Introduction
Cognitive models of psychosis propose that the way in which individuals appraise and respond to anomalous experiences can determine the development and maintenance of distress (Birchwood and Chadwick, Reference Birchwood and Chadwick1997; Garety et al., Reference Garety, Kuipers, Fowler, Freeman and Bebbington2001; Morrison, Reference Morrison2001). However, a clear taxonomy of unhelpful or maladaptive responding to psychotic experiences (PEs) has yet to be agreed, reflecting both the heterogeneity of the psychosis phenotype and the context-bound nature of ‘responding’.
‘Response styles’ have often been investigated in the context of voice-hearing and commonly associated with the concept of ‘coping’, influenced by the transactional stress-coping framework of Lazarus and Folkman (Reference Lazarus and Folkman1984). Early influential work identified engagement, resistance and indifference as key styles of responding to voices (Birchwood and Chadwick, Reference Birchwood and Chadwick1997), with appraisals and beliefs about voices (particularly relating to perceived power and control) playing a key mediating role. Using Principal Component Analysis (PCA), O'Sullivan (Reference O'Sullivan1994) proposed coping factors differing along three dimensions – active v. passive, hopeful v. despairing, acceptance v. rejection. More recently, Tully et al. (Reference Tully, Wells, Pyle, Hudson, Gumley, Kingdon, Schwannauer, Turkington and Morrison2017b) have validated a self-report measure of cognitive and behavioural responses to psychosis in a general psychosis sample (i.e. not exclusively voice-hearers) and identified three factors: ‘threat monitoring and avoidance’, ‘conscious self-regulation’ and ‘social control and reassurance-seeking’. The finding that ‘threat monitoring and avoidance’ showed an association with symptom severity is consistent with a previously reported association of avoidance with positive and negative symptoms (Depp et al., Reference Depp, Cardenas, Harris, Vahia, Patterson and Mausbach2011) as well as the role of avoidance as a key safety-seeking behaviour maintaining persecutory beliefs (Freeman et al., Reference Freeman, Garety and Kuipers2001; Freeman et al., Reference Freeman, Garety, Kuipers, Fowler, Bebbington and Dunn2007). Moritz et al. (Reference Moritz, Ludtke, Westermann, Hermeneit, Watroba and Lincoln2016b), using the Maladaptive and Adaptive Coping Styles Scale [MAX (Moritz et al., Reference Moritz, Jahns, Schroder, Berger, Lincoln, Klein and Goritz2016a)], have also found associations between avoidance and suppression and positive symptoms (particularly paranoia) which remain after controlling for depression. Recent work highlights the role of emotion with findings that individuals with a diagnosis of schizophrenia use more maladaptive Cognitive Emotional Regulation Strategies [CERS (O'Driscoll et al., Reference O'Driscoll, Laing and Mason2014)]; and show specific difficulties in emotion regulation skills (related to awareness, understanding and acceptance), which are proposed to affect regulation of anger, shame, anxiety and sadness (Lincoln et al., Reference Lincoln, Hartmann, Kother and Moritz2015).
Table 1. Demographic and clinical data by group

a Six missing.
b Two missing.
c One participant missing.
d Five missing.
e Ten missing.
f Seven missing.
g Three missing.
*Mann–Whitney tests (all SAPS and SANS scores). Bold denotes p < .05.
It should be noted that concepts such as stress, coping and emotional regulation are most relevant within the context of distressing experiences. However, PEs exist on a continuum, with replicated findings of benign or even positive PEs occurring in the general population (de Leede-Smith and Barkus, Reference de Leede-Smith and Barkus2013; Johns et al., Reference Johns, Kompus, Connell, Humpston, Lincoln, Longden, Preti, Alderson-Day, Badcock, Cella, Fernyhough, McCarthy-Jones, Peters, Raballo, Scott, Siddi, Sommer and Laroi2014; Peters et al., Reference Peters, Ward, Jackson, Morgan, Charalambides, McGuire, Woodruff, Jacobsen, Chadwick and Garety2016). Accordingly, cognitive models of psychosis predict that clinical and non-clinical groups with PEs will differ in how they respond to their anomalous experiences. One study comparing individuals with PEs with and without ‘need-for-care’ (Bak et al., Reference Bak, Myin-Germeys, Hanssen, Bijl, Vollebergh, Delespaul and van Os2003) involved individuals reporting incident PEs recruited through a prospective general population sample. The findings suggested that ‘symptomatic coping’ (i.e. going along with the content of psychotic symptoms), together with lower perceived control, is more common in the clinical group, while use of active problem solving and higher perceived control is more common in the non-clinical group. More recently, within the psychosis continuum literature, there is emerging evidence from studies, which purposively sample non-clinical individuals with full-blown, persistent PEs but no ‘need-for-care’. These individuals, with persistent PEs selected for absence of distress, have been shown to have high levels of psychological and emotional well-being (Brett et al., Reference Brett, Peters, Johns, Tabraham, Valmaggia and McGuire2007; Ward et al., Reference Ward, Gaynor, Hunter, Woodruff, Garety and Peters2014; Peters et al., Reference Peters, Ward, Jackson, Morgan, Charalambides, McGuire, Woodruff, Jacobsen, Chadwick and Garety2016) and represent a unique group of particular importance in identifying adaptive ways of responding to PEs. In early work (Brett et al., Reference Brett, Peters, Johns, Tabraham, Valmaggia and McGuire2007), it was found that this non-clinical group was less likely to endorse potentially maladaptive responses to PEs categorised as ‘avoidance’, ‘cognitive control’ and ‘immersion’ relative to a clinical psychosis group. However, this study, in keeping with much of the literature above, was based on retrospective interviews of participants’ experiences, an approach which makes it difficult to exclude the possibility that maladaptive responses simply reflect intrinsically more distressing experiences within the clinical group. One way to tackle this issue is by using an experimental design, presenting task-based analogues of psychotic symptoms, allowing all participants to encounter identical anomalous experiences (Linney and Peters, Reference Linney and Peters2007; Peters et al., Reference Peters, Ward, Jackson, Woodruff, Morgan, McGuire and Garety2017; Tully et al., Reference Tully, Wells and Morrison2017a). This allows response styles (as well as appraisals) to be investigated without the potential confound of differences in the nature of the experiences being responded to, while also counteracting limitations with retrospective report. A pilot study comparing individuals with PEs with and without need-for-care on experimental analogues of thought interference and voice-hearing (Ward et al., Reference Ward, Gaynor, Hunter, Woodruff, Garety and Peters2014) showed that those with ‘need-for-care’ were more likely to endorse maladaptive responses (notably rumination and distraction) and less likely to employ adaptive (decentring) ways of responding to unusual experiences. These findings now require both replication in a larger, fully powered sample, and the addition of a control group without PEs, to allow any observed group differences between the clinical and non-clinical group to be contextualised, and specifically to determine whether the non-clinical group is performing any differently from controls.
Aims
The current study, using a cross-sectional experimental design, aimed to investigate maladaptive and adaptive responses to three task-based analogues of PEs (thought interference, mind reading and voice-hearing) in a large sample consisting of three groups: people with persistent PEs with and without a need-for-care, and a control group without PEs.
Hypotheses
(1) The non-clinical group will endorse fewer maladaptive response styles than the clinical group following three experimental symptom analogues, but will not differ from controls.
(2) The non-clinical group will endorse more adaptive (‘decentring’) response styles than the clinical group following three experimental symptom analogues but will not differ from controls.
Methods
This was a planned study conducted within the larger UNIQUE study reported elsewhere (Peters et al., Reference Peters, Ward, Jackson, Morgan, Charalambides, McGuire, Woodruff, Jacobsen, Chadwick and Garety2016; Peters et al., Reference Peters, Ward, Jackson, Woodruff, Morgan, McGuire and Garety2017).
Design
The study is a cross-sectional experimental design, comparing three groups on responses to three tasks that induce anomalous experiences.
Participants
Three groups were recruited across two sites (urban – South London; rural – North Wales): (i) patients with PEs and diagnoses F20–F39 (clinical group); (ii) individuals with PEs without need-for-care (non-clinical group); (iii) controls with no PEs, matched to non-clinical group in age, gender, ethnicity and education.
Exclusion (all groups): (i) age <18; (ii) insufficient English; (iii) neurological history, head injury, epilepsy; (iv) primary substance dependence.
Main inclusion criterion for clinical/non-clinical groups was evidence of current PEs (past month/in clear consciousness), scoring ⩾2 (‘occasional’) on at least one item of the Scale for the Assessment of Positive Symptoms (SAPS) (Andreasen, Reference Andreasen1984b). Specific inclusion criteria for non-clinical group: (i) experiences started ⩾5 years previously (avoiding possibly prodromal individuals); (ii) did not score 2 (‘unmet need’) on basic self-care and ‘psychological distress’ items (relating to PEs) of Camberwell Assessment of Need Short Appraisal Schedule [CANSAS (Slade et al., Reference Slade, Loftus, Phelan, Thornicroft and Wykes1999)]; (iii) no previous contact with mental health services/general practitioner regarding PEs (nor anyone on their behalf); (iv) no previous contact with specialist mental health provision not available through general/family practitioner; (v) judged by research worker to not be in need-of-care for PEs. A specific exclusion criterion for controls was endorsement of any unusual experience item at screening. For additional information on these groups, see Peters et al. (Reference Peters, Ward, Jackson, Morgan, Charalambides, McGuire, Woodruff, Jacobsen, Chadwick and Garety2016) and Ward et al. (Reference Ward, Peters, Jackson, Day and Garety2018).
Measures
Screening
The clinical group were screened through clinician and/or case-note review. The non-clinical and control groups were screened with the Unusual Experiences Screening Questionnaire [UESQ; derived from the AANEX-Inventory (Brett et al., Reference Brett, Peters, Johns, Tabraham, Valmaggia and McGuire2007)] and the Psychosis Screening Questionnaire (PSQ) (Bebbington and Nayani, Reference Bebbington and Nayani1995). As well as no endorsement of any item on these measures, controls were required to score below one standard deviation of the mean on the Unusual Experiences (UnEx) subscale (i.e. a cut-off score of 15) of the Oxford-Liverpool Inventory of Feelings and Experiences (O-LIFE) (Mason and Claridge, Reference Mason and Claridge2006). Detailed information on the screening of participants is provided in Peters et al. (Reference Peters, Ward, Jackson, Morgan, Charalambides, McGuire, Woodruff, Jacobsen, Chadwick and Garety2016)
Appraisals of Anomalous Experiences Interview (AANEX) (Brett et al., Reference Brett, Peters, Johns, Tabraham, Valmaggia and McGuire2007): The first part of the interview (AANEX-Inventory, short form) (Lovatt et al., Reference Lovatt, Mason, Brett and Peters2010) was used, which consists of 17 anomalous experiences (including hearing voices, somatic experiences, experiences of reference and thought/mind permeability) that are rated on a three-point scale (1 = not present; 2 = unclear; 3 = present; potential range of scores 17–51) in the person's lifetime, and currently (within the last month). All inter-rater reliabilities (N = 35) indicated almost perfect agreement [Intra-class Correlation Coefficient (ICC) >0.8]: total number of experiences endorsed (ICC = 0.995); current experiences (ICC = 0.997); lifetime experiences (ICC = 0.998).
Experimental tasks
(a) Cards Task (http://sprott.physics.wisc.edu/pickover/esp2.html) (Linney and Peters, Reference Linney and Peters2007): This task was used as an ‘analogue’ of thought interference symptoms. This is a card trick that gives the impression that a computer has been able to read your mind. Participants are shown six playing cards (face cards only) on a computer, from which they are required to inwardly choose and memorise one. They are informed that the card they have chosen will be selected by the computer and removed from the pile. They are then shown five different cards (ensuring that the card they have chosen will be absent) for 3 s. This task relies on the fact that people only scan for the card they have chosen and do not notice that all the cards are different.
Table 2. Group means of adaptive and maladaptive response styles with significance tests, Sidak-adjusted p-values (Wright, Reference Wright1992) and effect sizes

a Four missing.
b One missing.
c Two missing.
d Six missing.
e Three missing.
*Fails test of Homogeneity of variance – Welch's F (Welch, Reference Welch1951) used. All p values are Sidak adjusted Wright (Reference Wright1992) for six multiple tests for adaptive and maladaptive response ratings and three for individual group comparisons. CT = Cards Task; VASP = Virtual Acoustic Space Paradigm; TP = Telepath app. Bold denotes p < .05 and associated Cohen's D.
(b) Telepath phone application (http://richardwiseman.wordpress.com/2009/11/24/wanttoreadapersonsmind/): Like the Cards Task, the telepath task is an analogue of thought interference, specifically ‘mindreading’ and assesses appraisals of a trick presented on an Apple Iphone application. Four numbers (1–4) are presented on the screen to the participant who is required to choose one number. The phone is then shaken before being placed face down in front of the participant. At this stage, the participant is asked to reveal their choice to the experimenter. Unknown to the participant, shaking the phone activates an animation in the phone, which then cycles through each number with the transition signalled by a sparkle sound of music, enabling the experimenter to keep track. When the phone is turned around by the experimenter, the animation freezes and ‘magically’ reveals the number chosen by the participant.
(c) Virtual Acoustic Space Paradigm (Hunter et al., Reference Hunter, Griffiths, Farrow, Zheng, Wilkinson, Hegde, Woods, Spence and Woodruff2003): This task was used as an analogue of voice-hearing (see Ward et al., Reference Ward, Gaynor, Hunter, Woodruff, Garety and Peters2014; Underwood et al., Reference Underwood, Kumari and Peters2016). This paradigm permits sounds to be perceived as externally spatially located through modification of acoustic stimuli, despite presentation via headphones (normally perceived as spatially located ‘inside the head’). Participants are told that the task assesses the effects of distraction on performance, and are asked to determine the presence of objects in blurred images while wearing headphones. Throughout the task the participant hears white noise (heard inside the head) with his or her own name (recorded by the research worker before the start of the experiment) followed by the command ‘listen up’ superimposed at random times (heard outside the head).
Tasks validity
The tasks have demonstrated good face validity in terms of inducing anomalous experiences in previously published studies (Linney and Peters, Reference Linney and Peters2007; Ward et al., Reference Ward, Gaynor, Hunter, Woodruff, Garety and Peters2014; Underwood et al., Reference Underwood, Kumari and Peters2016; Peters et al., Reference Peters, Ward, Jackson, Woodruff, Morgan, McGuire and Garety2017). In the current study, tasks were rated as moderately striking while not being unduly distressing [N = 254; Cards Task: mean salience = 4.63 (s.d. = 3.20); distress = 0.66 (s.d. = 1.71); Telepath: salience = 4.49 (s.d. = 3.69); distress = 0.60 (s.d. = 1.55); VASP: salience = 4.09 (s.d. = 3.18); distress = 1.85 (s.d. = 2.81)]. The large majority of participants did not guess the true nature of the tasks (Cards Task: clinical = 95%, non-clinical = 86%, control = 84%; Telepath: clinical = 99%, non-clinical = 93%, control = 95%). This percentage was lower on the VASP (clinical = 86%, non-clinical = 82%, control = 61%), although it was still rated as equally striking, and slightly more distressing, than the other tasks. There were no group differences in percentage correctly guessing on the Cards Task (χ2 = 5.5, df = 2, p = 0.64) or Telepath (χ2 = 3.2, df = 2, p = 0.21), but there was on the VASP (χ2 = 16.8, df = 2, p < 0.001), which was driven by higher rates of correct guesses in the controls compared with both the clinical (χ2 = 13.2, df = 1, p < 0.001) and non-clinical (χ2 = 9.6, df = 1, p = 0.002) groups, who did not differ from each other (χ2 = 0.52, df = 1, p = 0.47).
Assessment of response styles
After each experimental analogue, participants were asked to rate their endorsement of a number of specified response styles on 0–10 Visual Analogue Scales using the same categorisation of response styles as earlier work (Ward et al., Reference Ward, Gaynor, Hunter, Woodruff, Garety and Peters2014). The two adaptive responses captured different methods of ‘decentring’ either through cognitive reappraisal or mindful acceptance. The maladaptive responses (six items) included three styles: ‘active resistance’ (avoidance or attempts to control the experience), ‘active engagement’ (immersion or rumination) and ‘passive style’ (giving up or reliance on others). Means scores were calculated for the six maladaptive and two adaptive items. This categorisation was developed from the AANEX-CAR (Brett et al., Reference Brett, Peters, Johns, Tabraham, Valmaggia and McGuire2007) integrating dimensions of responding noted elsewhere in the literature [e.g. the ‘active/passive’ and ‘acceptance/rejection’ dimensions proposed by O'Sullivan (Reference O'Sullivan1994) as well as the work of Chadwick and Birchwood (Reference Chadwick and Birchwood1994); Birchwood and Chadwick (Reference Birchwood and Chadwick1997); Farhall and Gehrke (Reference Farhall and Gehrke1997)]. See Appendix 1 for details on specific items.
Procedures
Ethical and research governance approvals were given by: National Research Ethics Service Committee London–Westminster (Ref: 12/LO/0766), South London & Maudsley/Institute of Psychiatry Research &Development (R&D) Office (Ref: R&D2012/047) and Betsi Cadwaladr University Health Board R&D Office (Reference: Jackson/LO/0766). Participants were screened over the phone or in person. Eligible participants completed all assessments and were given an honorarium.
Statistical analysis
Analysis was conducted using SPSS (Version 24). Data were first visually inspected (using histograms and scatter plots) to check for normal distributions of response style data. For each task, analysis of variance was then used to compare the three groups on means of maladaptive and adaptive responses. Where the main group effect was significant, post-hoc (Tukey) tests were conducted to test for specific group differences. Sidak-adjusted p-values are presented to account for multiple testing (Wright, Reference Wright1992). These are calculated as pSidak = 1 – (1 – unadjusted p)n, where n is the number of multiple tests. In order to limit the number of significance tests, the individual response ratings for each task were not analysed separately. Effect sizes (Cohen's d; Cohen, Reference Cohen1988) with accompanying 95% confidence intervals are reported for post-hoc group comparisons.
A methodological issue that arises when comparing clinical and non-clinical individuals with PEs is the finding that these groups show differences in a range of demographic and clinical variables (Ward et al., Reference Ward, Gaynor, Hunter, Woodruff, Garety and Peters2014; Peters et al., Reference Peters, Ward, Jackson, Morgan, Charalambides, McGuire, Woodruff, Jacobsen, Chadwick and Garety2016). These are naturally occurring group differences, which include variables that reflect established risk factors for the development of need-for-care, such as low IQ/poorer pre-morbid functioning and ethnicity (Coid et al., Reference Coid, Kirkbride, Barker, Cowden, Stamps, Yang and Jones2008; Kirkbride et al., Reference Kirkbride, Errazuriz, Croudace, Morgan, Jackson, Boydell, Murray and Jones2012; Kendler et al., Reference Kendler, Ohlsson, Sundquist and Sundquist2015) and/or are sequelae of group status (such as impaired functioning, social isolation and anxiety). The view that ANCOVA (analysis of covariance, still commonly employed in psychological research) should be used to achieve the goal of ‘controlling for’ such real group differences has been condemned (Miller and Chapman, Reference Miller and Chapman2001), with the most appropriate use of ANCOVA suggested to be for designs that involve a random allocation of participants to groups. Consistent with earlier studies (Peters et al., Reference Peters, Ward, Jackson, Woodruff, Morgan, McGuire and Garety2017; Ward et al., Reference Ward, Peters, Jackson, Day and Garety2018), we therefore report group differences on our hypothesised variables, without including as covariates in the analysis clinical and demographic variables in which the groups naturally differ.
Results
Demographics and clinical data
The groups (clinical group n = 84; non-clinical group n = 92; controls n = 83) did not differ in age. In line with previous research, the non-clinical group was more likely to be female, and non-clinical and control groups were less likely to belong to black or minority ethnic groups, had higher IQ and were more likely to be in education/employment/training. The non-clinical group had a younger age of onset of their PEs than the clinical group, with 77.2% reporting voices during their lifetime. Overall they were less symptomatic than the clinical group on the SAPS (Andreasen, Reference Andreasen1984b) and SANS (Andreasen, Reference Andreasen1984a) although not significantly different on the AANEX (Brett et al., Reference Brett, Peters, Johns, Tabraham, Valmaggia and McGuire2007), a measure designed to assess anomalous experiences across the psychosis continuum. The non-clinical group experienced hallucinations in all modalities as well as first-rank symptoms, but scored lower on global delusions (with minimal endorsement of paranoid or grandiose delusions). Ideas of reference were the most commonly rated delusion in the non-clinical group, but these were still less common than in the clinical group. The non-clinical group also reported fewer cognitive difficulties and negative symptoms; see Peters et al. (Reference Peters, Ward, Jackson, Morgan, Charalambides, McGuire, Woodruff, Jacobsen, Chadwick and Garety2016) for further information and a full discussion of these group differences.
Hypothesis 1:
The non-clinical group will endorse fewer maladaptive response styles than the clinical group following three experimental symptom analogues, but will not differ from controls.
As hypothesised, there was a significant association between group and maladaptive responding replicated across the three experimental tasks, which was maintained following statistical adjustment for multiple testing. Post-hoc tests showed that for each task the clinical group scored significantly higher than the non-clinical group for maladaptive responding (large effect sizes on Telepath and Cards Task, medium effect size in VASP) and significantly higher than the control group on the Cards Task and Telepath (medium effect sizes) but not the VASP. There were no significant differences between the non-clinical and control groups on any task after adjusting for multiple testing.
Hypothesis 2:
The non-clinical group will endorse more adaptive (‘decentring’) response styles than the clinical group following three experimental symptom analogues but will not differ from controls.
The non-clinical group did not differ from controls in line with the hypothesis. However, contrary to our hypothesis, there were no significant group differences in adaptive response styles between the non-clinical and clinical groups on any task.
Individual response ratings
Individual response ratings for each task were not subjected to statistical testing (see above) but are presented graphically in Fig. 1 for illustrative purposes. The figure shows a consistent pattern on maladaptive scoring across the three tasks with the non-clinical group tending to score lowest and the clinical group tending to score highest on the majority of maladaptive items. On adaptive items, the pattern is less consistent with the non-clinical group showing higher endorsement than clinical group for reappraisal (as predicted), but the opposite pattern observed for endorsement of mindfulness on two of the three tasks.
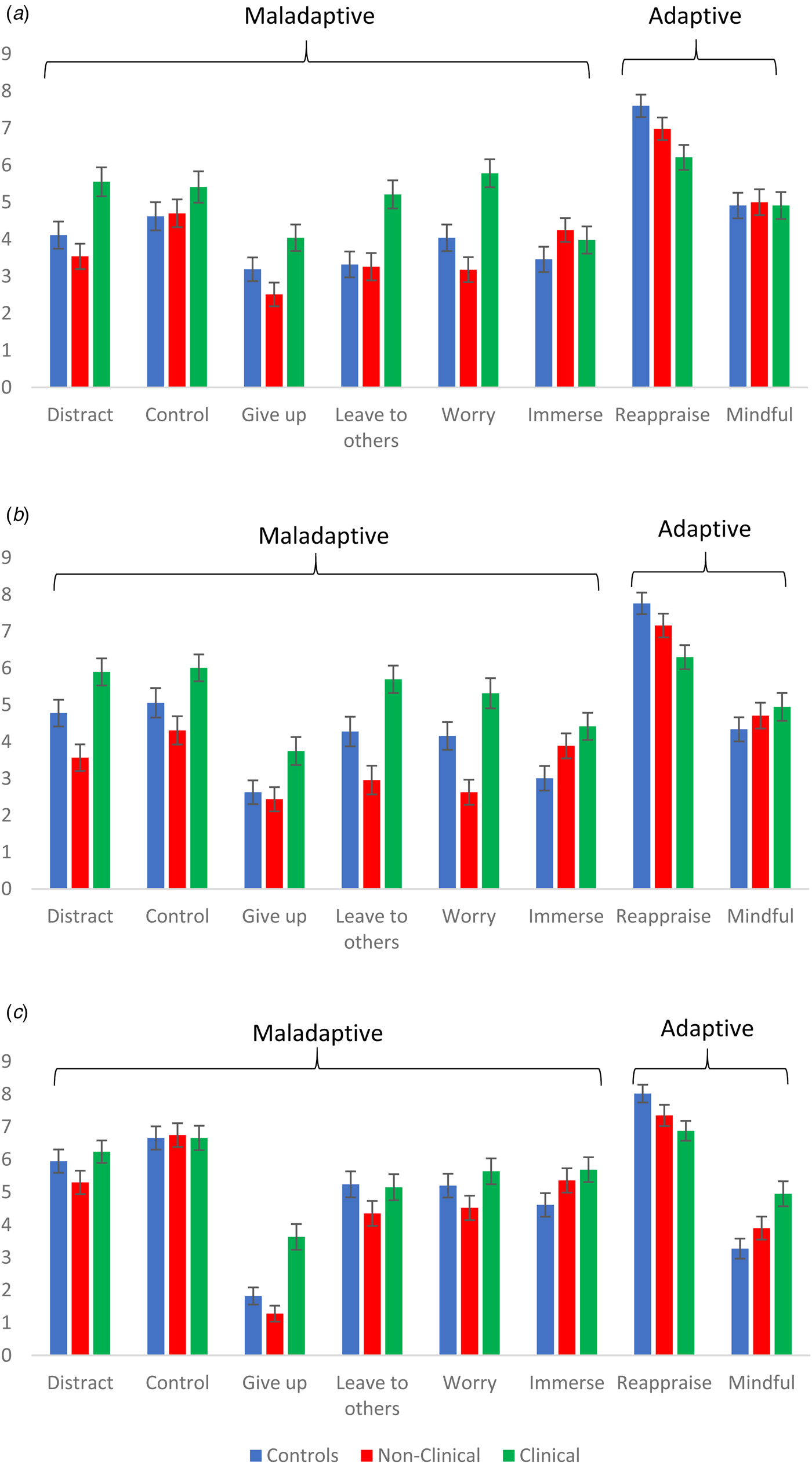
Fig. 1. Pattern of individual responses across each task. Data are means (error bars represent Standard Errors). (a) Cards Task: controls n = 82; non-clinical n = 92; clinical n = 80. (b) Telepath: controls n = 82; non-clinical n = 90 (n = 88 for ‘Give up’); clinical n = 81. (c) VASP: controls n = 83; non-clinical n = 92 (91 for ‘Distract’, ‘Worry’, ‘Immerse’, ‘Mindful’); clinical n = 78.
Discussion
As predicted, unhelpful ways of responding to PEs differed between non-clinical and clinical groups. These results suggest that maladaptive responding may be an important factor in contributing to developing and maintaining need for clinical care in the context of PEs. Using a novel experimental paradigm, permitting presentation of the same anomalous experiences across groups, we have shown that certain types of responding, including attempts to avoid, suppress, worry about or try to control mental experiences are characteristic of need-for-care and are not a simple consequence of having PEs. Notably, individuals who have PEs without developing a clinical need show lower rates of these potentially unhelpful response styles, performing similarly to controls with no PEs. However, contrary to hypothesis, group differences were not observed in potentially adaptive ‘decentring’ responses including cognitive reappraisal and mindfulness.
The main findings are consistent with previous work identifying safety-seeking behaviours, notably avoidance (Freeman et al., Reference Freeman, Garety and Kuipers2001; Freeman et al., Reference Freeman, Garety, Kuipers, Fowler, Bebbington and Dunn2007; Gaynor et al., Reference Gaynor, Ward, Garety and Peters2013; Moritz et al., Reference Moritz, Ludtke, Westermann, Hermeneit, Watroba and Lincoln2016b), worry and rumination (e.g. Vorontsova et al., Reference Vorontsova, Garety and Freeman2013; Hartley et al., Reference Hartley, Haddock, Sa, Emsley and Barrowclough2014; Freeman et al., Reference Freeman, Dunn, Startup, Pugh, Cordwell, Mander, Cernis, Wingham, Shirvell and Kingdon2015) and unhelpful emotional regulation strategies (O'Driscoll et al., Reference O'Driscoll, Laing and Mason2014) as important processes associated with clinical psychosis. The current study also explored adoption of a passive, ‘powerless’ stance in the face of ongoing experiences, reflecting the ‘social defeat’ commonly reported by individuals with psychosis (Birchwood et al., Reference Birchwood, Meaden, Trower, Gilbert and Plaistow2000; Birchwood et al., Reference Birchwood, Gilbert, Gilbert, Trower, Meaden, Hay, Murray and Miles2004), which has become a key target of relational approaches to voices (Hayward et al., Reference Hayward, Jones, Bogen-Johnston, Thomas and Strauss2017; Craig et al., Reference Craig, Rus-Calafell, Ward, Leff, Huckvale, Howarth, Emsley and Garety2018).
This study was also a novel test of a key tenet of cognitive models of psychosis. These results accord with cognitive models of both voice-hearing (Chadwick and Birchwood, Reference Chadwick and Birchwood1994; Birchwood and Chadwick, Reference Birchwood and Chadwick1997; Morrison, Reference Morrison2001) and paranoia (Freeman et al., Reference Freeman, Garety, Kuipers, Fowler and Bebbington2002; Freeman, Reference Freeman2016), which propose that such understandable but ultimately unhelpful ways of responding to PEs can maintain distress and therefore represent important treatment targets. Other studies from the larger UNIQUE project have demonstrated significant differences in the appraisals of these same anomalous experiences, specifically, the absence of paranoid and threatening appraisals in the non-clinical group (Peters et al., Reference Peters, Ward, Jackson, Woodruff, Morgan, McGuire and Garety2017). Gaynor et al. (Reference Gaynor, Ward, Garety and Peters2013) also demonstrated that the link between safety behaviours and distress in individuals with PEs is mediated by threat appraisals. Results from studies investigating this important non-clinical group who present with PEs in the absence of need-for-care are therefore consistent with the postulated links between appraisal and responding inherent to cognitive models of psychosis. In short, anomalous experiences appraised as threatening may increase the use of safety behaviours (in particular avoidance) in concert with both affective and attentional processes (such as hypervigilance to danger), thereby setting up interactive causal and maintenance processes which form the basis of cognitive formulation and treatment (Morrison, Reference Morrison2001; Freeman et al., Reference Freeman, Garety, Kuipers, Fowler and Bebbington2002; Garety et al., Reference Garety, Bebbington, Fowler, Freeman and Kuipers2007; Freeman, Reference Freeman2016).
Strengths and limitations
A key strength of this study is the comparison of three groups who differ with respect to PEs, and in particular the inclusion of the non-clinical group whose persistent PEs in the absence of distress make them important in terms of identifying factors that may protect against development of ‘need-for-care’ in the context of PEs. The evidence that this group is less likely to endorse the potentially unhelpful responding that is characteristic of the clinical group is part of an emerging picture of protective factors in this non-clinical group. In addition to the absence of paranoid and threatening appraisals noted above, this group is more likely to report positive social networks and show a preserved ability to engage in slower analytical thinking around their unusual experiences and less tendency to jumping to conclusions (Ward et al., Reference Ward, Peters, Jackson, Day and Garety2018). Protective factors are likely to operate in concert. For example, one could postulate that membership of sub-cultural groups where unusual experiences are validated may be facilitative in developing more flexible processes of appraisal, reasoning and responding, in keeping with the finding that belief flexibility in clinical populations may be associated with the presence of a carer (Jolley et al., Reference Jolley, Ferner, Bebbington, Garety, Dunn, Freeman, Fowler and Kuipers2014).
A second major strength is the experimental design. The use of experimentally controlled experiences counteracts limitations of retrospective self-report and the potential confound of PEs varying across groups. The large sample of three groups of people, with persistent PEs with and without a need-for-care and a control group without PEs, yields group differences on responding with consistent medium–large effect sizes, which replicate and extend previous work (Ward et al., Reference Ward, Gaynor, Hunter, Woodruff, Garety and Peters2014), and can therefore be considered robust.
With regards to limitations, the cross-sectional design means the possibility cannot be excluded that associations between maladaptive responding and need-for-care may be epiphenomenal to, or a consequence of, need-for-care, or relate only to specific resilience factors on which the groups differ. The anomalous experiences were designed to be deliberately mild in nature. Therefore, the current findings need to be viewed in the context of responses to simulacra of experiences that in daily life typically provoke stronger affective responses. While previous research indicates that maladaptive coping in particular appears closely related to emotion and emotional regulation (see, e.g. O'Driscoll et al., Reference O'Driscoll, Laing and Mason2014), the role of emotion has not been directly investigated in the current study. Nevertheless, evidence that the same mild experiences can trigger paranoid appraisals and be incorporated into ongoing PEs in clinical individuals (Peters et al., Reference Peters, Ward, Jackson, Woodruff, Morgan, McGuire and Garety2017) provides additional evidence for the validity of the tasks.
Any individual response can be viewed as fundamentally context-bound (Aldao, Reference Aldao2013). Response styles characterised as helpful/adaptive and unhelpful/maladaptive may fit more or less well into these categories depending on the specific context. For example, while distraction can form part of a broader picture of unhelpful responding involving avoidance and suppression, it is also a commonly used coping strategy (often advocated by professionals), which can allow the person to engage in positive activities they might otherwise avoid. In addition, while clear differences on maladaptive responding were observed, the expected differences in adaptive responding were not found. Of note here are findings that maladaptive coping may be more stable and less context-dependent than adaptive coping and more strongly related to psychopathology (Aldao and Nolen-Hoeksema, Reference Aldao and Nolen-Hoeksema2010, Reference Aldao and Nolen-Hoeksema2012; Moritz et al., Reference Moritz, Jahns, Schroder, Berger, Lincoln, Klein and Goritz2016a). The tasks in the current study may therefore be better equipped to tap into more stable maladaptive response orientations with potential differences in adaptive responding better suited to context-bound in situ assessment, for example, through use of ESM (Bak et al., Reference Bak, Drukker, van Os, Delespaul and Myin-Germeys2012; Myin-Germeys et al., Reference Myin-Germeys, Kasanova, Vaessen, Vachon, Kirtley, Viechtbauer and Reininghaus2018). Finally, only two items tapped adaptive responding (cognitive reappraisal and mindful responding) in contrast to six for maladaptive responding. There may have been other important adaptive responses not captured in the current study; of note is the pattern that the non-clinical group consistently showed higher endorsement than the clinical group on cognitive reappraisal but the opposite pattern was seen for two of the tasks for mindfulness, while the adaptive mean showed higher standard deviation than the maladaptive mean.
Theoretical and clinical implications
Cognitive models of psychosis propose that the ways in which individuals appraise and respond to PEs are crucial in the development and maintenance of distress. Evidence of benign (even positive) PEs occurring in the general population indicates that the fact that an experience is psychotic is not sufficient to cause a need-for-care. In addition to the key role ascribed to processes of appraisal and meaning-making, this study provides evidence for the importance of response style in understanding clinical distress, supporting the rationale of targeting unhelpful responding (encompassing behavioural, attentional, affective and relational processes) in interventions for distressing voices (Thomas et al., Reference Thomas, Hayward, Peters, van der Gaag, Bentall, Jenner, Strauss, Sommer, Johns, Varese, Garcia-Montes, Waters, Dodgson and McCarthy-Jones2014) and paranoia (Freeman and Garety, Reference Freeman and Garety2014; Freeman, Reference Freeman2016). Clinical formulation needs to strike a balance between the reduction of unhelpful responding and increasing potentially adaptive strategies. Consistent with the current findings, stronger associations with psychopathology have been found for maladaptive compared with adaptive strategies (Aldao and Nolen-Hoeksema, Reference Aldao and Nolen-Hoeksema2010, Reference Aldao and Nolen-Hoeksema2012; Moritz et al., Reference Moritz, Ludtke, Westermann, Hermeneit, Watroba and Lincoln2016b). It has been argued that reducing maladaptive coping may be more important for outcome than increasing adaptive strategies (Moritz et al., Reference Moritz, Ludtke, Westermann, Hermeneit, Watroba and Lincoln2016b), although focus and timing of clinical interventions is likely to be crucial.
Future directions
Psychosis is complex, multi-factorial and dynamic (Garety et al., Reference Garety, Bebbington, Fowler, Freeman and Kuipers2007). Having established the key tenets of cognitive models of psychosis regarding the centrality of appraisal and response, the time is ripe to investigate the interactive causal and maintenance processes that by nature vary across individuals, situations and time. Complex inter-relationships between social context, appraisal, reasoning and response will be illuminated by digital technology allowing dynamic real-world assessment and real-time feedback (Reininghaus et al., Reference Reininghaus, Depp and Myin-Germeys2016a, Reference Reininghaus, Kempton, Valmaggia, Craig, Garety, Onyejiaka, Gayer-Anderson, So, Hubbard, Beards, Dazzan, Pariante, Mondelli, Fisher, Mills, Viechtbauer, McGuire, van Os, Murray, Wykes, Myin-Germeys and Morgan2016b; Malhi et al., Reference Malhi, Hamilton, Morris, Mannie, Das and Outhred2017; Rus-Calafell et al., Reference Rus-Calafell, Garety, Sason, Craig and Valmaggia2018). Questions of causality will be elucidated by a ‘causal-interventionist’ approach to improving therapy effectiveness, involving tailored interventions to target specific putative causal mechanisms (Freeman, Reference Freeman2011; Mehl et al., Reference Mehl, Werner and Lincoln2015; Freeman et al., Reference Freeman, Bradley, Waite, Sheaves, DeWeever, Bourke, McInerney, Evans, Cernis, Lister, Garety and Dunn2016). Future research will increasingly harness the power of novel statistical techniques such as network analysis (Looijestijn et al., Reference Looijestijn, Blom, Aleman, Hoek and Goekoop2015; Isvoranu et al., Reference Isvoranu, van Borkulo, Boyette, Wigman, Vinkers and Borsboom2017; Bell and O'Driscoll, Reference Bell and O'Driscoll2018). These technological and analytic developments, underpinned by theory, will allow both the refinement of models and the improvement of targeted, individualised psychological treatments for psychosis, supporting individuals to tackle unhelpful patterns of responding and to promote flexible, adaptive alternatives which ultimately improve quality of life.
Author ORCIDs
Thomas Ward, 0000-0002-7608-5755
Acknowledgements
Study supported by Medical Research Council (Reference: G1100568). TW acknowledges support by the National Institute for Health Research (NIHR) collaboration for Leadership in Applied Health Research and Care South London at King's College Hospital NHS Foundation Trust. PAG acknowledges support from the National Institute for Health Research (NIHR) Biomedical Research Centre of the South London and Maudsley NHS Foundation Trust and King's College London. The views expressed are of the author(s).
Conflict of interest
None.
Maladaptive Response styles
‘Active resistance’ – analogous to ‘resistance’ (Chadwick and Birchwood, Reference Chadwick and Birchwood1994) and mirroring ‘resistance coping’ (Farhall and Gehrke, Reference Farhall and Gehrke1997). Includes:
Avoidance/distraction
‘I would find ways to escape these experiences or take my mind off them’.
Attempts to control the experience.
‘I would find ways to control these things or stop them from happening’.
‘Active engagement’ – Including:
Immersion in experience (including active listening and compliance) – seen as analogous to ‘engagement’ (Chadwick and Birchwood, Reference Chadwick and Birchwood1994), overlapping with ‘immersion’ style (Brett et al., Reference Brett, Peters, Johns, Tabraham, Valmaggia and McGuire2007) and ‘symptomatic coping’ (Bak et al., Reference Bak, Myin-Germeys, Hanssen, Bijl, Vollebergh, Delespaul and van Os2003).
‘I would listen closely to these voices’ (VASP).
‘I would try to get into these experiences as much as possible’ (Cards Task and Telepath).
Rumination (non-decentring) (Brett et al., Reference Brett, Peters, Johns, Tabraham, Valmaggia and McGuire2007).
‘I would worry about the experiences, running them over and over in my mind, trying to get to the bottom of what they mean’ (all tasks).
‘Passive style’ – Including:
Trusting in external sources (e.g. trusting in God) – this mirrors ‘passive coping’ (Farhall and Gehrke, Reference Farhall and Gehrke1997) and would correspond to passive, hopeful, acceptance according to the dimensions of (O'Sullivan, Reference O'Sullivan1994).
‘I would trust that someone/something would sort this out for me’.
‘Giving up’ [corresponding to passive, despairing acceptance according to the dimensions of O'Sullivan (Reference O'Sullivan1994)].
‘I would give up – there is nothing I can do about it’.
Adaptive Response styles
‘De-centring style’
Active acceptance and disengaging (Mindful response style) – overlapping with the ‘Neutral response’ of Brett et al. (Reference Brett, Peters, Johns, Tabraham, Valmaggia and McGuire2007).
‘I would let the experiences come and go without getting involved with them’.
Active cognitive reappraisal of experiences (‘Appraisal – Decentring’) (Brett et al., Reference Brett, Peters, Johns, Tabraham, Valmaggia and McGuire2007).
‘I would try to think of a sensible explanation of the experiences/find different way of thinking about them’.





