most to the least effective, according to their posterior mean effect v. waitlist. The tables also show the number of participants randomised to each intervention across RCTs included in each analysis, and the number of RCTs that assessed each intervention in each NMA. In each analysis, ranking is provided for all interventions tested on at least 100 individuals.
Table 1. NMA of psychological treatments for PTSD in adults, changes in PTSD symptom scores between baseline and treatment endpoint: interventions, magnitude of evidence base and results

CrI, credible intervals; EMDR, eye movement desensitisation and reprocessing; IPT, interpersonal psychotherapy; SMD, standardised mean difference; SSRI, selective serotonin reuptake inhibitor; TF-CBT, trauma-focused cognitive behavioural therapy.
k, number of RCTs that assessed each intervention; N, number randomised to each treatment across RCTs.
Negative values indicate a better effect for the intervention compared with the reference treatment (waitlist).
Only interventions tested on at least 100 people were considered in ranking.
In bold, effects where the 95% CrI do not cross the line of no effect (SMD = 0).
Table 2. NMA of psychological treatments for PTSD in adults, changes in PTSD symptom scores between baseline and 1–4-month follow-up: interventions, magnitude of evidence base and results
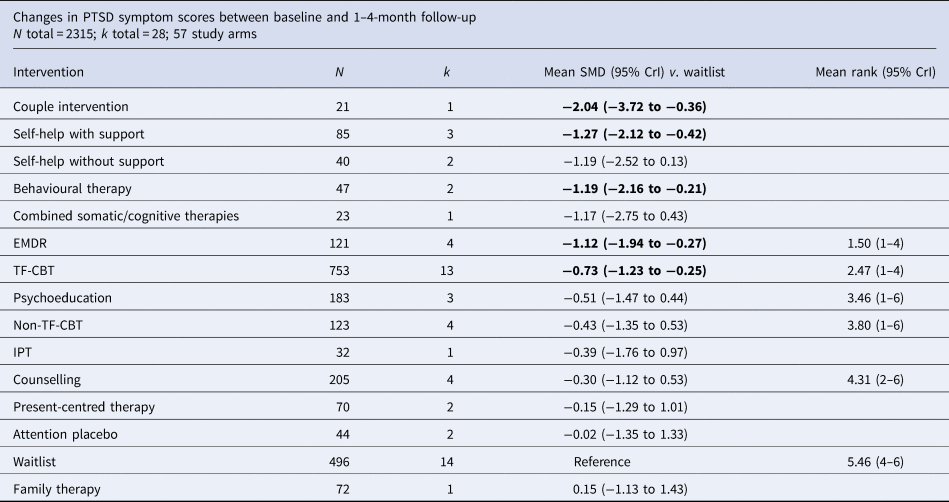
CrI, credible intervals; EMDR, eye movement desensitisation and reprocessing; IPT, interpersonal psychotherapy; SMD, standardised mean difference; TF-CBT, trauma-focused cognitive behavioural therapy.
k, number of RCTs that assessed each intervention; N, number randomised to each treatment across RCTs.
Negative values indicate a better effect for the intervention compared with the reference treatment (waitlist).
Only interventions tested on at least 100 people were considered in ranking.
In bold, effects where the 95% CrI do not cross the line of no effect (SMD = 0).
Table 3. NMA of psychological treatments for PTSD in adults, remission at treatment endpoint: interventions, magnitude of evidence base and results
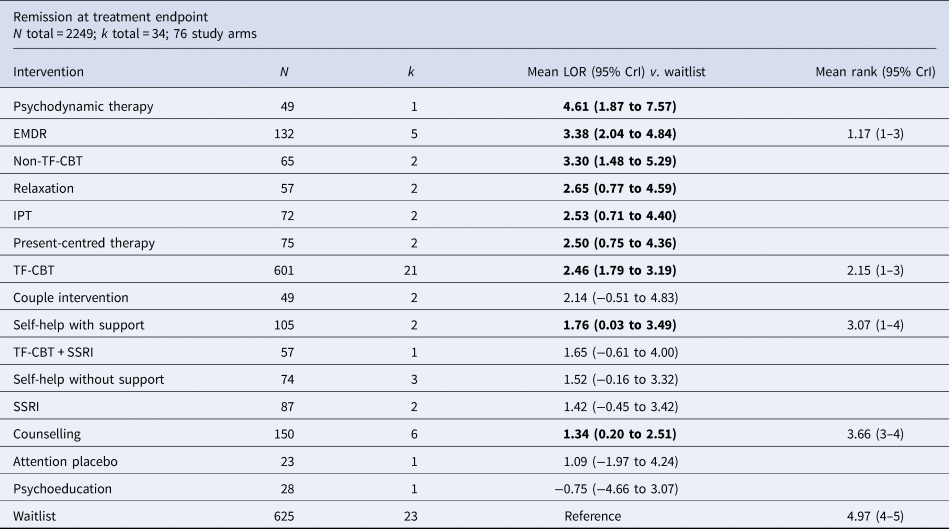
CrI, credible intervals; EMDR, eye movement desensitisation and reprocessing; IPT, interpersonal psychotherapy; LOR, log-odds ratio; SSRI, selective serotonin reuptake inhibitor; TF-CBT, trauma-focused cognitive behavioural therapy.
k, number of RCTs that assessed each intervention; N, number randomised to each treatment across RCTs.
Positive values indicate a better effect for the intervention compared with the reference treatment (waitlist).
Only interventions tested on at least 100 people were considered in ranking.
In bold, effects where the 95% CrI do not cross the line of no effect (LOR = 0).
Changes in PTSD symptom scores between baseline and treatment endpoint
The network of changes in PTSD symptom scores between baseline and treatment endpoint was formed by 71 RCTs with 151 arms that assessed 19 interventions tested on a total of 4700 participants (Fig. 2a). The majority of evidence was on TF-CBT (N = 903 in 29 trials), followed by self-help without support (N = 335 in 11 trials) and EMDR (N = 260 in 11 trials). There was also good- or moderately good-sized evidence on counselling (N = 278 in 9 trials), non-TF-CBT (N = 209 in 7 trials), self-help with support (N = 198 in 5 trials), combined somatic/cognitive therapies (N = 237 in 4 trials), selective serotonin reuptake inhibitors (SSRIs) (N = 166 in 5 trials), psychoeducation (N = 152 in 2 trials) and TF-CBT combined with SSRIs (N = 115 in 3 trials). All other interventions were tested on fewer than 100 participants each. Of the 71 trials, 26 recruited participants with a single trauma and 38 recruited participants with multiple traumas; the remaining seven studies did not report this kind of information.

Fig. 2. Networks of interventions for adults with PTSD. The width of lines is proportional to the number of trials in which each direct comparison is made. The size of each circle (treatment node) is proportional to the number of people who received each treatment. (a) Changes in PTSD symptom scores between baseline and treatment endpoint. (b) Changes in PTSD symptom scores between baseline and 1–4-month follow-up. (c) Remission at treatment endpoint.
For interventions tested on N ⩾ 100 each with evidence of effect v. waitlist (i.e. 95% CrI that did not cross the line of no effect), the ranking (from the most to the least effective) was as follows: EMDR (mean SMD v. waitlist −2.07, 95% CrI −2.70 to −1.44), combined somatic/cognitive therapies (mean SMD v. waitlist −1.69, 95% CrI −2.66 to −0.73), TF-CBT (mean SMD v. waitlist −1.46, 95% CrI −1.87 to −1.05), self-help with support (mean SMD v. waitlist −1.46, 95% CrI −2.33 to −0.59), non-TF-CBT (mean SMD v. waitlist −1.22, 95% CrI −1.95 to −0.49), TF-CBT combined with a SSRI (mean SMD v. waitlist −1.21, 95% CrI −2.35 to −0.07), SSRIs (mean SMD v. waitlist −1.14, 95% CrI −2.09 to −0.19), self-help without support (mean SMD v. waitlist −0.91, 95% CrI −1.67 to −0.15) and counselling (mean SMD v. waitlist −0.73, 95% CrI −1.41 to −0.05) (Table 1). Psychoeducation was the only intervention with an adequate evidence base (N = 152) and inconclusive effect v. waitlist. Although results suggest a trend towards the superiority of EMDR over other active interventions, no evidence of differential effects between EMDR and other treatments with a large evidence base was found. Comparisons between active treatments suggested differences in effect only between EMDR and counselling (mean SMD −1.34, 95% CrI −2.19 to −0.49) and between TF-CBT and counselling (mean SMD −0.73, 95% CrI −1.37 to −0.09).
Metacognitive therapy (mean SMD −3.04, 95% CrI −5.09 to −0.98) and present-centred therapy (mean SMD −1.42, 95% CrI −2.45 to −0.40) also showed large effects v. waitlist with 95% CrI that did not cross the zero line; however, these effects were based on a more limited evidence base (N = 10 and 99, respectively).
Overall, results were characterised by relatively wide 95% CrI around mean effects and ranks; for example, TF-CBT mostly ranked between the 2nd and 8th place in different iterations of the NMA model. High between-study heterogeneity may have contributed to the uncertainty around mean effects.
Changes in PTSD symptom scores between baseline and 1–4-month follow-up
The network of changes in PTSD symptom scores between baseline and 1–4-month follow-up included 28 RCTs, 2315 participants and 15 interventions (Fig. 2b). TF-CBT was again the intervention with the largest evidence base (N = 753 in 13 trials); other interventions with moderately good-sized evidence base were counselling (N = 205 in 4 trials), non-TF-CBT (N = 123 in 4 trials), EMDR (N = 121 in 4 trials) and psychoeducation (N = 183 in 3 trials). All other interventions were tested on fewer than 100 participants each. Of the 28 trials, 10 and 15 recruited participants with a single and multiple traumas, respectively; three studies did not provide any information on participants' number of previous traumas.
Of the interventions tested on N ⩾ 100 each, only two showed evidence of effect v. waitlist: EMDR (mean SMD −1.12, 95% CrI −1.94 to −0.27) and TF-CBT (mean SMD −0.73, 95% CrI −1.23 to −0.25) (Table 2). Comparison between the two showed no evidence of difference in effect (mean SMD −0.39 favouring EMDR, 95% CrI −1.30 to 0.54). Interventions with N ⩾ 100 but inconclusive effects v. waitlist included psychoeducation, non-TF-CBT and counselling.
Of interventions with a limited evidence base (each tested on N < 100), couple intervention, self-help with support and behavioural therapy also showed evidence of effectiveness against waitlist.
This analysis was also characterised by high between-study heterogeneity and uncertainty that was reflected in wide 95% CrI around mean effects and rankings across interventions.
Remission at treatment endpoint
The NMA of remission at treatment endpoint consisted of 34 studies, 2249 participants and 16 interventions (Fig. 2c). TF-CBT was tested on N = 601 participants in 21 trials; other interventions with a moderately good-sized evidence base were counselling (N = 150 in 6 trials); EMDR (N = 132 in 5 trials) and self-help with support (N = 105 in two trials). All other interventions were tested on fewer than 100 participants each. Of the 34 trials, 15 and 16 recruited participants with a single and multiple traumas, respectively; three studies did not provide any information on participants' number of previous traumas.
All interventions with an adequate evidence base (N ⩾ 100) showed evidence of large effects v. waitlist. Their order, from the most to least effective was: EMDR (mean LOR v. waitlist 3.38, 95% CrI 2.04–4.84), TF-CBT (mean LOR v. waitlist 2.46, 95% CrI 1.79–3.19), self-help with support (mean LOR v. waitlist 1.76, 95% CrI 0.03–3.49) and counselling (mean LOR v. waitlist 1.34, 95% CrI 0.20–2.51). Comparisons between active treatments suggested differences in effect only between EMDR and counselling (mean LOR 2.04, 95% CrI 0.37–3.79) and between TF-CBT and counselling (mean LOR 1.12, 95% CrI 0.12–2.15).
Several interventions with limited evidence (each tested on N < 100) showed large effects v. waitlist on the remission outcome; these included psychodynamic therapy, non-TF-CBT, relaxation, IPT and present-centred therapy.
As with previous outcomes, there was uncertainty in the results as suggested by very wide 95% CrI around mean effects and rankings across all interventions (Table 3). There was also very high between-study heterogeneity.
Results between all pairs of treatments examined in the NMAs and also results from indirect and, where available, direct (head-to-head) comparisons are reported in online Supplementary Appendix 11. For information, results of the NICE guideline analyses are shown in online Supplementary Appendix 12.
Pairwise sub-analyses
Exploratory sub-analyses of the pairwise meta-analysis comparing trauma-focused CBT and waitlist for PTSD symptom change scores between baseline and endpoint suggests no significant subgroup differences for different specific TF-CBT interventions (including CPT, CT, prolonged exposure, narrative exposure therapy, brief eclectic psychotherapy and non-branded individual and group CBT). There were also no significant subgroup differences between ITT, modified ITT and completer analysis or for single compared to multiple incident index trauma. See online Supplementary Appendix 13 for forest plots of these sub-analyses.
Discussion
Overview of findings
This study aimed to identify the relative treatment effects of various psychological treatments for PTSD. EMDR, combined somatic/cognitive therapies, TF-CBT and self-help with support appeared to have the greatest effects in reducing PTSD symptoms post-treatment, followed by non-TF-CBT, combined TF-CBT/SSRIs, SSRIs, self-help without support and counselling. No evidence of difference in effect post-treatment was identified between interventions, with the exception of EMDR and TF-CBT, both of which were found to be superior to counselling. Analysis of follow-up data suggested that EMDR and TF-CBT sustained this effect at 1–4 months. EMDR, TF-CBT, self-help with support and counselling were also effective at achieving remission from PTSD at treatment endpoint. Results for other interventions were either inconclusive or based on limited evidence.
Commonalities across effective psychotherapies for PTSD include psychoeducation, imaginal exposure and cognitive processing, restructuring and/or meaning making (Schnyder et al., Reference Schnyder, Ehlers, Elbert, Foa, Gersons, Resick and Cloitre2015). Moreover, all treatments found to be effective comprised structured therapies, delivered by healthcare professionals who have completed specialist training and who have access to regular supervision and undertake appropriate continuing professional development accreditation. Combined somatic/cognitive therapies are exposure-based therapies with cognitive and somatic components, thus they share some characteristics with the TF-CBT class. All except one of the RCTs on self-help with support included in the NMA focused on computerised TF-CBT, consistent with TF-CBT delivered by a therapist. On the other hand, of the 13 trials on self-help without support, only four focused on computerised TF-CBT. Further to the presence or absence of the TF-CBT element in self-help interventions for PTSD, which may have been the driver of their effectiveness, there is evidence that facilitated self-help is more effective than self-help without support in the treatment of anxiety disorders and depression (National Institute for Health and Care Excellence, 2011).
Counselling was found to be amongst the least effective interventions. This can be attributed to counselling's non-directive person-centred approach, which is less likely to help the person overcome avoidance (which is one of the criteria for PTSD), and thus less likely to reduce PTSD symptoms. However, in 10 out of the 11 RCTs examining counselling across the three NMAs, counselling served as a control treatment to other active interventions, primarily TF-CBT, and therefore it is possible that counselling's effectiveness has been underestimated to some extent, due to researcher allegiance.
Comparison with findings of other reviews
The results of our analysis are consistent with those of other published reviews, according to which TF-CBT interventions and EMDR have the strongest evidence of effectiveness post-treatment and at short follow-up, both showing highest effects v. inactive controls compared with other psychological interventions (Bisson et al., Reference Bisson, Roberts, Andrew, Cooper and Lewis2013; Cusack et al., Reference Cusack, Jonas, Forneris, Wines, Sonis, Middleton and Gaynes2016; Forman-Hoffman et al., Reference Forman-Hoffman, Middleton, Feltner, Gaynes, Weber, Bann and Green2018). This finding is also in line with five recently published PTSD clinical practice guidelines (as compared in Hamblen et al., Reference Hamblen, Norman, Sonis, Phelps, Bisson, Nunes and Schnurr2019). Four of these five guidelines, including the NICE clinical guideline (Departments of Veterans Affairs and Defense, 2017; International Society for Traumatic Stress Studies, 2019; National Institute for Health and Care Excellence, 2018a; Phoenix Australia Centre for Posttraumatic Mental Health, 2013), make recommendations of equal strength for TF-CBT and EMDR for adults, whereas in one guideline (American Psychological Association, 2017) TF-CBT interventions are favoured with a strong recommendation while EMDR has been given a moderate rating. Conversely, Khan et al. (Reference Khan, Dar, Ahmed, Bachu, Adnan and Kotapati2018) suggests that EMDR may be more effective than TF-CBT, however this finding was not supported by another publication that employed NMA techniques (Gerger et al., Reference Gerger, Munder, Gemperli, Nüesch, Trelle, Juni and Barth2014). The latter review is in agreement with our findings, which show no evidence of difference between EMDR and TF-CBT. Further research is needed to establish any reliable difference between the efficacy of TF-CBT and EMDR.
There is some published evidence suggesting that non-TF-CBT (Bisson et al., Reference Bisson, Roberts, Andrew, Cooper and Lewis2013), present-centred therapy (Frost et al., Reference Frost, Laska and Wampold2014) and self-help (mainly internet-based TF-CBT and expressive writing therapy) (Kuester et al., Reference Kuester, Niemeyer and Knaevelsrud2016; Sijbrandij et al., Reference Sijbrandij, Kunovski and Cuijpers2016; van Emmerik et al., Reference van Emmerik, Reijntjes and Kamphuis2013) are also effective options in the treatment of PTSD in adults. There are also recommendations for other psychotherapies in recently published clinical PTSD guidelines, although there was less consistency than for TF-CBT and EMDR (Hamblen et al., Reference Hamblen, Norman, Sonis, Phelps, Bisson, Nunes and Schnurr2019). For instance, three of the guidelines included recommendations for non-trauma focused psychotherapies (Departments of Veterans Affairs and Defense, 2017; International Society for Traumatic Stress Studies, 2019; Phoenix Australia Centre for Posttraumatic Mental Health, 2013). This evidence, from both published reviews and clinical guidelines, is in line with our findings that suggest that non-TF-CBT, present-centred therapy and self-help (with or without support) are effective relative to waitlist at improving PTSD symptoms.
Our findings on the effectiveness of combined somatic/cognitive therapies are consistent with results reported in the systematic review by Forman-Hoffman et al. (Reference Forman-Hoffman, Middleton, Feltner, Gaynes, Weber, Bann and Green2018), who carried out separate evaluations of the emotional freedom technique and thought field therapy (defined in the review as ‘imagery rehearsal therapy’) and found very limited evidence on both interventions which, nevertheless, indicated that these might be effective in the treatment of PTSD symptoms.
Another published NMA of treatments for adults with PTSD suggested that several interventions are effective in the management of PTSD (Gerger et al., Reference Gerger, Munder, Gemperli, Nüesch, Trelle, Juni and Barth2014). That study considered a more limited number of interventions than our analysis, including three types of TF-CBT (CBT, CT and exposure therapy) that were assessed separately but also as a TF-CBT class, EMDR, stress management (relaxation or biofeedback), supportive therapies (comprising psychotherapy placebos and counselling) and other psychological therapies (including psychodynamic, client-centred, gestalt and other forms). The authors reported that all assessed interventions were more effective than waitlist; TF-CBT interventions and EMDR were more effective than stress management and supportive therapies, but no difference was observed between TF-CBT and EMDR. The robustness of evidence varied considerably between different interventions and between-trial heterogeneity was high. These findings are in line with our results. The study considered only PTSD symptom severity at the end of treatment or at maximum of 1 month post-treatment, whereas our NMAs considered PTSD change scores at treatment endpoint and at 1–4-month follow-up and also remission at the end of treatment. Therefore, our conclusions cover a wider range of interventions and outcomes and longer-term effects, where available.
Our findings are also broadly consistent with the results of a NMA of psychological interventions in children and young people with PTSD, which suggested that TF-CBT, in particular individual forms, was most effective in the management of PTSD in youth, whereas EMDR was effective but to a lesser extent; counselling did not appear to be effective compared with waitlist. Results in young populations also suggested a large positive effect for emotional freedom technique (a form of combined somatic/cognitive therapies), but this finding was based on very limited evidence (Mavranezouli et al., Reference Mavranezouli, Megnin-Viggars, Daly, Dias, Stockton, Meiser-Stedman and Pilling2020).
Overall, our results and conclusions are in agreement with previously published meta-analyses in this area. Small differences between our study results and those of other studies (which, nevertheless, led to very similar conclusions) have potentially arisen from differences in inclusion criteria relating to the population (e.g. we included only adult populations while some other studies did not apply any age restrictions or considered only children and young people with PTSD; we did not restrict to people with a formal diagnosis of PTSD while some other studies did), interventions (we used a wider range of interventions compared with other reviews and it is also possible that our categorisation into classes is different from that used in other studies), comparators (we excluded studies that used TAU as a comparator or as a component of an active arm), outcomes (we included continuous PTSD symptom change scores at endpoint and 1–4 month follow-up as well as dichotomous remission, whereas some of the other studies included only continuous data and/or only treatment endpoint data) and study characteristics (we included studies with a sample size of at least 10 per arm, a criterion not applied in most, if not all, the other reviews), as well as differences in the method of analysis (we used NMA techniques whereas the vast majority of the other reviews in the area relied on pairwise meta-analysis of head-to-head comparisons).
Strengths and limitations of the analysis
To our knowledge, this is the first NMA of psychological treatments for adults with PTSD that was designed to inform a clinical guideline. The results of our NMAs further informed an economic analysis that assessed the cost-effectiveness of psychological interventions for adults with PTSD (Mavranezouli et al., Reference Mavranezouli, Megnin-Viggars, Grey, Bhutani, Leach, Daly and Pillingunder review). NMA techniques enabled evidence synthesis from both direct and indirect comparisons between interventions, and allowed simultaneous inference on all treatments examined in pairwise trial comparisons while respecting randomisation (Caldwell et al., Reference Caldwell, Ades and Higgins2005; Lu & Ades, Reference Lu and Ades2004). Inconsistency checks found no evidence of inconsistency between direct and indirect estimates in the NMAs of changes in PTSD symptoms post-treatment and at follow-up. This finding provides reassurance that the included studies were comparable across interventions, although it is acknowledged that, in agreement with the findings of other reviews, between-trial heterogeneity was high. On the other hand, we detected evidence of inconsistency in the NMA of remission post-treatment. However, we found that direct effects in this NMA were implausibly large and with very wide 95% CrI due to limitations in the direct evidence; therefore indirect/NMA evidence may be more trustworthy for the remission outcome. This means that results on this outcome (remission at treatment endpoint) should be treated with caution.
Between-trial heterogeneity was high across all analyses. This finding, which is consistent with previous reviews (Bisson et al., Reference Bisson, Roberts, Andrew, Cooper and Lewis2013; Forman-Hoffman et al., Reference Forman-Hoffman, Middleton, Feltner, Gaynes, Weber, Bann and Green2018; Gerger et al., Reference Gerger, Munder, Gemperli, Nüesch, Trelle, Juni and Barth2014), is likely to have been caused by heterogeneity across populations included in the trials considered in our analysis, for example, in terms of the presence of a formal PTSD diagnosis, the baseline severity and complexity of PTSD symptoms, the type, extent and multiplicity of trauma exposure, the chronicity of symptoms and the presence of comorbidity. Moreover, the vast majority of the included studies did not distinguish between PTSD and complex PTSD, which ICD-11 (unlike DSM-5) now conceptualises as distinct diagnoses. This distinction is supported by evidence (Brewin et al., Reference Brewin, Cloitre, Hyland, Shevlin, Maercker, Bryant and Reed2017) but some disagreement about the validity of the construct amongst experts remains, as suggested by the discrepancy between the two classification systems (ICD-11 and DSM-5). We note that our review was undertaken before ICD-11 (and the distinction between PTSD and complex PTSD) was released (June 2018). Trials are likely to have varied widely in the proportion of participants with complex PTSD; this may have had an impact on the effectiveness of assessed interventions in each study and the heterogeneity across studies. Another factor potentially contributing to the high between-trial heterogeneity of our NMAs is the variability of interventions within each treatment node of the analysis (including different levels of intensity), and the difference across study settings, e.g. inpatient v. outpatient. This high between-trial heterogeneity may have contributed to the uncertainty in the mean relative effects, as reflected in the wide CrI for some comparisons in our analyses, and has limited our ability to draw firm conclusions on the relative effectiveness between interventions. However, it is worth noting that, although exploratory in nature and limited to a single pairwise comparison, our sub-group analyses suggest that between-study heterogeneity cannot be accounted for solely by differences between specific TF-CBT interventions, based on the method of analysis (ITT v. completer), or by the multiplicity of index trauma (single v. multiple incident index trauma). This suggests that this heterogeneity is complex and further studies employing meta-regression techniques, ideally with access to individual patient data, are required to fully explore differences in effect estimates between studies.
We decided to analyse all TF-CBT interventions together, as a class, because, although they do not include exactly the same content or follow the same manual, they use the same broad approach; in grouping the interventions into a TF-CBT class we took the view that it is the core components of the treatments (e.g. exposure and cognitive restructuring) that make them effective. We also took into account that ‘breaking’ the solid evidence base for the TF-CBT class into smaller, separate pieces of evidence for specific interventions would unavoidably thin the evidence base and incur the risk of reducing the robustness of our conclusions on the effectiveness of interventions within the TF-CBT class relative to other types of treatment. Some reviews (e.g. Bisson et al., Reference Bisson, Roberts, Andrew, Cooper and Lewis2013; Khan et al., Reference Khan, Dar, Ahmed, Bachu, Adnan and Kotapati2018) have followed our approach and have evaluated the overall effects of the TF-CBT class, rather than looking at the effects of specific interventions within the TF-CBT class separately. The Departments of Veterans Affairs and Defense (2017) guideline also grouped TF-CBT interventions together but chose to list the specific treatments for which there was the strongest support, which is a similar approach to the one taken by the NICE clinical guideline (Hamblen et al., Reference Hamblen, Norman, Sonis, Phelps, Bisson, Nunes and Schnurr2019). There is now an emerging number of reviews that have attempted to evaluate the effects of distinct interventions within the TF-CBT class (e.g. American Psychological Association, 2017; Cusack et al., Reference Cusack, Jonas, Forneris, Wines, Sonis, Middleton and Gaynes2016; Forman-Hoffman et al., Reference Forman-Hoffman, Middleton, Feltner, Gaynes, Weber, Bann and Green2018), with another review assessing the overall effect of the TF-CBT class, and also effects of individual forms within TF-CBT class where evidence was adequate to allow sub-group analysis (International Society for Traumatic Stress Studies, 2019). These reviews have carried out separate evaluations of various TF-CBT interventions such as CPT, CT, prolonged exposure and mixed TF-CBT which has elements of different types of CBT. The majority of these studies have found evidence on the effectiveness of all interventions within the TF-CBT class but none of the studies reported any evidence on differential effects between different types of TF-CBT. A previously published NMA in the area (Gerger et al., Reference Gerger, Munder, Gemperli, Nüesch, Trelle, Juni and Barth2014), which evaluated CBT, exposure and CT separately and made indirect comparisons between them, identified no differences in relative effects. The authors then merged CBT and CT into one category of CBT with a focus on cognitions and reanalysed the data; no difference was found between CBT with focus on cognitions and exposure. These results suggest that there may be no difference in the effectiveness of different interventions within the TF-CBT class, and supports our decision to consider TF-CBT interventions together, as one class, in our analysis. It is worth noting here that our exploratory post-hoc sub-analysis by specific TF-CBT intervention for all studies including a waitlist control (see online Supplementary Appendix 13A) also suggests no significant sub-group difference between specific TF-CBT intervention types.
In our analyses, we prioritised self-reported over clinician-rated scale data, where possible, as self-reported outcomes were deemed to better capture symptoms experienced by adults with PTSD, based on the NICE guideline committee's expert opinion. This approach is in line with a previously published NMA in the same area (Gerger et al., Reference Gerger, Munder, Gemperli, Nüesch, Trelle, Juni and Barth2014), although other reviews have conducted separate analyses for clinician-rated and self-reported outcome data (Bisson et al., Reference Bisson, Roberts, Andrew, Cooper and Lewis2013; Forman-Hoffman et al., Reference Forman-Hoffman, Middleton, Feltner, Gaynes, Weber, Bann and Green2018), or even prioritised clinician-rated outcomes over self-reported ones, where both were available, in the primary analysis (International Society for Traumatic Stress Studies, 2019). It is acknowledged that in other mental health areas, such as depression, it is recommended that both clinician-rated and self-reported outcomes be assessed as they have been shown to capture different aspects of treatment outcome (Cuijpers, Li, Hofmann, & Andersson, Reference Cuijpers, Li, Hofmann and Andersson2010; Uher et al., Reference Uher, Perlis, Placentino, Dernovšek, Henigsberg, Mors and Farmer2012). A sub-group analysis conducted by Gerger et al. (Reference Gerger, Munder, Gemperli, Nüesch, Trelle, Juni and Barth2014) showed that the differences between effect sizes in trials reporting self-reported outcomes v. those reporting clinician-rated ones were small and non-significant (p = 0.58) and within-trial heterogeneity was not affected by inclusion of only one type of outcome in the analysis. Therefore, we are confident that our choice of prioritising self-reported over clinician-rated outcomes has not had a negative impact on results.
In our NMA we did not include TAU, either alone or combined with a control or with an intervention of interest; this is because the definition of TAU varied considerably across trials, so that inclusion of TAU in the networks was expected to considerably increase heterogeneity and reduce robustness of the results. Omission of studies that assessed interventions alone or combined with TAU v. TAU has limited the evidence base of our analyses. However, the number of included studies (which did not include TAU) was higher than the number of excluded studies that included TAU; moreover, included ‘non-TAU’ studies considered a higher number of participants than the excluded ‘TAU’ studies. Therefore, our analyses have considered a significant amount of evidence without introducing heterogeneity attributable to the diversity of TAU.
The studies included in the NMAs were subject to risk of bias, in particular selection and reporting bias. In none of the studies were participants blinded, which was unavoidable due to the nature of the interventions. In most trials assessors were not blinded either. As described earlier, self-rated PTSD symptom scores were preferred to clinician-rated ones if both were reported in a study, as they were deemed to better capture symptoms experienced by people with PTSD. However, self-rated assessment cannot be blinded in trials of psychological interventions; on the other hand, raters were less likely to have a conflict of interest in terms of detection bias. The quality and limitations of RCTs included in the analyses need to be considered when interpreting the results.
For the change in PTSD symptom score outcome we prioritised ITT over completer data where possible, nevertheless, for approximately 40% of the studies we used completer data as only these were available. An exploratory sub-group analysis of the TF-CBT v. waitlist comparison for PTSD symptom change scores between baseline and treatment endpoint suggests no statistically significant subgroup difference between the results of studies using ITT, modified ITT and completer analysis (see online Supplementary Appendix 13B). This is also consistent with a sub-group analysis conducted in the context of a NMA of treatments for PTSD by Gerger et al. (Reference Gerger, Munder, Gemperli, Nüesch, Trelle, Juni and Barth2014), which showed that the differences between effect sizes in trials reporting ITT data v. those reporting completer data were small and non-significant (p = 0.47), although within-trial heterogeneity was somewhat reduced by inclusion of ITT data only (from τ 2 = 0.30 when both ITT and completer data were included in the analysis it fell at τ 2 = 0.21 when only ITT data were analysed). Our ITT approach for the dichotomous remission analysis meant that all participants were analysed in the group to which they had been randomised and that study non-completers were assumed to have failed to remit. This strategy provides a conservative estimate of treatment effects compared with completer analysis (Nüesch et al., Reference Nüesch, Trelle, Reichenbach, Rutjes, Bürgi, Scherer and Jüni2009), assuming that active interventions have a higher risk of drop-out compared with control conditions (this higher risk could be attributable to side effects, unacceptability of the active intervention, or to people discontinuing treatment early if their symptoms improve).
Evidence on the longer-term effectiveness of treatments for PTSD is limited, as follow-up data are sparse. Adequate evidence on remission rates at 1–4-month follow-up was only available for TF-CBT; for this reason we were not able to conduct any meaningful NMA of remission follow-up data. Available evidence suggests that TF-CBT and EMDR are effective at sustaining improvements in PTSD symptoms at 1–4-month follow-up. Evidence for other interventions was limited or inconclusive.
Implications for practice and need for further research
Results support current clinical practice within which TF-CBT and EMDR are the mainstream options offered to adults with PTSD. Our findings suggest that other treatments, such as supported self-help, combined somatic/cognitive therapies and non-TF-CBT are also effective and could be potential alternative treatment options, although amongst them only supported self-help has some limited evidence for sustained effects beyond treatment. This might have implications for clinical practice as services currently focus on provision of TF-CBT and EMDR. In contrast, although effective v. waitlist, counselling appears to be less effective than other treatment options and therefore should not be routinely offered if more effective options are available. In our review, we were not able to focus on complex PTSD, which is currently less likely to be identified and managed effectively in routine practice. Further research is therefore needed to identify appropriate interventions specific to populations with complex PTSD.
Based on the results of the NMAs and the primary economic analysis (Mavranezouli et al., Reference Mavranezouli, Megnin-Viggars, Grey, Bhutani, Leach, Daly and Pillingunder review; National Institute for Health and Care Excellence, 2018b), the NICE guideline on PTSD recommended EMDR and individual TF-CBT for the treatment of adults with PTSD presenting more than 3 months after trauma (National Institute for Health and Care Excellence, 2018a). Both interventions were effective at reducing PTSD symptoms post-treatment and demonstrated sufficient evidence to suggest sustainment of effect beyond treatment. The recommendation for EMDR was restricted to people with non-combat-related trauma, as evidence from sub-group pairwise meta-analysis suggested a non-significant effect on people with combat-related trauma, a finding that was confirmed by a recent systematic review and meta-analysis (Kitchiner, Lewis, Roberts, & Bisson, Reference Kitchiner, Lewis, Roberts and Bisson2019).
In addition, based on the available evidence and after taking account of the narrower evidence base, a weaker (‘consider’) recommendation was made for self-help with support and SSRIs for people who expressed a preference for these interventions, and, in the case of self-help, did not have severe PTSD symptoms and were not at risk of harm to themselves or others. A ‘consider’ recommendation was also made for non-TF-CBT targeted at specific symptoms, for people who are unable or unwilling to engage in a trauma-focused intervention or have residual symptoms after treatment. Finally, the guideline committee noted the positive evidence for combined somatic/cognitive therapies, but also considered their particularly limited evidence base beyond treatment endpoint and the lack of specific indications for these interventions, and decided not to recommend them but instead to make a recommendation for further research.
TF-CBT was the treatment with the largest evidence base on PTSD symptom severity and remission, both at the end of treatment and at 1–4-month follow-up. Further research is needed to establish the results for EMDR more firmly, in particular in relation to TF-CBT, as conclusions on its effectiveness are based on a more limited evidence base compared with TF-CBT and its relative effects v. TF-CBT were characterised by uncertainty. Similarly, research should further explore the effectiveness of other interventions, especially combined somatic/cognitive therapies, which demonstrated high effects at treatment endpoint, but also non-TF-CBT and self-help with support regarding remission and effectiveness beyond end of treatment, as relevant evidence is limited or lacking. Future research should also establish the effects of different types of TF-CBT relative to other types of treatment, but also relative to other types of TF-CBT, as evidence on comparative effectiveness is limited for some types of TF-CBT. In particular, evidence on sustainability of effects beyond treatment endpoint is sparse and only available for a few treatments; this lack of evidence is most evident for remission rates beyond treatment endpoint. This gap in evidence needs to be addressed by future trials, which should ideally include at least 12 months of follow-up, to explore the longer-term effectiveness of psychological therapies for PTSD.
Conclusion
EMDR and TF-CBT appear to be most effective at reducing symptoms and improving remission rates in adults with PTSD. They also appear to be effective at sustaining the reduction of PTSD symptoms beyond treatment endpoint. Other interventions, such as combined somatic/cognitive therapies, self-help, non-TF-CBT, SSRIs and counselling appear to be effective at reducing PTSD symptoms post-treatment; self-help with support and counselling appear to improve remission rates post-treatment, too. Counselling is likely to be less effective than EMDR and TF-CBT. Further research is needed to establish these findings for EMDR, as its evidence base is more limited compared with TF-CBT, and to better assess the relative effectiveness of interventions such as different types of TF-CBT, combined somatic/cognitive therapies, self-help with support and non-TF-CBT, in particular regarding remission rates and effectiveness beyond end of treatment. Overall, there is a need for well-conducted RCTs to explore the long-term comparative effectiveness of psychological therapies for adults with PTSD.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291720000070.
Acknowledgements
We thank other members of the Guideline Committee for the NICE guideline on ‘Post-traumatic stress disorder’ for their contributions to this work. Members of the Committee were: Steve Hajioff, Philip Bell, Gita Bhutani, Sharif El-Leithy, Neil Greenberg, Nick Grey, Cornelius Katona, Jonathan Leach, Richard Meiser-Stedman, Rebecca Regler, Vikki Touzel and David Trickey.
Financial support
This work was initiated by the National Collaborating Centre for Mental Health (NCCMH) and continued by the National Guideline Alliance (NGA) at the Royal College of Obstetricians and Gynaecologists (RCOG) from 1 April 2016, with support from the NICE Guidelines Technical Support Unit (TSU), University of Bristol, which is funded by the Centre for Guidelines (NICE). NCCMH and NGA received funding from NICE to develop clinical and social care guidelines. The views expressed in this publication are those of the authors and not necessarily those of the RCOG, NGA, NCCMH or NICE. The funder of the study had no further role in the study design, data collection, data analysis, data interpretation or writing of the report. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication. National Institute for Health and Care Excellence (2018) Post-traumatic stress disorder, available from https://www.nice.org.uk/guidance/ng116.
Conflict of interest
SD and NW were co-applicants on a grant (unrelated to this work) from the MRC Methodology Research Programme which included an MRC Industry Collaboration Agreement with Pfizer Ltd, who part-funded a researcher to work on statistical methodology. GB is a co-investigator on a NIHR RfPB grant, Eye Movement Desensitization and Reprocessing Therapy in Early Psychosis (EYES): a feasibility randomised controlled trial. NGreenberg is the Royal College of Psychiatrists Lead for Military and Veterans' Health and is a trustee of two military charities. He is also a senior researcher with King's College London working on a number of military mental health studies. NGrey is a member of the Wellcome Trust Anxiety Disorders Group developing, testing and disseminating Cognitive Therapy for PTSD (CT-PTSD), a trauma-focused cognitive behavioural therapy (TF-CBT). He has published papers and book chapters on CT-PTSD, and facilitates teaching workshops for which payment is received. As editor, he receives royalties from sales of a trauma book, A Casebook of Cognitive Therapy for Traumatic Stress Reactions. CK is Medical Director of the Helen Bamber Foundation (a human rights charity) and refugee and asylum mental health lead for the Royal College of Psychiatrists. He writes expert psychiatric reports in the context of asylum mental health. JL is NHS England Medical Director for Military and Veterans Health. SP receives funding from NICE for the development of clinical guidelines. He is also supported by the NIHR UCLH Biomedical Research Centre.







