Introduction
About two-thirds of the children with attention-deficit/hyperactivity disorder (ADHD) show psychopathological signs beyond their core symptoms of inattention, hyperactivity and impulsivity. For example, elevated scores of the dysregulation profile (DP) can be diagnosed in ca. 30–40% of the cases. The DP is an independent, dimensional psychopathological construct and reflects clinically significant problems in self-regulation of emotion, attention and behavior. It is also an important indicator of severe general psychopathology and long-term psychosocial impairment (Ayer et al., Reference Ayer, Greaves-Lord, Althoff, Hudziak, Dieleman, Verhulst and van der Ende2013; De Caluwé et al., Reference De Caluwé, Decuyper and De Clercq2013; Deutz et al., Reference Deutz, Geeraerts, van Baar, Deković and Prinzie2016; Jordan et al., Reference Jordan, Rescorla, Althoff and Achenbach2016; Wang et al., Reference Wang, Brueni, Isensee, Meyer, Bock, Ravens-Sieberer, Klasen, Schlack, Becker and Rothenberger2018).
Best known is the DP measure originating from the Child Behavior Check List (CBCL) as a composite of the three subscales Aggressive Behavior, Anxious-Depressed and Attention Problems (Biederman et al., Reference Biederman, Petty, Day, Goldin, Spencer, Faraone, Surman and Wozniak2012). In addition, a more concise but equally psychometrically valid and highly correlated DP was derived from the Strengths and Difficulties Questionnaire (SDQ; German version: Woerner et al., Reference Woerner, Becker and Rothenberger2004) by Holtmann et al. (Reference Holtmann, Becker, Banaschewski, Rothenberger and Roessner2011).
Since EEG neurofeedback (NF) directly targets cortical self-regulation, it may be assumed that this operant learning procedure could be an adequate approach in order to treat self-regulation abilities as reflected in DP scores. NF has already shown positive clinical effects on ADHD and associated conduct and emotional problems (Gevensleben et al., Reference Gevensleben, Holl, Albrecht, Vogel, Schlamp, Kratz, Studer, Rothenberger, Moll and Heinrich2009a; Meisel et al., Reference Meisel, Servera, Garcia-Banda, Cardo and Moreno2013; Konicar et al., Reference Konicar, Veit, Eisenbarth, Barth, Tonin, Strehl and Birbaumer2015; Aggensteiner et al., Reference Aggensteiner, Brandeis, Millenet, Hohmann, Ruckes, Beuth, Albrecht, Schmitt, Schermuly, Wörz, Gevensleben, Freitag, Banaschewski, Rothenberger, Strehl and Holtmann2019). In our randomized controlled trial (Gevensleben et al., Reference Gevensleben, Holl, Albrecht, Vogel, Schlamp, Kratz, Studer, Rothenberger, Moll and Heinrich2009a; 6-month follow-up: Gevensleben et al., Reference Gevensleben, Holl, Albrecht, Schlamp, Kratz, Studer, Rothenberger, Moll and Heinrich2010), NF turned out to be superior to a computerized attention skills training (AST) that was designed as similarly as possible concerning the setting and the demands placed upon the participants. We obtained medium between-group effect sizes regarding ADHD symptom severity and small-to-medium effect sizes for conduct disorder-related scales.
NF in our trial comprised slow cortical potential (SCP) NF and θ/β NF, which belong to the ‘standard’ NF protocols for ADHD (Arns et al., Reference Arns, Heinrich and Strehl2014b). Comparing the effects of these two NF protocols at the behavioral level, comparable reductions of ADHD symptoms were found. Subsequent analysis of EEG and event-related potentials (ERP) indicated specific findings concerning the prediction of the clinical outcome and specific associations between clinical and neurophysiological changes. For example, higher pre-training θ activity in the resting EEG was a positive predictor for θ/β training while lower α activity was associated with a better outcome after SCP NF. The α activity and the contingent negative variation (CNV), a SCP component reflecting preparation processes, explained about 30% of the variance of the outcome after SCP NF (Gevensleben et al., Reference Gevensleben, Holl, Albrecht, Schlamp, Kratz, Studer, Wangler, Rothenberger, Moll and Heinrich2009b; Wangler et al., Reference Wangler, Gevensleben, Albrecht, Studer, Rothenberger, Moll and Heinrich2011).
None of the NF studies in ADHD conducted thus far considered whether NF also exerts positive effects on the DP. The aim of our present analysis was to compare DP effects of SCP NF and θ/β NF using data from our previous trial mentioned above and including only those children with a clinically significant SDQ-DP score (⩾3).
We expected larger effects for SCP NF than for θ/β NF as SCP NF is associated with the phasic regulation of cortical excitability, whereas θ/β NF addresses tonic aspects of cortical activation (Gevensleben et al., Reference Gevensleben, Kleemeyer, Rothenberger, Studer, Flaig-Röhr, Moll, Rothenberger and Heinrich2014; Van Doren et al., Reference Van Doren, Heinrich, Bezold, Reuter, Kratz, Horndasch, Berking, Ros, Gevensleben, Moll and Studer2017).
Furthermore, we tested the NF protocols against the AST control condition in order to estimate the clinical significance of the NF results.
Finally, we were interested to see whether EEG- and ERP-based predictors of NF regarding ADHD symptomatology were also related to the DP to learn more about the underlying processes.
Material and methods
Detailed descriptions of design and procedures of the RCT (trial registry: ISRCTN87071503). Comparison of NF and computerized AST in children with ADHD (http://www.controlled-trials.com/ISRCTN87071503) can be found in our previous papers (Gevensleben et al., Reference Gevensleben, Holl, Albrecht, Vogel, Schlamp, Kratz, Studer, Rothenberger, Moll and Heinrich2009a, Reference Gevensleben, Holl, Albrecht, Schlamp, Kratz, Studer, Wangler, Rothenberger, Moll and Heinrichb, Reference Gevensleben, Holl, Albrecht, Schlamp, Kratz, Studer, Rothenberger, Moll and Heinrich2010; Wangler et al., Reference Wangler, Gevensleben, Albrecht, Studer, Rothenberger, Moll and Heinrich2011).
Participants
Children with ADHD (aged 8–12 years) had been included in the trial. Ninety-four children (NF: 59 children, AST control group: 35 children) had completed their treatments. From the NF group, 30 children (ca. 50%) with a SDQ-DP score ⩾ 3 (range 3–6) at pre-treatment and available SDP-DP ratings at all three measurement points could be included in the present analysis. Also, 18 (ca. 50%) children of the AST control group fulfilled these criteria. Further both groups had similar baseline scores of the SDQ-DP (NF: 3.98; AST: 3.89).
As cut-off score for the SDQ-DP score, the value of 3 was chosen because it represents the mean of outpatient groups with children who were diagnosed with ADHD by experts in private offices and considered to be treated. For example, an actual evaluation of the ADORE dataset with n = 2199 children with ADHD (Rothenberger et al., Reference Rothenberger, Coghill, Döpfner, Falissard and Steinhausen2006) yielded a mean SDQ-DP score of 2.83 (s.d.: 1.97).
Diagnostics including a semi-structured clinical interview (CASCAP-D, Döpfner et al., Reference Döpfner, Berner, Flechtner, Lehmkuhl and Steinhausen1999) were conducted by a child and adolescent psychiatrist or a clinical psychologist, supervised by a board-certified child and adolescent psychiatrist. All children fulfilled DSM-IV criteria for ADHD (American Psychiatric Association, 1994) as confirmed with the Diagnostic Checklist for Hyperkinetic Disorders/ADHD (Döpfner and Lehmkuhl, Reference Döpfner and Lehmkuhl2000).
Children with comorbid disorders other than conduct disorder, emotional disorders, tic disorders, and dyslexia were excluded as were patients with gross neurological or other organic disorders. The major part of the children included was drug-naïve, and the remaining children were at least drug-free for 6 weeks before participating in the trial. Sample characteristics are summarized in Table 1.
Table 1. Sample characteristics
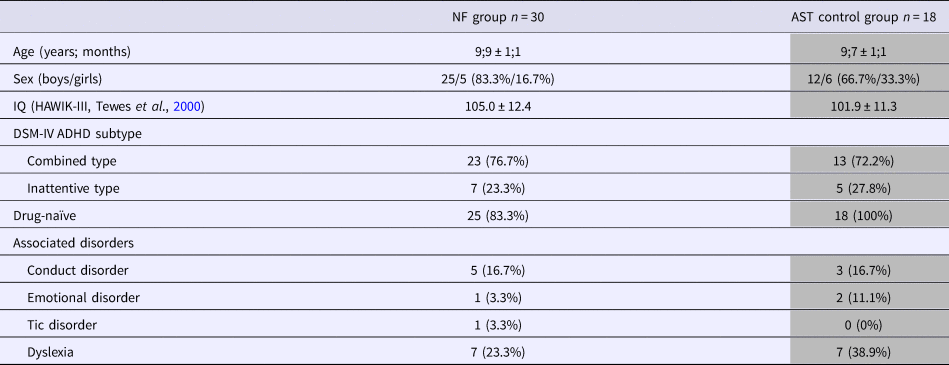
ADHD children of the NF group and the AST control group from Gevensleben et al. (Reference Gevensleben, Holl, Albrecht, Vogel, Schlamp, Kratz, Studer, Rothenberger, Moll and Heinrich2009a) with a higher SDQ dysregulation score (⩾3) and SDQ ratings at all assessments of the trial are considered
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The study was approved by the local ethics committees of the participating clinics. Assent was obtained from the children and written informed consent from their parents.
Procedure
Children participated in 36 sessions of NF training divided into two treatment blocks of 18 units each. Half of the children started with SCP NF, half of the children began with θ/β NF (counterbalanced order). In the second block, the other NF protocol was applied (cross-over) so that comparisons between the two NF protocols at the intraindividual level were possible.
At each visit, two training units of 50 min each were conducted (double sessions). Two to three visits per week took place. Between the two treatment blocks, there was a break of 2–3 weeks.
Assessments at the behavioral and neurophysiological level were conducted in the week before treatment started (pre-treatment testing/baseline), between the two blocks (intermediate testing) and in the week after the end of the treatment (post-treatment testing).
Neurofeedback
Children completed their treatments in pairs, with each child working at one computer. NF was administered by clinical psychologists supported by a student assistant.
For SCP NF and θ/β NF, the software ‘SAM’ developed by our group was used which contains different feedback animations in form of simple computer games. Feedback was calculated from electrode Cz (for details on methodical and technical settings, see Gevensleben et al., Reference Gevensleben, Holl, Albrecht, Schlamp, Kratz, Studer, Wangler, Rothenberger, Moll and Heinrich2009b).
In SCP NF, negative and positive SCPs (equal probability, random order) were addressed. The children had to find appropriate strategies to direct a ball upwards (negativity trials) or downwards (positivity trials). For successful neuroregulation, e.g. points could be earned in a computer game. Children were told that negative (resp. positive) SCPs are associated with an attentive (resp. relaxed) state. A training unit consisted of 100–120 trials of 8 s (baseline phase: 2 s; feedback phase: 6 s) divided into 2–3 runs of 40–60 trials.
In θ/β NF, children were instructed to reach a relaxed but attentive state and to find individual strategies to get into such a state by decreasing activity in the θ band of the EEG (4–8 Hz) and increasing activity in the β band (13–20 Hz). A bar on the left of the screen (representing θ activity) had to be reduced while simultaneously a bar on the right (representing β activity) had to be increased. If both criteria were fulfilled, e.g. a boy on a rope moved ahead.
A training unit consisted of about five or six trials of 5 min each, or up to three trials of 10 min each. Baseline values of θ and β activity were determined at the beginning of each visit (3 min).
Interpreting NF as a neurobehavioral approach (Gevensleben et al., Reference Gevensleben, Kleemeyer, Rothenberger, Studer, Flaig-Röhr, Moll, Rothenberger and Heinrich2014), it was also addressed how to apply the acquired regulation skill in daily life. As a first step regarding generalization, the so-called transfer trials (i.e. trials without contingent feedback) were applied (ca. 40% in the beginning of a treatment block and ca. 60% at the end of a treatment block). In the course of a treatment block, children were instructed to practice their strategies in certain daily life situations (e.g. ‘try to be very focused while reading’) and to document it in a log. These exercises did not differ between the NF protocols.
Attention skills training
For the AST, the German learning software ‘Skillies’ (Auer-Verlag, Donauwörth, Germany) was used which contains exercises that address, e.g. visual and auditory perception, vigilance, and sustained attention.
The control condition was designed as similarly as possible concerning the setting and the demands placed upon the participants (e.g. same number of training units, same trainer, comparable quality and quantity of interaction, addressing transfer into daily life).
Questionnaires
For the analysis in the present paper, we only considered parental ratings.
The SDQ consists of 25 items with each item rated from 0 (‘not true’) to 2 (‘certainly true’). They address both positive and negative attributes. The traditional outcome measures are the total difficulties score as well as the five subscales emotional symptoms, conduct problems, hyperactivity, peer problems, and prosocial behavior.
The SDQ-DP score (maximum value: 10) comprises the five items ‘Restless, overactive, cannot stay still for long’ (2), ‘Many worries, often seems worried’ (8), ‘Often fights with other children or bullies them’ (12), ‘Often unhappy, down-hearted or tearful’ (13), and ‘Steals from home, school or elsewhere’ (22).
The German ADHD rating scale (FBB-HKS) comprises 20 items related to DSM-IV and ICD-10 criteria for ADHD and hyperkinetic disorders, respectively. The severity of each item is rated from 0 (‘not at all’) to 3 (‘notably’). Besides the FBB-HKS total score (mean value of all 20 items; primary outcome measure of the trial), we also considered the inattention subscale (nine items) and the hyperactivity/impulsivity subscale (11 items).
EEG and ERP measures
The following measures had turned as significant predictor variables regarding the reduction of ADHD symptoms: α activity in the resting EEG (eyes-open condition) over posterior electrode sites as well as the CNV recorded over the vertex (electrode Cz) in spatial cue trials of the attention network test for SCP NF and θ activity in the resting EEG (eyes-open condition over parietal midline electrodes for θ/β NF (for details regarding EEG/ERP data acquisition and analysis, see Gevensleben et al., Reference Gevensleben, Holl, Albrecht, Schlamp, Kratz, Studer, Wangler, Rothenberger, Moll and Heinrich2009b and Wangler et al., Reference Wangler, Gevensleben, Albrecht, Studer, Rothenberger, Moll and Heinrich2011).
Statistics
A paired-sample t test was computed to compare θ/β NF and SCP NF effects on the SDQ-DP score. Effect sizes (Cohen's d) for a NF protocol were calculated as the difference of a measure from the assessment before the block started to the assessment after the block divided by the standard deviation of the difference score.
For the comparison of the NF protocols with the AST control condition, unpaired t tests were used. For this analysis, two measurements from each child of the AST group (change from pre-treatment to intermediate assessment and change from the intermediate assessment to post-treatment) were included to enhance the statistical power.
Between-group effect sizes (Cohen's d) were calculated as the difference of the change score for a NF protocol and the change score in the AST control group divided by the pooled standard deviations of these change scores.
Regarding the other SDQ scales and the FBB-HKS scores, the same statistical procedures were applied.
We computed Pearson correlation coefficients between the EEG/ERP measures that turned out as significant predictors of treatment outcome (for ADHD core symptoms) of the NF protocols in Gevensleben et al. (Reference Gevensleben, Holl, Albrecht, Schlamp, Kratz, Studer, Wangler, Rothenberger, Moll and Heinrich2009b) and Wangler et al. (Reference Wangler, Gevensleben, Albrecht, Studer, Rothenberger, Moll and Heinrich2011) and the SDQ-DP score at pre-treatment (baseline) considering all participants of the NF group with sufficient EEG signal quality (i.e. including all participants irrespective of the SDQ-DP score).
IBM SPSS Statistics (version 21.0) was used for statistical testing. According to the suggestion of Benjamin et al. (Reference Benjamin, Berger, Johannesson, Nosek, Wagenmakers, Berk, Bollen, Brembs, Brown, Camerer, Cesarini, Chambers, Clyde, Cook, De Boeck, Dienes, Dreber, Easwaran, Efferson, Fehr, Fidler, Field, Forster, George, Gonzalez, Goodman, Green, Green, Greenwald, Hadfield, Hedges, Held, Ho, Hoijtink, Hruschka, Imai, Imbens, Ioannidis, Jeon, Jones, Kirchler, Laibson, List, Little, Lupia, Machery, Maxwell, McCarthy, Moore, Morgan, Munafó, Nakagawa, Nyhan, Parker, Pericchi, Perugini, Rouder, Rousseau, Savalei, Schönbrodt, Sellke, Sinclair, Tingley, Van Zandt, Vazire, Watts, Winship, Wolpert, Xie, Young, Zinman and Johnson2018), the threshold for significance regarding our main question (i.e. intraindividual comparison of SCP v. θ/β NF effects on the SDQ-DP score) was defined as p < 0.005 (two-tailed) to reduce the probability of a false-positive (new) finding. For the other tests, p < 0.05 was used as threshold for statistical significance.
The achieved power was calculated using G*Power 3.1 (University of Kiel, Germany).
Results
Table 2 summarizes the comparison between SCP NF and θ/β NF regarding the SDQ and the FBB-HKS scores.
Table 2. NF group (n = 30): SCP NF v. θ/β NF
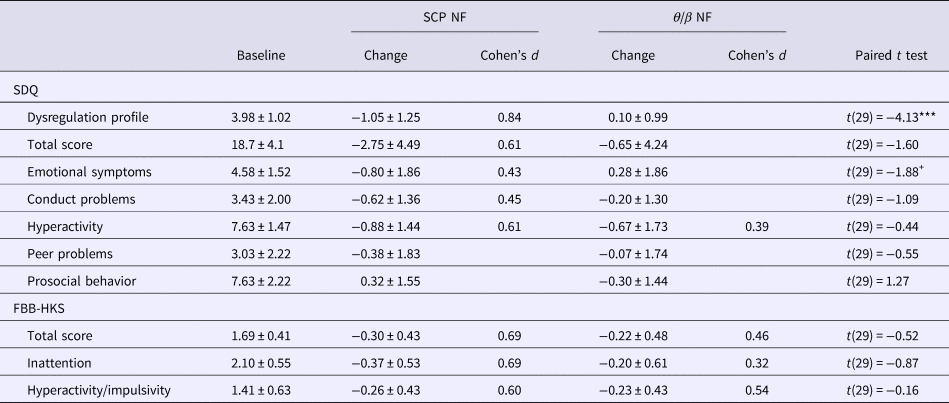
Change = value at assessment before the block started minus the value at the assessment after the block (negative values indicate improvement, except SDQ prosocial behavior). Means ± s.d. are reported. Only effect sizes (Cohen's d) ⩾0.3 are listed. +p < 0.1, ***p < 0.001
A highly significant effect was obtained for the SDQ-DP score [t(29) = −4.13; p < 0.001] indicating an advantage for SCP NF over θ/β NF. After the SCP NF block, the SDQ-DP score was reduced by about 26% (large effect size; Cohen's d = 0.84). For an error probability of 0.005 and a correlation between the two measures of 0.09, the achieved power was about 0.85.
As for the complete NF group considered in Gevensleben et al. (Reference Gevensleben, Holl, Albrecht, Vogel, Schlamp, Kratz, Studer, Rothenberger, Moll and Heinrich2009a), there were no statistically significant differences between SCP NF and θ/β NF regarding ADHD symptom severity, though, overall, there was a tendency for slightly larger effects for SCP NF.
The comparison of the NF protocols with the AST control condition further supported the positive effect of SCP NF on the DP as reflected in an effect size of 0.77 (p = 0.003). Reductions in the SDQ-total score, the FBB-HKS total score, and the FBB-HKS inattention subscale were also significantly larger compared with the control condition (p < 0.05), whereas no significant results were found for the θ/β NF block (see Supplementary Table S1 for detailed results).
Since only SCP NF had a significant effect on the SDQ-DP score, only predictor variables related to this NF protocol were considered further. Neither did the CNV (spatial cue condition of the attention network test) and α activity (eyes-open resting EEG at posterior recording sites) correlate with the SDQ-DP at pre-treatment nor were these EEG-related measures associated with the reductions in the SDQ-DP score after the SCP NF block (|r| < 0.1, n.s.).
Discussion
In our analysis, we considered data from a previous trial of our group and investigated the effects of NF standard protocols on self-regulation skills in a broader psychopathological way as reflected in the DP.
Comparing SCP NF and θ/β NF at the intraindividual level in children with ADHD with elevated DP scores, SCP NF (which is associated with the phasic regulation of cortical excitability) was superior to θ/β NF (which is related to tonic aspects of cortical activation) regarding the DP profile (measured via the SDQ). This was in line with our hypothesis. No significantly different effects regarding the reduction of ADHD symptom severity were found between SCP NF and θ/β NF, which is in line with our previous paper including children irrespective of their DP scores (Gevensleben et al., Reference Gevensleben, Holl, Albrecht, Vogel, Schlamp, Kratz, Studer, Rothenberger, Moll and Heinrich2009a). A comparable result pattern was obtained in a between-group analysis comparing the NF protocols with an AST, thus strengthening the DP-related finding for SCP NF.
Interestingly, the effect size regarding the SDQ-DP score (0.84) was even larger than those obtained for ADHD-related measures (⩽0.69). It has to be taken into account that a treatment block for a NF protocol only comprised 18 units. This number of treatment units is rather low compared with other trials with typically 25–40 sessions (Van Doren et al., Reference Van Doren, Arns, Heinrich, Vollebregt, Strehl and Loo2018). However, our design allowed us to compare SCP NF and θ/β NF intraindividually, which provides a higher statistical power (in the present analysis, the achieved power was 0.85) but probably at the cost of reduced effect sizes.
At pre-treatment, the average SDQ-DP score in our two samples was about 4 and a value of 6 reflecting the highest score. So, it remains open whether comparable results would be obtained for children with ADHD showing extremely high DP scores (up to 10).
Differences in emotional dysregulation are frequently observed between boys and girls (Kunze et al., Reference Kunze, Wang, Isensee, Schlack, Ravens-Sieberer, Klasen, Rothenberger and Becker2018). As our sample mainly consisted of boys it cannot be answered to what extent the observed effects are gender-specific.
Considering indication criteria for distinct NF protocols, our finding implicates preferring SCP NF v. θ/β NF in children with ADHD with a SDQ-DP score ⩾ 3. A SDQ-DP score of 3 is almost 1.5 s.d. above the mean value of representative community samples. The German BELLA sample of n = 2141 children (Ravens-Sieberer et al., Reference Ravens-Sieberer, Kurth, Wittchen, Rothenberger and Schulte-Markwort2008, Reference Ravens-Sieberer, Klasen and Rothenberger2015) presented with a mean SDQ-DP score of 1.17 (s.d.: 1.39), which is similar to the independent German SDQ normative sample (Woerner et al., Reference Woerner, Becker and Rothenberger2004; Holtmann et al., Reference Holtmann, Becker, Banaschewski, Rothenberger and Roessner2011)
We had already identified EEG and ERP measures as predictor variables before. Neither EEG α activity nor the CNV was correlated with the SDQ-DP score, i.e. they reflect different aspects and processes, respectively. It will be an important and challenging task to develop multivariate statistical models with predictor variables from different levels and multidimensional outputs (beyond ADHD core symptoms). Such models can only be developed based on larger multicenter trials.
Specificity of NF
There is an ongoing debate whether NF is primarily a ‘placebo’ treatment (e.g. Thibault et al., Reference Thibault, Veissière, Olson and Raz2018 v. Pigott et al., Reference Pigott, Cannon and Trullinger2018). In our opinion, there is clear evidence for specific effects for different EEG-NF protocols – not only regarding ADHD (e.g. Arns et al., Reference Arns, Feddema and Kenemans2014a; Gevensleben et al., Reference Gevensleben, Kleemeyer, Rothenberger, Studer, Flaig-Röhr, Moll, Rothenberger and Heinrich2014; Strehl et al., Reference Strehl, Aggensteiner, Wachtlin, Brandeis, Albrecht, Arana, Bach, Banaschewski, Bogen, Flaig-Röhr, Freitag, Fuchsenberger, Gest, Gevensleben, Herde, Hohmann, Legenbauer, Marx, Millenet, Pniewski, Rothenberger, Ruckes, Wörz and Holtmann2017; Wangler et al., Reference Wangler, Gevensleben, Albrecht, Studer, Rothenberger, Moll and Heinrich2011) but also in other fields (e.g. Gruzelier et al., Reference Gruzelier, Holmes, Hirst, Bulpin, Rahman, van Run and Leach2014). The differential outcome pattern for different NF protocols (i.e. SCP NF v. θ/β NF) in the present analysis further supports this notion.
Possible implications beyond ADHD
The DP indicates problems in self-regulation concerning cognitive (attention, worries), emotional (sadness, anger), and behavioral (fights, steals, restlessness) aspects. SCP NF might enhance self-regulation skills on an even broader level than primarily attention and hyperactivity in children with ADHD. The SDQ-DP combines internalizing and externalizing problems across diagnostic categories and often reflects precursors of ‘hard to treat’ behavioral or personality disorders (such as borderline personality disorder; Sharp and Tackett, Reference Sharp and Tackett2014). SCP NF as a module to be initiated early in the treatment of children with regulation deficits on multiple levels might attenuate the course of such disruptive disorders.
As calculated from our reference samples mentioned above, a SDQ-DP score of 4 (mean of this sample and about 2 s.d. above the norm) can be found in about 7% of the community samples of children and in 35% of clinical samples. Hence, our finding may suggest that this clinically significant SDQ-DP score may be an indication criterion not only for a broader and deeper clinical assessment, but also to consider SCP NF as a potential treatment approach (irrespective of ADHD diagnosis).
Conclusion
While SCP NF and θ/β NF appeared to be equally effective in reducing ADHD core symptoms, SCP NF was found to be superior to θ/β NF in reducing elevated DP scores associated with problems in self-regulation of cognition, emotion, and behavior. This finding may contribute to the individualization of NF in ADHD and may suggest to apply SCP NF in the treatment of early-onset multi-level regulation deficits of combined internalizing and externalizing symptoms, often indicating a serious course of disorders.
The differential effect of the two NF protocols on the DP provides further evidence for the specificity of NF effects in ADHD.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291718004130.
Author ORCIDs
Hartmut Heinrich, 0000-0002-8156-489X.
Acknowledgement
The authors are grateful to the participating children and their families and they also thank all colleagues in Göttingen, Erlangen, and Munich contributing to the trial. The suggestions of the two anonymous reviewers regarding our evaluation procedure that helped to strengthen our results are also much appreciated.
Author contributions
AR initiated this paper. HH conducted the analysis. AB contributed important methodical input. HH, HG, and AR wrote the manuscript. All authors approved the manuscript.
Financial support
The original trial had been supported by the German Research Foundation (HE 4536/2, MO 726/2, RO 698/4).
Conflict of interest
None.




