Introduction
The link between mood disorders, including depression and dysthymia (American Psychiatric Association, 2000), and cardiovascular disease have long been recognized (Seligman & Nemeroff, Reference Seligman and Nemeroff2015). Recent evidence suggests that the elevated risk of cardiovascular disease in people with mood disorders can be accounted for by their higher prevalence of risk behaviours, such as smoking and physical inactivity (Ye et al. Reference Ye, Muntner, Shimbo, Judd, Richman, Davidson and Safford2013). Of interest is that several risk behaviours have bi-directional associations with mood disorders. For example, smoking is associated with an increased risk of developing depression and having depression is associated with an increased likelihood of taking up smoking (Chaiton et al. Reference Chaiton, Cohen, O'Loughlin and Rehm2009). Similar findings have been reported for physical activity (McKercher et al. Reference McKercher, Sanderson, Schmidt, Otahal, Patton, Dwyer and Venn2014) and weight (De Wit et al. Reference De Wit, Luppino, Van Straten, Penninx, Zitman and Cuijpers2010; Sanderson et al. Reference Sanderson, Patton, McKercher, Dwyer and Venn2011).
Studying individual risk factors and their relationship with mood disorders ignores the fact that risk factors often cluster as unhealthy lifestyles in younger (Raitakari et al. Reference Raitakari, Leino, Rakkonen, Porkka, Taimela, Rasanen and Viikari1995; Gall et al. Reference Gall, Jamrozik, Blizzard, Dwyer and Venn2009) and older (Van Dam et al. Reference Van Dam, Li, Spiegelman, Franco and Hu2008) adults. Unhealthy lifestyles predict all-cause mortality, cardiovascular disease and type 2 diabetes (Spencer et al. Reference Spencer, Jamrozik, Norman and Lawrence-Brown2005; Khaw et al. Reference Khaw, Wareham, Bingham, Welch, Luben and Day2008; Van Dam et al. Reference Van Dam, Li, Spiegelman, Franco and Hu2008) but there has been little investigation of whether such lifestyles predict mood disorders. Understanding the associations between healthy lifestyles and mood disorders has implications for reducing cardiovascular risk in those with mood disorders and potentially reducing the burden of mood disorders. There is also a desire to find non-pharmacological ways to manage mood disorders given the modest effects of pharmacological agents in many people (Undurraga & Baldessarini, Reference Undurraga and Baldessarini2012; Seligman & Nemeroff, Reference Seligman and Nemeroff2015).
The rationale for this research question comes from the known biological links between unhealthy behaviours and mood disorders. Such behaviours are associated with inflammatory and immune pathways (Giugliano et al. Reference Giugliano, Ceriello and Esposito2006; Walsh et al. Reference Walsh, Gleeson, Shephard, Woods, Bishop, Fleshner, Green, Pedersen, Hoffman-Goetz, Rogers, Northoff, Abbasi and Simon2011) that affect the neurobiological pathways associated with mood disorders (Berk et al. Reference Berk, Kapczinski, Andreazza, Dean, Giorlando, Maes, Yucel, Gama, Dodd, Dean, Magalhaes, Amminger, McGorry and Malhi2011). Conversely, those with a mood disorder may engage in unhealthy behaviours in an attempt to control their mood. For example, nicotine and alcohol affect neurotransmitter systems related to the symptoms of mood disorders (Markou et al. Reference Markou, Kosten and Koob1998).
Our aim was to examine the bi-directional associations between healthy lifestyles and mood disorders in a cohort of young adults followed for 5 years. Based on the associations between mood disorders and individual risk factors, we hypothesized that those with a history of mood disorder would have unfavourable trajectories of their lifestyle and that healthier lifestyles would protect against mood disorder.
Method
Participants
This study was part of the Childhood Determinants of Adult Health (CDAH) study that began in 1985 with a nationally representative study (response proportion 64%) of 8498 children between the ages of 7 to 15 years (Fig. 1) (Venn et al. Reference Venn, Thomson, Schmidt, Cleland, Curry, Gennat and Dwyer2007). Full details are provided in the online Supplementary material. In brief, in 2004–2006 (herein ‘baseline’), participants completed assessments of their lifestyle (n = 2407). In 2009–2011 (herein ‘follow-up’), participants were re-contacted, with 1233 completing assessments of lifetime mood disorder. Of these, 1041 also had complete lifestyle information at follow-up.
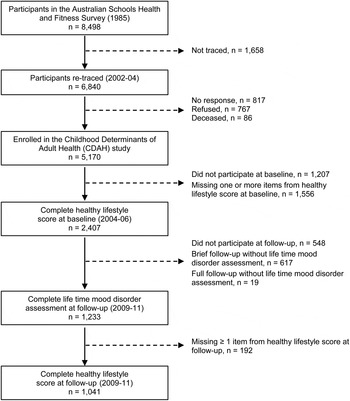
Fig. 1. Participation flow chart.
Measures
Mood disorder
The lifetime version of the Composite International Diagnostic Interview (CIDI-Auto 2.1 version; World Health Organization, 1997) was administered at follow-up providing retrospective lifetime diagnoses of major depression and dysthymia. Using dates of onset for the first and most recent episodes we classified people as having suffered from an episode of mood disorders before baseline, herein ‘history of mood disorder’, and those that experienced an episode between baseline and follow-up, herein ‘new episode of mood disorder’. This latter category could be separated into ‘recurrent’ and ‘first’ episodes of mood disorder.
Lifestyle risk factors
We calculated a Healthy Lifestyle Score at baseline and follow-up that is associated with biomedical cardiovascular risk factors in this cohort (Gall et al. Reference Gall, Jamrozik, Blizzard, Dwyer and Venn2009) and is similar to other scores (Khaw et al. Reference Khaw, Wareham, Bingham, Welch, Luben and Day2008; Lloyd-Jones et al. Reference Lloyd-Jones, Hong, Labarthe, Mozaffarian, Appel, Van Horn, Greenlund, Daniels, Nichol, Tomaselli, Arnett, Fonarow, Ho, Lauer, Masoudi, Robertson, Roger, Schwamm, Sorlie, Yancy and Rosamond2010). Our score comprised five ‘healthy’ items assigned one point each: body mass index (BMI) <25 kg/m2, never smoker or ex-smoker ⩾12 months, ⩾3 h of moderate to vigorous leisure time physical activity per week, ⩽20 g alcohol per day and for indicating a ‘healthy’ diet, scoring in the 75th percentile of a validated Dietary Guideline Index that assessed adherence to Australian dietary guidelines from a food frequency questionnaire (Sanjoti et al. Reference Sanjoti, David, Neville and Konrad2009). Details of item measurement are given in the online Supplementary material. The total score ranged from zero (no healthy behaviours) to five (all healthy behaviours).
Data analysis
History of mood disorder at baseline predicting changes in the Healthy Lifestyle Score between baseline and follow-up
We investigated whether a history of mood disorder before baseline predicted changes in the Healthy Lifestyle Score during follow-up (calculated as Healthy Lifestyle Scorefollow-up – Healthy Lifestyle Scorebaseline) using linear regression. Log multinomial regression was used to estimate the relative risk [RR ± 95% confidence interval (CI)] of changing category of the Healthy Lifestyle Score over follow-up by history of mood disorder before baseline. Healthy Lifestyle Scores at baseline and follow-up were categorized as low (zero to 2) or high (3 to 5) to make the following variable: highbaseline/highfollow-up (reference group); lowbaseline/highfollow-up; highbaseline/lowfollow-up; lowbaseline/lowfollow-up.
Sensitivity analyses were conducted excluding participants that developed an episode of mood disorder over follow-up, to explore potential reverse causation.
Healthy Lifestyle Score at baseline predicting episodes of mood disorder between baseline and follow-up
We estimated the RR (±95% CI) of having an episode of mood disorder between baseline and follow-up according to baseline Healthy Lifestyle Score using log binomial regression adjusted for covariates. The outcome was classified in several ways: (1) any new episode of mood disorder (i.e. first and recurrent) v. no new episode (this reference category included those with a history of mood disorder before baseline); (2) first v. no new episode (this reference category included those with a history of mood disorder before baseline); and (3) first v. no lifetime episode of mood disorder (this reference category excluded those with a history of mood disorder before baseline).
Sensitivity analyses included adjusting for baseline mental health [Short Form-12 (SF-12) mental component score; Ware et al. Reference Ware, Kosinski and Keller1996] and excluding those with subthreshold depressive symptoms in the 12 months before baseline (classified with CIDI 12-month version from baseline). The results are presented in the online Supplementary material. These were to explore whether mood disorders present at or before baseline, but below the threshold for Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV) diagnoses in the lifetime CIDI at follow-up, could explain any associations seen between baseline lifestyle and mood disorders during follow-up.
We also examined if the findings were influenced by particular health behaviours in the Healthy Lifestyle Score by re-running analyses with the score excluding BMI, physical activity, smoking and diet items. As an alternative way of considering the role of individual healthy lifestyle items, the association between each item in the Healthy Lifestyle Score and the risk of mood disorder was examined by entering each item alone into a model including confounders and then in a model mutually adjusted for all other items and confounders (see online Supplementary material).
Covariates
Covariates were included in accordance with purposeful model-building procedures, including the putative covariate being associated with the exposure and outcome (e.g. Healthy Lifestyle Score and mood disorders) and that the inclusion of the covariate in a model caused a change in the effect estimate of at least 10% (Greenland, Reference Greenland1989). The following potential covariates from baseline were considered: sex, age, highest attained education, area-level disadvantage, marital status, parental status, social support (Henderson Social Support Index; Henderson et al. Reference Henderson, Duncan-Jones, McAuley and Ritchie1978), personality (NEO five-factor inventory; Costa & McCrae, Reference Costa and McCrae1992), history of cardiovascular disease or diabetes (self-report or medication use), use of oral contraceptives (women only), self-rated physical and mental health-related quality of life (SF-12) (Ware et al. Reference Ware, Kosinski and Keller1996) and time between follow-ups. A 12-item life events inventory was administered at follow-up covering the 5 years since baseline (Brugha & Cragg, Reference Brugha and Cragg1990).
Multiple imputation using chained equations with 30 estimations was used to replace missing data on covariates. This method was used to replace missing data on the covariates listed above using the following variables from a previous follow-up of the cohort between 2001 and 2004 on sex, age, smoking status, education, BMI, state of residence, marital status, self-rated health and one variable from 1985 on scholastic ability.
We examined the effect of loss to follow-up on our results using inverse probability weighting, with weights based on the inverse of the probability of providing follow-up data given variables from a previous adult follow-up in 2001–2004 (sex, age, education, self-rated health, smoking and BMI) or, in a separate analysis, variables from childhood (age, sex, BMI, state of residence and three measures of cardiorespiratory fitness) (Seaman & White, Reference Seaman and White2013). Unweighted and weighted models, which did not have missing covariates imputed, were then compared. The results of these analyses are presented in the online Supplementary material. To examine the generalizability of our sample, we also compared our included participants with those not included using data from the 1985 study and the general Australian population of a similar age with data from the Australian Bureau of Statistics (Australian Bureau of Statistics, 2007; Australian Bureau of Statistics, 2011). These results are presented in the online Supplementary material.
There was no evidence of effect modification by sex (see online Supplementary material), so results for men and women are presented together. Analyses were conducted in Stata 12.0 (USA).
Ethical standards
All procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. Participants provided written informed consent and the study was approved by the Tasmanian Health and Medical Human Research Ethics Committee.
Results
The characteristics of participants are shown in Table 1. In general, participants were of higher socio-economic status and had healthier lifestyles than those lost to follow-up (see online Supplementary Results) or the Australian population of a similar age, with the exception of lifetime prevalence of mood disorders that were more common in the CDAH study (see online Supplementary Table S1).
Table 1. Characteristic of participants

s.d., Standard deviation; SF-12, Short Form-12.
a Women only.
Mood disorders as a predictor of the Healthy Lifestyle Score
Among the 1041 participants with data for these analyses, those with a history of mood disorder before baseline tended to have unfavourable trajectories of lifestyle (Fig. 2). Those with a history were less likely to improve their lifestyle (RR 0.76, 95% CI 0.49–1.18), more likely to worsen (RR 1.46, 95% CI 0.99–2.15) or stay in the low lifestyle score group (RR 1.30, 95% CI 1.01–1.66) than those without a history (Fig. 2, black squares). Models were adjusted for age, education, history of cardiovascular disease or diabetes, oral contraceptive use in females, area-level socio-economic status, social support and parental status.

Fig. 2. History of mood disorder before baseline as a predictor of categorical changes in the Healthy Lifestyle Score between baseline and follow-up for all participants (n = 1041) and excluding those that developed a mood disorder over follow-up (n = 934). Values are relative risk [95% confidence interval (CI)].
Sensitivity analyses excluding those that had a new episode of mood disorder over follow-up (n = 107, Fig. 2, grey squares) mostly strengthened the associations. For example, those with a history were less likely to improve their lifestyle (RR 0.46, 95% CI 0.21–1.01) and more likely to worsen (RR 1.95, 95% CI 1.18–3.22) than those without a history. Applying inverse probability weights did not appreciably change these results (see online Supplementary Results and Supplementary Fig. S1).
The findings using change in the continuous Healthy Lifestyle Score supported the categorical findings. Having a history of mood disorder before baseline was associated with worsening Healthy Lifestyle Score during follow-up, although the changes were small (β −0.18, 95% CI −0.35 to −0.01, p = 0.040) (online Supplementary Table S2). Sensitivity analyses excluding participants who developed a new episode of mood disorder over follow-up (n = 107) strengthened the association (β −0.28, 95% CI −0.52 to −0.04, p = 0.024). Applying inverse probability weights made small differences to these results (see online Supplementary Results and Supplementary Table S2).
Healthy Lifestyle Score as a predictor of mood disorder
Among the 1233 participants with data for these analyses, higher Healthy Lifestyle Scores at baseline protected against episodes of mood disorder over follow-up, particularly first episodes (Fig. 3). These analyses were adjusted for age, sex, education level, area-level disadvantage, time between follow-ups, history of cardiovascular disease, social support, having children, major life events and physical health-related quality of life. The relationship was such that each unit increase in the Healthy Lifestyle Score at baseline was associated with a 24% (RR 0.76, 95% CI 0.61–0.95) reduction in the risk of developing a first episode of mood disorder (n = 75) compared with a reference category of no new episode of mood disorder (n = 1158, Fig. 3, middle panel, black circle). The results were similar when the outcome compared first episodes (n = 75) with no lifetime history of mood disorder (n = 931, Fig. 3, final panel, RR 0.76, 95% CI 0.62–0.96).

Fig. 3. Healthy Lifestyle Score at baseline as a predictor of episodes of mood disorder between baseline and follow-up with adjustment for confounding factors and different measures of baseline mental health. Values are relative risk [95% confidence interval (CI)]. HRQoL, Health-related quality of life.
Sensitivity analyses explored if these findings were influenced by mental health at baseline. Adjusting the models for baseline mental health-related quality of life made no appreciable difference to the magnitude of the results, irrespective of the outcome classification used (Fig. 3, grey circles). Further, using the subset (n = 986) with data on the 12-month version of the CIDI administered at baseline we excluded those with threshold (n = 83) or subthreshold (n = 122) depression, which somewhat strengthened the results. As shown in Fig. 3 (white circles), each unit increase in the Healthy Lifestyle Score at baseline was associated with a significantly reduced risk of any new (i.e. first or recurrent) mood disorder episode (RR 0.79, 95% CI 0.65–0.97), or a first-ever episode (RR 0.67, 95% CI 0.51–0.89) or a first-ever episode compared with no lifetime history (RR 0.70, 95% 0.52–0.92).
Recalculating the Healthy Lifestyle Score to include only certain items (Fig. 4, grey circles) did not affect any of the results, suggesting that no single item was driving these associations. We also examined the association between individual items and the risk of mood disorder (see online Supplementary Table S3). All items were associated with a reduced risk of new episodes of mood disorder, particularly first-ever episodes, but only non-smoking appeared protective when all other items were included in a mutually adjusted model along with confounding factors.

Fig. 4. Sensitivity analyses examining Healthy Lifestyle Score (HLS) at baseline as a predictor of episodes of mood disorder between baseline and follow-up with exclusion of specific items from the HLS. Values are relative risk [95% confidence interval (CI)]. excl., Excluding; BMI, body mass index; LTPA, leisure time physical activity.
Applying inverse probability weights to account for loss to follow-up did not change the results for these analyses (online Supplementary Fig. S2).
Discussion
We found bi-directional associations between healthy lifestyles and mood disorders in young adults. People with healthier lifestyles at baseline were significantly less likely to develop a first episode of mood disorder over 5 years of follow-up. There was also a tendency for those with a history of mood disorder to have an unfavourable trajectory of their lifestyle over time.
This is the first study to consider the association between the number of health behaviours and risk of developing mood disorder over time. The association between healthy lifestyles and mood disorder was somewhat stronger for first than recurrent episodes. One potential explanation is the younger age of onset (around 10 years) between those with first and recurrent episodes in this study. There is some evidence that different risk factors are associated with development of mood disorders at different ages. For example, mood disorders with a younger age of onset are often associated with early childhood factors, such as perinatal insults and parental factors (Jaffee et al. Reference Jaffee, Moffitt, Caspi, Fombonne, Poulton and Martin2002). Our data suggest that a constellation of healthy behaviours is associated with a lower risk of depression in adulthood. This supports the limited randomized controlled trial evidence showing that lifestyle modification reduces depressive symptoms in older people at high risk for cardiovascular disease (Rubin et al. Reference Rubin, Wadden, Bahnson, Blackburn, Brancati, Bray, Coday, Crow, Curtis, Dutton, Egan, Evans, Ewing, Faulconbridge, Foreyt, Gaussoin, Gregg, Hazuda, Hill, Horton, Hubbard, Jakicic, Jeffery, Johnson, Kahn, Knowler, Lang, Lewis, Montez, Murillo, Nathan, Patricio, Peters, Pi-Sunyer, Pownall, Rejeski, Rosenthal, Ruelas, Toledo, Van Dorsten, Vitolins, Williamson, Wing, Yanovski, Zhang and Look2014). Targeting the health behaviours of young adults before the peak onset of mood disorders could have benefits in terms of reducing mood disorders, along with reducing the burden of cardiovascular disease, but this requires testing in well-designed intervention studies at either the population or individual level.
One possible explanation for our finding was that mood disorders before baseline that were subthreshold, therefore not identified using the standard diagnostic criteria, may have already resulted in poorer lifestyles, in a sense ‘reverse causation’. Our analyses suggested that this was not the case, as excluding those who reported subthreshold or threshold mood disorders in the 12 months prior to baseline, or adjusting for baseline mental health-related quality of life, still showed that those with better lifestyles had a lower risk of mood disorder over follow-up. The robustness of the results was further evident from the similar effect sizes when only some health behaviours were included in the score. This suggests that no individual health behaviour or cluster of health behaviours was responsible for the associations. With that said, analyses of the effects of individual items did suggest that non-smoking was particularly protective. This reflects the complex inter-relationship between smoking and mood disorders, noting the ongoing controversy regarding whether this is a causal relationship (Chaiton et al. Reference Chaiton, Cohen, O'Loughlin and Rehm2009) or the result of confounding (Bjorngaard et al. Reference Bjorngaard, Gunnell, Elvestad, Davey Smith, Skorpen, Krokan, Vatten and Romundstad2013). The similarity in effect sizes with items removed provides evidence that it is the latent construct of a ‘healthy lifestyle’ that is important for mental health. Bearing in mind the observational nature of these data, our results suggest that a healthier lifestyle may protect against new-onset mood disorder. Importantly, the magnitude of the reduction in risk of mood disorder per healthy behaviour was similar to the effects of psychological interventions in a meta-analysis of trials for the primary prevention of mood disorders (Cuijpers et al. Reference Cuijpers, Van Straten, Warmerdam and Andersson2008).The findings are therefore relevant to those managing the physical or mental health of younger adults.
The potential mechanisms explaining why those with healthy lifestyles might be protected against mood disorder are governed by the contents of the score, which contains items known to protect against depression; for example, being healthy weight (De Wit et al. Reference De Wit, Luppino, Van Straten, Penninx, Zitman and Cuijpers2010), not smoking (Patton et al. Reference Patton, Carlin, Coffey, Wolfe, Hibbert and Bowes1998; Taylor et al. Reference Taylor, McNeill, Girling, Farley, Lindson-Hawley and Aveyard2014), dietary factors (Smith et al. Reference Smith, Sanderson, McNaughton, Gall, Dwyer and Venn2014; Jacka et al. Reference Jacka, Cherbuin, Anstey and Butterworth2015) and physical activity (McKercher et al. Reference McKercher, Sanderson, Schmidt, Otahal, Patton, Dwyer and Venn2014). The mechanisms common across the healthy behaviours are the links with lower levels of inflammation, better immune system functioning and lower oxidative stress (Lopez-Garcia et al. Reference Lopez-Garcia, Schulze, Fung, Meigs, Rifai, Manson and Hu2004; Paul et al. Reference Paul, Thrift and Donnan2004; Raison et al. Reference Raison, Capuron and Miller2006; Berk et al. Reference Berk, Kapczinski, Andreazza, Dean, Giorlando, Maes, Yucel, Gama, Dodd, Dean, Magalhaes, Amminger, McGorry and Malhi2011). These mechanisms, in turn, may affect pathways implicated in the development and progression of mood disorders such as the monoaminergic system (Chaouloff, Reference Chaouloff1997; Dani & De Biasi, Reference Dani and De Biasi2001; Berk et al. Reference Berk, Kapczinski, Andreazza, Dean, Giorlando, Maes, Yucel, Gama, Dodd, Dean, Magalhaes, Amminger, McGorry and Malhi2011). The development of mood disorders and uptake and maintenance of health behaviours are complex and influenced by a range of genetic (Nabeshima & Kim, Reference Nabeshima and Kim2013; De Geus et al. Reference De Geus, Bartels, Kaprio, Lightfoot and Thomis2014; Ware & Munafò, Reference Ware and Munafò2015) and environmental factors (Baler & Volkow, Reference Baler and Volkow2011; Nabeshima & Kim, Reference Nabeshima and Kim2013) that were not measured in this study. It is therefore possible that the results seen here are the result of residual confounding by shared genetic or environmental factors. This might mean that the associations seen here are not causal. However, with confirmation of our findings in other longitudinal studies or randomized controlled trials it is possible that we could consider including the potential mental health benefits of adopting health behaviours that prevent cardiovascular disease in health promotion messages.
We acknowledge the behaviour change can be difficult but note that in this cohort, albeit relatively young and socio-economically advantaged, about 60% of people either maintained or gained a high Healthy Lifestyle Score over 5 years. There is also some evidence that interventions to change multiple behaviours in younger adults can be successful (An et al. Reference An, Demers, Kirch, Considine-Dunn, Nair, Dasgupta, Narisetty, Resnicow and Ahluwalia2013, Valve et al. Reference Valve, Lehtinen-Jacks, Eriksson, Lehtinen, Lindfors, Saha, Rimpela and Angle2013) which is somewhat contrary to studies that include older people (Butler et al. Reference Butler, Simpson, Hood, Cohen, Pickles, Spanou, McCambridge, Moore, Randell, Alam, Kinnersley, Edwards, Smith and Rollnick2013). Ideally, people would have healthy lifestyles from childhood and throughout adulthood with there being some evidence that multifaceted programmes (i.e. child and family) can have very long-term influences on lifestyle (Pahkala et al. Reference Pahkala, Hietalampi, Laitinen, Viikari, Ronnemaa, Niinikoski, Lagstrom, Talvia, Jula, Heinonen, Juonala, Simell and Raitakari2013).
There was also evidence that a history of mood disorder before baseline was associated with unfavourable changes in lifestyle over 5 years. This novel finding in a cohort of generally healthy young adults supports the literature on the bi-directional associations between mental health and single risk factors. It also reinforces recent analyses demonstrating that health behaviours accounted for much of the association between depression and cardiovascular disease albeit in older people (Ye et al. Reference Ye, Muntner, Shimbo, Judd, Richman, Davidson and Safford2013). There are many potential mechanisms linking a history of mood disorder with worsening lifestyle, including self-medication with alcohol (Dixit & Crum, Reference Dixit and Crum2000) and cigarettes (Patton et al. Reference Patton, Carlin, Coffey, Wolfe, Hibbert and Bowes1998) in an attempt to manage symptoms. The symptoms associated with mood disorder such as psychomotor retardation or alterations in appetite could also result in worse scores on items for physical activity and diet (Wenzel et al. Reference Wenzel, Steer and Beck2005; Simon et al. Reference Simon, Ludman, Linde, Operskalski, Ichikawa, Rohde, Finch and Jeffery2008). This finding highlights the need for more recognition of the close link between lifestyle and mental health and the need for a ‘whole of person’ approach to these conditions (Baird & Clarke, Reference Baird and Clarke2011). As noted by others (Ye et al. Reference Ye, Muntner, Shimbo, Judd, Richman, Davidson and Safford2013), addressing the lifestyles of people with mood disorders is imperative for reducing their risk of physical illness and may, indeed, ameliorate their symptoms of mood disorder if our findings regarding lifestyle predicting depression are confirmed in intervention studies.
This study has limitations that should be acknowledged. There was substantial loss to follow-up. We found that those included were of higher socio-economic status and had healthier lifestyles than those not included and compared with the general Australian population of a similar age. We addressed this issue by using inverse probability weights and showed this loss to follow-up appeared to only have a minor impact on our findings. Further, the validity of associative analyses is not reliant on a generalizable sample; rather, what is important is that the cohort has well-characterized participants; adequate sample size; and heterogeneity of determinants, modifiers and confounders, as is the case for our cohort (Miettinen, Reference Miettinen1985). Nonetheless, if the methods we used have not adequately accounted for the attrition in the study then it is possible that our findings are only applicable to relatively healthy, higher socio-economic-status individuals. Further, the study was based on younger individuals, which may be a strength in terms of less confounding by chronic conditions, but this may mean results are not generalizable to older people. Assessments of mood disorders were retrospective using the lifetime version of the CIDI at follow-up. Repeat assessments over shorter time periods may reduce misclassification but they would place a significant burden on participants and be costly, meaning they were not feasible in our study. The validity of the lifetime assessment of mood disorders in our study is potentially aided by the fact that our participants were in the peak ages for prevalence of mood disorder (Australian Bureau of Statistics, 2007) with the time since the most recent episode being 4.2 years (s.d. = 4.5 years). This suggests that the recall period for most people was short. Further, as shown in the online Supplementary material, the lifetime prevalence of mood disorder in our cohort was quite similar to the general population, so the risk of misclassification despite retrospective recall seems low. Regarding the Healthy Lifestyle Score itself, it gives equal weight to each item therefore not reflecting each item's contribution to the burden of disease. We countered this by examining the role of individual items in our analyses. The item for BMI could be considered an outcome of other items in the score but we included it because of the important role it plays in the burden of disease (GBD 2013 Risk Factor Collaborators et al. Reference Forouzanfar, Alexander, Anderson, Bachman, Biryukov, Brauer, Burnett, Casey, Coates, Cohen, Delwiche, Estep, Frostad, Astha, Kyu, Moradi-Lakeh, Ng, Slepak, Thomas, Wagner, Aasvang, Abbafati, Abbasoglu Ozgoren, Abd-Allah, Abera, Aboyans, Abraham, Abraham, Abubakar, Abu-Rmeileh, Aburto, Achoki, Adelekan, Adofo, Adou, Adsuar, Afshin, Agardh, Al Khabouri, Al Lami, Alam, Alasfoor, Albittar, Alegretti, Aleman, Alemu, Alfonso-Cristancho, Alhabib, Ali, Ali, Alla, Allebeck, Allen, Alsharif, Alvarez, Alvis-Guzman, Amankwaa, Amare, Ameh, Ameli, Amini, Ammar, Anderson, Antonio, Anwari, Argeseanu Cunningham, Arnlöv, Arsenijevic, Artaman, Asghar, Assadi, Atkins, Atkinson, Avila, Awuah, Badawi, Bahit, Bakfalouni, Balakrishnan, Balalla, Balu, Banerjee, Barber, Barker-Collo, Barquera, Barregard, Barrero, Barrientos-Gutierrez, Basto-Abreu, Basu, Basu, Basulaiman, Batis Ruvalcaba, Beardsley, Bedi, Bekele, Bell, Benjet, Bennett, Benzian, Bernabé, Beyene, Bhala, Bhalla, Bhutta, Bikbov, Bin Abdulhak, Blore, Blyth, Bohensky, Bora Başara, Borges, Bornstein, Bose, Boufous, Bourne, Brainin, Brazinova, Breitborde, Brenner, Briggs, Broday, Brooks, Bruce, Brugha, Brunekreef, Buchbinder, Bui, Bukhman, Bulloch, Burch, Burney, Campos-Nonato, Campuzano, Cantoral, Caravanos, Cárdenas, Cardis, Carpenter, Caso, Castañeda-Orjuela, Castro, Catalá-López, Cavalleri, Çavlin, Chadha, Chang, Charlson, Chen, Chen, Chen, Chiang, Chimed-Ochir, Chowdhury, Christophi, Chuang, Chugh, Cirillo, Claßen, Colistro, Colomar, Colquhoun, Contreras, Cooper, Cooperrider, Cooper, Coresh, Courville, Criqui, Cuevas-Nasu, Damsere-Derry, Danawi, Dandona, Dandona, Dargan, Davis, Davitoiu, Dayama, de Castro, De la Cruz-Góngora, De Leo, de Lima, Degenhardt, del Pozo-Cruz, Dellavalle, Deribe, Derrett, Des Jarlais, Dessalegn, deVeber, Devries, Dharmaratne, Dherani, Dicker, Ding, Dokova, Dorsey, Driscoll, Duan, Durrani, Ebel, Ellenbogen, Elshrek, Endres, Ermakov, Erskine, Eshrati, Esteghamati, Fahimi, Faraon, Farzadfar, Fay, Feigin, Feigl, Fereshtehnejad, Ferrari, Ferri, Flaxman, Fleming, Foigt, Foreman, Paleo, Franklin, Gabbe, Gaffikin, Gakidou, Gamkrelidze, Gankpé, Gansevoort, García-Guerra, Gasana, Geleijnse, Gessner, Gething, Gibney, Gillum, Ginawi, Giroud, Giussani, Goenka, Goginashvili, Gomez Dantes, Gona, Gonzalez de Cosio, González-Castell, Gotay, Goto, Gouda, Guerrant, Gugnani, Guillemin, Gunnell, Gupta, Gupta, Gutiérrez, Hafezi-Nejad, Hagan, Hagstromer, Halasa, Hamadeh, Hammami, Hankey, Hao, Harb, Haregu, Haro, Havmoeller, Hay, Hedayati, Heredia-Pi, Hernandez, Heuton, Heydarpour, Hijar, Hoek, Hoffman, Hornberger, Hosgood, Hoy, Hsairi, Hu, Hu, Huang, Huang, Hubbell, Huiart, Husseini, Iannarone, Iburg, Idrisov, Ikeda, Innos, Inoue, Islami, Ismayilova, Jacobsen, Jansen, Jarvis, Jassal, Jauregui, Jayaraman, Jeemon, Jensen, Jha, Jiang, Jiang, Jiang, Jonas, Juel, Kan, Kany Roseline, Karam, Karch, Karema, Karthikeyan, Kaul, Kawakami, Kazi, Kemp, Kengne, Keren, Khader, Khalifa, Khan, Khang, Khatibzadeh, Khonelidze, Kieling, Kim, Kim, Kim, Kimokoti, Kinfu, Kinge, Kissela, Kivipelto, Knibbs, Knudsen, Kokubo, Kose, Kosen, Kraemer, Kravchenko, Krishnaswami, Kromhout, Ku, Kuate Defo, Kucuk Bicer, Kuipers, Kulkarni, Kulkarni, Kumar, Kwan, Lai, Lakshmana Balaji, Lalloo, Lallukka, Lam, Lan, Lansingh, Larson, Larsson, Laryea, Lavados, Lawrynowicz, Leasher, Lee, Leigh, Leung, Levi, Li, Li, Liang, Liang, Lim, Lindsay, Lipshultz, Liu, Liu, Lloyd, Logroscino, London, Lopez, Lortet-Tieulent, Lotufo, Lozano, Lunevicius, Ma, Ma, Machado, MacIntyre, Magis-Rodriguez, Mahdi, Majdan, Malekzadeh, Mangalam, Mapoma, Marape, Marcenes, Margolis, Margono, Marks, Martin, Marzan, Mashal, Masiye, Mason-Jones, Matsushita, Matzopoulos, Mayosi, Mazorodze, McKay, McKee, McLain, Meaney, Medina, Mehndiratta, Mejia-Rodriguez, Mekonnen, Melaku, Meltzer, Memish, Mendoza, Mensah, Meretoja, Mhimbira, Micha, Miller, Mills, Misganaw, Mishra, Mohamed Ibrahim, Mohammad, Mokdad, Mola, Monasta, Montañez Hernandez, Montico, Moore, Morawska, Mori, Moschandreas, Moturi, Mozaffarian, Mueller, Mukaigawara, Mullany, Murthy, Naghavi, Nahas, Naheed, Naidoo, Naldi, Nand, Nangia, Narayan, Nash, Neal, Nejjari, Neupane, Newton, Ngalesoni, Ngirabega Jde, Nguyen, Nguyen, Nieuwenhuijsen, Nisar, Nogueira, Nolla, Nolte, Norheim, Norman, Norrving, Nyakarahuka, Oh, Ohkubo, Olusanya, Omer, Opio, Orozco, Pagcatipunan, Pain, Pandian, Panelo, Papachristou, Park, Parry, Paternina Caicedo, Patten, Paul, Pavlin, Pearce, Pedraza, Pedroza, Pejin Stokic, Pekericli, Pereira, Perez-Padilla, Perez-Ruiz, Perico, Perry, Pervaiz, Pesudovs, Peterson, Petzold, Phillips, Phua, Plass, Poenaru, Polanczyk, Polinder, Pond, Pope, Pope, Popova, Pourmalek, Powles, Prabhakaran, Prasad, Qato, Quezada, Quistberg, Racapé, Rafay, Rahimi, Rahimi-Movaghar, Rahman, Raju, Rakovac, Rana, Rao, Razavi, Reddy, Refaat, Rehm, Remuzzi, Ribeiro, Riccio, Richardson, Riederer, Robinson, Roca, Rodriguez, Rojas-Rueda, Romieu, Ronfani, Room, Roy, Ruhago, Rushton, Sabin, Sacco, Saha, Sahathevan, Sahraian, Salomon, Salvo, Sampson, Sanabria, Sanchez, Sánchez-Pimienta, Sanchez-Riera, Sandar, Santos, Sapkota, Satpathy, Saunders, Sawhney, Saylan, Scarborough, Schmidt, Schneider, Schöttker, Schwebel, Scott, Seedat, Sepanlou, Serdar, Servan-Mori, Shaddick, Shahraz, Levy, Shangguan, She, Sheikhbahaei, Shibuya, Shin, Shinohara, Shiri, Shishani, Shiue, Sigfusdottir, Silberberg, Simard, Sindi, Singh, Singh, Singh, Skirbekk, Sliwa, Soljak, Soneji, Søreide, Soshnikov, Sposato, Sreeramareddy, Stapelberg, Stathopoulou, Steckling, Stein, Stein, Stephens, Stöckl, Straif, Stroumpoulis, Sturua, Sunguya, Swaminathan, Swaroop, Sykes, Tabb, Takahashi, Talongwa, Tandon, Tanne, Tanner, Tavakkoli, Te Ao, Teixeira, Téllez Rojo, Terkawi, Texcalac-Sangrador, Thackway, Thomson, Thorne-Lyman, Thrift, Thurston, Tillmann, Tobollik, Tonelli, Topouzis, Towbin, Toyoshima, Traebert, Tran, Trasande, Trillini, Trujillo, Dimbuene, Tsilimbaris, Tuzcu, Uchendu, Ukwaja, Uzun, van de Vijver, Van Dingenen, van Gool, van Os, Varakin, Vasankari, Vasconcelos, Vavilala, Veerman, Velasquez-Melendez, Venketasubramanian, Vijayakumar, Villalpando, Violante, Vlassov, Vollset, Wagner, Waller, Wallin, Wan, Wang, Wang, Wang, Wang, Wang, Warouw, Watts, Weichenthal, Weiderpass, Weintraub, Werdecker, Wessells, Westerman, Whiteford, Wilkinson, Williams, Williams, Woldeyohannes, Wolfe, Wong, Woolf, Wright, Wurtz, Xu, Yan, Yang, Yano, Ye, Yenesew, Yentür, Yip, Yonemoto, Yoon, Younis, Younoussi, Yu, Zaki, Zhao, Zheng, Zhou, Zhu, Zhu, Zou, Zunt, Lopez, Vos and Murray2015) including mood disorders (De Wit et al. Reference De Wit, Luppino, Van Straten, Penninx, Zitman and Cuijpers2010).
The study also has several strengths. Lifestyle risk factors were measured with standardized questionnaires resulting in an overall score that we (Gall et al. Reference Gall, Jamrozik, Blizzard, Dwyer and Venn2009, Reference Gall, Abbott-Chapman, Patton, Dwyer and Venn2010) and others (Spencer et al. Reference Spencer, Jamrozik, Norman and Lawrence-Brown2005) have shown predicts cardiometabolic risk factors and mortality, demonstrating its validity. Similarly, mood disorder was measured with the CIDI, which is considered to be the ‘gold standard’ for mental disorder diagnosis in epidemiological studies. We conducted sensitivity analyses to confirm the influence of loss to follow-up and to identify the potential influence of individual lifestyle risk factors. We also considered a large range of potential confounders including major determinants of mood disorders such as major life events, personality, social support, and marital and parental status. The Healthy Lifestyle Score has strengths as it does not require invasive or lengthy testing; aligns with recommendations from peak health bodies; and that the items relate directly to behaviours, rather than biomarkers, meaning that people can immediately understand the changes required to improve their health.
Conclusions
Bi-directional associations between the number of healthy behaviours and mood disorders were found in our cohort of young adults followed for 5 years. This highlights the need for holistic management of young adults in terms of their mental and physical health including health behaviours. Our results suggest that achieving and maintaining a healthy lifestyle will not only reduce cardiovascular disease but also promote good mental health.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S0033291716000738
Acknowledgements
We gratefully acknowledge the CDAH study project manager Ms Marita Dalton. We thank the study sponsors for their assistance including Target and Asics that provided gifts for study participants, and Sanitarium, that provided food items consumed during study clinics. The sponsors had no role in the study design, conduct, analysis or reporting of results.
This study was supported by the National Health and Medical Research Council (project grant 211316, senior research fellowship to A.V.; ECF Fellowship 1072516 to K.J.S.), the National Heart Foundation (project grant GOOH 0578, fellowships PH 11H 6047 and FLF 100446 to S.L.G.) and Veolia Environmental Services. The supporters had no role in the study design, conduct, analysis or reporting of results.
S.L.G. designed, conducted and interpreted the analyses, drafted the manuscript and contributed to the acquisition of data. K.S., K.J.S., G.P., T.D. and A.V. interpreted analyses, contributed to the acquisition of data, provided intellectual content and contributed to the drafting of the manuscript All authors approved the final version of the manuscript.
Declaration of Interest
None.







