Introduction
The level of substance use in patients with severe mental illness is known to be high. This includes the diagnostic groups of both schizophrenia and bipolar disorder, but the prevalence of substance use in these groups varies considerably across studies (Regier et al. Reference Regier, Farmer, Rae, Locke, Keith, Judd and Goodwin1990; Mueser et al. Reference Mueser, Yarnold and Bellack1992; Cassidy et al. Reference Cassidy, Ahearn and Carroll2001; Kilbourne et al. Reference Kilbourne, Cornelius, Han, Pincus, Shad, Salloum, Conigliaro and Haas2004; Green et al. Reference Green, Young and Kavanagh2005; Swartz et al. Reference Swartz, Wagner, Swanson, Scott Stroup, McEvoy, Canive, Miller, Reimherr, McGee, Khan, Van Dorn, Rosenheck and Liebermann2006). Studies of the general population indicate differences in the prevalence of non-alcoholic drug use across different countries, and a varied prevalence of individual drug use across studies (Rehm et al. Reference Rehm, Room, van den Brink and Kraus2005; European Monitoring Centre for Drugs and Drug Addiction, 2006; Norwegian Institute for Alcohol and Drug Research, 2006; Office of Applied Studies & Substance Abuse and Mental Health Services Administration, 2006). Assuming the drug-use habits of patients with severe mental illness reflect those of the general population, this could partly explain the diverging prevalence data in patient populations. There are, however, few comparative studies between the general population and patient populations to support this hypothesis.
Substance use has been associated with a more severe course and outcome in both schizophrenia and bipolar disorder. Use of stimulants has been linked with criminality, violence and homelessness in severe mental disorders (Mueser et al. Reference Mueser, Essock, Drake, Wolfe and Frisman2001; Miles et al. Reference Miles, Johnson, Amponsah-Afuwape, Finch, Leese and Thornicroft2003), and high levels of cannabis use have been associated with increased psychopathology in both schizophrenia and bipolar disorder (Van Os et al. Reference Van Os, Bak, Hanssen, Bijl, de Graaf and Verdoux2002; Strakowski et al. Reference Strakowski, DelBello, Fleck, Adler, Anthenelli, Keck, Arnold and Amicone2007). Alcohol use has been associated with depression in bipolar disorder (Strakowski et al. Reference Strakowski, DelBello, Fleck and Arndt2000). Use of several substances (poly-use) has been associated with substance-use disorder in schizophrenia (Swartz et al. Reference Swartz, Wagner, Swanson, Scott Stroup, McEvoy, Canive, Miller, Reimherr, McGee, Khan, Van Dorn, Rosenheck and Liebermann2006).
Several lines of evidence indicate overlapping clinical profiles in schizophrenia and bipolar disorder (Crow, Reference Crow1998; Murray et al. Reference Murray, Sham, Van Os, Zanelli, Cannon and McDonald2004; Craddock et al. Reference Craddock, O'Donovan and Owen2006), but substance-use behaviour is studied to a limited extent in this context. Samples of patients with bipolar disorder are regularly found to have high levels of alcohol use (Sherwood Brown et al. Reference Sherwood Brown, Suppes, Adinoff and Rajan Thomas2001), and in epidemiological studies a higher degree of drug use than schizophrenia patients (Regier et al. Reference Regier, Farmer, Rae, Locke, Keith, Judd and Goodwin1990). Several studies have reported high levels of cannabis use in schizophrenia patients (Kavanagh et al. Reference Kavanagh, McGrath, Saunders, Dore and Clark2002; Green et al. Reference Green, Young and Kavanagh2005; Swartz et al. Reference Swartz, Wagner, Swanson, Scott Stroup, McEvoy, Canive, Miller, Reimherr, McGee, Khan, Van Dorn, Rosenheck and Liebermann2006), and the association between early cannabis use and later increased risk for schizophrenia seems now well documented (Moore et al. Reference Moore, Zammit, Lingford-Hughes, Barnes, Jones, Burke and Lewis2007). About 80% of patients with severe mental illness are addicted to tobacco (de Leon et al. Reference de Leon, Diaz, Rogers, Browne and Dinsmore2002; Ziedonis et al. Reference Ziedonis, Williams and Smelson2003).
There are few data about patterns of substance use (amount of total substance use, mono- versus poly-substance use, and regular versus sporadic use) and amount of use in severe mental disorders. It is expected that increased knowledge about the substance-use profiles for the two disorders can improve the phenotypic descriptions and thereby shed light on the nature of the conditions. A thorough patient characterization along with detailed descriptions of substance use could also reveal new aspects of the conditions necessary to improve the treatment of these complicated clinical conditions. To our knowledge, there are few studies directly comparing frequency of substance use in patients with schizophrenia and bipolar disorder, and none of these have investigated patterns of use beyond type of substance abused (Drake et al. Reference Drake, Osher and Wallach1989; Mueser et al. Reference Mueser, Yarnold and Bellack1992; Verdoux et al. Reference Verdoux, Mury, Besancon and Bourgeois1996). Also, few studies have investigated potentially harmful use that is below the level needed to meet the diagnostic criteria for abuse or addiction. It is not necessarily the case that the threshold for negative effects of drug use directly corresponds to the criteria for a DSM-IV or International Classification of Diseases (ICD)-10 diagnosis of abuse. It is possible that drug use of shorter duration and smaller amount can have important implications for understanding the relationship between drug use and severe mental illness, as for instance illustrated by studies showing that any cannabis use in adolescence interacted with a catechol-O-methyltransferase genotype to increase the risk for schizophreniform disorder (Caspi et al. Reference Caspi, Moffit, Cannon, McClay, Murray, Harrington, Taylor, Arseneault, Williams, Braithwaite, Poulton and Craig2005). This is in line with studies of the impact of any level of drug use as important factors in relation to other diseases like cancer (Hashibe et al. Reference Hashibe, Straif, Tashkin, Morgenstern, Greenland and Zhang2005) or to neurotoxicity (Cadet et al. Reference Cadet, Krasnova, Jayanthi and Lyles2007).
The present data were collected on a catchment area sample of predominantly stable out-patients. In a previous report from this ongoing study we have shown that patients with severe mental illness use about 50% more non-alcoholic drugs, and especially more centrally stimulating substances, than the general population (P. A. Ringen et al. unpublished observations).
The aims of the present study were to compare prevalence and type of alcohol and non-alcoholic drug use in representative samples of schizophrenia spectrum disorder and bipolar disorder, and to investigate possible differences in substance-use patterns between the two disorders.
Method
Sample
The present study was part of the Thematic Organized Psychosis Research (TOP) study, in which patients were recruited from the Departments of Psychiatry at Ullevål University Hospital, Aker University Hospital and Diakonhjemmet Hospital, all in Oslo (Norway). The three departments cover a geographical catchment area including 10 districts of Oslo and five suburbs. The catchment area corresponds to 485 000 inhabitants, Oslo's total population is about 550 000 (county), or 850 000 including the greater metropolitan area. The districts are located in different areas of the city and represent the city's variation in sociodemographic characteristics fairly well.
Inclusion criteria were as follows. To be eligible for the study the patients had to be aged 18–65 years, have a DSM-IV diagnosis of schizophrenia, schizophreniform disorder, schizoaffective disorder, bipolar I disorder, bipolar II disorder or bipolar disorder not otherwise specified (NOS). The recruitment teams were based in the out-patient clinics, where patients were transferred after acute illness phases. This procedure restricted inclusion of people in the most acute phases. We did not have specific inclusion criteria based on symptom load, but on a clinical evaluation of being able to participate in the clinical interviews and other assessments related to the protocol. Exclusion criteria were presence of a diagnosis of developmental disorder or serious brain damage and not speaking a Scandinavian language.
The present study sample is comprised of patients who were consecutively referred to the study from the out-patient clinics. A total of 336 patients were included in a cross-sectional study from October 2002 through to October 2006. The patients were recruited by their clinician, and thus the exact number of eligible patients who were not referred to the study based on the clinicians' decisions is unknown. However, there were 48 clearly eligible patients who were referred but refused to participate. The patient records at Ullevål University Hospital showed that a total of 1002 patients with either schizophrenia or bipolar disorder received treatment in any psychiatric department from May 2005 until the end of the patient inclusion of the present study. This constituted a reference group. The present study sample did not differ significantly from this reference group in proportion of subjects reporting non-alcoholic drug use in the previous 6 months (15.5% and 15.2% respectively). The patient reference sample had a mean age of 39.7 (s.d.=13.1) years and 53% were males. There were no statistically significant differences between the two samples in mean age or gender distribution.
Emphasis was put on recruiting all patients regardless of their ability to adhere to their respective treatment programmes.
Patients were divided into a schizophrenia patient group (schizophrenia, schizophreniform disorder and schizoaffective disorder) and a bipolar disorder group (bipolar I, bipolar II or bipolar disorder NOS).
Instruments/assessments
The patients were interviewed by trained clinicians (doctors of medicine or psychologists). Diagnoses were established using the Structural Clinical Interview for the DSM-IV Axis I disorders (SCID-I), modules A–E (APA, 1994). The E module includes assessment and diagnostics of the substance-use disorders. All interviewers participated in regular diagnostic consensus meetings led by a well-experienced clinical researcher in the field of diagnostics in severe mental disorders and finished a training course in SCID assessment based on the training programme at the University of California, Los Angeles (UCLA) (Ventura et al. Reference Ventura, Liberman, Green, Shaner and Mintz1998). Mean overall kappa for SCID diagnoses assessed by the UCLA was 0.77. To assess reliability for actual study interviews a stratified random sample was drawn, consisting of cases from every assessment staff member. Anonymous vignettes describing symptoms and development of the illness were then rated by two experts blind to the study ratings. For the 28 vignettes the overall agreement for the nine DSM-IV diagnostic categories was 82% and the overall kappa again 0.77 (95% confidence interval 0.60–0.94).
When trying to investigate for possible relationships between schizophrenia and bipolar disorder and drug-use habits, we found that the most simple and natural first step would be describing all levels of drug use in the two groups. This was done by simply asking for any use at different time intervals. Patients were asked about accumulated incidents of substance use during the previous 14 days, 6 months and 24 months, where type of substance was specified. These questions were validated in two ways. (1) Urine samples: of 10 patients with positive urine tests of any illicit substance, only one denied current use, implying that the patients' self-reports were fairly sensitive for current use of illicit substances. (2) Clinical information: the results of the research interviews were compared with data collected by the clinicians in the larger sample of n=1002 (the reference group), as shown in the previous section.
Reported mean amount of alcohol use in different intervals equivalent to at least two units or more of ethanol daily were considered ‘harmful use’. Patients reporting more incidents of psychoactive substance use than the common median for the two diagnostic groups were labelled ‘high users’.
Statistical analyses
All analyses were conducted by using the statistical package for the social sciences (SPSS) version 14.0 (SPSS Inc., Chicago, IL, USA). Group differences in independent samples of continuous variables were evaluated with independent t tests, and group differences in dichotomous data were evaluated with χ2/Fisher's exact tests. Differences between the groups in age and gender distribution were controlled for with logistic regression analyses, and in the Results section, we refer to these age- and gender-adjusted significance levels only. Group differences in incidents of use were analysed with non-parametric Mann–Whitney tests.
Results
The patient mean age was 35.2 (s.d.=11.0) years and 170 (50.6%) of the patients were male. Of the patients, 156 (46.4%) had schizophrenia, 39 (11.6%) schizoaffective disorder and 15 (4.5%) schizophreniform disorder (schizophrenia patient group). A total of 68 (20.2%) had bipolar I disorder, 49 (14.6%) bipolar II disorder and nine (2.7%) bipolar NOS disorder (bipolar patient group).
Age and gender were unevenly distributed between the diagnostic groups. Mean age for the schizophrenia patient group was 33.3 (s.d.=9.3) years, and for the bipolar disorder patient group 38.5 (s.d.=12.0) years; the difference between schizophrenia and bipolar disorder was highly statistically significant (p<0.001).
The schizophrenia group contained 56.7% males (n=119), significantly proportionally more than the 40.5% (n=51) males in the bipolar disorder group (p=0.005). The patient reference sample had a mean age of 39.7 (s.d.=13.1) years; 531 (53%) were males.
Patients reporting alcohol use in the 6-month and 24-month time intervals were significantly younger than the abstaining patients (p=0.005 and p=0.001 respectively). Patients reporting non-alcoholic drug use were significantly younger in all time intervals. Male gender was significantly associated with non-alcoholic drug use at all time intervals, but gender was not associated with alcohol use (Table 1). Daily tobacco smoking was reported by 59.1% (n=120) of the schizophrenia patients, and by 51.2% (n=64) of the bipolar disorder patients; the difference was not statistically significant after adjusting for age and gender.
Table 1. Reported use of substances, according to age and genderFootnote a

s.d., Standard deviation.
a Analysed using independent t tests and Fisher exact tests.
Schizophrenia patients had higher overall non-alcoholic drug-use prevalence for all time intervals than the bipolar patients, about four times higher rates of amphetamine and/or cocaine use, and about two times higher rates of cannabis use. However, when controlling for group differences in age and gender in the regression analyses, only the differences in the use of the centrally stimulating substances amphetamine and/or cocaine remained statistically significant (Table 2).
Table 2. Reported use of non-alcoholic drugsFootnote a
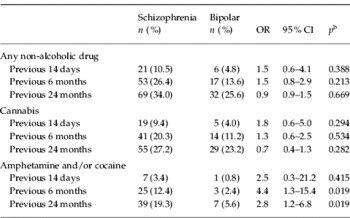
OR, Odds ratio; CI, confidence interval.
a Schizophrenia, n=210; bipolar disorder, n=126.
b p values of OR after adjusting for age and gender.
When assessing drug use over the previous 24 months, 66.0% of the schizophrenia patients and 74.4% of the bipolar disorder patients did not report any drug use (median number of incidents of drug use in the previous 24 months for both patient groups was 0). When assessing reported drug users in the previous 24 months only, median frequency of use was 48 (25th and 75th percentiles 6.0 and 284.5) in the schizophrenia group and 3 (25th and 75th percentiles: 1.0 and 26.8) in the bipolar disorder group (p<0.001).
Of the patients reporting non-alcoholic drug use in the previous 24 months, patients with bipolar disorder were significantly more likely to use only one substance, even after adjusting for age and gender differences. Cannabis was the only non-alcoholic drug used significantly more often in the bipolar group. Single use of centrally stimulating substances was nominally more prevalent in schizophrenia patients, but this difference did not reach statistical significance. Schizophrenia patients had, however, significantly more poly-substance use and a higher proportion of ‘high-users’, also after controlling for age and gender (Table 3). A total of 80 (65.5%) bipolar patients and 86 (43.4%) schizophrenia patients reported alcohol as the only substance used during the previous 24 months. Regression analysis controlling for age and gender showed this difference to be significant (p=0.004). When assessing mono-use of any substance, including alcohol, the figures were 106 (86.2%) and 122 (61.6%) for bipolar and schizophrenia patients respectively. The difference was again highly significant after controlling for age and gender (p<0.001).
Table 3. Pattern of reported use of non-alcoholic drugs in the previous 24 months

OR, Odds ratio; CI, confidence interval.
a Schizophrenia, n=210; bipolar disorder, n=126.
b Schizophrenia, n=69; bipolar disorder, n=32.
c p values of OR after adjusting for age and gender.
d High use: 24 incidents of use or more in the previous 24 months.
Alcohol use was more frequent among patients with bipolar disorder than with patients with schizophrenia; this difference remained highly significant across all time intervals, also after controlling for age and gender. More bipolar patients also had defined harmful use of alcohol in the previous 6 and 24 months after adjustment for age and gender (Table 4).
Table 4. Reported use of alcoholFootnote a

OR, Odds ratio; CI, confidence interval.
a Schizophrenia, n=210; bipolar disorder, n=126.
b p values of OR after adjusting for age and gender.
Relatively more patients with schizophrenia had a lifetime DSM-IV diagnosis of non-alcoholic drug abuse or dependence, but the difference compared with the bipolar group did not reach statistical significance. Overall rates of alcohol and substance abuse or dependence did not differ significantly between the diagnostic groups after adjustment for age and gender (Table 5).
Table 5. DSM-IV diagnosis of abuse/dependenceFootnote a

OR, odds ratio; CI, confidence interval.
a Schizophrenia, n=210; bipolar disorder, n=126.
b p values of OR after adjusting for age and gender.
When considering the schizoaffective disorder patients separately, we found that this group resembled the ‘narrow-schizophrenia’ group in alcohol use, and had statistically significantly more abstainers than the bipolar group (p=0.019 at the 24-month interval after adjusting for age and gender). The schizoaffective group had also a significantly lower proportion using only cannabis (p=0.042) compared with the bipolar group of individuals. There was a trend that the schizoaffective disorder patients resembled the bipolar group in having a lower proportion of psychoactive drug users compared with the ‘narrow-schizophrenia’ group, but this did not reach statistical significance. However, the schizoaffective group was small (n=39), which limits the statistical power of the analysis and makes the findings hard to interpret. The mean age of the schizoaffective disorder patients was 37.9 (s.d.=11.4) years, statistically significantly higher (p<0.001) than the ‘narrow-schizophrenia’ group [mean age 32.2 (s.d.=9.2) years]. Of the schizoaffective disorder patients, 41% (n=16) were males, significantly less than in the ‘narrow-schizophrenia’ group [60.2% males (n=103), p=0.023]. There were no statistically significant differences in demographics between the schizoaffective disorder patients and the bipolar disorder patients.
Discussion
The main finding of the present study was clear differences in substance-use patterns in schizophrenia and bipolar disorder. Patients with bipolar disorder had higher rates of alcohol consumption, while schizophrenia patients more often used centrally stimulating substances, had more frequent use of non-alcoholic drugs in general and more often used more than one non-alcoholic drug. These characteristics would not have been revealed through a diagnosis of abuse or dependence only, which shows the importance of evaluating substance use beyond the abuse or addiction diagnosis when the relationship to severe mental disorders is studied.
About twice as many schizophrenia patients as bipolar patients were abstaining from alcohol and twice as many bipolar patients could be defined as having harmful use of alcohol than schizophrenia patients. High rates of alcohol abuse in bipolar patients have been reported in numerous studies (Sherwood Brown et al. Reference Sherwood Brown, Suppes, Adinoff and Rajan Thomas2001). Alcohol use may induce affective, and most often depressive, episodes (Strakowski et al. Reference Strakowski, DelBello, Fleck and Arndt2000) and one could speculate about the existence of mechanisms linking alcohol use to bipolar disorder specifically.
Studies concerning alcohol consumption in patients with schizophrenia have been more diverging. In line with the current results several studies report lower rates of alcohol consumption in schizophrenia than in the general population (Etter & Etter, Reference Etter and Etter2004; Picchioni & Murray, Reference Picchioni and Murray2000). This could be due to possible mechanisms linked with schizophrenia that limit alcohol use, such as lower income or fewer social interactions. A higher prevalence of abstaining in the schizophrenia group could represent previous problematic use, although we found negative correlations between a lifetime diagnosis of alcohol abuse/dependence and current abstaining. Many studies, however, show higher rates of alcohol-use disorders among schizophrenia patients as compared with healthy controls (Farrell et al. Reference Farrell, Howes, Taylor, Lewis, Jenkins, Bebbington, Jarvis, Brugha, Gill and Meltzer1998; Green et al. Reference Green, Drake, Brunette and Noordsy2007) and schizophrenia patients have been found to show increased euphoric and stimulatory responses to alcohol (D'Souza et al. Reference D'Souza, Gil, Madonick, Perry, Forselius-Bielen, Braley, Donahue, Tellioglu, Zimolo, Gueorguieva and Krystal2006). Our findings regarding prevalence of use of centrally stimulating substances in schizophrenia and bipolar patients per se are more or less in line with other studies (Winokur et al. Reference Winokur, Turvey, Akiskal, Coryell, Solomon, Leon, Mueller, Endicott, Maser and Keller1998; Mueser et al. Reference Mueser, Essock, Drake, Wolfe and Frisman2001; Chengappa et al. Reference Chengappa, Levine, Gershon and Kupfer2000; Kilbourne et al. Reference Kilbourne, Cornelius, Han, Pincus, Shad, Salloum, Conigliaro and Haas2004). The higher proportion of stimulant use in the schizophrenia group compared with the bipolar group is, however, different to earlier comparisons between the two diagnostic groups, which found the prevalences to be more similar (Mueser et al. Reference Mueser, Yarnold and Bellack1992; Verdoux et al. Reference Verdoux, Mury, Besancon and Bourgeois1996), or with higher prevalence in the bipolar disorder group (Regier et al. Reference Regier, Farmer, Rae, Locke, Keith, Judd and Goodwin1990). Overall cannabis use did not seem to differ between diagnostic groups after controlling for age and gender.
When individuals with schizophrenia used non-alcoholic drugs they tended to have more poly-substance use and a higher frequency of use. Non-alcoholic drug users with bipolar disorder, on the other hand, more often used only cannabis. Bipolar disorder patients generally showed a stronger tendency for mono-use than the schizophrenia group. Preference for limited use of one type of substance could possibly reflect better functioning in the bipolar disorder group, as one would expect some level of discriminative ability in order to maintain a selective use pattern. The fact that bipolar disorder patients are indeed reported to have fewer cognitive deficits than schizophrenia patients (Daban et al. Reference Daban, Martinez-Aran, Torrent, Tabarés-Seisdedos, Balanzá-Martínez, Salazar-Fraile, Selva-Vera and Vieta2006) could support this interpretation.
The findings from our investigation of the different substance groups could be related to self-medication of symptoms (Khantzian, Reference Moore, Zammit, Lingford-Hughes, Barnes, Jones, Burke and Lewis1985). Depressive symptoms in bipolar patients have been reported to motivate for and be alleviated by substance use (Weiss et al. Reference Weiss, Kolodziej, Griffin, Najavits, Jacobson and Greenfield2004). Negative symptoms are in some studies reported to be milder in schizophrenia patients with substance-use disorder (Joyal et al. Reference Joyal, Hallé, Lapierre and Hodgins2003; Potvin et al. Reference Potvin, Sephery and Stip2005; Talamo et al. Reference Talamo, Centorino, Tondo, Dimitri, Hennen and Baldessarini2006). Following this line of reasoning, it is plausible that different substance preferences between diagnostic groups could reflect differences in the substances' effect on symptoms; i.e. that bipolar patients tend to use substances that are ‘relaxing’ such as alcohol and cannabis while schizophrenia patients use more centrally stimulating agents. However, a longitudinal study would be needed to address this question as both present and absent symptoms in a substance-using patient population could be regarded as indications of self-medication.
In recent years several longitudinal studies have concentrated on elucidating the strong associations found between substance use and severe mental illness (Strakowski et al. Reference Strakowski, DelBello, Fleck and Arndt2000; Van Os et al. Reference Van Os, Bak, Hanssen, Bijl, de Graaf and Verdoux2002; Henquet et al. Reference Henquet, Krabbendam, Spauwen, Kaplan, Lieb, Wittchen and van Os2005, Reference Henquet, Krabbendam, de Graaf, ten Have and van Os2006; Strakowski et al. Reference Strakowski, DelBello, Fleck, Adler, Anthenelli, Keck, Arnold and Amicone2007). Evidence is accumulating that cannabis is a risk factor for schizophrenia (Van Os et al. Reference Van Os, Bak, Hanssen, Bijl, de Graaf and Verdoux2002; Henquet et al. Reference Henquet, Krabbendam, Spauwen, Kaplan, Lieb, Wittchen and van Os2005), and possibly also for mania (Henquet et al. Reference Henquet, Krabbendam, de Graaf, ten Have and van Os2006; Strakowski et al. Reference Strakowski, DelBello, Fleck, Adler, Anthenelli, Keck, Arnold and Amicone2007). These results suggest a genetically linked vulnerability for substance use and severe mental disorders, but still little is known about possible differentiated substance-vulnerability between schizophrenia and bipolar disorder. The present findings of clear differences in drug-use patterns could be related to different interactions between genetic susceptibility and substance use for the two disorders. Such differences seem to be in opposition to a theory of a continuous psychotic-disorder spectrum (Crow, Reference Crow1998; Craddock et al. Reference Craddock, O'Donovan and Owen2006), and could suggest that schizophrenia and bipolar disorder are separate entities. However, our findings do not necessarily contradict this theory, as drug-use patterns show considerable overlap, and could also be operating along a continuum. Our results from the schizoaffective disorder group could support a possible ‘in-between’ position, but due to the low number, the results are difficult to interpret.
Recent advances in treatment regimens for severe mental disorders with co-morbid drug abuse (Mueser et al. Reference Mueser, Noordsy, Drake and Fox2003) are based on general principles which stress the importance of individually tailored and integrated approaches. If the two main severe mental disorders differ in drug-use susceptibility and drug-use habits on group levels, then the planning of the healthcare services for these patient groups should be adjusted accordingly.
The present findings were obtained in a sample from a catchment area-based healthcare system. This makes the data more representative for these patient populations than other studies, as for instance the CATIE study (Swartz et al. Reference Swartz, Wagner, Swanson, Scott Stroup, McEvoy, Canive, Miller, Reimherr, McGee, Khan, Van Dorn, Rosenheck and Liebermann2006). The inclusion of out-patients provides data from a stable patient population, avoiding the impact of drug use related to acute exacerbations seen in emergency ward studies. The study also has shortcomings, mainly that it is limited to cross-sectional registration of reported use, and thus cannot answer questions about causality or about subjective preferences or experiences. The patient selection criteria are not without some biasing effect; the study has excluded clinically unstable patients and there could be a possible over-representation of chronic cases in this sample of patients receiving specialized treatment. Possible systematic differences in drug use between schizophrenia and bipolar disorder patients from time periods before our assessment window are not accounted for, and represent potential confounders. The concrete availability of drugs of abuse on the illegal market in Oslo could affect the results, but prevalence of drug use in Oslo seems to be similar to reports from several other European countries (Rehm et al. Reference Rehm, Room, van den Brink and Kraus2005; European Monitoring Centre for Drugs and Drug Addiction, 2006).
The present study confirmed diagnosis-specific patterns of substance use in severe mental disorder. This suggests a need for disease-specific treatment strategies, and indicates separate underlying disease mechanisms. Future studies should focus on drug-use patterns' possible association with other clinical measures as motivation for use and preferably also longitudinal aspects, as well as more biological parameters such as genetics and brain imaging.
Acknowledgements
The study is part of the Thematic Organized Psychosis Research (TOP) study group and has been funded by grants from the Research Council of Norway (no. 147 787, 167 153 and 164 778/V50), Eastern Norway Health Authority (no. 123/2004) and from the Solveig and Johan P. Sommers Foundation to P.A.R. The funding sources had no involvement in the authors' work.
Declaration of Interest
None.







