Introduction
The term ‘childhood adversity’ is a broad concept which includes child maltreatment (all forms of physical and/or emotional ill-treatment, sexual abuse, neglect or negligent treatment or commercial or other exploitation), peer victimization (e.g. bullying), experiences of parental loss and separation, war-related trauma, natural disasters, and witnessing domestic or non-domestic violence (Butchart et al. Reference Butchart, Putney, Furniss and Kahane2006). About a third of the general population has a lifetime history of childhood adversity (Kessler et al. Reference Kessler, McLaughlin, Green, Gruber, Sampson, Zaslavsky, Aguilar-Gaxiola, Alhamzawi, Alonso, Angermeyer, Benjet, Bromet, Chatterji, de Girolamo, Demyttenaere, Fayyad, Florescu, Gal, Gureje, Haro, Hu, Karam, Kawakami, Lee, Lépine, Ormel, Posada-Villa, Sagar, Tsang, Ustün, Vassilev, Viana and Williams2010) and this is associated with poorer emotional wellbeing, self-harm, suicidal ideation and delinquent behaviour (Radford et al. Reference Radford, Corral, Bradley, Fisher, Bassett, Howat and Collishaw2011). Adverse childhood events also have strong associations with almost all psychiatric disorders at all life-course stages (Green et al. Reference Green, Berglund, Gruber, McLaughlin, Sampson, Zaslavsky and Kessler2010). Over the past decade, increasing interest has been shown in the relationship between childhood adversity and risk of experiencing psychotic experiences (PE) in adolescence as well as full-blown psychotic disorders in adulthood (Bebbington et al. Reference Bebbington, Bhugra, Brugha, Singleton, Farrell, Jenkins, Lewis and Meltzer2004; Morgan et al. Reference Morgan, Kirkbride, Leff, Craig, Hutchinson, McKenzie, Morgan, Dazzan, Doody, Jones, Murray and Fearon2007; Fisher et al. Reference Fisher, Jones, Fearon, Craig, Dazzan, Morgan, Hutchinson, Doody, McGuffin, Leff, Murray and Morgan2010; Arseneault et al. Reference Arseneault, Cannon, Fisher, Polanczyk, Moffitt and Caspi2011; Kelleher et al. Reference Kelleher, Keeley, Corcoran, Ramsay, Wasserman, Carli, Sarchiapone, Hoven, Wasserman and Cannon2013; Trotta et al. Reference Trotta, Di Forti, Mondelli, Dazzan, Pariante, David, Mulè, Ferraro, Formica, Murray and Fisher2013). Several reviews and meta-analyses have attempted to synthesize and quantify the magnitude of the association with onset of psychosis (Read et al. Reference Read, van Os, Morrison and Ross2005; Morgan & Fisher, Reference Morgan and Fisher2007; Bendall et al. Reference Bendall, Jackson, Hulbert and McGorry2008; Schäfer & Fisher, Reference Schäfer and Fisher2011; Varese et al. Reference Varese, Smeets, Drukker, Lieverse, Lataster, Viechtbauer, Read, van Os and Bentall2012). However, the potential long-lasting impact of traumatic early experiences on the course of PE and clinical psychotic symptoms remains a topic of controversy.
General population studies have suggested that childhood adversity may be associated not only with development but also with persistence of psychotic PE and higher symptom levels (Cougnard et al. Reference Cougnard, Mercelis, Myin-Germeys, de Graaf, Vollebergh, Krabbendam, Lieb, Wittchen, Henquet, Spauwen and van Os2007; De Loore et al. Reference De Loore, Drukker, Gunther, Feron, Deboutte, Sabbe, Mengelers, van Os and Myin-Germeys2007; Wolke et al. Reference Wolke, Lereya, Fisher, Lewis and Zammitt2013). For instance, Thapar et al. (Reference Thapar, Heron, Jones, Owen, Lewis and Zammit2012) reported that children with persistent PE have been shown to be more likely to come from adverse backgrounds and have disturbed childhood development compared to those with more transient PE. A recent meta-analysis (Linscott & van Os, Reference Linscott and van Os2013) concluded that around 20% of individuals with PE continue to have these experiences over time and the longer that PE persist for the greater risk of transition to psychosis has been shown to be (Dominguez et al. Reference Dominguez, Saka, Lieb, Wittchen and van Os2010). Thus factors which predict persistence of PE are of particular interest for prevention of psychotic disorder. Moreover, studies focusing on the course of clinically relevant psychotic disorders have demonstrated that victims of childhood adversity have poorer outcomes characterized by a higher number of suicide attempts, earlier onset of psychosis, and poor medication adherence (Garno et al. Reference Garno, Goldberg, Ramirez and Ritzler2005; Lecomte et al. Reference Lecomte, Spidel, Leclerc, MacEwan, Greaves and Bentall2008; Alvarez et al. Reference Alvarez, Roura, Osés, Foguet, Solà and Arrufat2011). However, findings are mixed concerning the impact of childhood adversity on the course of psychotic symptoms (Kim et al. Reference Kim, Kaspar, Noh and Nam2006; Davidson et al. Reference Davidson, Shannon, Mulholland and Campbell2009; Gil et al. Reference Gil, Gama, de Jesus, Lobato, Zimmer and Belmonte-de-Abreu2009; Newman et al. Reference Newman, Turnbull, Berman, Rodrigues and Serper2010; Cohen et al. Reference Cohen, Palekar, Barker and Ramirez2012). Therefore, despite some evidence suggesting that childhood adversity is related to heightened symptom levels (Ross et al. Reference Ross, Anderson and Clark1994; Heins et al. Reference Heins, Simons, Lataster, Pfeifer, Versmissen, Lardinois, Marcelis, Delespaul, Krabbendam, van Os and Myin-Germeys2011), it is still not clear what the impact is on the evolution of psychotic symptoms over time.
This study presents a systematic review of the available empirical literature, examining the impact of childhood adversity on persistence of PE and clinically relevant psychotic symptoms, focusing on trajectories of change in PE, transition to first-episode psychosis (FEP), and the course of psychotic symptoms after illness onset over time. In order to incorporate symptom trajectories at different levels of the hypothesized psychosis continuum, we focused on studies utilizing general population samples, individuals at ultra-high risk (UHR) of psychosis, patients with FEP, and patients with chronic psychosis.
Method
Literature search and selection criteria
We followed the PRISMA statement guidelines for systematic review and meta-analysis in this study (Moher et al. Reference Moher, Liberati, Tetzlaff and Altman2009). A systematic database search from 1 January 1956 up to 30 November 2014 was performed on Medline (PubMed), EMBASE and PsychINFO databases using search terms related to: (1) childhood adversity, (2) psychosis and (3) course of PE and psychotic symptoms, using the Boolean operator ‘and’ (full list provided in online Supplementary Material).
Studies were included if (a) they assessed adverse events in childhood, (b) follow-up yielded outcome data (in the PE and psychotic symptom domains), and (c) they were published in English in peer-reviewed journals. Studies were excluded if (a) they assessed adverse events that only occurred in adulthood, (b) the study involved a clinical sample that included organic aetiology of psychosis or substance-induced psychosis, with no separate data provided, and (c) clinical outcome was not explicitly defined. Childhood was defined as age ⩽18 years. UHR was defined as the presence of attenuated psychotic symptoms OR brief limited intermittent positive psychotic symptoms OR schizotypal personality disorder OR a family history of a psychotic disorder in a first-degree relative (full definition criteria can be found in Yung et al. Reference Yung, Phillips, Yuen and McGorry2004). FEP was defined as patients who were: making their first treatment contact for a psychotic disorder (schizophrenia-spectrum and affective psychoses) OR in their first admission for a psychotic disorder OR in their first episode of psychosis. Adversity included all forms of childhood abuse and neglect, parental death or separation, bullying by peers and being taken into care. Additional studies were identified by hand searching the bibliographies of each article found. Where the same study was reported in more than one publication, the dataset was only included once.
Only studies with sufficient statistical information for the computation of effects comparable to other reported studies were included. Each study was assessed using a quality assessment tool (see Supplementary material) adapted from Beards et al. (Reference Beards, Gayer-Anderson, Borges, Fisher and Morgan2013). A cut-off score of at least 11 out of 14 (>70%) was chosen to define the more ‘methodologically robust’ studies, based on criteria such as sample selection bias, measurement of exposure to childhood adversity, measurement of psychotic symptoms, and assessment of confounding.
Statistical analyses
All analyses were carried out using the meta-analysis commands of Stata v. 11 (StataCorp., 2009). We choose odds ratios (ORs) as the main outcome metric. When not reported in the primary studies, ORs and their associated standard errors were estimated from available descriptive statistics (i.e. frequencies) using standard computational techniques for dichotomous data. To examine the global association between adverse childhood events and persistence of psychotic symptoms, a meta-analysis was carried out on the effects extracted from studies providing a summary measure of exposure to childhood adversity. When this information was not available (i.e. in the absence of a summary measure of childhood adversity or studies reporting multiple effects for the associations between adverse events and specific psychotic symptoms), reports were excluded to avoid bias stemming from the violation of statistical independence. Furthermore, all analyses were also stratified by population (clinical or general population) in order to assess whether findings differed across sample types. Standardized effect sizes were meta-analysed using random-effects models. Heterogeneity between studies was assessed with the Q test (Der Simonian & Laird, Reference Der Simonian and Laird1986). The I 2 statistic was calculated to express the proportion of variation between studies that was due to heterogeneity (Higgins et al. Reference Higgins, Thompson, Deeks and Altman2003). The results are displayed using a forest plot.
Further exploration of heterogeneity was carried out using meta-regression analyses for testing effects of the following potential moderator variables: population studied (a two-level factor: clinical v. general population), inclusion of adjusted or unadjusted effect sizes, year of publication, quality score, and length of follow-up. Egger's test of publication bias was used to assess whether there was a tendency for selective publication of studies based on the nature and direction of results (Egger et al. Reference Egger, Davey Smith, Schneider and Minder1997). A significance level of p < 0.05 was used for the random-effects model, homogeneity, publication bias and meta-regression analyses.
Results
The search yielded a total of 2824 studies (Fig. 1). On the basis of title and abstract, a total of 243 studies were considered potentially relevant and the full text of each was assessed manually. Of these, 223 did not satisfy one or more of the inclusion criteria and were excluded. A summary of the 20 eligible studies and their empirical findings relating to the association between childhood adversity and persistence of psychotic phenomena is provided in Table 1. Nine were studies of general population samples, three of UHR individuals, and eight of psychosis patient samples. A total of 13 studies scored above the cut-off of ⩾11 (⩾70%) and thus were considered to have a reasonable level of methodological quality.
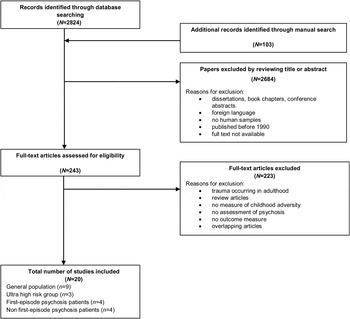
Fig. 1. Flow chart of published papers selected and excluded from the initial online database search to the publications included in the review.
Table 1. Studies included in the review which explore the association between childhood adversity and persistence of psychotic experiences or symptoms split into general population, ultra-high risk, first-episode and chronic psychosis patient samples

Adj., adjusted; CI, confidence interval; HR, hazard ratio; OR, odds ratio; s.d., standard deviation; s.e., standard error.
aNumber of participants included in the study. For references cited in Table 1, see online Supplementary material.
Childhood adversity and persistence of PE
Among the available studies, childhood adversity tended to be associated with persistence of PE over time in general population samples, with ORs ranging from 1.8 to 3.26 (Wigman et al. Reference Wigman, van Winkel, Jacobs, Wichers, Derom, Thiery, Vollebergh and van Os2011a , Reference Wigman, van Winkel, Raaijmakers, Ormel, Verhulst, Reijneveld, van Os and Vollebergh b ; Konings et al. Reference Konings, Stefanis, Kuepper, de Graaf, ten Have, van Os, Bakoula and Henquet2012). For instance, Wigman et al. (Reference Wigman, van Winkel, Jacobs, Wichers, Derom, Thiery, Vollebergh and van Os2011a , Reference Wigman, van Winkel, Raaijmakers, Ormel, Verhulst, Reijneveld, van Os and Vollebergh b ) investigated patterns of the developmental course of PE at 2 and 6 years in a sample of female twins, aged 18–45 years, and a cohort of adolescents, aged 10–11 years at baseline, respectively. The authors identified four groups with distinct developmental trajectories of low, decreasing, increasing and persistent levels of PE. In both samples, exposure to childhood adversity significantly predicted persistent PE group membership with a dose-response effect. However, PE and childhood adversity were assessed using self-report questionnaires rather than gold standard interviews which may have adversely impacted on the quality of the data obtained and the sample of twins was restricted to women thus limiting generalizability.
Another study found that child rape predicted stability of PE over time, independently of cannabis use (Murphy et al. Reference Murphy, Houston, Shevlin and Adamson2013). However, this result was not confirmed for sexual assault more broadly and other types of childhood adversity were not assessed. Additionally, Mackie et al. (Reference Mackie, Castellanos-Ryan and Conrod2011) found that bullying victimization increased the risk of persistent PE by three times in a sample of adolescents assessed over a period of 18 months. Peer victimization predicted persistent class membership over and above all the other risk factors, such as depression, anxiety and substance use. Only one study included in this section did not show evidence of association between childhood adversity and course of psychotic symptoms. Escher et al. (Reference Escher, Romme, Buiks, Delespaul and van Os2002) found that delusional ideation over a 3-year period was not significantly associated with higher levels of reported childhood adversity in adolescents who were hearing voices (hazard ratio 1.25, p = 0.100). However, the sample included only 80 adolescents, some of the subjects were quite young at the time of assessment (age range 9–19), and baseline hallucinatory experiences could also have been driving the findings.
Childhood adversity and transition to psychotic disorder
A total of three studies investigating the association between childhood adversity and transition to psychosis in individuals at high risk for psychosis were included. A high-risk 3-year cohort study, following individuals with higher than average genetic risk for psychotic disorder (van Nierop et al. Reference van Nierop, Janssens, Bruggeman, Cahn, de Haan, Kahn, Meijer, Myin-Germeys, van Os and Wiersma2013), found that transition to psychosis was associated with childhood adversity [adjusted OR 34.4, 95% confidence interval (CI) 4.4–267.4] with an estimate of 86% of transitions in this type of population attributable to childhood trauma (van Nierop et al. Reference van Nierop, Janssens, Bruggeman, Cahn, de Haan, Kahn, Meijer, Myin-Germeys, van Os and Wiersma2013). However, only nine subjects had a transition to psychosis, with eight reporting early trauma, and no adjustment for baseline psychotic symptoms was made, which could have biased the results.
Two studies conducted on individuals at UHR of psychosis, assessed the association between childhood adversity and transition to psychosis in a help-seeking clinical population with attenuated psychotic symptoms. Specifically, Bechdolf et al. (Reference Bechdolf, Thompson, Nelson, Cotton, Simmons, Amminger, Leicester, Francey, McNab, Krstev, Sidis, McGorry and Yung2010) reported that 36% of the UHR patients experienced sexual trauma and such experiences increased the chances of converting to psychotic disorder by almost three times (OR 2.96), compared to those UHR patients that did not report experiencing such adversity during childhood. However, the association fell short of statistical significance in the case of other types of childhood adversity, such as physical and emotional abuse and neglect (Bechdolf et al. Reference Bechdolf, Thompson, Nelson, Cotton, Simmons, Amminger, Leicester, Francey, McNab, Krstev, Sidis, McGorry and Yung2010). Moreover, the relationship between trauma and onset of psychotic disorder may have been confounded by the early intervention programme provided to all participants, which might have reduced the rate of conversion to psychosis. These findings were replicated in a larger UHR cohort with a longer follow-up (Thompson et al. Reference Thompson, Nelson, Yuen, Lin, Amminger, McGorry, Wood and Yung2014), confirming a positive association between experience of childhood sexual abuse and psychosis transition, such that the higher the sexual abuse score the higher was the risk of transition to a psychotic disorder in the medium-to-long term. This was not the case for other types of trauma (physical or emotional abuse or neglect). Therefore, there is some evidence for a specific association between sexual trauma and transition to psychosis in this help-seeking population.
Childhood adversity and persistence of psychotic symptoms in patients with psychotic disorders
A total of eight studies were conducted on patients with a full-blown psychotic disorder. Four studies investigated the association between childhood adversity and course of psychotic symptoms in FEP samples with mixed findings. Álvarez-Jiménez et al. (Reference Álvarez-Jiménez, Gleeson, Henry, Harrigan, Harris, Amminger, Killackey, Yung, Herrman, Jackson and McGorry2011) found that the loss of one or both parents was associated with a four-fold increased risk of having more than one psychotic episode over a 7.5-year follow-up period. However, two studies (Conus et al. Reference Conus, Cotton, Schimmelmann, McGorry and Lambert2010; Greenfield et al. Reference Greenfield, Strakowski, Tohen, Batson and Kolbrener1994) observed no significant differences between sexually and/or physically abused and non-abused psychosis patients in terms of symptomatic remission (OR 0.88, p = 0.150) or recovery over 18 months following first admission. Similarly, Uçok & Bickmaz (Reference Uçok and Bikmaz2007), in their 6-month follow-up study, reported no correlation between sexual or physical abuse and severity of positive or negative symptoms but significant correlations for emotional abuse and emotional and physical neglect. Studies on FEP focused on different types of adversity and psychosis outcomes which makes it difficult to compare their results.
A total of four studies focused on non-FEP cases. In the study by Davidson et al. (Reference Davidson, Shannon, Mulholland and Campbell2009), 55% of participants from community mental health services in Northern Ireland reported a history of childhood adversity. Although the authors reported no statistically significant differences between those with and without a history of childhood adversity in terms of the course of psychotic symptoms over time, patients who reported childhood adversity had higher positive and negative symptom scores at all the three assessments (baseline, 9 and 18 months) compared to patients who did not. Similarly, in the GROUP study sample (van Dam et al. Reference van Dam, van Nierop, Viechtbauer, Velthorst, van Winkel, Bruggeman, Cahn, de Haan, Kahn, Meijer, Myin-Germeys, van Os and Wiersma2014), individuals with childhood adversity reported higher levels of symptoms at both baseline and 3-year follow-up compared to individuals without such reports, indicating that heightened symptom levels were present over time. Interestingly, these results were consistent in unaffected siblings and controls, with those reporting trauma during childhood also having higher schizotypy levels at both baseline and follow-up. However, the association between trauma and developmental course of psychotic symptoms and schizotypy did not reach statistical significance. Similar findings come from shorter follow-up studies, with patients reporting physical or sexual abuse having higher levels of positive symptoms over 4 months and more frequent relapses over 1 year than patients not reporting abuse histories (Goff et al. Reference Goff, Brotman, Kindlon, Waites and Amico1991; Lysaker et al. Reference Lysaker, Beattie, Strasburger and Davis2005). However, the numbers of patients in these two studies was small (<100 in each study) and no other types of adversity were considered so the generalizability of these findings is limited.
Meta-analysis
Additionally, we carried out a meta-analysis of a subset of nine studies in which the ORs between adverse childhood events and persistence of psychotic symptoms had been reported (Fig. 2). Due to the low number of studies and heterogeneity of the samples of individuals at UHR of psychosis, this subgroup was excluded from the analyses. The meta-analysis for general population studies yielded a weighted OR of 1.76 (95% CI 1.19–2.32, p < 0.001), which suggests that individuals who reported childhood adversity were almost two times more likely to report persistence of PEs than those without reported adversity. However, there was significant heterogeneity between this subgroup of studies (I 2 = 58%, p = 0.049).

Fig. 2. Forest plot for the meta-analysis examining the overall association between childhood adversity and persistence of subclinical psychotic experiences and clinically relevant psychotic symptoms. CI, confidence interval; ES, effect sizes are displayed as odds ratios.
Interestingly, the OR for the clinical samples (OR 1.55, 95% CI 0.32–2.77, p = 0.007) was similar to that for the general population studies (OR 1.76, 95% CI 1.19–2.32, p < 0.001), and indicated a significant association between childhood adversity and persistence of psychotic symptoms even after illness onset. Heterogeneity did not reach significant levels in this subgroup of clinical studies (I 2 = 0%, p = 0.407) and there was no significant heterogeneity overall (I 2 = 36.4%, p = 0.114). In the meta-regression analyses, there were no effects of population studied, inclusion of adjusted or unadjusted effect sizes, year of publication, quality score, or length of follow-up (results, not shown, are available from the authors).
Discussion
The goal of this review was to combine results from existing studies exploring the association between childhood adversity and course of psychotic symptoms, which is novel for the literature. We focused on trajectories of PE in the general population, transition to psychosis in individuals at UHR, and course of psychotic symptoms in clinical samples. There were two main findings: (a) the literature on childhood adversity and course of psychotic symptoms is surprisingly small (only 20 studies spread over 23 years); (b) most studies suggest that childhood adversity impacts on the course of both PE and clinically relevant psychotic symptoms, with our meta-analysis suggesting around a two-fold increased odds of persistence of psychotic phenomena in those reporting childhood adversity compared to those who did not. Therefore, the findings of this review could be seen to provide some support for aetiological continuity between subclinical and clinical psychosis phenotypes (van Os et al. Reference van Os, Linscott, Myin-Germeys, Delespaul and Krabbendam2009). Indeed previous studies have reported that individuals who persistently reported PE were more likely to report other risk factors for schizophrenia compared to individuals with low endorsement of PE (Thapar et al. Reference Thapar, Heron, Jones, Owen, Lewis and Zammit2012). However, in clinical samples there were inconsistent findings with some studies not confirming the effect of childhood adversity on symptom course (e.g. Greenfield et al. Reference Greenfield, Strakowski, Tohen, Batson and Kolbrener1994; Davidson et al. Reference Davidson, Shannon, Mulholland and Campbell2009; Conus et al. Reference Conus, Cotton, Schimmelmann, McGorry and Lambert2010). Moreover, very few studies have been published on conversion to psychotic disorder in relation to experience of adversity and thus it is still not possible to draw any firm conclusions in the UHR group due to the lack of findings.
Methodological issues
The findings of this review should be interpreted in the context of the strengths and limitations of the studies included. A major strength is that all 20 studies included used a prospective design. This design allows us to tentatively make causal inferences regarding the association between childhood adversity and course of psychotic symptoms compared to cross-sectional studies, at least in terms of the temporal ordering of the exposure and outcome. Another important strength of the studies in this review is that data on PE was available at two or more time-points, covering the transition period between childhood and adolescence, which is considered an important stage in the development of psychotic phenomena (Thapar et al. Reference Thapar, Heron, Jones, Owen, Lewis and Zammit2012). Data on clinical psychotic symptoms was also available at different time-points, allowing tentative inferences to be made concerning potential trajectories in the prodromal phase as well as after the illness onset. Furthermore, trajectory-based analyses are more robust to occasional misreporting or temporary fluctuations in a condition compared to data collected at a single time-point (Willett & Sayer, Reference Willett and Sayer1994; Wang & Bodner, Reference Wang and Bodner2007). Finally, the prevalence rate of childhood adversity, within the studies reviewed here, varied between 8% and 39% in the general population and between 8.5% and 69.6% in clinical samples, depending on the type of childhood adversity studied. This is similar to rates found in previous reviews of adversity and psychosis onset (Read et al. Reference Read, van Os, Morrison and Ross2005; Varese et al. Reference Varese, Smeets, Drukker, Lieverse, Lataster, Viechtbauer, Read, van Os and Bentall2012).
However, there are a number of methodological limitations to the studies included in this review. A significant one is the variability in definitions and study parameters making comparisons between studies difficult and limiting the generalizability of the findings. There are currently no systematic methods of classifying adversity; so different criteria are employed for assessing the characteristics of adversity exposure (e.g. severity and frequency) making comparisons of findings between different studies or research groups very difficult (Cicchetti, Reference Cicchetti1994; Manly et al. Reference Manly, Cicchetti and Barnett1994). Instruments to assess childhood adversity generally fall into two categories: checklist or semi-structured interview. Of the studies reviewed, nine used checklists, two used a checklist that was interviewer administered, and 9 used semi-structured interviews. Thus differing rates of experiences may have been captured by the different assessment tools. Additionally, the majority of studies included in this review relied on retrospective self-reports of childhood adversity. Although self-report of childhood adversity has been criticized because of the susceptibility to memory deficiencies, it has been shown that reports of early adversity by psychosis patients appear reliable over time and between assessment methods (Fisher et al. Reference Fisher, Craig, Fearon, Morgan, Dazzan, Lappin, Hutchinson, Doody, Jones, McGuffin, Murray, Leff and Morgan2011). The assessment of outcome variables was also not uniform across the studies and heterogeneity was significant for assessment of PE in general population studies. The heterogeneity of outcome definitions as well as the different types and severity of childhood adversity included reduce the comparability and sample size for each variable, limiting the validity and relevance of conclusions.
Moreover, causal interpretations in clinical studies are limited by the small number of first-episode and non-FEP samples available and by the lower methodological quality of clinical compared to non-clinical studies. It is clear that more methodologically robust studies based on clinical samples are needed, which utilize appropriate outcome measures and objective ratings of the impact of childhood adversity. Finally, adjustment for potential confounders was inconsistent. Where adjustments were made, the majority controlled for age, gender, and ethnicity, with some controlling for a wider range of factors, such as substance use or psychotic symptoms at baseline, and education. No study adjusted for adversity occurring in adulthood which has also been associated with the onset and course of psychosis (Beards et al. Reference Beards, Gayer-Anderson, Borges, Fisher and Morgan2013).
Theoretical and clinical implications
If there is a continuum of psychosis, then it is likely that at least some of the environmental and genetic causes contributing to variation at the highest disorder level of the continuum also impact at lower levels. The psychosis proneness–persistence–impairment model, in fact, considers that some of the non-genetic risk factors associated with schizophrenia such as urbanicity, ethnic minority status, childhood adversity and cannabis use may also impact on the rate of PE (van Os et al. Reference van Os, Linscott, Myin-Germeys, Delespaul and Krabbendam2009). According to this model, developmental expression of PE is common and mostly transitory (Linscott & van Os, Reference Linscott and van Os2013). However, PE may become persistent through a mechanism of psychological and biological sensitization, depending on the degree of environmental risk the person is additionally exposed to. Persistence in turn might increase the probability of onset of impairment and need for care (Cougnard et al. Reference Cougnard, Mercelis, Myin-Germeys, de Graaf, Vollebergh, Krabbendam, Lieb, Wittchen, Henquet, Spauwen and van Os2007).
Furthermore, persistence of psychotic symptoms may be related to an underlying process of dopamine sensitization, associated with repeated exposure to environmental risk factors acting on a final common pathway (Collip et al. Reference Collip, Myin-Germeys and van Os2008; van Winkel et al. Reference van Winkel, Stefanis and Myin-Germeys2008; Howes & Murray, Reference Howes and Murray2014). Exposure to adverse experiences early in life might alter the function of the hypothalamus–pituitary–adrenal (HPA) axis, potentially leading to atypical responsiveness of the HPA axis to later stressors, which in turn may predispose to psychiatric vulnerability in later life (Read et al. Reference Read, van Os, Morrison and Ross2005; van Goozen & Fairchild, Reference van Goozen and Fairchild2008; McCrory et al. Reference McCrory, De Brito and Viding2011; Mondelli et al. Reference Mondelli, Cattaneo, Belvederi Murri, Di Forti, Handley, Hepgul, Miorelli, Navari, Papadopoulos, Aitchison, Morgan, Murray, Dazzan and Pariante2011). Elevated cortisol levels, pronounced reductions in hippocampal volume, activation of dopaminergic circuits and the impact of pre- and post-natal factors in the aetiology of schizophrenia support the hypothesis of a link between childhood adversity, HPA activity, and psychosis (Walker & Diforio, Reference Walker and Diforio1997).
Cognitive and affective mechanisms might also be involved in the persistence of psychotic phenomena. Negative perceptions of the self, anxiety, and depression have been found to partially mediate associations between early adversity and emergence of PE (Fisher et al. Reference Fisher, Schreier, Zammit, Maughan, Munafò, Lewis and Wolke2013) in keeping with cognitive models of psychosis (Garety et al. Reference Garety, Bebbington, Fowler, Freeman and Kuipers2007), though other psychological mechanisms are also likely to be involved (Bentall et al. Reference Bentall, de Sousa, Varese, Wickham, Sitko, Haarmans and Read2014). Studies have also shown that cognitive factors and depression may be involved in the maintenance of psychotic symptoms over time (Vorontsova et al. Reference Vorontsova, Garety and Freeman2013), though this has not been explored specifically in the context of adversity exposure. Therefore, there are several biological and psychological mechanisms, by which childhood adversity may not only increase risk for onset of PE and symptoms but also impact on the course of such phenomena, which merit further research attention.
Finally, it is possible that an association between childhood adversity and persistence of PE might go some way towards accounting for poorer outcomes of individuals with depression that have a history of childhood adversity. Childhood maltreatment has been associated with a more chronic course of depression (Brown et al. Reference Brown, Craig, Harris, Handley and Harvey2007) and a meta-analysis revealed that childhood maltreatment was associated with lack of response or remission during treatment for depression with psychological therapy, antidepressant medication, or combined treatment (Nanni et al. Reference Nanni, Uher and Danese2012). PE has been shown to confer a high risk for development of depression (Verdoux et al. Reference Verdoux, van Os, Maurice-Tison, Gay, Salamon and Bourgeois1999) and the presence of PE among individuals with depression has been linked to more severe depressive symptoms and worse treatment response (Wigman et al. Reference Wigman, van Nierop, Vollebergh, Lieb, Beesdo-Baum, Wittchen and van Os2012, Reference Wigman, van Os, Abidi, Huibers, Roelofs, Arntz, Kelleher and Peeters2014; van Os, Reference van Os2014). Therefore, assuming a robust association could be found between childhood adversity and persistence of PE, then it would be plausible to suggest that persistent PE might be mediating the association between childhood adversity and poorer outcome of depression. This is merely speculation and requires investigation. Moreover, it is unclear whether a history of childhood adversity would also impact on treatment outcomes in psychosis patients but this would be a useful avenue for future research in order to inform early intervention and prevention strategies.
Conclusions
This systematic review suggests that victims of childhood adversity may demonstrate a more persistent symptomatic course of clinical or subclinical psychosis compared to non-victims. However, it should be noted that much of the existing research is methodologically limited and this necessarily urges caution in drawing any firm inferences about the role of adverse childhood events in the course of psychotic disorder or PE. To date, only a few studies have focused on this issue and the broadness and the variety of outcome measures make it difficult to have a clear idea about the state of the art. Further research is warranted to develop a greater understanding of which individuals with psychosis are likely to have the poorest outcomes and whether this is associated with exposure to different forms of adversity as this would assist clinicians in targeting interventions at those patients with the highest risk of a poor prognosis. Specifically, it is clear that more methodologically robust investigations are needed into the association between childhood adversity and course of psychotic phenomena based on general population, high-risk and clinical samples, which utilize more objective ratings of a range of early adverse experiences, include well-defined outcome measures obtained prospectively over multiple time-points and take into account relevant confounders.
Supplementary material
To view supplementary material for this article, please visit http://dx.doi.org/10.1017/S0033291715000574.
Acknowledgements
Helen L. Fisher was supported by a UK Medical Research Council (MRC) Population Health Scientist fellowship (G1002366) and Antonella Trotta by the Psychiatry Research Trust.
Declaration of Interest
Robin M. Murray is an editor of this journal.





