Introduction
Since the first psychiatric surveys in the 1980s it has been established that common mental disorders (CMDs) are highly prevalent in the general population, that they often involve considerable functional impairments (Ormel et al. Reference Ormel, VonKorff, Üstün, Pini, Korten and Oldehinkel1994) and that most people with CMDs are untreated (Bijl et al. Reference Bijl, de Graaf, Hiripi, Kessler, Kohn, Offord, Üstün, Vicente, Vollebergh, Walters and Wittchen2003). These findings prompted various authors to conclude that unmet need for treatment of mental disorders is a major problem. However, it has also been recognized that not all those with CMDs need treatment because many disorders are mild and do not interfere with daily activities (Narrow et al. Reference Narrow, Rae, Robins and Regier2002).
Need for treatment is a complex issue and is best conceptualized as a series of overlapping constructs viewed from different perspectives (clinician, patient, society). In assessing potential need it is crucial to complement diagnosis with other measures such as symptom severity, role impairment, treatment effectiveness and consumer perceptions (Druss et al. Reference Druss, Wang, Sampson, Olfson, Pincus, Wells and Kessler2007). The first psychiatric surveys were, however, designed to estimate the prevalence rather than the clinical significance of mental disorders. With the rise of a new generation of psychiatric surveys from the twenty-first century onwards using the Composite International Diagnostic Interview version 3.0 (CIDI 3.0), which includes more questions on disorder-specific functional impairment, it has become possible to study the association between CMD severity and treatment contact in more depth (Kessler & Üstün, Reference Kessler and Üstün2004).
An important study based on these new-generation surveys, carried out in 14 countries (six less developed, eight developed) participating in the World Health Organization (WHO) World Mental Health (WMH) Survey Initiative, showed that the proportion of 12-month cases of CMDs classified as severe was 29.3% in the USA and varied between 10.9% and 20.0% in six Western European countries (Belgium, France, Germany, Italy, The Netherlands, Spain). Although disorder severity was correlated with probability of treatment in all eight developed countries studied, 35.5–50.3% of severe cases in the six Western European countries and 47.7% in the USA had received no health care in the past 12 months. At the same time, a high proportion of treatment was devoted to subthreshold cases (Demyttenaere et al. Reference Alonso, Angermeyer, Bernert, Bruffaerts, Brugha, Bryson, de Girolamo, de Graaf, Demyttenaere, Gasquet, Haro, Katz, Kessler, Kovess, Lépine, Ormel, Polidori, Russo, Vilagut, Almansa, Arbabzadeh-Bouchez, Autonell, Bernal, Buist-Bouwman, Codony, Domingo-Salvany, Ferrer, Joo, Martínez-Alonso, Matschinger, Mazzi, Morgan, Morosini, Palacín, Romera, Taub and Vollebergh2004).
Thus, there seems to be a problem in the allocation of treatment resources for those with mental health problems. However, more detailed information is needed to state this with certainty and to act on these signs. The European surveys had some specific limitations, in that there was no assessment of the severity of major depression and of prevalence rates of severe disorders such as bipolar disorder and drug disorders, and four out of six had a response rate below 60% (Alonso et al. Reference Alonso, Angermeyer, Bernert, Bruffaerts, Brugha, Bryson, de Girolamo, de Graaf, Demyttenaere, Gasquet, Haro, Katz, Kessler, Kovess, Lépine, Ormel, Polidori, Russo, Vilagut, Almansa, Arbabzadeh-Bouchez, Autonell, Bernal, Buist-Bouwman, Codony, Domingo-Salvany, Ferrer, Joo, Martínez-Alonso, Matschinger, Mazzi, Morgan, Morosini, Palacín, Romera, Taub and Vollebergh2004), and hence the proportion of 12-month disorders classified as severe is doubtful. Moreover, no results were available on the type and intensity of treatment received (Demyttenaere et al. Reference Alonso, Angermeyer, Bernert, Bruffaerts, Brugha, Bryson, de Girolamo, de Graaf, Demyttenaere, Gasquet, Haro, Katz, Kessler, Kovess, Lépine, Ormel, Polidori, Russo, Vilagut, Almansa, Arbabzadeh-Bouchez, Autonell, Bernal, Buist-Bouwman, Codony, Domingo-Salvany, Ferrer, Joo, Martínez-Alonso, Matschinger, Mazzi, Morgan, Morosini, Palacín, Romera, Taub and Vollebergh2004), so it is unknown to what extent severe cases received adequate treatment after initial treatment contact was made.
A later study based on 17 WMH surveys tried to fill this gap by showing that CMD severity was associated with adequate treatment in only two Western European countries and in the USA (Wang et al. Reference Wang, Aguilar-Gaxiola, Alonso, Angermeyer, Borges, Bromet, Bruffaerts, de Girolamo, de Graaf, Gureje, Haro, Karam, Kessler, Kovess, Lane, Lee, Levinson, Ono, Petukhova, Posada-Villa, Seedat and Wells2007). Adequate treatment use was defined broadly; it included being in ongoing treatment at interview, and treatment could be received in health-care and also in non-health-care settings. Based on data from the National Comorbidity Survey Replication (NCS-R) in the USA, it was found that adequate treatment determined by a more rigorous definition was more often received in mental health care (MHC) than in general medical care (GMC) (Wang et al. Reference Wang, Lane, Olfson, Pincus, Wells and Kessler2005). The NCS-R also showed that severity of major depression was narrowly significantly related to treatment adequacy in MHC but not in GMC (Kessler et al. Reference Kessler, Berglund, Demler, Jin, Koretz, Merikangas, Rush, Walters and Wang2003). It is not known whether this applies to severity of CMDs in general and whether these findings can be generalized to other developed countries. Moreover, an important policy issue that has not been studied comprehensively to date is the extent to which sociodemographic inequalities in treatment adequacy exist after the influence of disorder severity is taken into account.
To summarize, population-based information on the relationship between CMD severity and mental health treatment is heavily based on North American research. In the current study we used data from the Netherlands Mental Health Survey and Incidence Study-2 (NEMESIS-2) to replicate and expand existing knowledge by studying CMD severity and its association with treatment contact and treatment intensity.
Within the Dutch MHC system, the twin principles of equity and proportionality are particularly important. In the present context of limited resources, the aim should be that a greater proportion of severe cases can access mental health treatment and receive higher-intensity treatment than mild cases, and that cases of equivalent severity would be equally likely to access treatment and to be treated at the same level of intensity irrespective of their sociodemographic background.
Our levels of treatment intensity are based on those formulated in previous research, where they were called ‘levels of minimally adequate treatment’ because the definitions were based on available evidence-based guidelines at that time. We prefer the term ‘treatment intensity’ because, in population-based research, the level of precision required to assess guideline-concordant care may not be attainable (e.g. in NEMESIS-2 no information was available about medication dosages and type of psychotherapy given).
In The Netherlands, general practitioners most often constitute the first point of medical contact and act as gatekeepers to the rest of the health-care system, including MHC. In general, there are few, if any, financial barriers to accessing MHC in The Netherlands.
Method
NEMESIS-2 is a psychiatric epidemiological survey in the Dutch general population from 18 to 64 years old. It is based on a multistage, stratified random sampling of households, with one respondent randomly selected in each household. This resulted in a total sample of 6646 respondents (response rate 65.1%). The sample was nationally representative, although younger subjects were somewhat under-represented (de Graaf et al. Reference de Graaf, ten Have and van Dorsselaer2010). The interviews (average duration 95 min) were laptop computer-assisted and almost all were held at the respondent's home. The fieldwork was performed from November 2007 to July 2009.
The study was approved by a medical ethics committee. After having been informed about the study aims, respondents provided written informed consent. For a more detailed description of the design and fieldwork, see de Graaf et al. (Reference de Graaf, ten Have and van Dorsselaer2010) .
Diagnostic instrument
DSM-IV diagnoses were made using the CIDI 3.0, a fully structured lay-administered diagnostic interview. This instrument was developed and adapted for use in the WMH Survey Initiative (Kessler & Üstün, Reference Kessler and Üstün2004). In The Netherlands, the CIDI 3.0 was first used in the European Study on the Epidemiology of Mental Disorders (ESEMeD), which is part of this initiative. The CIDI 3.0 version used in NEMESIS-2 was an improvement on the one used in the Dutch ESEMeD study.
The 12-month disorders considered in this paper include: mood disorders (major depression, dysthymia, bipolar disorder), anxiety disorders (panic disorder, agoraphobia without panic disorder, social phobia, specific phobia, generalized anxiety disorder), substance use disorders (alcohol/drug abuse and dependence) and attention-deficit/hyperactivity disorder (ADHD). All disorders were determined among all respondents, except ADHD, which was limited to respondents aged 18–44 years because of concerns about recall bias in older respondents (Kessler et al. Reference Kessler, Angermeyer, Anthony, de Graaf, Demyttenaere, Gasquet, de Girolamo, Gluzman, Gureje, Haro, Kawakami, Karam, Levinson, Medina Mora, Oakley Browne, Posada-Villa, Stein, Adley Tsang, Aguilar-Gaxiola, Alonso, Lee, Heeringa, Pennell, Berglund, Gruber, Petukhova, Chatterji and Üstun2007).
Clinical calibration studies in various countries (Haro et al. Reference Haro, Arbabzadeh-Bouchez, Brugha, de Girolamo, Guyer, Jin, Lepine, Mazzi, Reneses, Vilagut, Sampson and Kessler2006) found that the CIDI 3.0 assesses mood, anxiety and substance use disorders with generally good validity in comparison to blinded clinical reappraisal interviews.
Severity of CMDs
Cases that met 12-month criteria for at least one disorder were classified in terms of clinical severity, consistent with previous studies (Demyttenaere et al. Reference Alonso, Angermeyer, Bernert, Bruffaerts, Brugha, Bryson, de Girolamo, de Graaf, Demyttenaere, Gasquet, Haro, Katz, Kessler, Kovess, Lépine, Ormel, Polidori, Russo, Vilagut, Almansa, Arbabzadeh-Bouchez, Autonell, Bernal, Buist-Bouwman, Codony, Domingo-Salvany, Ferrer, Joo, Martínez-Alonso, Matschinger, Mazzi, Morgan, Morosini, Palacín, Romera, Taub and Vollebergh2004; Medina-Mora et al. Reference Medina-Mora, Borges, Lara, Benjet, Blanco, Fleiz, Villatoro, Rojas and Zambrano2005). Cases rated as severe had at least one of the following: bipolar I disorder, substance dependence with a physiological dependence syndrome, a suicide attempt in the past 12 months, or severe self-reported impairment in at least two areas of role functioning, as assessed with the Sheehan Disability Scales (SDS; Leon et al. Reference Leon, Olfson, Portera, Farber and Sheehan1997). The SDS is a widely used self-report measure of condition-specific disability and is incorporated in all diagnostic CIDI sections. It consists of four questions, each asking the respondent to rate, on a scale from 0 to 10, the extent to which a particular disorder ‘interfered with’ activities in one of four role domains (home, work, social, close relationships) during the month in the past year when the disorder was most severe. The response options were visualized with the labels none (0), mild (1–3), moderate (4–6), severe (7–9) and very severe (10). Cases not classified as severe were classified as moderate if the individual had substance dependence without a physiological dependence syndrome, or at least moderate role impairment in any domain of the SDS. All other cases of 12-month disorder were classified as mild.
The severity classification including severe, moderate and mild disorders, and also no 12-month disorder, was significantly associated with days out of role (p < 0.0001, two-sided test) and the Mental Health Inventory-5 (Stewart et al. Reference Stewart, Hayes and Ware1988; Ware & Sherbourne, Reference Ware and Sherbourne1992: p < 0.0001, two-sided test). These results indicate that the severity classification used is valid; a conclusion that was also drawn in previous research using a similar definition of severity (Kessler et al. Reference Kessler, Chiu, Demler and Walters2005).
Treatment contact
Treatment contact refers to at least one contact made in the GMC or MHC sector for emotional or addiction problems in the past 12 months. It was assessed with the question ‘In the past 12 months, did you visit any of the following professionals or institutions because of emotional or alcohol or drugs problems of your own?’ Included were general medical professionals (general practitioners, company doctors, social work, home care or district nurses, physiotherapists or haptonomists, medical specialists or other professionals working within the GMC sector) and mental health services (psychiatrists, psychologists, psychotherapists, part-time or full-time psychiatric treatment).
Respondents who visited one of these professionals or services were asked what type of treatment they received from each (psychotherapy, pharmacotherapy, referral, practical assistance). When psychotherapy was received, follow-up questions for each provider consulted concerned the number and duration of visits. When pharmacotherapy was received, questions on type and duration of medication prescribed by each provider were asked.
Treatment intensity
As in previous research, four levels of treatment intensity were assessed based on the type and duration of therapy received in the past 12 months for a specific disorder in GMC and MHC:
(1) At least two visits with any professional (Wang et al. Reference Wang, Lane, Olfson, Pincus, Wells and Kessler2005; Reference Wang, Aguilar-Gaxiola, Alonso, Angermeyer, Borges, Bromet, Bruffaerts, de Girolamo, de Graaf, Gureje, Haro, Karam, Kessler, Kovess, Lane, Lee, Levinson, Ono, Petukhova, Posada-Villa, Seedat and Wells2007; Kessler et al. Reference Kessler, Berglund, Chiu, Demler, Glantz, Lane, Jin, Merikangas, Nock, Olfson, Pincus, Walters, Wang, Wells, Kessler and Üstün2008).
(2) At least four visits with any professional, or at least 0.5 month of any medication plus at least two visits to a physician or a MHC professional.
(3) At least eight visits with any professional, or at least 1 month of any medication plus at least four visits to a physician or a MHC professional (Shen et al. Reference Shen, Zhang, Huang, He, Liu, Cheng, Tsang, Lee and Kessler2006; Wang et al. Reference Wang, Aguilar-Gaxiola, Alonso, Angermeyer, Borges, Bromet, Bruffaerts, de Girolamo, de Graaf, Gureje, Haro, Karam, Kessler, Kovess, Lane, Lee, Levinson, Ono, Petukhova, Posada-Villa, Seedat and Wells2007).
(4) At least eight visits with any professional lasting on average at least 30 min, or at least 1 month of an appropriate medication for the disorder in question plus at least four visits to a physician or a MHC professional (Kessler et al. Reference Kessler, Berglund, Demler, Jin, Koretz, Merikangas, Rush, Walters and Wang2003). Appropriate medications for disorders included antidepressants for depressive disorders, mood stabilizers or antipsychotic agents for bipolar disorders, antidepressants or anxiolytic agents for anxiety disorders, antagonists or agonists for alcohol and other substance use disorders and stimulant medication for ADHD, as in previous research (Wang et al. Reference Wang, Lane, Olfson, Pincus, Wells and Kessler2005).
Correlates
The correlates included in this study are: disorder severity, physical disorder (at least one of 17 chronic physical disorders treated or monitored by a medical doctor in the past 12 months, none), sex, age, education, living situation, employment situation, household income and urbanicity of residence.
Statistical analysis
The data were weighted to correct for differences in the response rates in several sociodemographic groups and in the probability of selection of respondents within households. Robust standard errors were calculated in Stata version 11 (Stata Corporation, USA) to obtain correct 95% confidence intervals and p values (Skinner et al. Reference Skinner, Holt and Smith1989).
First, prevalence rates of 12-month mental disorders and severity levels for each disorder were calculated. Second, rates of any 12-month treatment contact made in GMC and MHC among respondents with different severity levels and rates of severity levels among service users of GMC and MHC were calculated. Third, multinomial logistic regression analyses were used to examine clinical and sociodemographic correlates of any 12-month treatment contact for mental health problems. In these analyses, two categories of service users were compared (those using GMC only and those using MHC regardless of whether they used GMC) with the respondents reporting no use of either type of care. The results were adjusted for sex and age (model 1) and all variables in the table (model 2). Fourth, levels of treatment intensity received by the two categories of service users (GMC only, MHC regardless of GMC) with different severity levels were calculated. Fifth, logistic regression analyses were performed to examine clinical and sociodemographic correlates of high-intensity treatment received in the MHC sector (reference group: no treatment received according to the highest intensity level). Again, results were adjusted for sex and age (model 1) and all variables in the table (model 2). Similar analyses were not performed for the GMC-only sector because of the low intensity of treatment received by service users of GMC only.
Results
Table 1 shows prevalence rates of mental disorders and severity levels for each disorder. The 12-month prevalence of any mental disorder was 18.0%. Anxiety disorders were the most prevalent class, followed by mood and substance use disorders. The most prevalent individual disorders were major depression, specific phobia and social phobia.
Table 1. Twelve-month prevalence and severity of mental disorders in the general population (n = 6646)
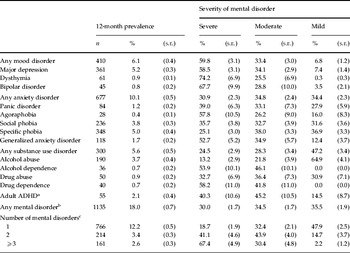
ADHD, Attention-deficit/hyperactivity disorder.
Values given as unweighted numbers and weighted percentages with standard errors (s.e.).
Percentages in the three severity columns are repeated as proportions of all cases and add up to 100% across each row.
a ADHD is measured for subjects aged 18–44 years only.
b For any mental disorder and for number of mental disorders, adult ADHD was coded as absent among subjects aged 45–64 years who were not assessed for this disorder.
c To assess co-morbidity, diagnostic hierarchy rules were ignored. Therefore, the numbers of respondents with 1, 2 and 3 or more mental disorders (n = 1141) do not correspond to the number of respondents with any mental disorder (n = 1135).
Among respondents with a disorder, 30.0% were classified as severe, 34.5% as moderate and 35.5% as mild. Mood disorders had the highest percentage of severe cases, and substance use disorders the lowest. The mood disorder with the highest percentage of severe cases was dysthymia, agoraphobia had the highest percentage of severe cases among anxiety disorders, and drug dependence the highest among substance use disorders. The individual disorders with the lowest percentage of severe cases were alcohol abuse and specific phobia.
It should be noted that our severity classification is based on all 12-month disorders reported by the respondent along with their associated role impairment. This means that a person with a mild alcohol abuse disorder and severe depression is classified as severe in both disorders reported in Table 1.
Table 2 shows a clear relationship between CMD severity and probability of service use in both health-care sectors. Thus 51.9% of the cases classified as severe received GMC, compared to 26.8% of the moderate cases, 10.8% of the mild cases and 4.8% of those without a 12-month mental disorder. Although a similar relationship was seen for MHC, only 39.0% of the severe cases received this type of care, and 3.0% of those without a 12-month disorder. Even though a small proportion of non-cases received treatment for their mental health problems, these cases constitute a substantial proportion of all service users. Among respondents receiving MHC, for example, 40.3% had no 12-month mental disorder whereas 33.7% had a severe disorder.
Table 2. Severity of mental disorders and 12-month treatment contact for mental health problems

Values given as weighted percentages with standard errors (s.e.).
Row % reply to the question ‘What proportion of those with a specific severity level received treatment?’
Column % reply to the question ‘What proportion of service users had a specific disorder severity level?’
Column percentages add up to 100%.
a No 12-month mental disorder.
Table 3 shows correlates of any 12-month treatment contact for mental health problems. Respondents with more severe mental disorders, with a physical disorder, females, middle-aged respondents (35–54 years), those without a partner and those with low income levels were more likely to have used MHC and GMC for their mental health problems than no care, after adjustment for sex and age (model 1). Respondents without a paid job and those with primary, basic vocational education were also more likely to have used MHC (but not GMC).
Table 3. Clinical and sociodemographic correlates of 12-month treatment contact for mental health problems

GMC, General medical care; MHC, mental health care; aRRR, adjusted relative risk ratio; CI, confidence interval; n.s., non-significant; ref., reference category.
Bold type indicates a significant aRRR/p value at the 0.05 level, two-sided test.
Model 1: adjusted for sex and age at interview. Model 2: adjusted for all variables in the table.
a The reference group consists of respondents without treatment contact in the GMC or MHC sector.
b No 12-month mental disorder.
After adjustment for all variables (model 2), fewer correlates were significantly associated with both types of health care. One correlate of GMC (low income) and three correlates of MHC (low income, presence of a physical disorder, female sex) failed to reach significance in model 2. Whereas respondents with primary or basic vocational education were more likely to have used MHC in model 1, those with secondary education were less likely to have used this type of care than no care compared to those with the highest education in model 2.
After the influence of all variables was taken into account, respondents with a severe or mild disorder and those without a paid job were more likely to have used MHC than GMC (last two columns of Table 3). The opposite held for those with a physical disorder; they were more likely to have used GMC than MHC. Respondents with higher secondary education were less likely to have used MHC than GMC, indicating that they have a lower chance of being referred to specialty care compared to those with the highest education.
Table 4 shows rates of treatment intensity experienced by service users with different levels of severity. Depending on the definition, the rates of treatment intensity ranged from 51.6% to 13.0% in GMC and from 81.4% to 51.1% in MHC. CMD severity was related to treatment intensity in MHC but not in GMC. More precisely, although all of those in MHC irrespective of disorder severity had at least two visits (level 1), MHC users with severe disorders more often experienced higher levels of treatment intensity compared to those without a 12-month disorder. In MHC, those with moderate disorders most often received treatment according to all levels of intensity. This could be a result of chance because of the small number of respondents in this group.
Table 4. Severity of mental disorder by 12-month treatment intensity for mental health problems in the general medical care (GMC) and mental health care (MHC) sectors (n = 748)

n.s., Non-significant.
Values are given as weighted percentages with standard errors (s.e.).
Bold type indicates a significant p value at the 0.05 level, two-sided test.
a No 12-month mental disorder.
Level 1: at least two visits with any professional.
Level 2: at least four visits with any professional, or at least 0.5 month of any medication plus at least two visits to a physician or MHC professional.
Level 3: at least eight visits with any professional, or at least 1 month of any medication plus at least four visits to a physician or MHC professional.
Level 4: at least eight visits with any professional lasting an average of at least 30 min, or at least 1 month of an appropriate medication for the focal disorder plus at least four visits to a physician or MHC professional.
In MHC, service users with severe or moderate mental disorders were more likely to have experienced the highest level of treatment intensity compared to those without a 12-month disorder, after adjustment for all variables in Table 5 (model 2). By contrast, MHC users with lower secondary education were less likely to have received this level of care compared to those with the highest education in model 2. Sociodemographic characteristics were not significantly related to highest treatment intensity, before and after the influence of disorder severity was taken into account.
Table 5. Clinical and sociodemographic correlates of 12-month treatment intensity in the mental health care (MHC) sector (n = 431)

aOR, Adjusted odds ratio; CI, confidence interval; ref., reference category.
Model 1: adjusted for sex and age at interview. Model 2: adjusted for all variables in the table.
Bold type indicates a significant aOR at the 0.05 level, two-sided test.
a The reference group consists of respondents who did not experience treatment intensity according to level 4 in the MHC sector. Level 4: at least eight visits with any professional lasting an average of at least 30 min, or at least 1 month of an appropriate medication for the focal disorder plus at least four visits to a physician or MHC professional.
b No 12-month mental disorder.
Discussion
This study confirms earlier North American findings that 30.0% of the people with a CMD in the past 12 months have a severe disorder. It also strengthens earlier non-quantified statements that only 39.0% of severe cases receive MHC, and that at the same time 40.3% of MHC users do not have a 12-month disorder. This is the first study to provide detailed information on levels of treatment intensity in two distinct health-care sectors by disorder severity. The results show that users of GMC only experience low levels of treatment intensity irrespective of disorder severity. Consistent with policy in The Netherlands, no major sociodemographic inequalities in treatment intensity exist after initial treatment contact is made.
Strengths and limitations
A significant advantage of NEMESIS-2 is that it makes use of CIDI 3.0, enabling a more detailed study of CMD severity. Moreover, a substantial number of respondents were interviewed, making it feasible to study relationships among smaller subgroups (i.e. treated cases).
Although the NEMESIS-2 sample was representative of the Dutch population on most parameters, people with an insufficient mastery of Dutch, those with no fixed address and residents of institutions were under-represented. As it is difficult to estimate how this under-representation might have affected the results, it is safest to conclude that the findings are not generalizable to these particular categories.
Recall problems might conceivably have compromised respondents' estimations of their service use in the past year, especially regarding number of visits and duration of medication use. However, it is difficult to gauge how this might have influenced the results of our study. Any recall bias would probably have weakened the effects of correlates on treatment intensity.
In NEMESIS-2, the most common Axis 1 mental disorders were assessed. Personality disorders (except for antisocial personality disorder) were not recorded in the dataset. This means that, in reality, the proportion of service users without a 12-month disorder is probably somewhat lower.
Discussion of the research findings
Compared to the USA (Demyttenaere et al. Reference Alonso, Angermeyer, Bernert, Bruffaerts, Brugha, Bryson, de Girolamo, de Graaf, Demyttenaere, Gasquet, Haro, Katz, Kessler, Kovess, Lépine, Ormel, Polidori, Russo, Vilagut, Almansa, Arbabzadeh-Bouchez, Autonell, Bernal, Buist-Bouwman, Codony, Domingo-Salvany, Ferrer, Joo, Martínez-Alonso, Matschinger, Mazzi, Morgan, Morosini, Palacín, Romera, Taub and Vollebergh2004), a similar proportion of 12-month disorders classified as severe was found: 30.0% in the present study versus 29.3% in the USA. These proportions are higher than those found in the six Western European WMH surveys, most probably because these surveys had not assessed severity of some important mental disorders (Demyttenaere et al. Reference Alonso, Angermeyer, Bernert, Bruffaerts, Brugha, Bryson, de Girolamo, de Graaf, Demyttenaere, Gasquet, Haro, Katz, Kessler, Kovess, Lépine, Ormel, Polidori, Russo, Vilagut, Almansa, Arbabzadeh-Bouchez, Autonell, Bernal, Buist-Bouwman, Codony, Domingo-Salvany, Ferrer, Joo, Martínez-Alonso, Matschinger, Mazzi, Morgan, Morosini, Palacín, Romera, Taub and Vollebergh2004).
Consistent with the NCS-R (Kessler et al. Reference Kessler, Chiu, Demler and Walters2005), we found that mood disorders and ADHD had a higher percentage of severe cases than anxiety disorders. However, in the NCS-R, substance use disorders had a higher percentage of severe cases than anxiety disorders whereas in the present study and the Australian WMH survey (Slade et al. Reference Slade, Johnston, Oakley-Browne, Andrews and Whiteford2009), the opposite was seen. These discrepancies are probably the result of differences in sample composition and the number of anxiety disorders assessed.
In the present study 51.9% of the severe cases received GMC and 39.0% MHC. Additional analyses show that 58.7% of the severe cases received any of these types of care. This means that a fairly substantial proportion of severe cases (41.3%) did not receive any health care in the past 12 months. This is in line with previous research showing that 35.5–50.3% of severe cases in six Western European countries and 47.7% in the USA received no health-care treatment in the past 12 months (Demyttenaere et al. Reference Alonso, Angermeyer, Bernert, Bruffaerts, Brugha, Bryson, de Girolamo, de Graaf, Demyttenaere, Gasquet, Haro, Katz, Kessler, Kovess, Lépine, Ormel, Polidori, Russo, Vilagut, Almansa, Arbabzadeh-Bouchez, Autonell, Bernal, Buist-Bouwman, Codony, Domingo-Salvany, Ferrer, Joo, Martínez-Alonso, Matschinger, Mazzi, Morgan, Morosini, Palacín, Romera, Taub and Vollebergh2004). There are several possible reasons why only 39.0% of severe cases sought MHC. These include: people had received a referral to MHC and were on the waiting list for MHC treatment; they had received MHC on one occasion but did not benefit from it and as a result had no confidence in care providers; they wanted to solve their problems by themselves or thought the problem would go away by itself (Sareen et al. Reference Sareen, Jagdeo, Cox, Clara, ten Have, Belik, de Graaf and Stein2007); and errors in the classification of disorder severity and MHC treatment contact.
A substantial proportion of MHC users (40.3%) did not have a 12-month mental disorder. This is in line with Demyttenaere et al. (Reference Alonso, Angermeyer, Bernert, Bruffaerts, Brugha, Bryson, de Girolamo, de Graaf, Demyttenaere, Gasquet, Haro, Katz, Kessler, Kovess, Lépine, Ormel, Polidori, Russo, Vilagut, Almansa, Arbabzadeh-Bouchez, Autonell, Bernal, Buist-Bouwman, Codony, Domingo-Salvany, Ferrer, Joo, Martínez-Alonso, Matschinger, Mazzi, Morgan, Morosini, Palacín, Romera, Taub and Vollebergh2004) suggesting that either the majority or near majority of people in GMC or MHC are non-cases or mild cases, although exact results were not presented. These high proportions of non-cases in treatment probably reflect the joint effects of not assessing all mental disorders, some true cases being incorrectly classified as non-cases, people in treatment not meeting criteria for a recent mental disorder (which could also have been the result of adequate treatment), and the fact that non-cases make up the vast majority of the general population. Additional analyses based on NEMESIS-2 show that MHC users without a 12-month mental disorder often had recent functional impairments or a mental disorder dated before the past year (ten Have et al. Reference ten Have, van Dorsselaer and de Graaf2012). Based on the NCS-R, it was found that most people who used any services for mental health problems also had either a diagnosis or some other indicator of possible need for treatment (Druss et al. Reference Druss, Wang, Sampson, Olfson, Pincus, Wells and Kessler2007). One focus of future research should be on these MHC patients who do not have a fully developed mental disorder, to find out what problems and functional impairments they face, what prompted them to seek specialty care and to what extent they can be adequately treated in GMC.
Consistent with previous studies (Bebbington et al. Reference Bebbington, Brugha, Meltzer, Jenkins, Ceresa, Farrell and Lewis2000; Demyttenaere et al. Reference Alonso, Angermeyer, Bernert, Bruffaerts, Brugha, Bryson, de Girolamo, de Graaf, Demyttenaere, Gasquet, Haro, Katz, Kessler, Kovess, Lépine, Ormel, Polidori, Russo, Vilagut, Almansa, Arbabzadeh-Bouchez, Autonell, Bernal, Buist-Bouwman, Codony, Domingo-Salvany, Ferrer, Joo, Martínez-Alonso, Matschinger, Mazzi, Morgan, Morosini, Palacín, Romera, Taub and Vollebergh2004), respondents with severe mental disorders were more likely to have used MHC and GMC for their mental health problems than no care, compared to non-cases. Severe cases were also more likely to have used MHC than GMC, implying that they had a higher chance of being referred to specialty care. In the WMH Survey Initiative there was also a clear trend for severity to be related positively to proportional treatment in MHC. Data were not presented on the strength of this relationship in the participating countries or on the extent to which severity was associated with a higher chance of being referred to specialty care (Demyttenaere et al. Reference Alonso, Angermeyer, Bernert, Bruffaerts, Brugha, Bryson, de Girolamo, de Graaf, Demyttenaere, Gasquet, Haro, Katz, Kessler, Kovess, Lépine, Ormel, Polidori, Russo, Vilagut, Almansa, Arbabzadeh-Bouchez, Autonell, Bernal, Buist-Bouwman, Codony, Domingo-Salvany, Ferrer, Joo, Martínez-Alonso, Matschinger, Mazzi, Morgan, Morosini, Palacín, Romera, Taub and Vollebergh2004).
Consistent with previous research in the USA (Wang et al. Reference Wang, Lane, Olfson, Pincus, Wells and Kessler2005), higher-intensity treatment was more often received in MHC than in GMC. Other studies focusing on anxiety and depressive disorders in six Western European countries (Fernández et al. Reference Fernández, Haro, Martinez-Alonso, Demyttenaere, Brugha, Autonell, de Girolamo, Bernert, Lépine and Alonso2007; Gabilondo et al. Reference Gabilondo, Rojas-Farreras, Rodrigues, Fernández, Pinto-Meza, Vilagut, Haro and Alonso2011) and Canada (Duhoux et al. Reference Duhoux, Fournier, Nguyen, Roberge and Beveridge2009; Roberge et al. Reference Roberge, Fournier, Duhoux, Nguyen and Smolders2011) also found higher levels of treatment intensity in MHC than in GMC. In these countries, the rates of treatment intensity were somewhat higher, but still low in GMC. The reasons for this more general phenomenon of low levels of treatment intensity in the GMC sector are unclear, but presumably involve provider characteristics (competing demands, inadequate reimbursement for treating mental disorders, low levels of training and experience in treating mental disorders, providers' conception of their job) and patient characteristics (poorer compliance with treatments than in MHC) (Wang et al. Reference Wang, Lane, Olfson, Pincus, Wells and Kessler2005; Olfson et al. Reference Olfson, Mojtabai, Sampson, Hwang, Druss, Wang, Wells, Pincus and Kessler2009).
In line with previous research in the USA focusing on major depression (Kessler et al. Reference Kessler, Berglund, Demler, Jin, Koretz, Merikangas, Rush, Walters and Wang2003), disorder severity was related to treatment intensity in MHC but not in GMC. A study among primary care patients with a depressive or anxiety disorder in The Netherlands also showed that symptom severity was unrelated to guideline-concordant care, unless the general practitioner had diagnosed them as such (Smolders et al. Reference Smolders, Laurant, Verhaak, Prins, van Marwijk, Penninx, Wensing and Grol2009).
In the present study, no consistent sociodemographic inequalities in treatment intensity in MHC were found. This was also suggested by Kessler et al. (Reference Kessler, Berglund, Demler, Jin, Koretz, Merikangas, Rush, Walters and Wang2003), who studied treatment intensity among those with major depression in the NCS-R and has been confirmed by the results of Duhoux et al. (Reference Duhoux, Fournier, Nguyen, Roberge and Beveridge2009), who studied treatment intensity for depressive disorders in Canada.
Final comments
This study shows that there is a problem in the allocation of treatment resources for those with common mental health problems: only 39.0% of severe cases receive MHC, and at the same time 40.3% of MHC users are non-cases. Moreover, patients using GMC only experience low levels of treatment intensity, irrespective of the severity of their disorder. However, we cannot estimate the scale of this problem because optimal allocation rules are not obvious. To guide treatment resource allocation, more information is needed on, for example, the disease burden of non-cases (what problems and functional impairments do non-cases face and what prompted them to seek treatment?), illness course of mild cases and non-cases (to what extent do symptoms grow worse when mild cases and severe cases in remission are not treated in time?), the cost-effectiveness of different treatments for society (to what extent can relapse prevention be effectively implemented in GMC?) and non-compliance by patients (to what extent is treatment intensity in GMC caused by patients' non-compliance?).
Notwithstanding these comments, MHC treatment in GMC should be improved, especially when policy is aimed at increasing the role of primary care in the management of mental health problems. Effective strategies for strengthening primary MHC are interventions that incorporate clinician education, an enhanced role of nurses (nurse case management) and a greater degree of integration between primary and specialty care (consultation liaison) (Gilbody et al. Reference Gilbody, Whitty, Grimshaw and Thomas2003).
Acknowledgements
NEMESIS-2 is conducted by the Netherlands Institute of Mental Health and Addiction (Trimbos Institute) in Utrecht. Financial support has been received from the Ministry of Health, Welfare and Sport, with supplementary support from the Netherlands Organization for Health Research and Development (ZonMw) and the Genetic Risk and Outcome of Psychosis (GROUP) investigators.
Declaration of Interest
None.







