Background
Cannabis is the most widely used illicit substance in the world, and both use and misuse of the substance are increasing in many countries. In Europe, the lifetime prevalence of cannabis use is about five times higher than for other illicit substances (European Monitoring Centre for Drugs and Drug Addiction, 2019). It is estimated that approximately 96 million adult Europeans, i.e. more than a quarter of the European population, have used illicit substances at some point in their lives, with cannabis accounting for some 91.2 million lifetime users (European Monitoring Centre for Drugs and Drug Addiction, 2019). From 2005 to 2009, there was an increase in people in Denmark estimated to suffer from illicit substance use disorders from around 20 000 people to around 33 000 people. For cannabis use disorders, the increase was from around 7900 people to around 10 900 people (Sundhedsstyrelsen, n.d.).
Several studies have linked cannabis to an increased risk of psychoses such as schizophrenia (Marconi, Di Forti, Lewis, Murray, & Vassos, Reference Marconi, Di Forti, Lewis, Murray and Vassos2016; Moore et al., Reference Moore, Zammit, Lingford-Hughes, Barnes, Jones, Burke and Lewis2007; Nielsen, Toftdahl, Nordentoft, & Hjorthøj, Reference Nielsen, Toftdahl, Nordentoft and Hjorthøj2017). While some studies have indicated that this may be in part due to shared genetic architecture between cannabis use and psychosis, other studies have indicated that this may not be the case (Carey et al., Reference Carey, Agrawal, Bucholz, Hartz, Lynskey, Nelson and Bogdan2016; Hiemstra et al., Reference Hiemstra, Nelemans, Branje, van Eijk, Hottenga, Vinkers and Boks2018; Hjorthøj et al., Reference Hjorthøj, Uddin, Wimberley, Dalsgaard, Hougaard, Børglum and Nordentoft2019; Power et al., Reference Power, Verweij, Zuhair, Grant, Henders, Heath and Martin2014; Verweij et al., Reference Verweij, Abdellaoui, Nivard, Sainz Cort, Ligthart, Draisma and Vink2017). The causal hypothesis is further strengthened by the psychosis-inducing properties of cannabis, which has been shown to transiently induce psychotic-like symptoms in healthy individuals (Morrison et al., Reference Morrison, Zois, McKeown, Lee, Holt, Powell and Murray2009). Furthermore, a psychiatric diagnosis known as cannabis-induced psychosis is an entity both in ICD-10 and in DSM-5. There is relatively little research into the area of cannabis-induced psychosis, but previous research has shown that cannabis-induced psychosis is a strong risk factor for later development of schizophrenia (Arendt, Rosenberg, Foldager, Perto, & Munk-Jørgensen, Reference Arendt, Rosenberg, Foldager, Perto and Munk-Jørgensen2005; Kendler, Ohlsson, Sundquist, & Sundquist, Reference Kendler, Ohlsson, Sundquist and Sundquist2019; Starzer, Nordentoft, & Hjorthøj, Reference Starzer, Nordentoft and Hjorthøj2018).
Little is known about the development over time of cannabis-induced psychosis. However, given that countries like Denmark have seen an increase in both use and misuse of cannabis, an increase in cannabis-induced psychoses would be expected. Similarly, it would be expected that there would then also be an increase in dually diagnosed schizophrenia and cannabis use disorders. Finally, the same development would not be expected for other substances since the use of these does not appear to be increasing in Denmark. Establishing whether the observed increase in use of cannabis coincides with an increase in incidence of cannabis-induced psychosis is important in light of the movements, both in Denmark and internationally, to decriminalize or legalize cannabis for recreational purposes.
In the present study, we aimed to investigate:
• The development in the incidence of cannabis-induced psychosis over time in Denmark compared to other substance-induced psychoses
• The development in the incidence of cannabis-induced psychosis over time in Denmark compared to the development in incident dually diagnosed schizophrenia and harmful use or dependence of cannabis
Methods
Data for the present study is based on unselected, nationwide Danish registers. The linkage of these registers is made possible by the use of the unique personal identification number introduced with the Civil Registration System and given to all people born in Denmark or obtaining permanent residence in Denmark since 1968 (Pedersen, Gøtzsche, Møller, & Mortensen, Reference Pedersen, Gøtzsche, Møller and Mortensen2006).
Definitions and sources of data
Data for the present study are obtained from the Psychiatric Central Research Register (Mors, Perto, & Mortensen, Reference Mors, Perto and Mortensen2011). This register contains information on all inpatient admissions to psychiatric hospitals in Denmark since 1969. Since 1994, it has also included information on outpatient and emergency psychiatric facilities. The register contains information on, among other items, both date of admission and discharge, and a completely list of both primary and secondary diagnoses associated with each contact. From 1994, diagnoses have been made using ICD-10, and prior to that, ICD-8. ICD-9 was never implemented in Denmark.
Since ICD-8 does not contain substance-specific diagnostic codes for substance-induced psychosis, we exclusively used information from 1994 onwards. We included all living in Denmark in at least part of the period from 1994 to 2016. Incident substance induced psychosis was defined as the first time one of the following diagnostic codes were registered, all detailing psychoses induced by various substances: F10.5 (alcohol), F11.5 (opioids), F12.5 (cannabis), F13.5 (sedatives), F14.5 (cocaine), F15.5 (amphetamines), F16.5 (hallucinogens), and F18.5 and F19.5 combined to form a category of mixed or other substances.
Incident dual diagnosis was defined as getting an incident diagnosis of schizophrenia (295 in ICD-8 or F20 in ICD-10) and being given a diagnosis of harmful use or dependence of cannabis (304.5 in ICD-8 or F12.1 or F12.2 in ICD-10) at the same date as the incident schizophrenia diagnosis. A previous diagnosis of harmful use or dependence of cannabis did not disqualify people from being considered having an incident dual diagnosis.
Statistics
We estimated the yearly incidence of both substance induced psychoses and dual diagnoses. As the register for psychiatric data was only updated until April 2017, we present only data until 2016. The incidence was presented as both absolute incidence (i.e. number of cases per year) and as incidence rate per 100 000 person years. The population size used for the estimation of the incidence rate was obtained from Statistics Denmark as the average of the population size (ages 15+) on 1st January of the year in question and 1st January of the following year. For cannabis-induced psychosis, we conducted further post-hoc analyses in which the annual incidence rate ratio (IRR) was estimated compared to 2006 (at which point the incidence rate was lowest) as the reference year. Spearman's rho was used to quantify the correlation between duration of the first admission for cannabis-induced psychosis and year of such diagnosis. Analyses were conducted using STATA/MP version 15.1.
Ethical considerations
According to Danish law, register-based studies do not require institutional review board approval. Analyses were conducted using encrypted personal identification numbers, using an encryption key which was not available to the research team.
Results
From 1994 to 2016 (both inclusive), a total of 13 716 incident cases of substance-induced psychoses were identified. Of these, 4402 were incident cases of cannabis-induced psychosis. In the same period, 2004 cases of incident dually diagnosed schizophrenia with cannabis use disorder were identified. Table 1 shows the characteristics of the study population.
Table 1. Characteristics of the study populations

s.d., standard deviation; IQR, interquartile range.
The same person may be present in more than one population.
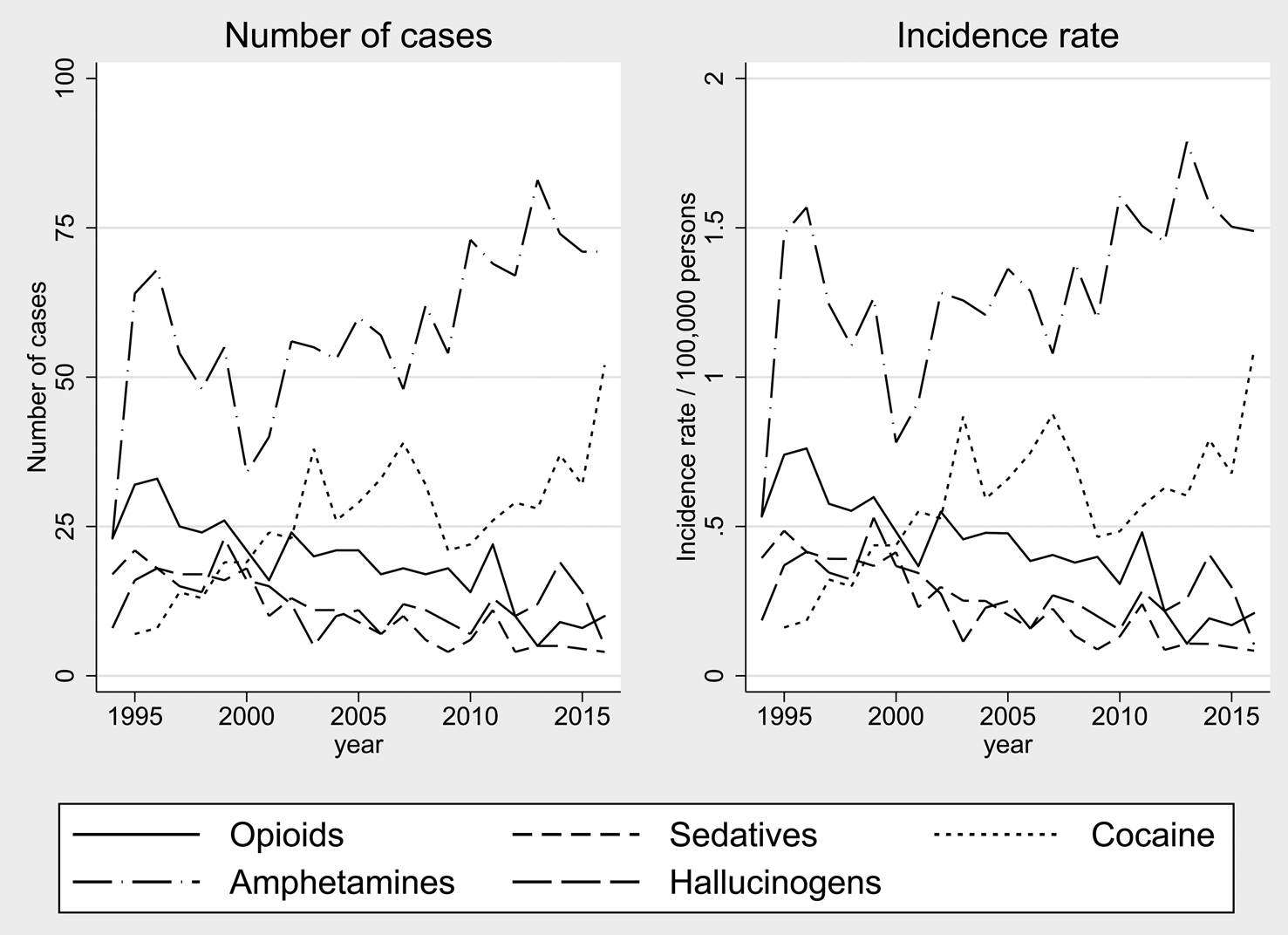
Figure 1 shows the annual incidence (number of cases) and the incidence rate of both any substance-induced psychosis as well as the most frequently occurring subtypes of substance-induced psychosis. Figure 2 shows the same, but for the five most infrequently occurring subtypes of substance-induced psychosis. While the incidence of any substance-induced psychosis remains relatively stable, it is evident that the incidence of cannabis-induced psychosis has remained relatively stable until approximately 2006, at which point the incidence appears to increase from 2.8 per 100 000 person years to 6.9 per 100 000 person years in 2014 and 6.1 per 100 000 person years in 2016. Figure 3 shows the annual development in incidence rates of cannabis-induced psychosis as IRRs with the year 2006 as the reference category. With a few single-year exceptions, the incidence of the years before 2006 is not statistically significant from 2006, whereas it increases from 2006, being statistically significantly higher than in 2006 from the year 2008 and onwards. The peak incidence of cannabis-induced psychosis was observed in 2014, for a total of 322 cases (or 6.9 per 10 000 person years), corresponding to an IRR of 2.44 (95% confidence interval 1.98–2.99) compared to 2006. In order to test if the increased incidence of cannabis-induced psychosis could be attributed to a lower threshold for seeking treatment, we set up a post-hoc analysis to check whether the duration of admission for cannabis-induced psychosis correlated with year of first diagnosis. There was no such correlation (ρ = 0.02 regardless of whether the full period was examined or just the period from 2006 to 2016).

Fig. 1. Incidence of cannabis-induced psychosis and the most frequent other substance-induced psychoses in Denmark from 1994 to 2016.

Fig. 2. Incidence of infrequent types of substance-induced psychoses in Denmark from 1994 to 2016.

Fig. 3. IRR of cannabis-induced psychosis per year in Denmark compared to 2006.
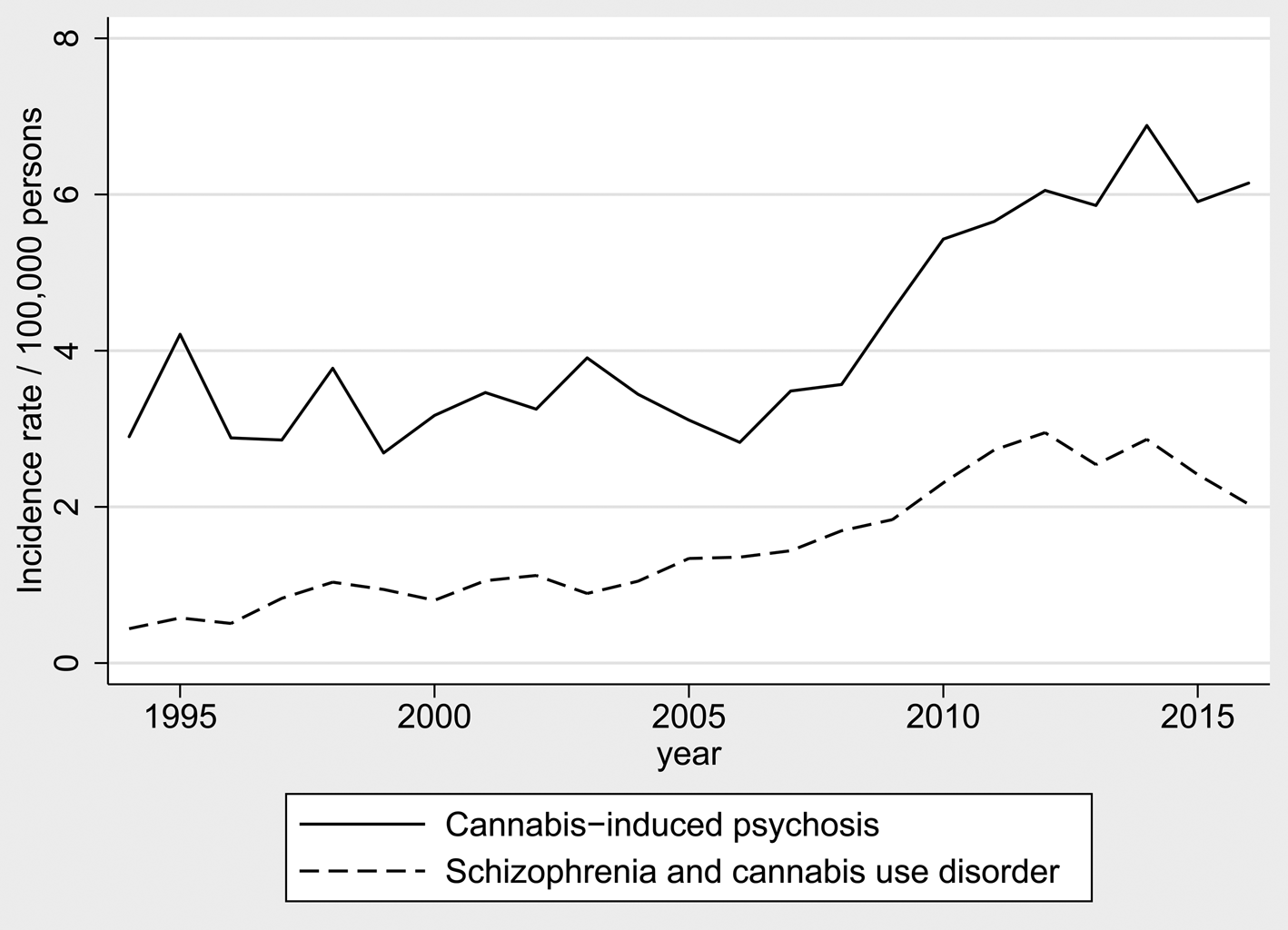
Figure 4 shows the annual incidence rate of cannabis-induced psychosis alongside incident dually diagnosed schizophrenia and cannabis use disorder. The incidence of the two disorders is shown to run roughly in parallel.
Fig. 4. Incidence of cannabis-induced psychosis and dually diagnosed schizophrenia and cannabis use disorder in Denmark from 1994 to 2016.
Discussion
While the overall incidence of substance-induced psychosis has remained relatively stable from 1994 to 2016, the yearly incidence of cannabis-induced psychosis has increased since 2006 when it was at its lowest. The incidence of alcohol-induced psychosis has been declining steadily throughout the period. The development of dually diagnosed incident schizophrenia and cannabis use disorder was roughly parallel to the development of cannabis-induced psychosis.
The observed increase in the incidence of cannabis-induced psychosis may have several explanations. One possibility is that the use of cannabis may have increased over time. Danish data indicates that this is the case (Sundhedsstyrelsen, n.d.). Another possibility is that the strength of cannabis, as measured by the concentration of THC, may have increased. Several studies have indicated that the use of cannabis containing high concentrations of THC may put people at particular risk of schizophrenia-like psychoses (Di Forti et al., Reference Di Forti, Marconi, Carra, Fraietta, Trotta, Bonomo and Murray2015, Reference Di Forti, Quattrone, Freeman, Tripoli, Gayer-Anderson and Quigley2019; Gage, Hickman, & Zammit, Reference Gage, Hickman and Zammit2016). The same may be true for the ratio of THC:CBD (Gage et al., Reference Gage, Hickman and Zammit2016). We are not aware of any studies linking the concentration of THC or THC:CBD ratio specifically to the risk of cannabis-induced psychosis, but it is likely that such a dose-response relationship would also be present here. Cannabis products in Denmark are among those, on a European level, with the highest concentrations of THC, having increased from around 13% THC in 2006 to nearly 30% THC in 2016 (Freeman et al., Reference Freeman, Groshkova, Cunningham, Sedefov, Griffiths and Lynskey2019).
A further explanation might be found in the use of other substances. At least one study has indicated that the risk of cannabis-induced psychosis increases when the person also uses other substances (Caton, Samet, & Hasin, Reference Caton, Samet and Hasin2000). However, this is not likely to explain our findings. First, we do not see a corresponding increase in other types of substance-induced psychosis, which would then also be expected. And second, such an increase in the use of other substances has not been reported in Denmark (Sundhedsstyrelsen, n.d.).
It may also be the case that the increase in incidence rather reflects a change in diagnostic practice. It can be difficult to distinguish cannabis-induced psychosis from incident schizophrenia with comorbid cannabis use disorder (Sara, Burgess, Malhi, Whiteford, & Hall, Reference Sara, Burgess, Malhi, Whiteford and Hall2014). The increasing incidence of cannabis-induced psychosis could thus be caused by a changed in diagnostic practice where patients that would previously have been dually diagnosed with schizophrenia and cannabis use disorder were increasingly being diagnosed with cannabis-induced psychosis instead. If this were the case, the increase in cannabis-induced psychosis should have been matched with a corresponding decrease in dually diagnosed schizophrenia and cannabis use disorder. We did not observe this in our data, and this explanation consequently seems unlikely. Indeed, the development of dually diagnosed schizophrenia and cannabis use disorder was almost perfectly parallel to that of cannabis-induced psychosis. It should be noted, however, that underreporting of substance use disorder is well described in register-based data. While it is not inconceivable that such underreporting may have decreased over time, it is highly unlikely that the observed increase in dual diagnosis actually reflects a decrease in underlying cannabis use disorder (Hansen et al., Reference Hansen, Munk-Jorgensen, Guldbaek, Solgard, Lauszus, Albrechtsen and Bertelsen2000). This lends further support to the notion that the increase in incidence is true and is probably caused by the increasing use of cannabis or increasing concentrations of THC.
Finally, data from the United States indicate that both adults and adolescents today view cannabis as less risky than in the beginning of the millennium (Carliner, Brown, Sarvet, & Hasin, Reference Carliner, Brown, Sarvet and Hasin2017). While such data is not, to our knowledge, available for Denmark, it is likely that the same is true here. This may also indicate that the use of cannabis is perceived as less stigmatizing now than it has been previously. Consequently, it cannot be ruled out that people have become more willing to seek help for cannabis-related problems, which could at least in part explain some of the increased incidence we observed in the present study. A similar explanation would be that the threshold for being admitted for cannabis-induced psychosis had been lowered from the perspective of the psychiatric departments. However, there was no correlation between year of first diagnosis of cannabis-induced psychosis and duration of first admission for the disorder. If the threshold for seeking treatment had become lower over time, this should have led to an increase of lighter cases with shorter demands for treatment. Since we did not observe this correlation, we do not find it likely that our results are explained by a reduced threshold for seeking treatment.
Strengths and limitations
This study holds a number of important strengths. First, the use of the nationwide Danish registers ensures an unselected population, since individuals did not have to consent to form part of the study population. This means that all cases of substance-induced psychosis or dually diagnosed schizophrenia with cannabis use disorder, treated in the secondary healthcare sector in Denmark, were included. However, this also means that we could not include information on patients who were either treated in primary care or remained completely untreated for their psychotic disorder. This means that we underestimate the true incidence of particularly substance-induced psychosis. Furthermore, the use of register-based data limits the information available to use. For instance, we do not know how much cannabis (or other substances) an individual has used, the potency of the cannabis products, the age at which the use started, etc.
In conclusion, an increase in cannabis-induced psychosis has been observed since 2006, and this is likely due to an increase in the use and potency of cannabis. This is of concern, as we have previously shown that people with cannabis-induced psychosis have more than 40% risk of later developing schizophrenia (Starzer et al., Reference Starzer, Nordentoft and Hjorthøj2018). This information is important in the ongoing debate regarding decriminalization or legalization of cannabis.