Introduction
Current evidence suggests that childhood adversity is associated not only with depression (Heim & Nemeroff, Reference Heim and Nemeroff2001; Chapman et al. Reference Chapman, Whitfield, Felitti, Dube, Edwards and Anda2004; Wiersma et al. Reference Wiersma, Hovens, van Oppen, Giltay, van Schaik, Beekman and Penninx2009) but also with psychotic outcomes. Although reviews on the association between childhood trauma and psychosis are not consistent (Read et al. Reference Read, van Os, Morrison and Ross2005; Bendall et al. Reference Bendall, Jackson, Hulbert and McGorry2008; Larkin & Read, Reference Larkin and Read2008), numerous methodologically robust studies, including several prospective studies (Spauwen et al. Reference Spauwen, Krabbendam, Lieb, Wittchen and van Os2006; Deloore et al. Reference Deloore, Drukker, Gunther, Feron, Deboutte, Sabbe, Mengelers, van Os and Myin-Germeys2007; Schreier et al. Reference Schreier, Wolke, Thomas, Horwood, Hollis, Gunnell, Lewis, Thompson, Zammit, Duffy, Salvi and Harrison2009; Elklit & Shevlin, Reference Elklit and Shevlin2010; Arseneault et al. Reference Arseneault, Cannon, Fisher, Polanczyk, Moffitt and Caspi2011; Mackie et al. Reference Mackie, Castellanos-Ryan and Conrod2011), have all demonstrated associations between childhood trauma and psychotic symptoms/psychotic disorder (Whitfield et al. Reference Whitfield, Dube, Felitti and Anda2005; Lataster et al. Reference Lataster, van Os, Drukker, Henquet, Feron, Gunther and Myin-Germeys2006; Scott et al. Reference Scott, Chant, Andrews, Martin and McGrath2007; Shevlin et al. Reference Shevlin, Dorahy and Adamson2007, Reference Shevlin, Houston, Dorahy and Adamson2008; Kelleher et al. Reference Kelleher, Harley, Lynch, Arseneault, Fitzpatrick and Cannon2008; Fisher et al. Reference Fisher, Morgan, Dazzan, Craig, Morgan, Hutchinson, Jones, Doody, Pariante, McGuffin, Murray, Leff and Fearon2009; Freeman & Fowler, Reference Freeman and Fowler2009). The pattern of shared environmental risk indexed by childhood trauma is of major interest because depression and psychosis are found to cluster in the same individuals (Shergill et al. Reference Shergill, van Os, Murray and Keck1999; Hanssen et al. Reference Hanssen, Peeters, Krabbendam, Radstake, Verdoux and van Os2003; van Rossum et al. Reference van Rossum, Dominguez, Lieb, Wittchen and van Os2011; Varghese et al. Reference Varghese, Scott, Welham, Bor, Najman, O'Callaghan, Williams and McGrath2011) and also in the same families (Argyropoulos et al. Reference Argyropoulos, Landau, Kalidindi, Toulopoulou, Castle, Murray and Picchioni2008; Mortensen et al. Reference Mortensen, Pedersen and Pedersen2010), suggesting shared genetic liability.
There is strong evidence that genetic risk for depression is expressed in part as sensitivity to childhood trauma (Kendler & Prescott, Reference Kendler and Prescott2006; Wichers et al. Reference Wichers, Schrijvers, Geschwind, Jacobs, Myin-Germeys, Thiery, Derom, Sabbe, Peeters, Delespaul and van Os2009b;Lardinois et al. Reference Lardinois, Lataster, Mengelers, van Os and Myin-Germeys2011). Given that major depression and psychotic disorder share genetic risk, it is attractive to hypothesize that (i) genetic liability for depression moderates the effect of an environmental risk factor, such as childhood adversity, on the development of psychotic outcomes and (ii) moderation is occasioned by affective mechanisms (Fig. 1). Daily life stress sensitivity has been identified as an intermediate phenotype for both psychosis and depression; that is, it is associated with genetic risk for these disorders (Gottesman & Gould, Reference Gottesman and Gould2003; Myin-Germeys & van Os, Reference Myin-Germeys and van Os2007; Wichers et al. Reference Wichers, Myin-Germeys, Jacobs, Peeters, Kenis, Derom, Vlietinck, Delespaul and van Os2007; Lataster et al. Reference Lataster, Wichers, Jacobs, Mengelers, Derom, Thiery, van Os and Myin-Germeys2009). In addition, childhood adversity, alone and in interaction with genetic liability for depression, has been shown to increase adult daily life stress sensitivity (Glaser et al. Reference Glaser, van Os, Portegijs and Myin-Germeys2006; Wichers et al. Reference Wichers, Schrijvers, Geschwind, Jacobs, Myin-Germeys, Thiery, Derom, Sabbe, Peeters, Delespaul and van Os2009b). Stress sensitivity has also been shown to predict follow-up depressive and psychotic symptoms (Wichers et al. Reference Wichers, Myin-Germeys, Jacobs, Peeters, Kenis, Derom, Vlietinck, Delespaul and van Os2007; Lataster et al. Reference Lataster, Wichers, Jacobs, Mengelers, Derom, Thiery, van Os and Myin-Germeys2009). Therefore, genetic liability for depression may act on risk for both psychosis and depression by increasing daily life stress sensitivity (Fig. 1, hypothesis 1). However, another possibility is that genetic risk on the pathway to vulnerability is shared until the emergence of depressive symptoms themselves (Fig. 1, hypothesis 2), which may impact on the subsequent emergence of psychosis (Garety et al. Reference Garety, Kuipers, Fowler, Freeman and Bebbington2001; Freeman, Reference Freeman2007). Depressive symptomatology may induce misassignment of emotional salience, which can give rise to the onset of psychotic symptoms (van Rossum et al. Reference van Rossum, Dominguez, Lieb, Wittchen and van Os2011).
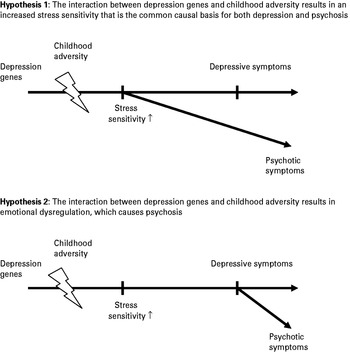
Fig. 1. Model of the hypothesized moderating influence of the genetic disposition for depression on the relationship between childhood trauma and the development of psychosis. Stress sensitivity and experience of depression are hypothesized to represent underlying mechanisms.
In the current study we examined whether genetic liability for depression moderates the effect of childhood adversity on the development of follow-up psychotic symptoms. We hypothesized that stress sensitivity or experience of depressive symptoms may represent potential mechanisms underlying this interaction (Fig. 1); that is, that the interaction between genetic liability for depression and childhood adversity is mediated by stress sensitivity or depressive symptomatology. Analyses were conducted in a large general population twin sample, making it possible to build interactive models with genetic liability for depression as hypothesized. It has been shown that psychotic experiences exist as a continuous distribution of symptoms in the general population (van Os et al. Reference van Os, Verdoux, Maurice-Tison, Gay, Liraud, Salamon and Bourgeois1999b), ranging from subclinical psychotic experiences to a psychotic disorder. The median prevalence of these psychotic experiences in the general population is 5.3%, with a median incidence of 3.1% (van Os et al. Reference van Os, Linscott, Myin-Germeys, Delespaul and Krabbendam2009). Subclinical psychosis may be more sensitive to detect associations with risk factors in general population studies. The advantage of a general population design is that effects of illness characteristics, such as medication or severe psychopathology, on the variables under examination can be avoided.
Method
Sample
The study sample consisted of 621 general population female twins and their non-twin sisters (n=44), aged 18–61 years, from Flanders, Belgium. Given the evidence for gender differences in the type of environmental stressors that are associated with psychosis (Myin-Germeys et al. Reference Myin-Germeys, Krabbendam, Delespaul and van Os2004) and depression (Kendler et al. Reference Kendler, Thornton and Prescott2001), a female-only sample was chosen to improve homogeneity. The intended age range was young to middle adulthood (mean age at baseline 27.9 years, s.d.=7.9). The sample was relatively highly educated (63% college or university degree, 36% secondary education, and 1% primary education only). The twins (218 pairs) were recruited from the East Flanders Prospective Twin Survey (EFPTS) and from birth registers of Flemish municipalities in Belgium. The EFPTS population-based survey has prospectively recorded all multiple births in the province of East Flanders since 1964 (Loos et al. Reference Loos, Derom, Vlietinck and Derom1998; Derom et al. Reference Derom, Vlietinck, Thiery, Leroy, Fryns and Derom2006). Zygosity was determined through sequential analysis based on sex, fetal membranes, blood groups, and DNA fingerprints. The project was approved by the local ethics committee and all participants gave written informed consent.
Procedure
The sample was assessed at five time points, including a baseline (T0) and four follow-up measurements (T1–T4). The average number of days between T0 and T1 was 132, 91 between T1 and T2, 116 between T2 and T3, and 91 between T3 and T4. The first interview was at individuals' homes, and follow-up data were collected using questionnaires and telephone interviews. All interviews were performed by trained research psychologists or graduate psychological assistants. The Experience Sampling Method (ESM) was only carried out at T0.
Measurements
Childhood adversity
Childhood adversity was measured at baseline (T0) using the shortened version of the 70-item Childhood Trauma Questionnaire (CTQ; Bernstein et al. Reference Bernstein, Fink, Handelsman, Foote, Lovejoy, Wenzel, Sapareto and Ruggiero1994, Reference Bernstein, Ahluvalia, Pogge and Handelsman1997; Arntz & Wessel, Reference Arntz and Wessel1996). The shortened version (Bernstein et al. Reference Bernstein, Stein, Newcomb, Walker, Pogge, Ahluvalia, Stokes, Handelsman, Medrano, Desmond and Zule2003) comprises 25 items that assess five dimensions of childhood maltreatment: (1) physical abuse, (2) emotional abuse, (3) sexual abuse, (4) physical neglect, and (5) emotional neglect. At the request of the Flemish Twin Register, the four most explicit items concerning sexual and physical abuse were omitted, resulting in a 21-item self-report questionnaire (e.g. ‘I was maltreated’, ‘I was beaten often’, ‘I was abused’, ‘There was not enough food’ and ‘I was neglected’). Items were scored on a scale from 1 (never true) to 5 (very often true). Cronbach's α for this 21-item questionnaire was 0.93.
Depressive symptoms
The Structured Clinical Interview for DSM-IV Axis I disorders (SCID-I; First et al. Reference First, Spitzer, Gibbon and Williams1998) was administered by trained psychologists to obtain current and lifetime diagnoses of major depressive disorder of both proband and co-twin. The SCID was administered twice, at baseline (T0) and at follow-up period 4 (T4).
A continuous measure of depressive symptoms was obtained using the Symptom Checklist-90 – Revised (SCL-90-R; Derogatis, Reference Derogatis1977; Arrindel & Ettema, Reference Arrindel and Ettema1986), which is a widely used 90-item self-report questionnaire measuring general psychological distress. The depression subscale consists of 13 items. The SCL-90-R was administered five times, including baseline (T0) and all four follow-up periods (T1–T4).
Psychotic symptoms
Psychotic symptoms were measured in three ways. First, SCID psychotic symptoms were assessed with SCID-I (First et al. Reference First, Spitzer, Gibbon and Williams1998). The sum score of the subscales delusions (consisting of 15 items) and hallucinations (consisting of eight items) was used to rate SCID psychotic symptoms. The SCID was administered twice, at T0 and at T4 follow-up.
Second, psychotic symptoms were assessed with the SCL-90-R (Derogatis, Reference Derogatis1977; Arrindel & Ettema, Reference Arrindel and Ettema1986). The mean score of the subscales paranoid ideation (consisting of six items) and psychoticism (consisting of 10 items) was used to rate SCL-90-R psychotic symptoms. The SCL-90-R was administered five times, that is at all T0–T4 measurement occasions.
Third, the measurement of psychotic trait liability consisted of the Community Assessment of Psychic Experiences (CAPE; Stefanis et al. Reference Stefanis, Hanssen, Smirnis, Avramopoulos, Evdokimidis, Stefanis, Verdoux and van Os2002; Hanssen et al. Reference Hanssen, Peeters, Krabbendam, Radstake, Verdoux and van Os2003; Konings et al. Reference Konings, Bak, Hanssen, van Os and Krabbendam2006), which is based on the Peters et al. Delusions Inventory (PDI; Peters et al. Reference Peters, Joseph and Garety1999), modified to also include hallucinatory experiences. The CAPE is a 42-item self-report questionnaire to assess lifetime psychotic experiences. It measures positive (20 items), negative (14 items) and depressive (eight items) dimensions of the subclinical psychosis phenotype in the general population. A new variable was created consisting of the mean score of the positive symptom dimension of the CAPE. The CAPE was administered three times, at T0 and at T2 and T4.
Stress sensitivity
Stress sensitivity was measured in daily life as appraisals of minor daily events and their effect on negative affect (NA), collected within the ESM framework. ESM is a momentary assessment technique to assess subjects in their daily living environment and has been extensively validated for the use of immediate effects of stressors on mood (Csikszentmihalyi & Larson, Reference Csikszentmihalyi and Larson1987; de Vries, Reference de Vries1992; Delespaul, Reference Delespaul1995; Wichers et al. Reference Wichers, Myin-Germeys, Jacobs, Peeters, Kenis, Derom, Vlietinck, Delespaul and van Os2007; Myin-Germeys et al. Reference Myin-Germeys, Oorschot, Collip, Lataster, Delespaul and van Os2009; Simons et al. Reference Simons, Wichers, Derom, Thiery, Myin-Germeys, Krabbendam and van Os2009; Palmier-Claus et al. Reference Palmier-Claus, Myin-Germeys, Barkus, Bentley, Udachina, Delespaul, Lewis and Dunn2011). Subjects received a digital wristwatch and a set of ESM self-assessment forms collected in a booklet for each day. The wristwatch was programmed to emit a signal (beep) at an unpredictable moment in each of ten 90-min time blocks between 0730 and 2230 h, on five consecutive days. Compliance with the ESM protocol was evaluated in a random subsample (58 subjects; 1938 observations) of the sample used in the current study and was very high (96.4%) (Jacobs et al. Reference Jacobs, Nicolson, Derom, Delespaul, van Os and Myin-Germeys2005).
Measures of daily life stress and NA were collected at each beep within the ESM framework. To measure ESM event-related stress, subjects were asked to report the most important event that happened between the current and the previous beep. This event was subsequently rated on a seven-point bipolar scale (from −3=very unpleasant, 0=neutral, to 3=very pleasant). The scale was reversed so that higher scores represent higher disliking of the event (event stress). NA was assessed at each beep with six mood adjectives (‘insecure’, ‘lonely’, ‘anxious’, ‘low’, ‘guilty’ and ‘suspicious’) rated on a seven-point Likert scale. NA was calculated by averaging the NA items weighted for the rotated factor loadings of these items obtained in principal component analysis (Cronbach's α=0.76). Stress sensitivity was defined as NA reactivity towards small daily life stressors in the flow of an individual's daily life. To create the variable stress sensitivity, the weighted mean NA was regressed on ESM event-related stress.
Statistical analysis
First, the effect of childhood adversity on the development of psychotic symptoms over the follow-up period was examined. Second, a new variable was constructed that represented the individual's genetic vulnerability to depression. This variable was coded 0 in the case of no genetic vulnerability (a twin sister without a lifetime depression diagnosis), 1 for having a dizygotic (DZ) sister with a lifetime depression diagnosis and 2 for a monozygotic (MZ) sister with a lifetime depression diagnosis (Kendler et al. Reference Kendler, Kessler, Walters, MacLean, Neale, Heath and Eaves1995; Wichers et al. Reference Wichers, Schrijvers, Geschwind, Jacobs, Myin-Germeys, Thiery, Derom, Sabbe, Peeters, Delespaul and van Os2009b). The higher an individual loads on this factor, the greater the genetic liability for major depression. To examine whether the effect of childhood adversity on follow-up psychotic outcomes was moderated by genetic vulnerability to depression, a multilevel linear regression model was used to account for clustering of multiple measurements of psychosis (level 1) within subjects (level 2) and clustering of subjects within twin pairs (level 3). Follow-up psychotic outcomes, adjusted for their baseline values, were modeled at three separate levels of (i) psychotic experiences, indexed by the SCL-90-R at T1–T4, (ii) SCID psychotic symptoms, indexed by the SCID at T4, and (iii) trait liability indexed by the CAPE positive symptom dimension at T2 and T4. Effect sizes on psychotic outcomes at different levels of genetic liability and childhood adversity were calculated from the model containing the interaction, forming the appropriate linear combinations with the STATA LINCOM routine (StataCorp, 2009). Main effects and interactions were assessed by Wald tests (Clayton & Hill, Reference Clayton, Hill, Clayton and Hill1993).
Finally, in the case of significant interaction, we examined whether stress sensitivity or depressive symptoms mediated the interaction effects on follow-up psychotic outcomes. For this purpose, the interaction model was additionally controlled for stress sensitivity or mean depressive symptoms on either the SCL-90-R or the CAPE respectively. Furthermore, follow-up psychotic outcomes were regressed on these putative mediators to demonstrate that variations in these variables significantly accounted for variations in the outcome variables, thus meeting all mediator conditions. Data were analysed with the xtreg and xtmixed modules in Stata v. 11.0 (StataCorp, 2009).
All models of psychotic outcomes were adjusted for their baseline value. By correcting for the baseline psychosis value, measures of follow-up psychotic outcomes thus indexed increase in psychotic symptomatology over the follow-up period. All variables included in the analyses were standardized (by dividing the variables by their between-subject standard deviation), yielding standardized effect sizes (β). This allows for a comparison of effect sizes across different measurements.
Results
Subjects' characteristics
Of the total sample of 621 subjects, all 44 non-twin sisters were excluded. One subject was excluded because of incorrect data on zygosity. Another 68 subjects were excluded because of missing data on either childhood adversity or co-twin lifetime depression diagnosis. This resulted in a dataset of 508 subjects (312 MZ and 196 DZ subjects), with a mean age of 27.1 years (s.d.=7.4, range 18–46). The majority of the subjects were currently employed (59.0% employed, 38.3% students, 2.4% unemployed, and 0.4% on sick leave). A small number of subjects used psychotropic medication: 21 (4.1%) used antidepressants, one (0.2%) antipsychotics, four (0.8%) anxiolytics, and eight (1.6%) hypnotics.
For all three psychosis variables, subjects were included in the analyses if at least one of the follow-up measurements was completed. Mean follow-up psychotic experience score assessed by the SCL-90-R ranged from 1 to 3.1 (median of 1.2), the sum score of follow-up psychotic symptoms assessed by the SCID ranged from 0 to 4 (median of 0), and mean follow-up psychotic liability measured by the CAPE ranged from 1 to 1.9 (median of 1.1). Owing to partial missing data on the follow-up measurements of psychotic experiences, differences in group size exist, ranging from 409 subjects for SCID measurements to 476 for SCL-90-R scores and 463 subjects for CAPE measurements. No differences could be demonstrated between subjects who dropped out after baseline compared to subjects who did not for SCL-90-R, SCID or CAPE psychotic-like symptoms.
The average childhood adversity score was 1.7 (s.d.=0.6). Sixty-one subjects (12.0%) had one or more SCID psychotic symptoms at baseline. Twenty-three subjects (4.5%) had a current depression at baseline. Eighty-seven subjects (17.2%) had a lifetime depression diagnosis. These prevalence rates are comparable to the 1-month prevalence of 3.4% and the lifetime prevalence of 20.4% reported in another female general population (Bijl et al. Reference Bijl, Ravelli and van Zessen1998). Ninety probands (17.7%) had a co-twin with a lifetime diagnosis of depression. Eleven percent of the mothers of the twins were diagnosed with depression, 0.6% with bipolar disorder, and 0.2% with a psychotic disorder. With respect to the fathers of the twins, 5.8% were diagnosed with depression, 0.8% with bipolar disorder, and 0% with a psychotic disorder. Independence of the variables of the interaction term (adversity and genetic liability for depression) was demonstrated (β=0.05, p=0.68 for the DZ twins and β=−0.04, p=0.75 for the MZ twins).
Association between childhood adversity and follow-up psychotic outcomes
Childhood adversity was associated with the development of follow-up SCL-90-R psychotic experiences (β=0.16, p⩽0.001) and with follow-up CAPE psychotic liability (β=0.13, p⩽0.001). A trend towards significance was demonstrated between childhood adversity and the development of follow-up SCID psychotic symptoms (β=0.09, p=0.08).
Moderation by genetic liability for depression
Genetic liability for depression significantly moderated the effect of childhood adversity on follow-up SCL-90-R psychotic experiences. High genetic risk was associated with a greater effect of childhood adversity on SCL-90-R psychotic experiences. MZ co-twin lifetime depression, compared to no co-twin depression (the reference category), significantly increased the effect of childhood adversity on follow-up SCL-90-R psychotic experiences, whereas the effect of DZ co-twin lifetime depression was not significantly different compared to the effect of no co-twin depression (Table 1 and Fig. 2 a). Similarly, the effect of childhood adversity on follow-up CAPE trait liability was greater for subjects with a high genetic risk for depression. MZ co-twin lifetime depression, compared to no co-twin depression, significantly increased the effect of childhood adversity on follow-up CAPE trait liability, whereas the effect of DZ co-twin lifetime depression was comparable to the effect of no co-twin depression (Table 1 and Fig. 2 b). The interaction effect on follow-up SCID psychotic symptoms was not significant.

Fig. 2. Standardized effect sizes of childhood adversity on (a) follow-up SCL-90-R psychotic symptoms and (b) follow-up CAPE psychosis scores with and without correction for possible underlying mechanisms, stratified by level of genetic vulnerability to depression. □, Interaction with childhood adversity; ![]() , interaction corrected for stress sensitivity; ▪, interaction corrected for emotional dysregulation.
, interaction corrected for stress sensitivity; ▪, interaction corrected for emotional dysregulation.
Table 1. Overview of the interaction models with β coefficient, χ2, p value, and number of subjects and twin pairs for each separate analysis on three different scales of psychotic-like symptoms (SCL-90-R, SCID and CAPE)

SCL-90-R, Symptom Checklist-90 – Revised; SCID, Structured Clinical Interview for DSM-IV Axis I disorders; CAPE, Community Assessment of Psychic Experiences; MZ, monozygotic; DZ, dizygotic; Co-Dep, co-twin lifetime depression.
a Analyses were corrected for current psychotic symptoms.
b Analyses that demonstrated a significant interaction effect were corrected for stress sensitivity.
c Analyses that demonstrated a significant interaction effect were corrected for mean depressive symptoms.
Stress sensitivity as a mediator of interaction
To examine whether stress sensitivity might represent the mechanism underlying the significant interaction effect between genetic liability for depression and childhood adversity in the models of follow-up SCL-90-R psychotic symptoms and follow-up CAPE trait liability, analyses were carried out again controlling for stress sensitivity. This did not result in a large or significant reduction of the interaction effect between genetic liability for depression and childhood adversity in the model of SCL-90-R or CAPE psychotic outcomes. If anything, controlling for stress sensitivity resulted in an increase in effect size (0.3% and 4.7% increase for SCL-90-R and CAPE respectively). Having an MZ co-twin with lifetime depression, compared to a co-twin without depression, still moderated the effect of childhood adversity in the model of both follow-up SCL-90-R psychotic experiences (Table 1 and Fig. 2 a) and follow-up CAPE trait liability (Table 1 and Fig. 2 b).
Depressive symptoms as a mediator of the interaction
Similarly, to examine whether depressive experiences might represent the mechanism underlying the significant interaction effect between genetic liability for depression and childhood adversity in the models of follow-up SCL-90-R psychotic symptoms and follow-up CAPE trait liability, analyses were carried out again controlling for mean SCL-90-R or mean CAPE depressive symptoms. This resulted in a loss of significance of the interaction effect between genetic liability for depression and childhood adversity on both the follow-up SCL-90-R and follow-up CAPE scores (a 73.6% and 64.9% decrease in effect size respectively). Having an MZ co-twin with a lifetime depression, compared to a co-twin without depression, no longer moderated the effect of childhood adversity in the model of both follow-up SCL-90-R psychotic experiences (Table 1 and Fig. 2 a) and follow-up CAPE trait liability (Table 1 and Fig. 2 b). Sensitivity analyses that excluded depressive items that overlap with negative symptoms, such as vital symptoms and anhedonia, yielded similar results. In addition, the results showed that depressive symptoms preceded the development of psychotic-like symptoms because mean baseline depressive symptoms on either the SCL-90-R or the CAPE predicted follow-up psychotic-like symptoms (β=0.23, p⩽0.001 and β=0.16, p⩽0.001 respectively).
Discussion
In this study we aimed to investigate whether genetic liability for depression acts as a moderator in the association between childhood adversity and the development of psychotic-like symptoms.
First, we demonstrated that, in general population females, genetic liability for depression moderates the association between childhood adversity and follow-up psychotic-like symptoms. In females, a high genetic risk for depression increased the effect of childhood adversity on developing psychotic-like symptomatology over the follow-up period. This finding was replicated in two separate measures of psychotic-like symptoms. The identification of genetic liability for depression as a moderator of the effect of childhood adversity on the development of follow-up psychotic-like outcomes may suggest a partially shared genetic pathway to both depression and psychosis in females (Maier et al. Reference Maier, Lichtermann, Minges, Hallmayer, Heun, Benkert and Levinson1993).
Second, two hypothesized mechanisms underlying the interaction effect in the development of follow-up psychotic-like symptoms were tested: stress sensitivity and emotional dysregulation. The upper figure in Fig. 1 depicts hypothesis 1, where increased stress sensitivity resulting from childhood adversity×genetic liability to depression is the hypothesized shared pathway to psychotic-like symptoms. Although stress sensitivity has been identified previously as an underlying intermediate phenotype for both depression and psychosis (Wichers et al. Reference Wichers, Myin-Germeys, Jacobs, Peeters, Kenis, Derom, Vlietinck, Delespaul and van Os2007; Lataster et al. Reference Lataster, Wichers, Jacobs, Mengelers, Derom, Thiery, van Os and Myin-Germeys2009), the current results support the second hypothesis in which increased risk for psychotic-like symptoms emerges from the experience of depressive symptoms rather than from increased stress sensitivity (Fig. 1, hypothesis 2). This indicates that, in females, the occurrence of depressive symptoms plays a role in the development of psychotic-like symptoms. The finding is in accordance with other studies that showed that depressive symptoms precede the onset of psychotic disorders (Häfner et al. Reference Häfner, Maurer, Trendler, an der Heiden, Schmidt and Könnecke2005, Reference Häfner, an der Heiden and Maurer2008; Owens & Johnstone, Reference Owens and Johnstone2006). Because stress sensitivity is a risk factor for future depressive symptoms (Wichers et al. Reference Wichers, Myin-Germeys, Jacobs, Peeters, Kenis, Derom, Vlietinck, Delespaul and van Os2007, Reference Wichers, Geschwind, Jacobs, Kenis, Peeters, Derom, Thiery, Delespaul and van Os2009a, Reference Wichers, Schrijvers, Geschwind, Jacobs, Myin-Germeys, Thiery, Derom, Sabbe, Peeters, Delespaul and van Osb), stress sensitivity is probably on the pathway to psychosis indirectly via a path where stress sensitivity increases the experience of depressive symptoms, which in turn induce psychotic-like symptoms. The fact that depressive symptoms may mediate the onset of psychotic-like symptoms is of relevance to the development of new effective interventions and prevention strategies to battle psychosis. Furthermore, the partially shared etiology reported in the current study [gene–environment interaction (G×E) on risk for depressive symptoms] provides an explanation for the observed co-occurrence of the two symptom clusters in psychotic patients.
Emotional processes are involved in attributing salience to experiences and are therefore undeniably involved in the development of psychotic symptoms (Verdoux et al. Reference Verdoux, van Os, Maurice-Tison, Gay, Salamon and Bourgeois1999; Birchwood, Reference Birchwood2003; Allen et al. Reference Allen, Freeman, McGuire, Garety, Kuipers, Fowler, Bebbington, Green, Dunn and Ray2005; Häfner et al. Reference Häfner, Maurer, Trendler, an der Heiden, Schmidt and Könnecke2005; Krabbendam & van Os, Reference Konings, Bak, Hanssen, van Os and Krabbendam2005; Krabbendam et al. Reference Krabbendam, Myin-Germeys, Bak and van Os2005; van Os, Reference van Os2009a, Reference van Osb). According to the cognitive model of psychosis of Garety et al. (Reference Garety, Kuipers, Fowler, Freeman and Bebbington2001, Reference Garety, Bebbington, Fowler, Freeman and Kuipers2007), stress triggers emotional and cognitive changes that can, in a biopsychosocial vulnerable individual, result in appraisals of the origins of anomalous experiences as externally caused. Externalizing appraisal, the judgment that the experience is externally caused, can lead to positive symptoms of psychosis, for example delusions. Owing to biased appraisals, emotional processes can also lead to misassignment of emotional salience to experiences. This mechanism has recently been proposed as an intermediate (cognitive) mechanism that facilitates the transition from emotional dysregulation to reality distortion (van Rossum et al. Reference van Rossum, Dominguez, Lieb, Wittchen and van Os2011). Another mechanism leading to psychosis may be the tendency to worry, which is associated with both the onset and the persistence of hallucinations (Krabbendam & van Os, Reference Krabbendam, Myin-Germeys, Bak and van Os2005). For example, the experience of auditory hallucinations has been related to higher scores on metacognitive beliefs concerning both positive beliefs about worry and negative beliefs about uncontrollability and danger (Baker & Morrison, Reference Baker and Morrison1998). Anomalous experiences can lead, by means of delusional interpretation of these experiences, to an increased tendency to worry (Freeman & Garety, Reference Freeman and Garety1999; Morrison & Baker, Reference Morrison and Baker2000) and a depressive response (Birchwood & Chadwick, Reference Birchwood and Chadwick1997; Morrison & Baker, Reference Morrison and Baker2000; Krabbendam et al. Reference Krabbendam, Myin-Germeys, Bak and van Os2005). Specific aspects of the delusional interpretation have been related to emotional distress and depression (Green et al. Reference Green, Garety, Freeman, Fowler, Bebbington, Dunn and Kuipers2006). The results also emphasize the likelihood of shared neurobiological mechanisms involved in psychosis and depression. Shared mechanisms may involve altered hypothalamic–pituitary–adrenal (HPA) axis activation (Corcoran et al. Reference Corcoran, Walker, Huot, Mittal, Tessner, Kestler and Malaspina2003; Phillips et al. Reference Phillips, McGorry, Garner, Thompson, Pantelis, Wood and Berger2006; Heim et al. Reference Heim, Newport, Mletzko, Miller and Nemeroff2008) and neurobiological sensitization mechanisms (Collip et al. Reference Collip, Myin-Germeys and van Os2008; Wichers et al. Reference Wichers, Schrijvers, Geschwind, Jacobs, Myin-Germeys, Thiery, Derom, Sabbe, Peeters, Delespaul and van Os2009b). Prevention of psychosis could take place not only at the stage of the emergence of depressive symptoms but also at the stage where certain individuals, following experience of depressive symptoms, make the transition to psychosis. Therefore, efforts should be put into elucidating the underlying mechanism of this transition and understanding how emotional, cognitive and biological factors may act together in the transition from depressive to psychotic symptoms.
Psychosis: a dimensional phenotype
No significant interaction effects on follow-up SCID scores could be demonstrated, probably because of a lack of power. Psychotic symptoms as measured using the SCID are rare in the general population and were experienced by only 38 subjects (9.3%) in this sample at the follow-up measurement. However, evidence has accumulated that the phenotype of psychosis, like other psychopathological phenotypes, is dimensional in nature (van Os et al. Reference van Os, Gilvarry, Bale, Van Horn, Tattan, White and Murray1999a, Reference van Os, Hanssen, Bijl and Ravelli2000, Reference van Os, Linscott, Myin-Germeys, Delespaul and Krabbendam2009; Stefanis et al. Reference Stefanis, Hanssen, Smirnis, Avramopoulos, Evdokimidis, Stefanis, Verdoux and van Os2002; Verdoux & van Os, Reference Verdoux and van Os2002; Krabbendam et al. Reference Krabbendam, Myin-Germeys, De Graaf, Vollebergh, Nolen, Iedema and van Os2004; Allardyce et al. Reference Allardyce, Suppes and van Os2007; Boks et al. Reference Boks, Leask, Vermunt and Kahn2007; Cougnard et al. Reference Cougnard, Marcelis, Myin-Germeys, De Graaf, Vollebergh, Krabbendam, Lieb, Wittchen, Henquet, Spauwen and van Os2007; Häfner et al. Reference Häfner, an der Heiden and Maurer2008) and that the much more frequent subclinical psychotic experiences share a similar etiological background with the more severe SCID psychotic symptoms (van Os et al. Reference van Os, Verdoux, Maurice-Tison, Gay, Liraud, Salamon and Bourgeois1999b, Reference van Os, Linscott, Myin-Germeys, Delespaul and Krabbendam2009; Olfson et al. Reference Olfson, Lewis-Fernandez, Weissman, Feder, Gameroff, Pilowsky and Fuentes2002; Stefanis et al. Reference Stefanis, Hanssen, Smirnis, Avramopoulos, Evdokimidis, Stefanis, Verdoux and van Os2002). Therefore, examining subclinical psychotic symptoms in the general population is (i) informative with regard to the clinical expression of these symptoms, (ii) has much higher power than when examining clinical symptoms or diagnosis of psychosis, and (iii) does not suffer from confounding due to medication or other disease status-associated factors, which is often the case in clinical studies. The current results showed two similar and significant interaction effects for the two separate measures of subclinical psychotic symptoms used in this study. The fact that the interaction effect between genetic liability and early adversity was replicated in another measure of psychotic-like symptoms supports the results.
Limitations
There were several methodological issues. Childhood adversity was measured with a self-report questionnaire and retrospectively. The measure for childhood adversity, the short version of the CTQ, was adapted on request of the Flemish Twin Register. Although the total average childhood adversity score may be somewhat lower because of the omission of the four most explicit items, the interaction between childhood adversity and genetic liability for depression was significant. Omission of these items may have resulted in reduced effect sizes of early adversity on psychosis. Thus, the current results probably reflect a conservative estimation of the effects in the general population. The low average childhood adversity score and its limited variability may also indicate that the subjects sample is a privileged and relatively healthy group.
Subjects were female with a high mean educational level. Because of gender differences in risk factors for different pathways to psychosis (Myin-Germeys & van Os, Reference Myin-Germeys and van Os2007), the results of the study may not be generalized to men and to those with a lower educational level.
A limitation of ESM in the measurement of stress sensitivity is that the effects between stress appraisals and NA can go in either direction. However, either explanation bears clinical relevance.
Acknowledgements
This research was supported by The Netherlands Organization for Scientific Research; the Fund for Scientific Research, Flanders and Twins, a non-profit association for scientific research in multiple births (Belgium) (to the East Flanders Prospective Survey). All twins are thanked for their cooperation. M. C. Wichers was supported by the Dutch Medical Council (VENI grant no. 916.76.147). I. Myin-Germeys was supported by a 006NARSAD Young Investigator award and by the Dutch Medical Council (VENI and VIDI grant).
Declaration of Interest
None.





