Introduction
Having a parent with mental disorders is a significant risk factor for developing a severe mental illness, which can be explained by genetic, environmental and psychosocial factors (Hosman, van Doesum, & van Santvoort, Reference Hosman, van Doesum and van Santvoort2009; Mattejat & Remschmidt, Reference Mattejat and Remschmidt2008; Wille, Bettge, & Ravens-Sieberer, Reference Wille, Bettge and Ravens-Sieberer2008). The mechanisms of this association are very complex and subtle, with strong interrelationships between genetic and environmental factors (Apter, Bobin, Genet, Gratier, & Devouche, Reference Apter, Bobin, Genet, Gratier and Devouche2017). In addition, the interactional pathways between the suffering parent and their child are often bidirectional (Dodge, Bates, & Pettit, Reference Dodge, Bates and Pettit1990). The presence of a mental disorder in a parent may thus be associated with poorer attachment, negative parenting and even abuse (O'Donnell et al., Reference O'Donnell, Maclean, Sims, Morgan, Leonard and Stanley2015). In turn, the child's subsequent difficulties may worsen the parent's psychological suffering and mental disorder. Children of depressed parents are about three times more likely to develop anxiety disorders, major depression or substance use disorder (Weissman et al., Reference Weissman, Wickramaratne, Nomura, Warner, Pilowsky and Verdeli2006). A previous meta-analysis (Rasic, Hajek, Alda, & Uher, Reference Rasic, Hajek, Alda and Uher2014) highlighted that one-third of children of parents suffering from a severe mental illness may develop psychiatric disorders by early adulthood. Offspring are also at greater risk of developing internalizing and externalizing symptoms (Connell & Goodman, Reference Connell and Goodman2002), relationship difficulties (Bella et al., Reference Bella, Goldstein, Axelson, Obreja, Monk, Hickey and Birmaher2011; Larsson, Knutsson-Medin, Sundelin, & Trost von Werder, Reference Larsson, Knutsson-Medin, Sundelin and Trost von Werder2000) and demonstrate lower academic competences (Hay et al., Reference Hay, Pawlby, Sharp, Asten, Mills and Kumar2001). Moreover, these long-term outcomes and adverse consequences have been shown to lead to high direct and indirect costs (Prince et al., Reference Prince, Patel, Saxena, Maj, Maselko, Phillips and Rahman2007). The impact of preventive interventions on these costs has been evaluated in some studies that have highlighted significant economic benefits (Arango et al., Reference Arango, Díaz-Caneja, McGorry, Rapoport, Sommer, Vorstman and Carpenter2018; Knapp, McDaid, & Parsonage, Reference Knapp, McDaid and Parsonage2011).
A previous meta-analysis (Siegenthaler, Munder, & Egger, Reference Siegenthaler, Munder and Egger2012) focusing on the offspring of parents with mental disorders showed that preventive interventions decreased by 40% [combined relative risk of 0.60, 95% confidence interval (CI) 0.45–0.79] the risk of developing the same mental illness as the parents and led to a small but significant decrease of internalizing symptoms. A more recent meta-analysis (Thanhäuser, Lemmer, de Girolamo, & Christiansen, Reference Thanhäuser, Lemmer, de Girolamo and Christiansen2017), which focused on emotional and behavioural symptoms in children and adolescents, reported similar results for internalizing symptoms, and small effects on externalizing symptoms, reaching significance only at follow-up. However, these previous studies did not systematically refer in their inclusion process to international classifications such as the Diagnostic and Statistical Manual of Mental Disorders (DSM; American Psychiatric Association, 2013) or the International Classification of Disease (ICD; World Health Organization, 1992) for the diagnosis of parental mental disorders, and did not assess the incidence in the offspring of mental disorders different than the parental ones.
Despite mounting data supporting the efficacy of early preventive intervention in the offspring of individuals with mental illness, a gap still exists between evidence from research and public health policies. The limited interest of health authorities in mental health prevention can be partly explained by several factors (Arango et al., Reference Arango, Díaz-Caneja, McGorry, Rapoport, Sommer, Vorstman and Carpenter2018): the lack of awareness of the substantial economic savings from preventive interventions, the stigma of this population and the need for an initial investment in the training of professionals (which is costly and often yield limited short-term beneficial return). An almost decade-old review of available preventive programs (Reupert et al., Reference Reupert, Cuff, Drost, Foster, Van Doesum and Van Santvoort2012) found that most of the interventions were based on psychosocial education, with the need for further research to establish the conditions that can improve children's outcomes. In addition, this study only focused on children aged 5–18 years, excluded parenting programs that did not involve children and did not screen out based on study quality.
Therefore, the aims of the present study are: (i) to review existing preventive interventions focusing on children and adolescents of mentally ill parents and evaluated by randomized controlled trials; and (ii) to perform a meta-analysis of their efficacy on children's outcomes in terms of incidence of mental disorders (same or different than the parental ones) and internalizing and externalizing symptoms.
Methods
A systematic review of the literature and a meta-analysis of randomized controlled trials of preventive interventions in the offspring of parents with mental illness were performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines (Moher, Liberati, Tetzlaff, & Altman, Reference Moher, Liberati, Tetzlaff and Altman2009). The review protocol was developed in advance and registered within PROSPERO (#CRD42020170843).
Search methods
The eight following electronic databases were used to identify relevant published literature: MEDLINE, MEDLINE in-process, EMBASE, Cochrane Central Register of Controlled Trials (CENTRAL, Cochrane Library), Web of Science, PsycINFO, PsycArticles and ERIC. In addition to this systematic screening, an exploration of the grey literature was conducted using the OpenGrey database. Search strategies, based on a previous meta-analysis (Siegenthaler et al., Reference Siegenthaler, Munder and Egger2012) and adapted to the other databases, are provided in online Supplement 1. Reference lists of the relevant articles were screened, as well as studies included in prior reviews and meta-analyses, and a hand-search of the Journal of the American Academy of Child and Adolescent Psychiatry was performed (1987–2021). All articles identified were included with no backward limit to 30 June 2021. No language restrictions were applied.
Selection criteria
For inclusion in this review and meta-analysis, studies had to meet the following criteria: (i) child and adolescent under 18 years old of parents with a diagnosis of mental illness as classified by the DSM or the ICD, including mood disorders, anxiety disorders, psychotic disorders or substance use disorders; (ii) intervention aimed at child, parents or both, from different theoretical underpinnings (cognitive and behavioural psychotherapy, family system therapy, skill-building techniques, etc.), compared to a control group (no intervention, treatment as usual or another intervention); (iii) outcomes in child included the incidence of mental disorders (same or different than the parental ones) and/or the severity of internalizing and externalizing symptoms, measured by standardized instruments (including self-reports, parent or expert reports, or structured interviews); (iv) randomized controlled trials.
Exclusion criteria were defined as follows: (i) child with a diagnosis of mental disorder at the time of inclusion, or child belonging to another high-risk group (like premature babies); (ii) parents with unclear diagnosis of mental illness or only at-risk for mental illness (i.e. vulnerable population); (iii) interventions reporting outcomes exclusively related to parent–child interaction; (iv) clinical trials other than randomized controlled trials and studies with insufficient power making it impossible to calculate a standardized mean difference (SMD).
Data extraction and quality appraisal
Two reviewers (AL and AR) independently performed database search and article screening using Zotero software (Corporation for Digital Scholarship, USA). Data from each included trial were extracted and coded independently using a data extraction form. Any disagreement was resolved by discussion with a third reviewer (JPR) to reach a consensus.
The coded variables included characteristics of studies (characteristics of participants, sample size, type of interventions and control groups, funding and target audiences, outcome measures and instruments used, follow-up time points) and necessary data to calculate the effect size.
When data were missing or to clarify some values, the study's authors were contacted for further information. Twelve authors were contacted, of whom only four replied (Clarke et al., Reference Clarke, Hornbrook, Lynch, Polen, Gale, Beardslee and Seeley2001; Compas et al., Reference Compas, Forehand, Thigpen, Hardcastle, Garay, McKee and Sterba2015; Kelley & Fals-Stewart, Reference Kelley and Fals-Stewart2002; Van Santvoort, Hosman, van Doesum, & Janssens, Reference Van Santvoort, Hosman, van Doesum and Janssens2014). Three trials could not be included in our meta-analysis because either the design (Zhang, Slesnick, & Feng, Reference Zhang, Slesnick and Feng2018) or the available data (Murray, Cooper, Wilson, & Romaniuk, Reference Murray, Cooper, Wilson and Romaniuk2003; Van Santvoort et al., Reference Van Santvoort, Hosman, van Doesum and Janssens2014) did not allow us to conduct our analysis.
The quality of included studies was evaluated by two reviewers independently (AR and AL), using the quality assessment tool QUALSYST, from the Standard Quality Assessment Criteria for Evaluating Primary Research Papers from a Variety of Fields (Kmet, Lee, & Cook, Reference Kmet, Lee and Cook2004; Table 1). The classification of methodological quality was determined based on percentage scores and therefore identified strong quality (score > 80%), good quality (score = 70–79%), fair quality (score = 50–69%) and poor quality (score < 50%).
Table 1. QUALSYST 14-item checklist for quality assessment of included studies

(NA) not applied; (+) fulfilled; (+/−) partly fulfilled; (−) not fulfilled.
Criteria: 1: Question/objective sufficiently described?; 2: Study design evident and appropriate?; 3: Method of subject/comparison group selection or source of information/input variables described and appropriate?; 4: Subject (and comparison group, if applicable) characteristics sufficiently described?; 5: If interventional and random allocation was possible, was it described?; 6: If interventional and blinding of investigators was possible, was it reported?; 7: If interventional and blinding of subjects was possible, was it reported?; 8: Outcome and (if applicable) exposure measure(s) well defined and robust to measurement/misclassification bias? Means of assessment reported?; 9: Sample size appropriate?; 10: Analytic methods described/justified and appropriate?; 11: Some estimate of variance is reported for the main results?; 12: Controlled for confounding?; 13: Results reported in sufficient detail?; 14: Conclusions supported by the results?
Calculation of the summary score: summary score (%) = (total sum/total possible sum) × 100. Total sum = [number of (+) × 2] + [number of (+/−) × 1]. Total possible sum = 28 – [number of (NA) × 2].
Statistical analyses
Characteristics of the included studies were summarized narratively. Meta-analyses were conducted to pool data using RevMan 5.4 (RevMan 5.4, The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark) and STATA 14 (Stata 14, StataCorp LP, College Station, TX, USA). Because there were some differences between included studies' characteristics, a random-effects model was chosen for the analysis.
Risk ratios (RR) were calculated with their 95% CIs to estimate the difference between groups in the incidence of mental disorders at post-intervention. The RR gives an indication of the likelihood of the onset of a mental illness in the experimental group compared to the control condition. Values between 0 and 1 indicate a positive effect of the intervention, whereas values >1 indicate a negative effect of the intervention.
For internalizing and externalizing symptoms, SMD and 95% CI were used as the effect measure using the inverse variance method (Higgins & Green, Reference Higgins and Green2011). A negative effect represented an improvement (less emotional and behavioural symptoms), and effect sizes were interpreted as small 0.20–0.49, medium 0.50–0.79, and large 0.8 and higher (Cohen, Reference Cohen1988). The mean scores with their standard deviations were extracted separately for the active interventions and the control groups. When multiple scales were reported for the symptoms, Child Behaviour Checklist (CBCL; Achenbach, Reference Achenbach1991) was favoured since it was the most widely used.
For the externalizing symptoms, the Eyberg Child Behaviour Inventory (ECBI; Eyberg & Pincus, Reference Eyberg and Pincus1999), which is a behaviour-specific instrument consisting of a list of 36 behaviours, was preferred to the Strengths and Difficulties Questionnaire (SDQ; Goodman, Reference Goodman2001), which is less specific and includes both emotional and behavioural difficulties. When the outcome was the functioning impairment, the specific scale used (Global Assessment of Functioning scale, GAF) was chosen (Clarke et al., Reference Clarke, Hornbrook, Lynch, Polen, Gale, Beardslee and Seeley2001).
In two instances, when the outcome was a measure of depressive symptoms (Clarke et al., Reference Clarke, Hornbrook, Lynch, Polen, Gale, Beardslee and Seeley2001; Garber et al., Reference Garber, Clarke, Weersing, Beardslee, Brent, Gladstone and Iyengar2009), the pre-defined hierarchical ranking (Hazell, O'Connell, Heathcote, & Henry, Reference Hazell, O'Connell, Heathcote and Henry2002) was followed for inclusion in the meta-analysis: (i) Children's Depression Rating Scale (CDRS-R); (ii) Hamilton Depression Rating Scale (HAMD); (iii) Children's Depression Inventory (CDI); (iv) Centre for Epidemiological Studies Depression Scale (CES-D). For all measures, subscales of specific symptoms were always preferred over total scores.
Most of the trials reported multiple assessments at different follow-up times for the effects of preventive interventions. Therefore, continuous outcome variables (internalizing and externalizing symptoms) were clustered into three different time windows: post-intervention follow-up (0–4 months), short-term follow-up (5–12 months) and long-term follow-up (15–68 months). ‘Post-intervention’ was defined as the completion of the main intervention, excluding booster sessions. When trials reported more than one assessment within a time window, the datapoint closest in time to that of the other studies within that window was chosen to minimize heterogeneity.
Regarding dichotomous outcomes (incidence of mental disorders in children), only five trials reported data on this variable, which did not allow us to cluster data in different time windows. For this reason, we selected the time points that were most similar to each other between trials, which resulted in combining assessments from 6, 12 and 144-month follow-up.
The I 2 statistic and Cochran Q's χ2 test were performed to assess the heterogeneity of the results between trials. For the interpretation of the I 2 statistics, which indicates the proportion of the total variation in the estimated effects caused by heterogeneity between trials rather than chance, the Cochrane Handbook for Systematic Review of Interventions (Higgins & Green, Reference Higgins and Green2011) was used. Values of I 2 suggest low heterogeneity between 0% and 40%, moderate heterogeneity between 30% and 60%, substantial heterogeneity between 50% and 90% and considerable heterogeneity between 75% and 100%. For the χ2 test, heterogeneity was statistically significant when the p value was <0.1 (Higgins & Green, Reference Higgins and Green2011). Publication bias was assessed using funnel plots and Egger's tests.
When studies significantly differed from the others, particularly in terms of extreme follow-up points, sensitivity analyses were conducted to identify outliers. When outliers could not be identified to reduce heterogeneity, subgroup analyses were conducted to examine the effect of some variables on the outcomes. These variables included the type of interventions (family, children or parents-based interventions), the type of control groups (active or non-active), the age of children and parents' and children's symptoms at baseline (when >50% participants had symptoms at baseline, it was considered as a presence of symptoms). For the age of children, when the range was large in the studies, we took the mean age of the children included to classify them in the different subgroups (0–2, 3–12 or 13–18 years old). The first assessment time point after the intervention was selected for subgroup analyses.
Results
A total of 31 articles reporting data from 20 independent randomized controlled trials were included in the systematic review, of which 17 trials were included in the meta-analysis. The selection process is reported in Fig. 1.
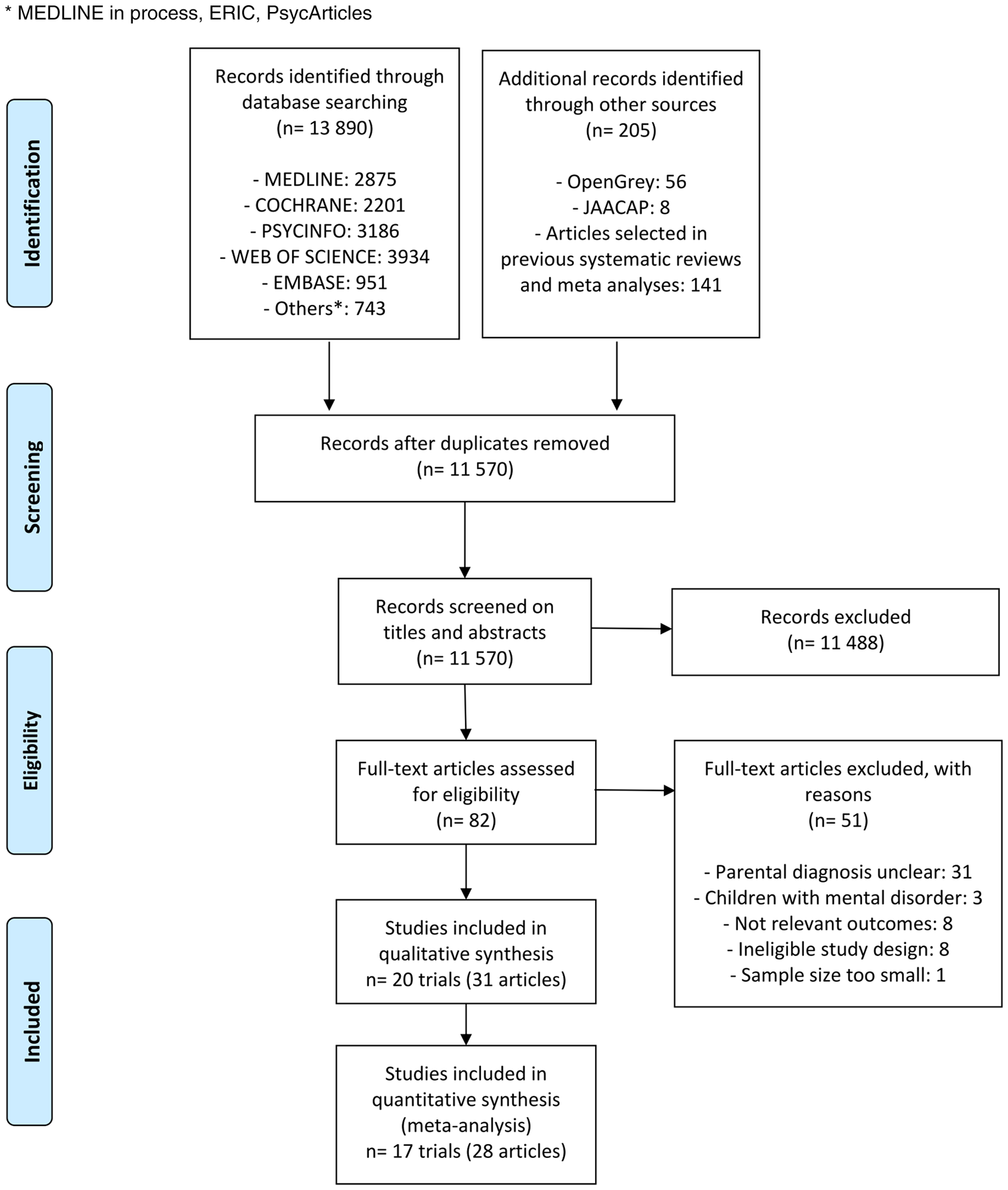
Fig. 1. Flow diagram of the selection process.
Characteristics of studies
Sample sizes ranged from 30 to 316 children per study, with a total of N = 2689 randomized children and N = 2523 parents included in the narrative synthesis, 80.9% of whom were mothers. For our meta-analysis, a total of N = 2081 randomized children and N = 1915 parents were included. Parents were diagnosed with mood disorders in 13 trials, substance use disorders in five, anxiety disorders in one and multiple disorders in one trial. Further details on the characteristics of parents are provided in online Supplementary Table S1. Studies were published from 1999 to 2021. Eleven were performed in the USA, four in the UK, two in the Netherlands, one in Canada, one in Greece and one in Finland. No articles needed to be translated.
Study quality
Studies quality is reported in Table 1. The control group could be an active intervention, such as groups for parents (lecture, discussion or training sessions), or self-study of written information. In contrast, treatment as usual and waiting list were considered as non-active control groups. Fourteen studies had strong quality score, five studies good quality score and one study fair quality score. The quality criteria that differed the most between studies were the blinding of investigators, the description of the method used for randomization and the justification of an appropriate sample size.
Characteristics of interventions
Characteristics and main findings of each study are summarized in Table 2 and a detailed description of each intervention can be found in online Supplementary Table S2, based on the TIDieR (Template for Intervention Description and Replication) Checklist (Hoffmann et al., Reference Hoffmann, Glasziou, Boutron, Milne, Perera, Moher and Michie2014). Preventive interventions were heterogeneous with respect to the age range of children included (from 4.5 months to 18 years old), their symptoms at baseline, the place (at clinic or at home) and the number and length of sessions (from 6 to 33 sessions, each lasting between 30 min and 2 h), the family members involved, and the type of control group used. Interventions focused on families (including the child and at least one of the two parents) in nine trials, on parents in four trials, on mothers only in four trials and on youth in three trials. Among the 11 studies reporting it, the average participation rate in the main sessions was 67.9%. The drop-out rate ranged from 4% (Clarke et al., Reference Clarke, Hornbrook, Lynch, Polen, Gale, Beardslee and Seeley2001, at post-test) to 46% (Verduyn, Barrowclough, Roberts, Tarrier, & Harrington, Reference Verduyn, Barrowclough, Roberts, Tarrier and Harrington2003, in the control group at 12-month follow-up).
Table 2. Characteristics and main results of the 20 randomized controlled trials included in the systematic review
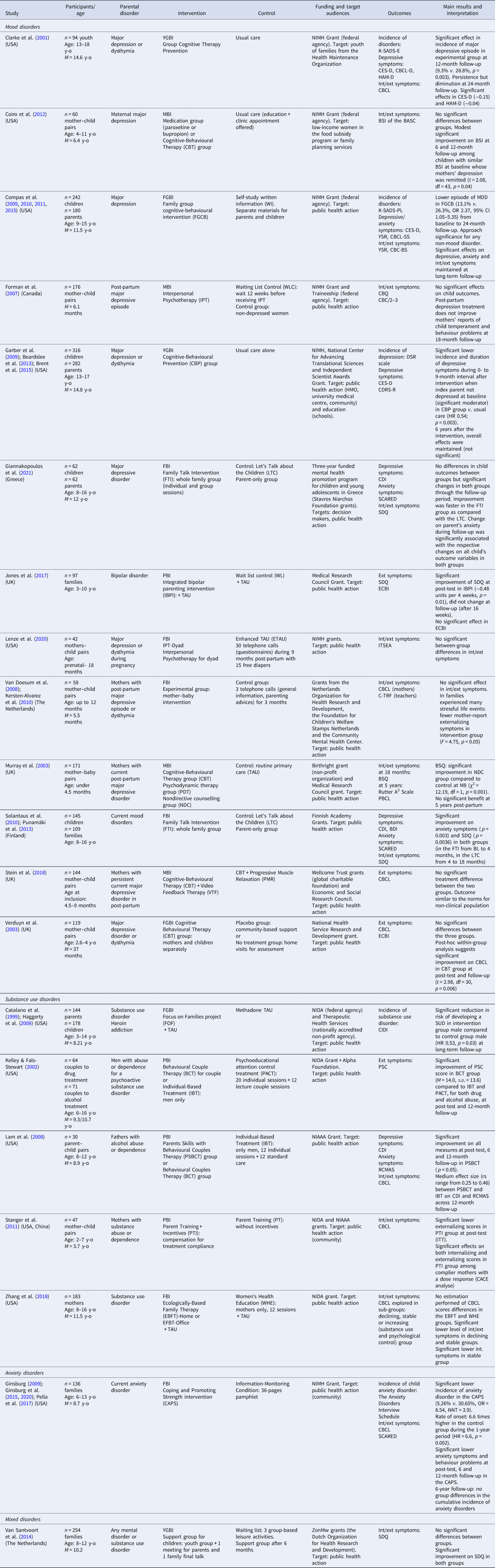
BASC, Behaviour Assessment System for Children; BSI, Behavioural Symptoms Index; BSQ, Behavioural Screening Questionnaire; CBCL, Child Behaviour Check List (-SS: syndrome scales; -BS: broadband scales); CBQ, Child Behaviour Questionnaire; CDI, Children's Depression Inventory; CDRS-R, Children's Depression Rating Scale Revised; CES-D, Center for Epidemiologic Studies Depression scale; CIDI, Composite International Diagnostic Interview; C-TRF, Caregiver-Teacher Report; DSR, Depression Symptom Rating; ECBI, Eyberg Child Behaviour Inventory; FBI, Family-Based Intervention; FGBI, Family Group-Based Intervention; HAM-D, Hamilton Depression Rating Scale; Int/ext, internalizing/externalizing symptoms; K-SADS, Kiddie Schedule for Affective Disorders and Schizophrenia (-E: Epidemiological, -PL: Present and Lifetime Version); M, mean age; MBI, Mother-Based Intervention; MDD, major depressive disorder; NIAAA, National Institute on Alcohol Abuse and Alcoholism; NIDA, National Institute on Drug Abuse; NIMH, National Institute of Mental Health; PBCL, Problem Behaviour Check List; PBI, Parent-Based Intervention; PSC, Pediatric Symptom Checklist; RCMAS, The Revised Children's Manifest Anxiety Scale; SCARED, Screen for Child Anxiety Related Disorders; SDQ, Strengths and Difficulties Questionnaire; TAU, treatment as usual; YGBI, Youth Group-Based Intervention; YSR, Youth Self-Report.
Cognitive-behavioural therapy (CBT)
Seven trials (Clarke et al., Reference Clarke, Hornbrook, Lynch, Polen, Gale, Beardslee and Seeley2001; Coiro, Riley, Broitman, & Miranda, Reference Coiro, Riley, Broitman and Miranda2012; Compas et al., Reference Compas, Forehand, Thigpen, Hardcastle, Garay, McKee and Sterba2015; Garber et al., Reference Garber, Clarke, Weersing, Beardslee, Brent, Gladstone and Iyengar2009; Kersten-Alvarez, Hosman, Riksen-Walraven, Van Doesum, & Hoefnagels, Reference Kersten-Alvarez, Hosman, Riksen-Walraven, Van Doesum and Hoefnagels2010; Murray et al., Reference Murray, Cooper, Wilson and Romaniuk2003; Verduyn et al., Reference Verduyn, Barrowclough, Roberts, Tarrier and Harrington2003) assessed intervention techniques mainly based on cognitive restructuring and behavioural therapy, among which three used formal treatment manuals. All these programs were designed for parents with mood disorders and focused either on youth, mothers or the whole family. In youth, the aims were to increase their understanding of parents' disorders, to identify and challenge negative thoughts and beliefs related to having a depressed parent, and to learn problem-solving skills. In parents, the aims were to improve parenting skills with behavioural training focused on positive, child-centred methods of control, to focus on cognitive management of mood and to support interactions with reinforcement of positive family relationships.
Psychoeducation
Psychoeducational techniques were evaluated in nine trials (Catalano, Gainey, Fleming, Haggerty, & Johnson, Reference Catalano, Gainey, Fleming, Haggerty and Johnson1999; Giannakopoulos, Solantaus, Tzavara, & Kolaitis, Reference Giannakopoulos, Solantaus, Tzavara and Kolaitis2021; Jones et al., Reference Jones, Jovanoska, Calam, Wainwright, Vincent, Asar and Lobban2017; Kelley & Fals-Stewart, Reference Kelley and Fals-Stewart2002; Lam, Fals-Stewart, & Kelley, Reference Lam, Fals-Stewart and Kelley2008; Pella, Drake, Tein, & Ginsburg, Reference Pella, Drake, Tein and Ginsburg2017; Solantaus, Paavonen, Toikka, & Punamäki, Reference Solantaus, Paavonen, Toikka and Punamäki2010; Stein et al., Reference Stein, Netsi, Lawrence, Granger, Kempton, Craske and Murray2018; Van Santvoort et al., Reference Van Santvoort, Hosman, van Doesum and Janssens2014), sometimes associated with CBT approaches. Interventions targeted parents with mood disorders, substance use disorders (in association with behavioural couple therapy) or anxiety disorders. They could take place at the clinic (with group sessions) or at home (home visits or online self-management).
The aim of family approaches was to target theory-driven modifiable child and parent risk factors, with an improvement of the communication and a deeper understanding of mental illness and its impact on family members. Families were taught how to identify the signs of the parents' disorder and how to reduce them. Parenting skills training focused on the improvement of communication, positive behavioural exchanges and problem-solving skills.
Other approaches
One trial (Murray et al., Reference Murray, Cooper, Wilson and Romaniuk2003) assessed a psychodynamic approach for mothers suffering from post-partum depressive symptoms, aiming at understanding mothers' representations of their infant by exploring the aspects of their own early attachment history.
In two studies (Forman et al., Reference Forman, O'Hara, Stuart, Gorman, Larsen and Coy2007; Lenze, Potts, Rodgers, & Luby, Reference Lenze, Potts, Rodgers and Luby2020), an interpersonal therapy for these mothers was evaluated, respectively based on a biopsychosocial perspective (targeting interpersonal problems, including interpersonal conflicts, social role transitions and loss and grief) and on attachment theory to explore the development of the mother–child dyadic relationship.
Other researchers (Coiro et al., Reference Coiro, Riley, Broitman and Miranda2012) reported, in parallel with a CBT group, a medication group for depressive mothers, consisting of taking an antidepressant treatment for 6 months.
A study evaluated a family system therapy (Zhang et al., Reference Zhang, Slesnick and Feng2018), focusing on mothers with a substance use disorder to target dysfunctional family interactions and identify factors contributing to maintain maternal symptoms. The efficacy of incentives (monetary prices) on compliance of parents with substance use disorders was also reported in another trial (Stanger, Ryan, Fu, & Budney, Reference Stanger, Ryan, Fu and Budney2011).
Effects on children's outcomes
Incidence of mental disorders (five trials)
Forest-plots of the effect of intervention (v. any of the control conditions) on the incidence of mental disorders in children at post-intervention (same as parental ones or any disorders) are provided in Fig. 2.
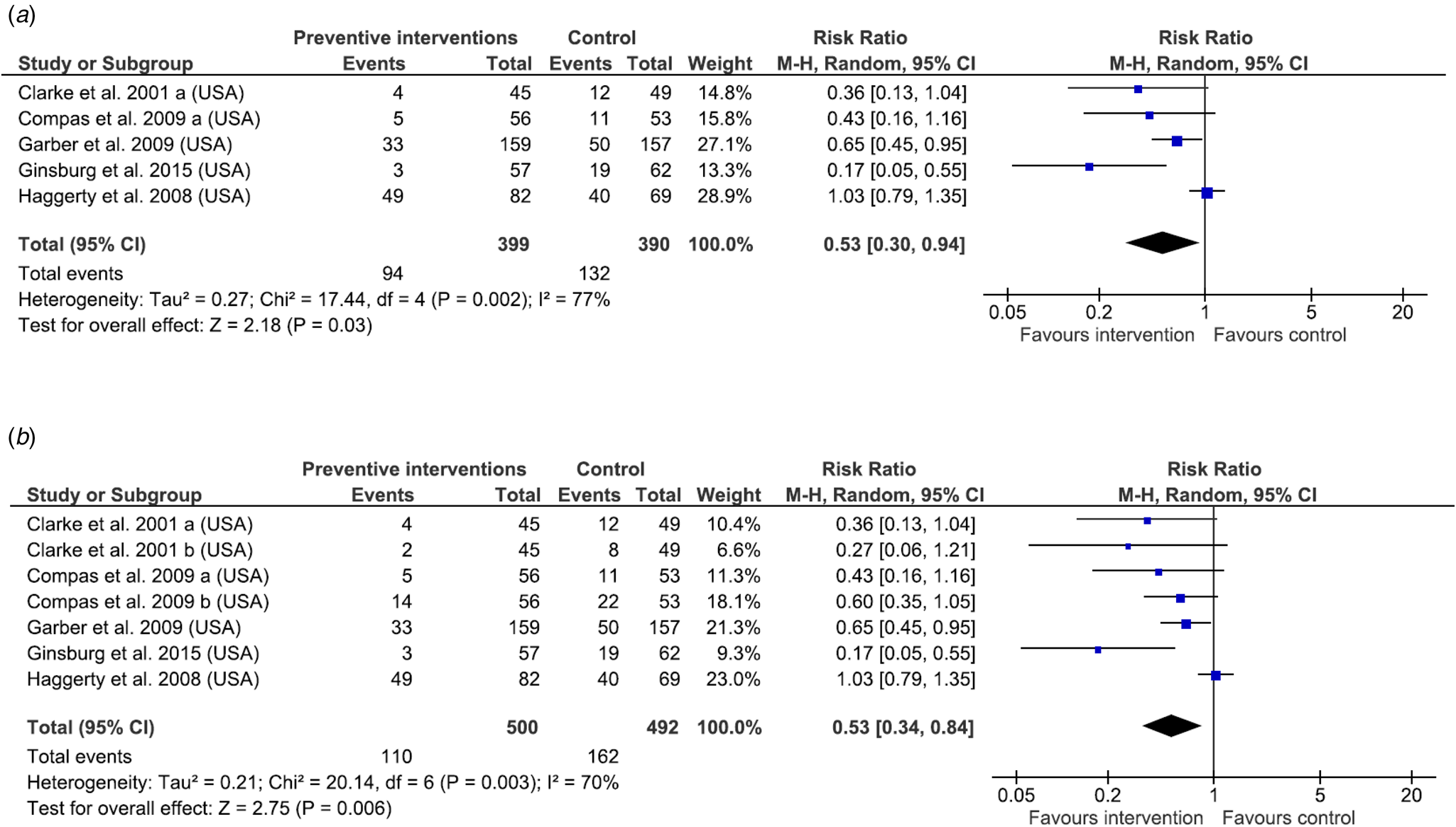
Fig. 2. Forest-plots of the effect of intervention v. any control condition on the risk in children to develop mental disorders. Note: (a) Incidence of the same mental disorders in children; (b) incidence of any mental disorders in children.
The risk in the offspring of developing the same mental illness as the parent was decreased by 47% (Fig. 2a: combined RR = 0.53, range 0.17–1.03, 95% CI 0.30–0.94, Z = 2.18, p = 0.03). Results were similar for the risk of developing any mental disorder (Fig. 2b: combined RR = 0.53, range 0.17–1.03, 95% CI 0.34–0.84, Z = 2.75, p = 0.006).
There was statistical evidence of considerable and substantial between-trial heterogeneity (Fig. 2a: I 2 = 77%, p = 0.002; Fig. 2b: I 2 = 70%, p = 0.003, respectively). A sensitivity analysis identified an outlier (Haggerty, Skinner, Fleming, Gainey, & Catalano, Reference Haggerty, Skinner, Fleming, Gainey and Catalano2008) because of its very long-term follow-up (144 months compared to other studies with data from 6 and 12-month follow-up). Excluding this trial lowered heterogeneity to low levels (I 2 = 47%, p = 0.13 and I 2 = 25%, p = 0.25, respectively), but had no significant impact on the results.
Internalizing symptoms (12 trials)
The effect of the active interventions (v. any of the control intervention) on internalizing symptoms in children is provided in Fig. 3a at post-intervention (A: 0–4 months), short-term (B: 5–12 months) and long-term follow-up (C: 15–68 months).
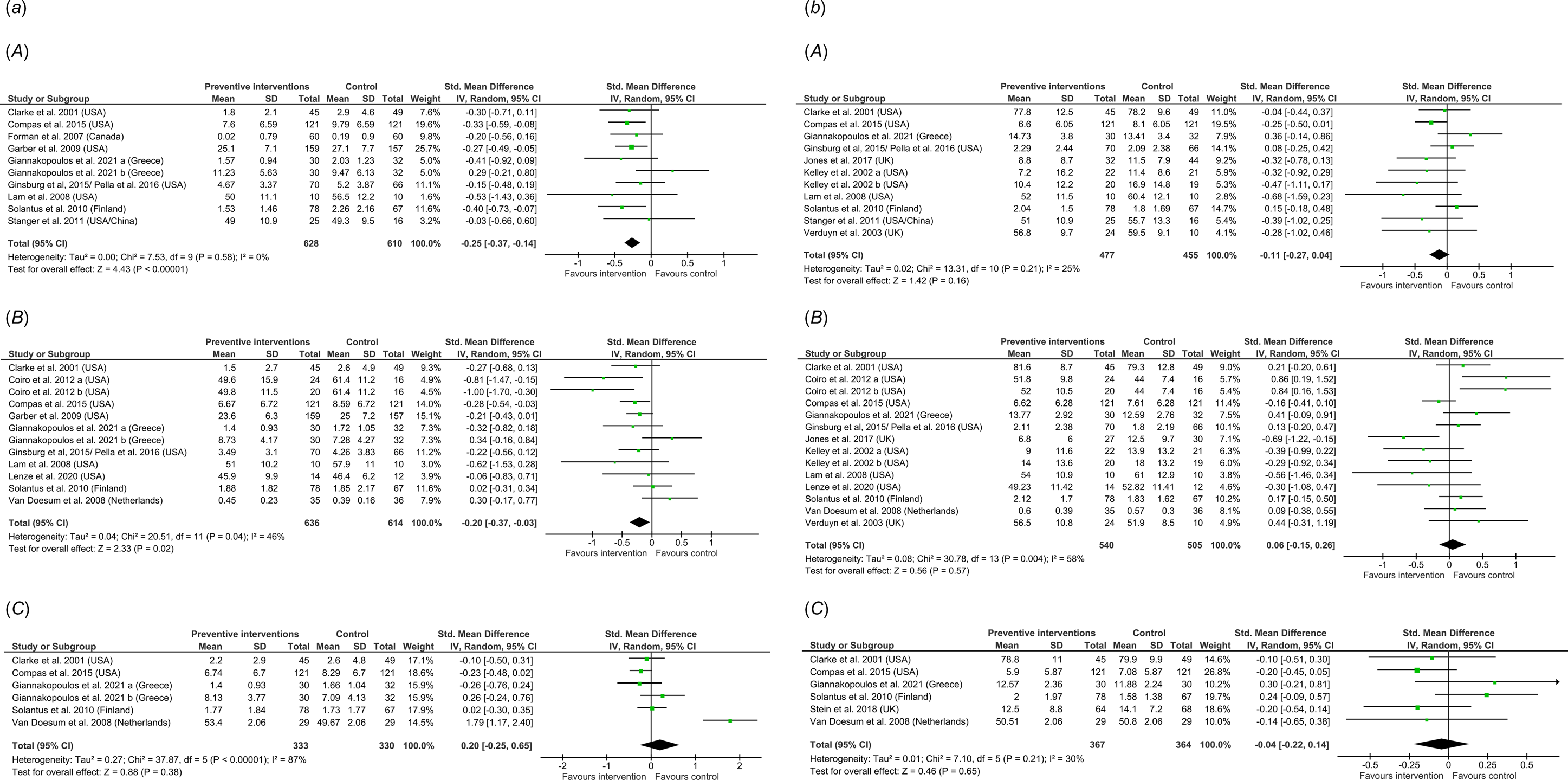
Fig. 3. Forest-plots of the effect of intervention v. any control condition in internalizing symptoms (a) and externalizing symptoms (b) in children over time. (A) At post-intervention follow-up; (B) at short-term follow-up; (C) at long-term follow-up.
One study (Coiro et al., Reference Coiro, Riley, Broitman and Miranda2012) included two separate comparison groups: CBT group (a in Fig. 3a) and medication group (b in Fig. 3a). Another study (Giannakopoulos et al., Reference Giannakopoulos, Solantaus, Tzavara and Kolaitis2021) reported two measures of internalizing symptoms (a, anxiety symptoms and b, depressive symptoms in Fig. 3a).
Post-intervention effects were small but significant (SMD = −0.25, range −0.53 to 0.29, 95% CI −0.37 to −0.14, Z = 4.43, p < 0.00001, I 2 = 0%), as well as short-term follow-up effects (SMD = −0.20, range −1 to 0.34, 95% CI −0.37 to −0.03, Z = 2.33, p = 0.02). Only five studies reported data at the long-term follow-up, and no effect of the intervention was found (SMD = 0.20, range −0.26 to 1.79, 95% CI −0.25 to 0.65, Z = 0.88, p = 0.38). Heterogeneity was significant but moderate at short-term (I 2 = 46%, p = 0.04) and high at long-term follow-up (I 2 = 87%, p < 0.00001). A sensitivity analysis identified an outlier (Van Doesum, Riksen-Walraven, Hosman, & Hoefnagels, Reference Van Doesum, Riksen-Walraven, Hosman and Hoefnagels2008) which reported data at very long-term follow-up (68 months). Excluding this trial from the long-term follow-up group lowered the heterogeneity to non-significant low levels (I 2 = 0%, p = 0.42), with no significant impact on the results. Subgroup analyses, including the type of intervention, the type of control groups, the presence or absence of children's and parents' symptoms at baseline and the age of children, failed to show significant subgroup differences (online Supplementary Fig. S1).
Externalizing symptoms (14 trials)
Figure 3b reports the effect of intervention on externalizing symptoms in children at post-intervention (A), short-term (B) and long-term follow-up (C).
One study (Kelley & Fals-Stewart, Reference Kelley and Fals-Stewart2002) included two separate comparison groups: alcohol-abusing fathers (a in Fig. 3b) and drug-abusing fathers (b in Fig. 3b).
No significant effect of intervention was reported at post-intervention (SMD = −0.11, range −0.68 to 0.36, 95% CI −0.27 to 0.04, Z = 1.42, p = 0.16, I 2 = 25%), short-term (SMD = 0.06, range −0.69 to 0.86, 95% CI −0.15 to 0.26, Z = 0.56, p = 0.57, I 2 = 58%) and long-term follow-up (SMD = −0.04, range −0.20 to 0.30, 95% CI −0.22 to 0.14, Z = 0.46, p = 0.65, I 2 = 30%). The sensitivity analysis identified no outliers. A subgroup analysis according to the presence or absence of children's symptoms at baseline revealed statistically significant subgroup differences [online Supplementary Fig. S2 (C), χ2 = 7.45, p = 0.006, I 2 = 86.6%] and reduced heterogeneity to low levels for the no symptoms subgroup (I 2 = 0%, p = 0.84) with a significant effect (Z = 2.75, p = 0.006). The other subgroup analyses founded non-significant differences (online Supplementary Fig. S2).
Publication bias
Online Supplementary Fig. S3 provided the funnel-plots of standard error (s.e.) against SMD for internalizing symptoms (A) and externalizing symptoms (B) at post-intervention. It seems that the studies were symmetrically distributed around the mean effect size, and Egger's tests suggested no evidence of publication bias (p = 0.541 and p = 0.264, respectively).
Discussion
This systematic review and meta-analysis identified 31 publications from 20 independent randomized controlled trials focused on preventive intervention in infants, children and adolescents of mentally ill parents. Most of the interventions were based on CBT approaches and psycho-educational techniques, either at home or in an outpatient clinic. The results of the meta-analysis showed that these interventions were efficacious on the risk of developing mental disorders in children, with a 47% reduction in risk. In addition, preventive interventions (compared to any control group) had a significant positive effect on internalizing symptoms after the intervention, during the first year.
Our results are in line with those of a previous study (Siegenthaler et al., Reference Siegenthaler, Munder and Egger2012), and we found larger effects (with a greater reduction in the incidence of mental disorders in children).
To our knowledge, this is the first meta-analysis to explore the incidence of any mental disorders in offspring, and to assess both internalizing and externalizing outcomes at different follow-up periods (post-intervention, short-term and long-term) in this population. Only two trials (Clarke et al., Reference Clarke, Hornbrook, Lynch, Polen, Gale, Beardslee and Seeley2001; Compas et al., Reference Compas, Forehand, Thigpen, Hardcastle, Garay, McKee and Sterba2015) assessed the incidence of mental disorders different from the parental ones, with no significant effect. Previous meta-analyses only explored the incidence of the same mental illness as parents in offspring (Loechner et al., Reference Loechner, Starman, Galuschka, Tamm, Schulte-Körne, Rubel and Platt2018; Siegenthaler et al., Reference Siegenthaler, Munder and Egger2012). However, the risk for children developing a mental disorder themselves is not a uniform and one-way process. A recent systematic review (Van Santvoort et al., Reference Van Santvoort, Hosman, Janssens, van Doesum, Reupert and van Loon2015) examined the relationship between parental affective or anxiety disorders and children's diagnostic outcomes in 76 studies. The authors found that children of parents with affective disorders had more transgenerational multifinality (children with the same parental diagnostic were at risk of a broad spectrum of symptoms) and equifinality (children of parents with different diagnoses were at risk of the same problems) patterns, in line with the results of another study (Weissman et al., Reference Weissman, Wickramaratne, Nomura, Warner, Pilowsky and Verdeli2006). In contrast, when parents were affected by anxiety disorders, transgenerational specificity and concordance patterns were more prevalent, which means their children were mainly at risk to have the same disorder, with specifically related symptoms. Therefore, complex factors seem to be involved in the transmission of mental disorders, and children are at risk of developing various disorders and not only the same as their parents. In view of these results, investigation of the incidence of various diagnoses in offspring in future studies appears essential to explore broader effects of preventive interventions in this high-risk population.
Five studies (Brent et al., Reference Brent, Brunwasser, Hollon, Weersing, Clarke, Dickerson and Garber2015; Compas et al., Reference Compas, Forehand, Thigpen, Hardcastle, Garay, McKee and Sterba2015; Garber et al., Reference Garber, Clarke, Weersing, Beardslee, Brent, Gladstone and Iyengar2009; Pella et al., Reference Pella, Drake, Tein and Ginsburg2017; Stein et al., Reference Stein, Netsi, Lawrence, Granger, Kempton, Craske and Murray2018; Van Santvoort et al., Reference Van Santvoort, Hosman, van Doesum and Janssens2014) included booster sessions, between 3 and 10 months later, in addition to the acute treatment, with the aim of prolonging the effects. Among these studies, an overall effect was maintained at 12-month follow-up in one trial (Pella et al., Reference Pella, Drake, Tein and Ginsburg2017) and at 24-month follow-up in another trial (Compas et al., Reference Compas, Forehand, Thigpen, Hardcastle, Garay, McKee and Sterba2015). At 6-year follow-up, the maintenance of initial gains was true only in parents who were not depressed at baseline (Brent et al., Reference Brent, Brunwasser, Hollon, Weersing, Clarke, Dickerson and Garber2015; Garber et al., Reference Garber, Clarke, Weersing, Beardslee, Brent, Gladstone and Iyengar2009). The impact of additional reminder sessions over time therefore appears to be an interesting approach to sustain the effects of these interventions over the long term, but it needs to be studied more precisely and systematically in future research.
Our study is the first to evaluate the impact of several variables on the effect of preventive interventions in children of parents with mental illness. In their meta-analysis, Siegenthaler et al. (Reference Siegenthaler, Munder and Egger2012) failed to find evidence for an effect of children's participation in the interventions (v. interventions focused on parents only). In the present study, we performed five subgroup analyses: the recipients of the interventions (family including the child and at least one of the two parents, parents only, v. children only); the presence of symptoms in parents and their children at baseline; the age of children; and the use of active v. non-active control groups. A significant difference was found only for the subgroup of children with no symptoms at baseline, in externalizing outcomes, suggesting that children with few or no symptoms prior to the intervention may benefit more from an intervention. However, these results need to be interpreted with caution and have not been found for the internalizing symptoms. We can also note that the majority of the children included were between 3 and 12 years old, with only two studies focusing specifically on adolescents (Clarke et al., Reference Clarke, Hornbrook, Lynch, Polen, Gale, Beardslee and Seeley2001; Garber et al., Reference Garber, Clarke, Weersing, Beardslee, Brent, Gladstone and Iyengar2009). We did not find significant differences in our subgroup analyses and it would be interesting in future research to study the impact of interventions on different age groups in order to compare their effectiveness according to the developmental stage of the children.
Another interesting consideration is the high level of variability in the attrition rates of participation in intervention, which requires a better identification of the factors that improve compliance in participants. For example, only 39% of women completed a substantial number of sessions in a CBT group intervention with distinct sessions for mothers and children in an outpatient clinic (Verduyn et al., Reference Verduyn, Barrowclough, Roberts, Tarrier and Harrington2003), while 90.3% of mothers attended at least nine out of 13 sessions when the intervention was delivered at home (Stein et al., Reference Stein, Netsi, Lawrence, Granger, Kempton, Craske and Murray2018). The drop-out rate was also highly variable and important, especially in long-term follow-ups, often reported as a limitation in the included studies. We found that five studies used monetary compensation to enhance participation and assessment completion, in particular with low-income parents suffering from substance use disorders (online Supplementary Table S2). Among them, one trial examined the effect of monetary incentives in addition to a parent training intervention for parents with substance use disorders (Stanger et al., Reference Stanger, Ryan, Fu and Budney2011). Surprisingly, homework completion and session attendance did not differ between the experimental and the control group, but higher rates of daily monitoring were highlighted in the group with incentives (twice as often as control group). The authors found an improvement of behavioural symptoms in the experimental group, suggesting that this daily intervention, improved by the incentives and combined with weekly groups, contributed significantly to the better outcomes observed in the experimental group. This might suggest that the improvement of family's engagement and retention is essential to implement preventive interventions in the most effective way. An earlier review of 17 randomized controlled trials (Ingoldsby, Reference Ingoldsby2010) of interventions to enhance family participation in parent and child mental health programs reported four types of interventions improving family engagement: brief early treatment engagement discussions, family systems approach, interventions focusing on enhancing coping and family support, and motivational interviewing. Engaging families with a severe mental illness in an intensive program can be complicated. Interventions can be experienced as intrusive for families, and communication about the risk of parental mental illness for offspring can be perceived as stigmatizing and guilt-ridden for the parents. Participation and retention of families are critical issues for clinical practices, and those dimensions must be taken into account in the evaluation of the effectiveness of preventive interventions.
This brings up the question of the generalizability of these results in clinical practice. Some studies focused on a very selective sample (Brent et al., Reference Brent, Brunwasser, Hollon, Weersing, Clarke, Dickerson and Garber2015; Clarke et al., Reference Clarke, Hornbrook, Lynch, Polen, Gale, Beardslee and Seeley2001) and were difficult to transpose to a real-life setting. Moreover, participants' differences between studies, particularly in regard to the severity of mental illness, comorbidities and socio-economic background, do not allow to generalize the results to a larger and different clinical population. Targeting parents with severe mental illness who did not seek help led to engagement difficulties in the recruitment process (difficulties in making contact, refusal to participate in the intervention, etc.). Other enrolment strategies, close to the patients' living environment, could be more interesting (for instance through general practitioners, schools or Internet). Another study (Stuart, Bradshaw, & Leaf, Reference Stuart, Bradshaw and Leaf2015) provided an overview of existing designs and analysis methods for enhancing external validity of randomized controlled trials to target populations, and their limitations. Further studies are required to extend these results to population encountered in real-life clinical practice. For instance, future studies could include qualitative analyses, to collect parents' experience of intervention and assess their acceptability. Moreover, most of the trials were conducted by the team who developed the intervention. Replication studies are needed, including in other settings (less selective population, more naturalistic conditions, etc.). Finally, both the lack of geographical diversity of the included trials (the vast majority of clinical trials were conducted in the USA and for substance use disorders in particular, all studies were conducted in the USA), and of racial and ethnic diversity in the included samples, limited the generalizability of our results to all racial and ethnic groups (Sue, Zane, Nagayama Hall, & Berger, Reference Sue, Zane, Nagayama Hall and Berger2009) and to all health care systems.
Our study was limited by the relatively low number of trials included on the final screening and their small samples (only three studies included more than 200 participants). However, our study's strict inclusion criteria allowed for the inclusion of rigorously selected trials as well as more homogeneous samples, than in previous meta-analyses (Siegenthaler et al., Reference Siegenthaler, Munder and Egger2012; Thanhäuser et al., Reference Thanhäuser, Lemmer, de Girolamo and Christiansen2017). Moreover, our search found no trials on parents with a psychotic disorder, and future trials in this specific population are warranted.
Another limitation is that most studies used only one informant's report for symptoms scales, especially parental reports, while it has been reported that parents with depression or substance use disorder might be less sensitive indicators of intervention effects (Compas et al., Reference Compas, Forehand, Thigpen, Hardcastle, Garay, McKee and Sterba2015; Lam et al., Reference Lam, Fals-Stewart and Kelley2008; Zhang et al., Reference Zhang, Slesnick and Feng2018). Future trials should assess outcomes using multiple informants, including parents, children, as well as others such as teachers, to prevent this bias.
In conclusion, this meta-analysis should be regarded as a step towards the implementation in clinical practice of preventive interventions for children and adolescents of parents with a mental illness. Through the analysis of 17 trials, we found evidence of positive effects of preventive interventions in the offspring of mentally ill parents, with a decrease of the risk of onset of mental disorders in children and of internalizing symptoms. Future studies should include an evaluation of the acceptability of these interventions and a study of potential moderating factors, in order to improve the therapeutic alliance and thus the clinical impact on this high-risk population.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291721003366.
Author contributions
AL and AR designed the study and wrote the protocol. AL and AR independently conducted the systematic review and AL produced the first draft of the manuscript. AR oversaw all aspects of the research. AR and EB drafted portions and substantively edited all drafts of the manuscript. AL, AR and EB analysed the data. CA and JPR critically revised the manuscript for important intellectual content. All authors contributed to and have approved the final manuscript. AL, AR and EB take responsibility for the integrity and the accuracy of the data analysis.
Financial support
This study is academic (University of Toulouse and Institut National de la Santé et de la Recherche Médicale). The authors received no specific funding for this study.
Conflict of interest
None.








