Introduction
Autism spectrum disorder (ASD) is an early-onset, heritable, neurodevelopmental condition characterised by impairments in social communication and interaction, as well as impaired behavioural flexibility (American Psychiatric Association, 2013), presenting with (ASD + ID) or without intellectual disability (ASD without ID). ASD has been diagnosed increasingly during the last decades, and the prevalence is now estimated to about 1.5% (Centers for Disease Control and Prevention (CDC), 2014; Idring et al., Reference Idring, Lundberg, Sturm, Dalman, Gumpert, Rai, Lee and Magnusson2015). ASD is associated with poor education, occupation, and social outcomes (Steinhausen et al., Reference Steinhausen, Mohr Jensen and Lauritsen2016), high perceived stress (Hirvikoski and Blomqvist, Reference Hirvikoski and Blomqvist2015), low quality of life (Jonsson et al., Reference Jonsson, Alaie, Lofgren Wilteus, Zander, Marschik, Coghill and Bolte2017), and high rates of psychiatric comorbidity (Simonoff et al., Reference Simonoff, Jones, Baird, Pickles, Happe and Charman2013; Russell et al., Reference Russell, Murphy, Wilson, Gillan, Brown, Robertson, Craig, Deeley, Zinkstok, Johnston, Mcalonan, Spain and Murphy2016). Previous results from small clinical studies suggest that individuals with ASD are at increased risk for suicidal ideation (Shtayermman, Reference Shtayermman2007; Raja et al., Reference Raja, Azzoni and Frustaci2011; Mayes et al., Reference Mayes, Gorman, Hillwig-Garcia and Syed2013; Storch et al., Reference Storch, Sulkowski, Nadeau, Lewin, Arnold, Mutch, Jones and Murphy2013; Cassidy et al., Reference Cassidy, Bradley, Robinson, Allison, Mchugh and Baron-Cohen2014), attempted suicide (Balfe and Tantam, Reference Balfe and Tantam2010; Mayes et al., Reference Mayes, Gorman, Hillwig-Garcia and Syed2013; Storch et al., Reference Storch, Sulkowski, Nadeau, Lewin, Arnold, Mutch, Jones and Murphy2013), and death by suicide (Raja et al., Reference Raja, Azzoni and Frustaci2011). The latter finding was recently replicated in a large register-based study showing a 2.4-fold suicide risk in individuals with ASD and ID and a 9.4-fold suicide risk in the ASD without ID group, compared to the general population (Hirvikoski et al., Reference Hirvikoski, Mittendorfer-Rutz, Boman, Larsson, Lichtenstein and Bolte2016).
The role of concomitant ID for suicidal behaviours is poorly understood since most of the previous studies were underpowered for comparison of ASD with and without ID, respectively. The high co-occurrence of additional neurodevelopmental conditions, such as ADHD, is another important factor to study (Lai et al., Reference Lai, Lombardo, Auyeung, Chakrabarti and Baron-Cohen2015): up to 40–50% of individuals with ASD also have ADHD which per se is strongly related to increased risk of suicidal behaviours (Ljung et al., Reference Ljung, Chen, Lichtenstein and Larsson2014). Moreover, although a majority of individuals with ASD have co-existing psychiatric disorders (Simonoff et al., Reference Simonoff, Jones, Baird, Pickles, Happe and Charman2013; Russell et al., Reference Russell, Murphy, Wilson, Gillan, Brown, Robertson, Craig, Deeley, Zinkstok, Johnston, Mcalonan, Spain and Murphy2016), e.g. depression and anxiety disorders, the role of psychiatric comorbidity for suicidal behaviours is not known in the context of ASD.
Given the indication of higher suicide risk in females with ASD (Hirvikoski et al., Reference Hirvikoski, Mittendorfer-Rutz, Boman, Larsson, Lichtenstein and Bolte2016), additional research is needed to resolve if these findings extend to attempted suicide. Previous research has also indicated possible gender differences in ASD-related characteristics and developmental trajectories, as well as gendered socio-cultural expectations and systems leading to sex differences in diagnostic thresholds and delayed identification of females with ASD as compared to males with ASD (Lai et al., Reference Lai, Lombardo, Auyeung, Chakrabarti and Baron-Cohen2015). This kind of gender differences may affect risk of suicidal behaviours, given the importance of environmental factors such as access to mental health care, as well as social structures and values (Turecki and Brent, Reference Turecki and Brent2016). Additional important environmental factors are social support and resources in the closest social environment (Turecki and Brent, Reference Turecki and Brent2016), partly reflected by family socio-economic status. However, studies on the possible role of family SES on the later suicidal behaviours are still lacking in the context of ASD.
Moreover, no previous study has used genetically informed study designs to explore the role of shared familial risk factors for ASD and suicidal behaviour. This is a critical limitation given that ASD is a highly heritable condition (Tick et al., Reference Tick, Bolton, Happe, Rutter and Rijsdijk2016) and suicidal behaviour is also partly attributable to genetic factors (Roy et al., Reference Roy, Segal, Centerwall and Robinette1991; Statham et al., Reference Statham, Heath, Madden, Bucholz, Bierut, Dinwiddie, Slutske, Dunne and Martin1998; Tidemalm et al., Reference Tidemalm, Runeson, Waern, Frisell, Carlstrom, Lichtenstein and Langstrom2011). An improved understanding of gender differences, psychiatric comorbidity, and the underlying aetiologic mechanisms will ultimately facilitate interventions to prevent suicidal behaviour in ASD.
The methodological challenges and knowledge gaps regarding literature on suicidal behaviour in ASD have been described in a review by Segers and Rawana (Reference Segers and Rawana2014), including a list of issues to be addressed in future research, such as longitudinal follow-up of clearly operationalised and well-validated constructs of suicidal behaviours, occurrence rates including death by suicide, analyses of risk and protective factors, inclusion of females and gender-specific analyses, separate analyses of individuals with or without ID, as well as appropriate comparison groups. Thus, the aim of the current study was to estimate the occurrence of suicidal behaviour associated with ASD in a large population-based cohort. To identify high-risk groups, we described gender-specific risk of suicide attempt and suicide, respectively, separately for ASD without ID (with/without ADHD) and ASD + ID (with/without ADHD) groups. Further, we analysed the role of socioeconomic status and psychiatric comorbidity for suicidal behaviour. Finally, the use of family data from longitudinal national registers enabled an analysis of shared familial risk factors for the association between ASD and suicidal behaviour.
Material and methods
Study design
We conducted a matched case-cohort study to assess the risk of suicide attempts and suicide in four ASD groups (1) ASD without ID (ASD) or ADHD, (2) ASD without ID with ADHD; (3) ASD with ID without ADHD; and (4) ASD with ID and ADHD, and across three levels of family relatedness to assess familial liability for suicidal behaviours.
Ethical approval
The Regional Ethics Committee in Stockholm approved the study (2013/862-31/5).
Study setting
Several nationwide population-based Swedish registers were linked using the unique ten-digit personal identification number used in registers for all Swedish residents, including migrants with a residence permit. The National Patient Register (NPR) includes primary and secondary diagnosis (up to seven diagnosis registered at a time point) for all inpatient treatment episodes for psychiatric disorders in Sweden since 1973, as well as for specialised outpatients (including diagnostic assessments with no further contact with psychiatric services) since 2001. The Cause of Death Register (CDR) covers nearly all deceased persons registered in Sweden at the time of their death from 1952 onward and provides information on the underlying causes of death. The diagnoses in both NPR and the CDR are coded according to the Swedish versions of the International Classification of Diseases (ICD) by the World Health Organisation (WHO). For identification of psychiatric comorbidity in the adjusted analyses, we also used the Swedish Prescribed Drug Register (established in 2005 and providing national information on all dispensed prescribed medication, with missing data for <0.3% of the population) (Wettermark et al., Reference Wettermark, Hammar, Fored, Leimanis, Otterblad Olausson, Bergman, Persson, Sundstrom, Westerholm and Rosen2007). The Multi-Generation Register links everyone living in Sweden at any time from 1961 onward to their biological parents, thus enabling identification of full siblings, half-siblings, and cousins. The Total Population Register provides information on sex, birth year, migration status, and county of residence in Sweden (Ludvigsson et al., Reference Ludvigsson, Almqvist, Bonamy, Ljung, Michaelsson, Neovius, Stephansson and Ye2016).
Family education level [highest education level (elementary, secondary, higher) held by either of the biological parents during life-time] for adjusted analyses was identified using three data sources from Statistics Sweden. For years 1970–1984, we used census 1970 (population and housing census); for years 1985–1989 Register-based labour market statistics (RAMS by Swedish acronym) a database combining statistics from administrative sources aim to offer annual information on employment, commuters, employees, and industrial structures; and for years 1990–2013 a longitudinal integration database for health insurance and labour market studies (LISA by Swedish acronym), which integrates existing data from the labour market, as well as educational and social sectors. LISA holds annual registers and includes all individuals 16 years of age and older registered in Sweden.
Study population
Individuals with ICD diagnosis codes for any ASD were identified from the NPR (see next section for the case ascertainment procedure), and the sample comprised 54 168 individuals with autism spectrum disorder: 43 570 ASD without ID (68.03% males; 43.69% with ADHD) and 10 598 ASD + ID (66.44% males; 27.31% with ADHD). The distribution of psychiatric comorbidity and sociodemographic variables is depicted in Table 1. To reduce confounding, misclassification of exposure and to ensure equal time at register follow-up, the controls were matched to the individuals with ASD. Thus, when the probands were registered in the NPR first time with an ASD diagnosis, they were matched with up to five controls from the Total Population Register. The controls (n = 270 840) were alive at the time point of inclusion; not diagnosed with neurodevelopmental disorders ASD, ADHD or ID during the study period (1987–2013); of same sex as the ASD probands; born during the same year as the individual with ASD; and living in the same county in Sweden as the individual with ASD at the time-point for the diagnosis (exact matching).
Table 1. Distribution of study variables in ASD without ID group (with/without ADHD), and ASD with intellectual disability (ASD + ID) group (with/without ADHD) and the general population controls, matched for each of the ASD groups

M, mean; s.d., Standard deviation; Md, median.
The sample characteristics in each cell are expressed as numbers and percent of column total number, except for age which is expressed as years.
For the analysis of risk of suicidal behaviour among relatives of ASD, an individual with ASD and his/her relatives (siblings, half-siblings and cousins) were matched to five unaffected controls and their corresponding relatives on gender and birth year (exact matching). Several pairs could be associated with one individual with ASD (e.g. in case of several siblings), and each individual could appear in multiple relative groups (e.g. sibling, cousin).
Ascertainment of ASD, ID, and ADHD, and the classification of the subgroups
We first identified all individuals with an ASD diagnosis between 1987 and 2013. The ICD-9 ASD diagnoses (years 1987–1996: 299A, 299B, 299W, 299X) were converted to corresponding ICD-10 diagnoses (1997 onwards) using a conversion instrument provided by the Swedish National Board of Health and Welfare. In the final cohort, the included diagnoses were autism (F84.0), Asperger syndrome (F84.5), atypical autism (F84.1), and pervasive developmental disorder – not otherwise specified (F84.9), other childhood disintegrative disorder (F84.3), and other pervasive developmental disorders (F84.8). Diagnoses of Rett syndrome (F84.2) and overactive disorder associated with mental retardation and stereotyped movements (F84.4) were excluded, as these are no longer classified as ASD in DSM-5 (American Psychiatric Association, 2013). In the Swedish clinical practice, diagnostic assessment of ASD was rare before 1990 (0.89% of the final study cohort) and a majority of the study cohort (n = 50 953 out of the total n = 54 168, i.e. 94.06%) was diagnosed after 2001, i.e. after inclusion of specialised outpatient data in the NPR. Previous studies have shown good diagnostic validity of ASD in the Swedish health registers (Idring et al., Reference Idring, Rai, Dal, Dalman, Sturm, Zander, Lee, Serlachius and Magnusson2012). The dichotomisation into ASD without ID and ASD + ID groups was based on the registered ICD diagnosis codes for intellectual disability. The ICD-8 codes 311–315 and the ICD-9 codes 317–319 were converted to the corresponding ICD-10 diagnoses mild (F70), moderate (F71), severe (F72), profound (F73), other (F78), and unspecified (F79) intellectual disability. Individuals with any co-existing intellectual disability were classified as ASD + ID regardless of which ASD diagnosis they had. The same type of classification strategy has been applied in previous studies based on ASD + ID v. ASD-IA as a key specifier of ASD in DSM-5 (Magnusson et al., Reference Magnusson, Rai, Goodman, Lundberg, Idring, Svensson, Koupil, Serlachius and Dalman2012; Idring et al., Reference Idring, Magnusson, Lundberg, Ek, Rai, Svensson, Dalman, Karlsson and Lee2014; Hirvikoski et al., Reference Hirvikoski, Mittendorfer-Rutz, Boman, Larsson, Lichtenstein and Bolte2016).
A further classification was conducted to split the autism spectrum disorder group to four different exposures of neurodevelopmental disorders: ASD without ID with/without ADHD and ASD + ID with/without ADHD, respectively. Lifetime psychiatric comorbidity with ADHD was identified from the NPR using ICD-9 codes (314J, 314W, 314X) and ICD-10 code F90. Moreover, since ADHD medication has very few indications other than ADHD [compared to many other psychoactive drugs with broader indication, e.g. selective serotonin reuptake inhibitors (SSRI) described for treatment of e.g. premenstrual dysphoric disorder and generalised anxiety disorder in addition to depression], we also used the Swedish Prescribed Drug Register to identify cases with ADHD according to The Anatomical Therapeutic Chemical (ATC) – codes N06BA01, N06BA02, N06BA04, N06BA09, and N06BA12.
Classification of suicide attempts and death by suicide
The codes for (first, if several) suicide attempts (identified from NPR) registered according to ICD-8 (E950, E952–E959, E980, E982–E989) and ICD9 (E950–E959, E980–E989) were converted into corresponding ICD-10 codes (X60–X84, Y10–Y34, Y87.0, Y87.2) using the conversion instrument provided by the Swedish National Board of Health and Welfare. Inclusion of all registered suicide attempts in the analyses (i.e. both outpatient and inpatient data), may lead to overinclusion of cases with self-harm without suicidal intent, thus compromising internal validity of the study. However, the inclusion of inpatient data only (i.e. suicide attempts with high suicidal intent leading to inpatient care) would limit the generalizability to more severe cases of suicide attempts only. Therefore, the data were analysed separately including all suicide attempts and inpatient data only, respectively.
The codes for death by suicide (identified from Cause of Death Register) according to ICD-6 (E963, E970–E979), ICD-7 (E963, E970–E979), ICD-8 (E950-E959, E980–E989), as well as ICD-9 (E950–E959, E980–E989), were converted into ICD-10 codes (X60–X84, Y10–Y34, Y87.0, Y87.2). Thus, codes for intentional self-harm/suicide X60–X84 and sequelae of intentional self-harm Y87.0 in ICD-10 were combined with undetermined suicide Y10–Y34 and sequelae of undetermined self-harm Y87.2 in ICD-10 and corresponding codes from previous ICD classifications. These codes were combined in order to limit the temporal and geographic variation in the ascertainment, and the combined measure was referred to as suicide. This practice is common in research and reporting concerning public health statistics (Mittendorfer-Rutz et al., Reference Mittendorfer-Rutz, Rasmussen and Wasserman2004; Lager et al., Reference Lager, Berlin, Heimerson and Danielsson2012). Previous sensitivity analysis has proved the comparability of the two diagnostic groups (Hirvikoski et al., Reference Hirvikoski, Mittendorfer-Rutz, Boman, Larsson, Lichtenstein and Bolte2016).
Classification of psychiatric comorbidity for covariate adjustment
Based on previous research we expected a high frequency of comorbid psychiatric condition in the ASD groups. To enable investigation of the mediating role of psychiatric comorbidity for suicidal behaviour, we identified lifetime comorbid psychiatric disorders associated with increased risk for suicidal behaviours using ICD-10 codes and corresponding ICD-9 and ICD-8 codes (Table 1). E.g. for identification of lifetime comorbidity with depressive disorders, we used ICD-8 codes 296.2, 298.0, and 300.4; ICD-9 codes 296B, 298A, 300E, and 311; as well as ICD-10 codes F32 and F33. Lifetime anxiety disorders and substance use disorders were identified using the same strategy as for the depression disorders: the ICD-10 codes for the anxiety disorders (F40 – F48.9) and for the substance use disorders (F10.10 – F19.99), as well as corresponding codes from ICD-9 and ICD-8 (a detailed list of diagnostic codes for all psychiatric diagnoses can be obtained from the corresponding author upon request). Details and frequencies of the psychiatric diagnoses are depicted in Table 1.
Statistical analyses
The lifetime diagnoses of ASD, ID, ADHD and psychiatric comorbidity, as well as the diagnoses for suicidal behaviour, were identified regardless the position of the diagnosis in the NPR (primary or secondary diagnosis).
Association of ASD with suicide attempt and death by suicide
Conditional logistic regression models were used to estimate the risk for suicidal behaviour (suicide attempt and suicide, respectively) in ASD cases relative to that in matched controls. The results were presented as odds ratios (ORs) with 95% confidence intervals (CIs). The possible modifying effect of gender on the association between ASD and suicidal behaviour was examined by gender-stratified analyses. All crude and gender-stratified analyses were conducted separately for the four subgroups: ASD without ID with/without ADHD and ASD + ID with/without ADHD. The analyses were further adjusted for family educational level, as well as psychiatric comorbidity. Due to the high frequency of psychiatric comorbidity (varying between 59 and 72% in the subgroups, Table 1), adjustment to all psychiatric diagnosis would lead to too few cases in certain cells and thus obstruct the analysis. Therefore, in the first step, the most common comorbid diagnosis (depression) was included as a single covariate. In the next steps, all psychiatric disorders that reached the frequency of at least 10% in any of the subgroups were included as covariates (i.e. depression, anxiety disorders, and substance use disorders).
Familial liability for suicidal behaviours
Conditional logistic regression models were also used to estimate the relative risk of different aspects of suicidal behaviour (suicide attempt and suicide, respectively) among relatives of ASD cases across different levels of relatedness. The entire ASD group was included in the analyses, given a potential overlapping genetic risk for the neurodevelopmental disorders ASD, ID, and ADHD (Stessman et al., Reference Stessman, Xiong, Coe, Wang, Hoekzema, Fenckova, Kvarnung, Gerdts, Trinh, Cosemans, Vives, Lin, Turner, Santen, Ruivenkamp, Kriek, Van Haeringen, Aten, Friend, Liebelt, Barnett, Haan, Shaw, Gecz, Anderlid, Nordgren, Lindstrand, Schwartz, Kooy, Vandeweyer, Helsmoortel, Romano, Alberti, Vinci, Avola, Giusto, Courchesne, Pramparo, Pierce, Nalabolu, Amaral, Scheffer, Delatycki, Lockhart, Hormozdiari, Harich, Castells-Nobau, Xia, Peeters, Nordenskjold, Schenck, Bernier and Eichler2017; Miller et al., Reference Miller, Musser, Young, Olson, Steiner and Nigg2019). Thus, we compared the odds ratios between first-degree (i.e. full-siblings), second-degree (i.e. maternal and paternal half-siblings), and third-degree (i.e. first cousins) relatives to assess the genetic and environmental contribution to the overlap between ASD and suicidal behaviour. The inclusion of relatives within the same generation was chosen to avoid confounding by changes over time in clinical routines and practices. Increased risk of suicidal behaviours among higher-degree relatives of individuals with ASD would suggest familial effects for the overlap, while the comparison of risk estimates among maternal half-siblings v. paternal half-siblings provides information about shared environmental factors. Shared environmental factors were assumed to be associated with higher risk estimates among maternal half-siblings, compared to paternal half-siblings, since offspring predominantly live with their mothers when parents separate.
In all analyses, cells included ⩽5 cases were dropped and the data are thus not shown. The alpha level was set at p < 0.05. All analyses (both case/control analyses and analyses of familial liability) were planned a priori and performed in SAS 9.4 (SAS Institute Inc., Cary, NC, USA), along with a robust sandwich estimator to supply standard errors corrected for the dependence between repeated observations within families.
Results
Association between ASD without ID with/without ADHD and suicidal behaviour
Individuals with ASD with neither ID nor ADHD, had an increased risk of both attempted suicide [OR (95% CI); 4.20 (3.96–4.46); most severe cases only i.e. suicide attempts leading to inpatient care 6.67 (6.18–7.19)] and suicide [8.13 (6.23–10.60)] compared to the matched population-based controls (Table 2). Adjustment for family education level had minimal effect on the magnitude of the risk of suicidal behaviour. After adjustment for psychiatric comorbidity (in the first step adjusted for depression only; in the second step adjusted for depression, anxiety disorders, and substance use disorders), both risk of attempted suicide and suicide attenuated substantially, but remained significantly higher compared to matched controls [after second step: attempted suicide 1.70 (1.57–1.84), inpatient data only 2.12 (1.92–2.34); suicide 4.46 (3.24–6.13)]. The association between ASD without neither ID nor ADHD, and suicidal behaviour was stronger in females [attempted suicide: 6.27 (5.72–6.88), inpatient data only 8.14 (7.31–9.06); and suicide 12.05 (6.85–21.21)] than in males [attempted suicide 3.06 (2.82–3.32), inpatient data only 5.41 (4.85–6.03); and suicide 7.19 (5.31–9.73)].
Table 2. Suicide attempts and death by suicide in ASD group without intellectual disability, with or without comorbid ADHD respectively, compared to general population controls

Note: Crude OR were not adjusted for any covariates; adjusted for SES refers to the educational level in the upbringing family. N/A not applicable due to a low number of cases in certain cells.
The risk is expressed as odds ratio, OR (95% confidence interval, CI).
In the ASD without ID group, 19 035 individuals (43.69%) also had an ADHD diagnosis. In this group, the pattern of heightened suicide risk was similar to the ASD without ID or ADHD group (Table 2), although the odds ratios were generally higher among individuals with combined ASD and ADHD [attempted suicide 7.25 (6.79–7.73); inpatient data only 12.37 (11.33–13.52); suicide 13.09 (8.54–20.08)]. Again, adjustment for psychiatric comorbidity attenuated the risk considerably, although the association remained significant [after adjustment for depression, anxiety disorders and substance use disorders: attempted suicide 2.31 (2.11–2.53), inpatient data only 2.90 (2.56–3.28); suicide 3.61 (1.94–6.71). Corresponding to the results in the ASD without ID or ADHD group, females with combined ASD and ADHD without ID had higher risk of suicide attempts [10.27 (9.27–11.37), inpatient data only 13.42 (11.87–15.18)]; than males with both ASD and ADHD [attempted suicide 5.55 (5.10–6.05), inpatient data only 11.33 (9.98–12.86)]. Thus, among females with both ASD and ADHD (without ID), every fifth individual (20.39%) had attempted suicide at least once. Regarding death by suicide however, the OR confidence intervals for females with ASD and ADHD (without ID) [14.26 (6.03–33.72)] were largely overlapping the CI for males with combined ASD and ADHD [12.72 (7.77–20.82)], thus indicating no between-group differences.
Association between ASD + ID with/without ADHD and suicidal behaviour
The ASD + ID without ADHD group had an increased risk of attempted suicide [2.60 (2.31–2.92); inpatient data only 3.45 (2.96–4.02)] (Table 3). The adjustment for family education level had little impact on the risk estimates, while the adjustment for psychiatric disorders attenuated the estimates [attempted suicide adjusted for depression, anxiety disorders and substance use disorders 2.00 (1.76–2.27); inpatient data only 2.37 (1.99–2.81)]. There we no significant gender differences in attempted suicide in the ASD + ID without ADHD group. The OR for risk of death by suicide in the ASD + ID without ADHD group [2.31 (1.16–4.57)] was based on few cases (in total n = 12 individuals with ASD + ID without ADHD had died by suicide), and the low cell number constrained possibilities to establish an association in the adjusted analyses (i.e. wide CI's overlapping 1 indicated imprecise estimation), as well as exploration of the potential role of gender differences.
Table 3. Suicide attempts and death by suicide in the ASD group with intellectual disability (ASD + ID) with or without ADHD, respectively
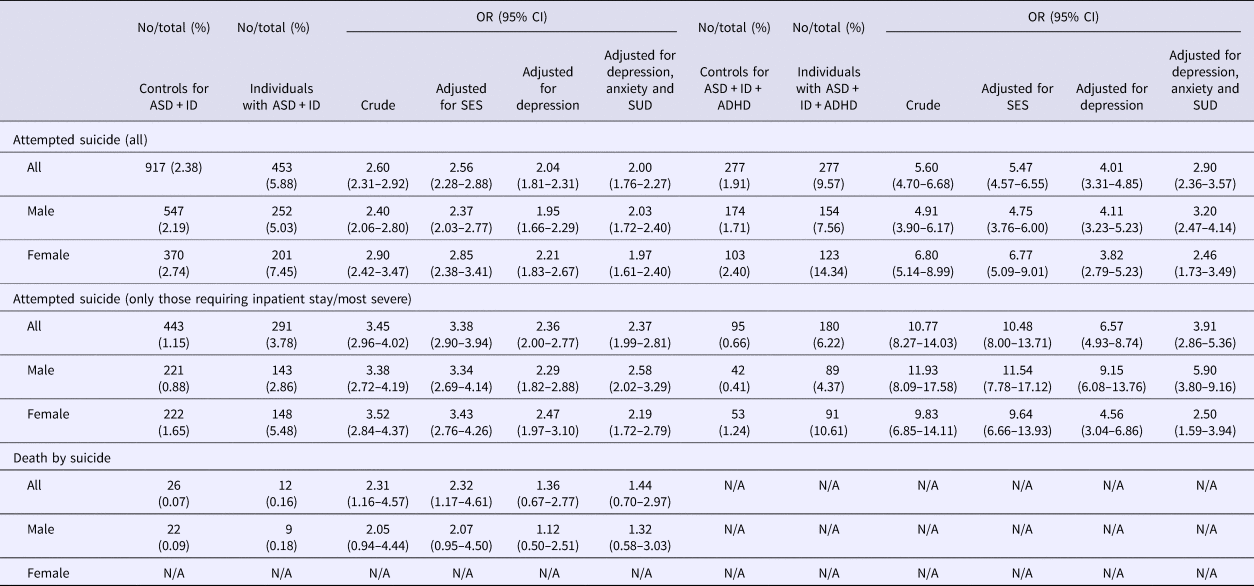
Note: Crude OR were not adjusted for any covariates; adjusted for SES refers to the educational level in the upbringing family; adjusted to psychiatric disorders includes depression and ADHD as covariates. N/A not applicable due to a low number of cases in certain cells.
Among the individuals with ASD + ID, n = 2894 individuals (27.31%) also had ADHD. In the ASD + ID + ADHD group, the OR for attempted suicide was 5.60 (4.70–6.68); inpatient data only 10.77 (8.27–14.03). Following the pattern for other groups in the current study, adjustment for family education level had a marginal impact on the risk estimates, while adjustment for psychiatric comorbidity attenuated the risk for suicide attempt [all attempts 2.90 (2.36–3.57); inpatient data only 3.91 (2.86–5.36)], although both estimates remained significant. There were no significant gender differences in the risk of attempted suicide. Suicide risk could not be analysed in the ASD + ID + ADHD group due to a small number of individuals.
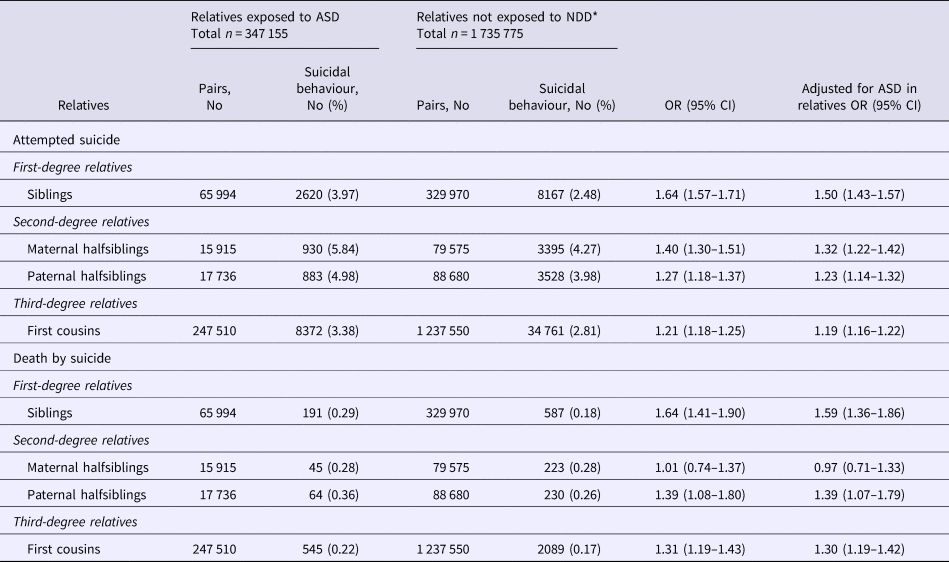
Familial liability for the association
The risk of suicide attempts, reported as OR (95% CI), was significantly increased in full siblings of individuals with ASD compared to full siblings of matched controls [1.64 (1.57–1.71)] (Table 4). The relative risks were increased (although to a lesser degree as compared to full siblings) also in half-siblings to ASD cases and were similar for maternal [1.40 (1.30–1.51)] and paternal [1.27 (1.18–1.37)] half-siblings of ASD cases. First cousins of the ASD cases were also at increased risk of attempting suicide compared to cousins of matched controls [1.21 (1.18–1.25)].
Table 4. Attempted suicide and death by suicide among relatives of individuals with ASD with or without ID and/or ADHD (ASD total n = 54 168), compared to general population controls

Note: relatives not exposed to NDD refers to neurodevelopmental disorders ASD, ID and ADHD; adjusted to ASD in relatives refers to the relatives' own diagnostic status
The frequencies are expressed as number, No (percent), and the risk increase as odds ratio, OR (95% confidence interval)of the ASD as a covariate.
The risk of death by suicide was increased in full siblings of individuals with ASD [1.64 (1.41–1.90)] as compared to siblings of the control participants. Further, the risk was increased (to a lesser degree as compared to first-degree relatives, i.e. siblings) also in paternal half-siblings [1.39 (1.08–1.80)] and cousins [1.31 (1.19–1.43)] to individuals with ASD, as compared to second- and third-degree relatives of the control participants. In the maternal half-siblings, the association could not be established [1.01 (0.74–1.37)].
Discussion
This population-based register-study analysed the risk of suicidal behaviour in individuals and families with ASD. Individuals with ASD were at an increased risk of suicidal behaviour. The risk of suicidal behaviours was highest in ASD females without ID with ADHD. Mediation by psychiatric comorbidities partially explained these associations. To the best of our knowledge, this is the first genetically informative study of ASD and suicidal behaviour. The risk of suicide attempts and death by suicide was higher in full siblings than in half-siblings, but similar for maternal and paternal half-siblings, which indicate that the shared familial effect most probably reflects underlying genetic factors rather than shared environmental factors. Such shared genetic risk factors may in part reflect a general genetic factor of psychopathology (Pettersson et al., Reference Pettersson, Larsson and Lichtenstein2016), but also specific behavioural dimensions, such as low socialization and poor problem-solving/coping skills, with a strong load on both ASD and suicidal behaviours (Hirvikoski and Jokinen, Reference Hirvikoski and Jokinen2012; Hirvikoski and Blomqvist, Reference Hirvikoski and Blomqvist2015; Turecki and Brent, Reference Turecki and Brent2016).
The ASD without ID group had a four-fold (without ADHD) to seven-fold (with ADHD) risk of attempted suicide compared to general population controls. Approximately 8% (without ADHD) to 12.5% (with ADHD) of individuals in the ASD without ID group had attempted suicide at some point during the study period, which is consistent with studies regarding suicide attempts in adolescents with ASD (Balfe and Tantam, Reference Balfe and Tantam2010; Mayes et al., Reference Mayes, Gorman, Hillwig-Garcia and Syed2013; Karakoc Demirkaya et al., Reference Karakoc Demirkaya, Tutkunkardas and Mukaddes2016), and suicidal ideation in adults with ASD (Raja et al., Reference Raja, Azzoni and Frustaci2011; Cassidy et al., Reference Cassidy, Bradley, Robinson, Allison, Mchugh and Baron-Cohen2014). The analyses restricted to the most severe cases only (inpatient register data) showed even stronger associations. In our population-based sample, 0.59% (without ADHD) and 0.40% (with ADHD) of ASD without ID individuals had died by suicide (compared to approximately 0.07 and 0.03% of matched controls, respectively). The eight-fold (without ADHD) to thirteen-fold (with ADHD) risk of death by suicide in the ASD without ID group corresponds to the previous findings based on a smaller sample of ASD without ID individuals (Hirvikoski et al., Reference Hirvikoski, Mittendorfer-Rutz, Boman, Larsson, Lichtenstein and Bolte2016). We were for the first time able to identify female gender as a distinct risk factor for attempted suicide: 13.98% (without ADHD) and 20.39% (with ADHD) of females with ASD-ID had attempted suicide as compared to 5.80% (without ADHD) and 8.95% (with ADHD) of males with ASD without ID. Despite wide confidence intervals regarding death by suicide, the female ASD without ID group also had higher suicide risk (OR 12.05 without and 14.26 with ADHD, respectively), as compared to males with ASD without ID (OR 7.19 without and 12.72 with ADHD, respectively). The higher risk in females may reflect both individual and environmental factors. Also in case of the same level of social understanding difficulties, girls with ASD exhibit more expressive social behaviours such as adjusting behaviour to a specific situation and reciprocal social skills compared to boys with ASD (Hiller et al., Reference Hiller, Young and Weber2014). Consequently, teacher report fewer concerns for girls with ASD (ibid.). The diagnosis of ASD is often established later in females, and studies also indicate that more severe comorbidity and/or cognitive problems are required before female ASD is recognised (Russell et al., Reference Russell, Steer and Golding2011). Moreover, women with ASD have reported conflicts between ASD-related characteristics and a traditional feminine identity (Bargiela et al., Reference Bargiela, Steward and Mandy2016), thus indicating a possible role of gendered socio-cultural systems and expectations for well-being in women with ASD (Lai et al., Reference Lai, Lombardo, Auyeung, Chakrabarti and Baron-Cohen2015). The complex reasons behind the high risk for suicidal behaviours in females with ASD is an important topic for future research.
In both genders in the ASD without ID, individuals with comorbid ADHD appeared to be a high-risk group regarding suicidal behaviours. This may be expected given that ADHD as such is associated with a high risk for suicidal behaviours (Ljung et al., Reference Ljung, Chen, Lichtenstein and Larsson2014), probably reduced but not abolished by pharmacological treatment of ADHD (Chen et al., Reference Chen, Sjolander, Runeson, D'onofrio, Lichtenstein and Larsson2014). Living with two disabilities (both ASD and ADHD) may imply additional and larger difficulties in everyday life, compared to individuals with ASD without ADHD. Moreover, we observed higher frequency of psychiatric comorbidity in the combined ASD + ADHD groups, especially regarding substance use disorders, an additional known risk factor for suicidal behaviours (Ferrari et al., Reference Ferrari, Norman, Freedman, Baxter, Pirkis, Harris, Page, Carnahan, Degenhardt, Vos and Whiteford2014). The association between ASD and suicidal behaviours was attenuated but remained significant when adjusted for psychiatric comorbidity (in first step depression only; in second step depression, anxiety disorders and substance use disorders). The finding that psychiatric comorbidity in part mediated the association between ASD and suicidal behaviours was expected given that psychiatric comorbidities are common in ASD (Simonoff et al., Reference Simonoff, Jones, Baird, Pickles, Happe and Charman2013; Russell et al., Reference Russell, Murphy, Wilson, Gillan, Brown, Robertson, Craig, Deeley, Zinkstok, Johnston, Mcalonan, Spain and Murphy2016) as well as strongly associated with suicidal behaviour (Ferrari et al., Reference Ferrari, Norman, Freedman, Baxter, Pirkis, Harris, Page, Carnahan, Degenhardt, Vos and Whiteford2014; Turecki and Brent, Reference Turecki and Brent2016). These findings facilitate the identification of specific risk groups among individuals with ASD. Detection and treatment of co-occurring ADHD and psychiatric comorbidity can help to reduce the risk of suicidal behaviour in ASD. However, since mediation by psychiatric comorbidity only partially explained the association between ASD and suicidal behaviour, the results also call for further studies on risk and protective factors.
In contrast to psychiatric comorbidity, we found that adjustment for family socio-economic status had a limited impact on the association between ASD and suicidal behaviour. This finding does not rule out the potential role of family-wide environmental risk factors, but indicate that other risk factors also need to be considered, such as social isolation and loneliness (Bauminger and Kasari, Reference Bauminger and Kasari2000; Rotheram-Fuller et al., Reference Rotheram-Fuller, Kasari, Chamberlain and Locke2010; Pelton and Cassidy, Reference Pelton and Cassidy2017), bullying victimization (Maiano et al., Reference Maiano, Normand, Salvas, Moullec and Aime2016), as well as experience of being a burden for family members and/or society (Pelton and Cassidy, Reference Pelton and Cassidy2017). Possible gender differences in risk and protective factors should be considered, given that the phenomenology may differ from the general population, as indicated by the results in the current study. Future research also needs to identify how service accessibility, and individual coping and communication skills are associated with suicide risk in people with ASD. The socio-communicative impairments in ASD may impede help-seeking behaviours and contact with service providers, thus being a target for interventions increasing both service availability and individual resilience.
The overall pattern of results in ASD + ID was analogous to the results of the ASD without ID group, regarding suicidal behaviours and the role of comorbid ADHD. However, the magnitude of the risk was consistently lower. Moreover, the number of ASD + ID probands was low, especially in the analyses of death by suicide, thus leading to low statistical power which also limited our possibility to analyse the role of gender and psychiatric comorbidity. In the group ASD + ID + ADHD, death by suicide could not be analysed due to a low number of individuals in almost all cells. The reasons for the lower suicide risk in ASD + ID group could not be analysed within the framework of the current study, but may be related to both individual factors (e.g. cognition) and social cohesion (such as more often living in supported housing as compared to the ASD without ID group), which may also decrease environmental risk factors (e.g. access to means) (Turecki and Brent, Reference Turecki and Brent2016).
One of the main strengths of the study was the use of longitudinal data from nationwide registers enabling the use of the entire Swedish population as study base, decreasing the risk of misclassification and eliminating the risk of selection bias, recall bias or reluctance to report sensitive data. The validity or diagnostic accuracy in Swedish registers has been shown to be good regarding both ASD diagnoses (Idring et al., Reference Idring, Rai, Dal, Dalman, Sturm, Zander, Lee, Serlachius and Magnusson2012) and mortality statistics including suicide (de Faire et al., Reference De Faire, Friberg, Lorich and Lundman1976). However, some misclassification of outcome may still occur. For example, suicidal behaviour in ASD + ID probands may have been interpreted as a part of the autism symptomatology (stereotyped behaviour), and not registered as suicidal behaviour. However, regarding rare events such as suicidal behaviour, these should not have a major impact on the estimates. To decrease the risk of misclassifications due to differences in clinical practice over time, we used matching on birth year to ensure equal follow-up time. Also in the familial analyses, relatives of different degree of relatedness were all in the same generation (siblings, half-sibling and first cousins). Moreover, use of register data may be associated with left truncation leading to misclassification of exposure (Cain et al., Reference Cain, Harlow, Little, Nan, Yosef, Taffe and Elliott2011), e.g. in our case not including individuals with ASD diagnosed in specialised outpatient services before 2001 (i.e. when outpatient data was included in the NPR). However, given that the diagnostic assessment of ASD was not as common during those years (94% of the individuals with ASD were diagnosed after 2001 in current data), we think that left truncation did not have a major impact on our results. However, we assume that the coverage rate in the Swedish NPR is lower for the ASD + ID group as compared to the ASD without ID: based on the intellectual disability, individuals with ASD + ID are sometimes identified early on within other services than psychiatric care (such as child health care centres, disability services) and thus escape the register coverage of the NPR. On the contrary, individuals with ASD without ID are diagnosed in specialised outpatient psychiatric services and thus enter the NPR also in cases with no further contact with psychiatric or other services. A further limitation regarding the identification of depression in the NPR; milder depression is often treated within primary care and not as part of specialised psychiatric care. Therefore, we most probably only included the most severe cases of depression in the adjusted analyses. A further limitation is that we used a single variable (family educational level) as a proxy for family SES. However, since the educational level is a strong predictor of both occupation and income (Sumanen et al., Reference Sumanen, Pietilainen, Lahti, Lahelma and Rahkonen2015), and had a marginal impact on the association between ASD and suicidal behaviour, we assumed that inclusion of additional (probably multicollinear) proxies for SES such as income would not improve the regression models.
Bearing the limitations of the study in mind, we have nevertheless been able to address several recommendations for studies on suicidality in ASD (Segers and Rawana, Reference Segers and Rawana2014), although we were not able to analyse the role of cultural factors and many potentially important risk and protective factors remain to be further elucidated. It should be noted that individuals with ASD may perceive and experience their context, social situations, and communication differently than typically developing individuals, and therefore may not have the same risk and protective factors, or exhibit the same type of suicidal behaviours as their typically developing peers.
Taken together, the results of this study endorse clinical management of suicidality to be established as an indispensable aspect of services for individuals with ASD. This effort may need to be extended to involve family members of individuals with ASD. Both pharmacological and non-pharmacological treatments of mental disorders can often prevent suicidal behaviour (Turecki and Brent, Reference Turecki and Brent2016). Although not much is known about diagnosis-specific interventions for suicide prevention in the context of ASD, our results further stress the need of improved access to mental health care, proper suicide risk assessment, screening for suicidal behaviours (Kato et al., Reference Kato, Mikami, Akama, Yamada, Maehara, Kimoto, Kimoto, Sato, Takahashi, Fukushima, Ichimura and Matsumoto2013), treatment of psychiatric comorbidity and regular follow-up of ASD individuals who have attempted suicide. Consolidation of environmental factors may involve the individual's closest network such as support to family members and significant others; physical environment e.g. means restriction; social environments such as interventions preventing social isolation; as well as work with increasing knowledge and reducing stigma in society regarding both ASD and mental health issues. Identification of protective factors and interventions increasing individual resilience in his or her context are key targets for future studies.
Author ORCIDs
T. Hirvikoski, 0000-0003-1824-3003
Author contribution
The study was designed by HL and TH with the assistance of MB, PL, and SB. Data were extracted and analysed by MB. TH conducted the literature search and wrote the first draft. Data interpretation was conducted by TH, HL, and MB in the first step. All authors read and commented on the manuscript, and thus participated in the final interpretation of the results.
Acknowledgements
Stockholm County Council and American Foundation for Suicide Prevention.
Conflict of interest
Tatja Hirvikoski reports no direct conflict of interest related to this article. She receives royalties for textbooks from Hogrefe. Henrik Larsson has served as a speaker for Eli-Lilly and Shire and has received research grants from Shire; all outside the submitted work. Sven Bölte reports no direct conflict of interest related to this article. Bölte discloses that he has in the last 5 years acted as an author, consultant or lecturer for Shire, Medice, Roche, Eli Lilly, Prima Psychiatry, GLGroup, System Analytic, Kompetento, Expo Medica, and Prophase. He receives royalties for text books and diagnostic tools from Huber/Hogrefe, Kohlhammer and UTB. Marcus Boman, Qi Chen, Brian D'Onofrio, Ellenor Mittendorfer-Rutz, and Paul Lichtenstein, report no conflict of interest related to this article.