Introduction
Anxiety disorders occur in between 6% and 12% of the general population (Alonso et al. 2004 a; Andlin-Sobocki & Wittchen, Reference Andlin-Sobocki and Wittchen2005). Help seeking may mean that prevalence is somewhat higher in general practice attendees than the general population (Ansseau et al. Reference Ansseau, Fischler, Dierick, Mignon and Leyman2005); however only about one-quarter of sufferers will contact a health service professional over any one year (Alonso et al. 2004 b). The high prevalence and relapsing nature of anxiety disorders means that they account for at least 35% of all disability and sick leave days due to mental disorders (Andlin-Sobocki & Wittchen, Reference Andlin-Sobocki and Wittchen2005). Even subclinical anxiety states may have major impacts on quality of life (Andlin-Sobocki & Wittchen, Reference Andlin-Sobocki and Wittchen2005; Das-Munshi et al. Reference Das-Munshi, Goldberg, Bebbington, Bhugra, Brugha, Dewey, Jenkins, Stewart and Prince2008). Although there appear to be high indirect costs from the substantial burden of illness, direct treatment costs tend to be relatively low due to low recognition and low rates of treatment (Andlin-Sobocki & Wittchen, Reference Andlin-Sobocki and Wittchen2005). There are established, effective treatments for anxiety disorders (Deacon & Abramowitz, Reference Deacon and Abramowitz2004; van Boeijen et al. Reference van Boeijen, van Oppen, van Balkom, Visser, Kempe, Blankenstein and van Dyck2005) but even when the disorders are recognized, treatment is often not provided adequately (Fernández et al. Reference Fernández, Haro, Martinez-Alonso, Demyttenaere, Brugha, de Autonell, de Girolamo, Bernert, Lépine and Alonso2007). Research into prevention is much more limited (Schmidt & Zvolensky, Reference Schmidt and Zvolensky2007). The key challenge in prevention is to develop a clear understanding of the nature of risk factors and vulnerability processes underlying the development of anxiety disorders (Schmidt & Zvolensky, Reference Schmidt and Zvolensky2007). We aimed to develop a risk algorithm (predictA) for first onset or recurrence of generalized anxiety and panic syndromes in European general practice attendees and test its predictive power in external populations in Europe and in Chile. We modelled our approach on our earlier work to develop a predictD algorithm for onset of Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) major depression (King et al. 2006, Reference King, Walker, Levy, Bottomley, Royston, Weich, Bellón-Saameño, Moreno, Svab, Rotar, Rifel, Maaroos, Aluoja, Kalda, Neeleman, Geerlings, Xavier, Carraca, Goncalves-Pereira, Vicente, Saldivia, Melipillan, Torres-Gonzalez and Nazareth2008).
Method
Study setting and design
The cohort to be described in this paper was originally recruited with the aim of developing a risk model (predictD) for the onset of major depression (King et al. Reference King, Weich, Torres-González, Svab, Maaroos, Neeleman, Xavier, Morris, Walker, Bellón-Saameño, Moreno-Küstner, Rotar, Rifel, Aluoja, Kalda, Geerlings, Carraça, de Almeida, Vicente, Saldivia, Rioseco and Nazareth2006). However, we also aimed to predict the onset of anxiety syndromes and how predictors of risk for anxiety might relate to those for the development of major depression. The study was approved by ethical committees and conducted in seven countries: (1) 25 general practices in the Medical Research Council's General Practice Research Framework (MRC GPRF), in the UK; (2) nine large primary care centres in Andalucía, Spain; (3) 74 general practices nationwide in Slovenia; (4) 23 general practices nationwide in Estonia; (5) seven large general practice centres near Utrecht, The Netherlands; (6) two large primary care centres in the Lisbon area of Portugal; and (7) 78 general practitioners in 10 health centres in Concepción and Talcahuano in the Eighth region of Chile. The practices covered urban and rural populations with substantial socio-economic variation.
In our original 12-month cohort for the predictD study, data on anxiety syndromes as possible risk factors for major depression were only collected at recruitment and the 6-month follow-up. However, when further funding became available for a 24-month follow-up of all participants in the UK, Spain, Portugal and Slovenia (hereafter referred to as Europe4 countries), we included a further evaluation of anxiety symptoms at this point in order to develop a predictA risk model for anxiety. To best use these data, we decided to construct the predictA risk model for anxiety over 6 and 24 months in the Europe4 countries and validate it over 6 months in three external populations, namely The Netherlands, Estonia and Chile.
Study participants
Consecutive attendees aged between 18 and 75 years in all seven countries were recruited, consented and interviewed between April 2003 and September 2004 and re-interviewed after 6 months. In the Europe4 countries all participants were once again re-interviewed at 24 months from April 2005 to November 2005. Exclusion criteria were an inability to understand one of the main languages involved, psychosis, dementia and incapacitating physical illness. Participants gave informed consent and undertook a research evaluation within 2 weeks.
Anxiety syndromes and measured risk factors
Our main outcome of interest was anxiety and/or panic syndrome over the preceding 6 months as defined by the Patient Health Questionnaire (PHQ; Spitzer et al. Reference Spitzer, Kroenke and Williams1999). These symptoms match exactly onto the DSM-IV criteria for generalized anxiety disorder and panic disorder but do not include other anxiety syndromes such as phobias and post-traumatic stress disorder. Where possible we used standardized measures of our chosen risk factors. Questions adapted from standardized questionnaires or developed for the study were evaluated for test–retest reliability in 285 general practice attendees recruited in all the European countries before the main study began (King et al. Reference King, Weich, Torres-González, Svab, Maaroos, Neeleman, Xavier, Morris, Walker, Bellón-Saameño, Moreno-Küstner, Rotar, Rifel, Aluoja, Kalda, Geerlings, Carraça, de Almeida, Vicente, Saldivia, Rioseco and Nazareth2006). Each instrument or question not available in the relevant languages was translated from English and back-translated by professional translators (King et al. Reference King, Weich, Torres-González, Svab, Maaroos, Neeleman, Xavier, Morris, Walker, Bellón-Saameño, Moreno-Küstner, Rotar, Rifel, Aluoja, Kalda, Geerlings, Carraça, de Almeida, Vicente, Saldivia, Rioseco and Nazareth2006). A total of 38 risk factors were assessed; each is numbered in square brackets and those assessed for test–retest reliability are in italics:
(a) Age[1], sex[2], occupation[3], educational level[4], marital status[5], employment status[6], ethnicity[7], owner occupier accommodation[8], living alone or with others[9], born in country of residence or abroad[10], satisfaction with living conditions[11] and long-standing physical illness[12].
(b) A DSM-IV diagnosis of major depression in the preceding 6 months was made using the Depression Section of the Composite International Diagnostic Interview (CIDI; Robins et al. Reference Robins, Wing, Wittchen, Helzer, Babor, Burke, Farmer, Jablenski, Pickens and Regier1988; World Health Organization, 1997)[13].
(c) Lifetime depression was based on affirmative answers to both of the first two questions of the CIDI depression section[14] (Arroll et al. Reference Arroll, Khin and Kerse2003).
(d) Stress in paid and unpaid work in the preceding 6 months using questions from the job content instrument (Karasek & Theorell, Reference Karasek and Theorell1990). Participants were categorized as feeling in control in paid[15] or unpaid work[16]; as experiencing difficulties without support in paid or unpaid work[17]; and experiencing distress without feeling respect for their paid or unpaid work[18].
(e) Financial strain using a question used in UK government social surveys[19] (Weich & Lewis, Reference Weich and Lewis1998).
(f) Self-rated physical[20] and mental health[21] was assessed by the Short Form 12 (Jenkinson et al. Reference Jenkinson, Layte, Jenkinson, Lawrence, Petersen, Paice and Stradling1997). The weights used to calculate scores are from version 1.
(g) Alcohol use in the preceding 6 months using the Alcohol Use Disorder Test (AUDIT)[22] (Barbor et al. Reference Barbor, de la Fuente, Saunders and Grant1989). We asked whether participants had ever had an alcohol problem or treatment for the same[23].
(h) Whether participants had ever used recreational drugs using adapted sections of the CIDI[24].
(i) Questions on the quality of sexual[25] and emotional relationships[26] with partners or spouses (Taylor et al. Reference Taylor, Rosen and Leiblum1994).
(j) Presence of serious physical, psychological or substance-misuse problems, or any serious disability, in people who were in close relationship to participants[27].
(k) Difficulties in getting on with people and maintaining close relationships[28] (Tyrer, Reference Tyrer, Peck and Shapiro1990).
(l) Childhood experiences of physical and/or emotional[29] and sexual abuse[30] (Fink et al. Reference Fink, Bernstein, Handelsman, Foote and Lovejoy1995).
(m) Holding religious and/or spiritual beliefs[31] (King et al. Reference King, Speck and Thomas1995).
(n) History of serious psychological problems[32] or suicide in first-degree relatives[33] (Qureshi et al. Reference Qureshi, Bethea, Modell, Brennan, Papageorgiou, Raeburn, Hapgood and Modell2005).
(o) Satisfaction with the neighbourhood[34] and perceived safety inside/outside of the home[35] using questions from the Health Surveys for England (Sproston & Primatesta, Reference Sproston and Primatesta2003).
(p) Major life events in the preceding 6 months[36], using the List of Threatening Life Experiences Questionnaire (Brugha et al. Reference Brugha, Bebbington, Tennant and Hurry1985).
(q) Experiences of discrimination[37] in the preceding 6 months on grounds of sex, age, ethnicity, appearance, disability or sexual orientation using questions from a European study (Janssen et al. Reference Janssen, Hanssen, Bak, Bijl, de Graaf, Vollebergh, McKenzie and van Os2003).
(r) Adequacy of social support[38] from family and friends (Blaxter, Reference Blaxter1990).
We emphasize that all participants were re-evaluated for anxiety and panic symptoms using the PHQ after 6 and 24 months in the Europe4 countries, whereas in The Netherlands, Estonia and Chile they were assessed again only after the 6-month follow-up.
Statistical analysis
All analyses and data imputation were performed using Stata release 10 (StataCorp. LP, USA).
Imputation
Multiple imputation was carried out for the dataset on which the model was built (Europe4) and for each of the external datasets (The Netherlands, Estonia and Chile). For each variable with missing data, imputation was conducted using other risk factors and outcome variables. In all four imputed datasets, the imputation model included 38 risk factors and the outcome measure at baseline, 6 and 24 months. In Europe4, the imputation model also included country. The imputation process was conducted 10 times to produce 10 imputed datasets. Parameter estimates were obtained by fitting models to each of the imputed datasets and then combining these estimates using Rubin's rules (Rubin, Reference Rubin1987).
Model selection
We employed standard methods for model building (Royston et al. Reference Royston, Moons, Altman and Vergouwe2009). Logistic models were fitted to each of the 10 imputed datasets only using participants without anxiety or panic syndromes at baseline. Robust standard errors were used to account for dependence between observations on the same individual at 6 and 24 months. There was negligible clustering within practices (intra-cluster correlation=0.003) and thus standard errors were not adjusted for practice-level clustering. The initial model consisted of country, time, 38 risk factors, and interactions between each of the risk factors and time. Stepwise regression (backwards elimination) at a significance level of p=0.01 was used to identify a parsimonious model with age, sex, country and time forced into the model. The backwards elimination consisted of two steps: (1) selection of interaction terms and (2) selection of main effects. In the first step, all main effects were forced into the model and backwards elimination was conducted on the interaction terms; this was done to avoid models in which interaction terms were present without their constituent main effects. In step (2) backward elimination was carried out on the main effects and interaction terms identified in (1). For the interaction terms identified as significant in (1), the risk factor was jointly tested with the interaction term. Continuous variables were modelled using fractional polynomials of order 1.
Shrinkage
Parameter estimates were ‘shrunk’ using a method proposed by Copas (Reference Copas1983). According to this method, model coefficients are multiplied by a shrinkage factor to provide more accurate predictions when the risk algorithm is applied in new settings. The degree of shrinkage is related to the number of model parameters. We used the number of parameters in the original model (country, time, 38 risk factors, and interactions between time and risk factors), to compensate for over-fitting as a result of the model selection procedure.
Validation
C-indices and Hedges' g were computed for Europe4 and the three external countries; both are measures of the ability of the model to predict anxiety. For a discordant pair of individuals one anxious, the other not, the C-index is the probability that the anxious individual has the higher risk score. Hedges' g measures effect size: the difference between average logit transformed risk among individuals who became anxious compared with those who did not, standardized by an estimate of the pooled standard deviation. Both measures were computed separately for 6- and 24-month outcome data and using combined outcome data. For the combined 6- and 24-month data confidence intervals (CIs) for Hedges' g were obtained using robust standard errors for the estimate of the average difference in logit transformed risk; we did this to account for dependence between the repeat measures at 6 and 24 months on the same individual.
Model stability
The model selection procedure was conducted on each imputed dataset separately rather than on the combined estimates, obtained using Rubin's rules, described above. The variables selected in each imputed dataset were compared to assess the stability of the model. The fraction of missing information was used to quantify the uncertainty in each parameter estimate attributable to missing data; it is computed by estimating the proportion of the total variability of an estimate that is due to variability between imputations (Rubin, Reference Rubin1987; Schafer, Reference Schafer1999).
Sensitivity/specificity
In practice, the risk of panic/anxiety can only be assessed for individuals with complete covariate data. Sensitivity and specificity were estimated for a range of predictA cut-offs for individuals with complete covariate data using the imputed outcome data.
Results
A total of 10 045 people took part in the seven countries. Response to recruitment was high in Portugal (76%), Estonia (80%), Slovenia (80%) and Chile (97%) but lower in the UK (44%) and The Netherlands (45%). Ethical considerations prevented the collection of data on non-responders at baseline. The response to follow-up was 86.4% at 6 months and 66.9% at 24 months in the Europe4 countries and 92.6% at 6 months in Estonia, The Netherlands and Chile.
Numbers in the analysis
The model was built using 4905 individuals in Europe4 (UK, Spain, Slovenia and Portugal). They provide data on outcome (PHQ-defined anxiety and/or panic syndrome) at baseline, 6 and 24 months. Validation was carried out using 6-month outcome data from Estonia (n=1094), The Netherlands (n=1221) and Chile (n=2825). Demographic information on key variables for the whole sample is provided in Table 1. The amount of missing data in outcome and covariates is summarized in Table 2. For all countries there are few outcome data missing at baseline, but this increases significantly at 6 and 24 months. In Europe4 countries 14.7% are missing outcome at 6 months and this rises to 34.4% at 24 months. Taking the set of covariates as a whole, a large proportion of individuals were missing data in at least one covariate. In Europe4, 57.2% of individuals are missing data in at least one covariate. However, restricting the set of covariates to only those used in the final model, this proportion decreases to 5.2%.
Table 1. Demographic characteristics of primary care attendees without anxiety or panic syndrome at baseline

Data are given as number (percentage). n.a., Not applicable.
Table 2. Missing data in outcome and covariates in Europe4Footnote a countries, Estonia, The Netherlands and Chile

Data are given as number (percentage).
a Europe4 is the UK, Spain, Slovenia and Portugal combined.
Onset of anxiety and panic syndromes
We estimated that the incidence of either anxiety or panic syndrome or both at 6 months in Europe4 was 5.5% (95% CI 4.6–6.6). For the other countries, the incidence at 6 months was 3.1% (95% CI 2.2–4.3) in The Netherlands, 5.2% (95% CI 3.6–7.3) in Estonia and 8.6% (95% CI 7.2–10.2) in Chile. Occurrence of anxiety or panic syndrome at either 6 and/or 24 months in Europe4 was 10.7% (95% CI 9.0–12.6). We use the word occurrence here as the PHQ covered only the preceding 6 months, so strictly we cannot express the onset as an incidence rate at 24 months. It is also important to note that the figures given here vary very slightly from Table 1, as they are based on imputed data.
Development of the predictA algorithm in the Europe4 countries
Non-linear transformations of continuous variables did not significantly improve the model fit. In addition to time, age, sex and country, five variables were retained after the backwards elimination procedure (Table 3). In the final model, four variables concerned past events or patient characteristics (sex, age, lifetime depression screen, family history of psychological difficulties); three current status (Short Form 12 physical health subscale score, Short Form 12 mental health subscale score, and unsupported difficulties in paid and/or unpaid work); one concerned country, and one concerned time of follow-up. None of the interactions with time was included in the final model. Examination of the predictA model developed in each of the 10 imputed datasets revealed that it was relatively stable in terms of the variables selected. Besides country, age and sex, four variables (family history of psychological difficulties, Short Form 12 physical health subscale score, Short Form 12 mental health subscale score and lifetime depression screen) were selected in all 10, while unsupported difficulties in paid and/or unpaid work were selected in eight imputed datasets. A number of variables not contained in the final predictA model nevertheless appeared in some imputed datasets as follows: discrimination appeared in seven, religious belief in seven, major depression in five and lack of control in paid or unpaid work in five datasets. Other variables not in the final model appeared in only one imputed dataset. A moderate amount of uncertainty in parameter estimates could be attributed to missing data. The fraction of missing (Table 3) information for the parameter estimates ranged from 0.126 (first-degree relative with an emotional problem) to 0.412 (unsupported difficulties in paid and unpaid work).
Table 3. Regression coefficients before and after shrinkage in Europe4Footnote a countries

s.e., Standard error; SF12, Short Form 12.
a Europe4 is the UK, Spain, Slovenia and Portugal combined.
b The Europe4 country average is (0+0.1–0.285–0.108)/4.
c The coefficients for external countries were obtained by recalibrating in these countries.
The ability of the predictA model to discriminate between those who became anxious, and those who did not was assessed through the C-index (Table 4) and the Hedges' g estimate of effect size (Table 5). In Europe4 the overall C-index was 0.752 (95% CI 0.724–0.780). The model was better able to discriminate anxiety status at 6 than 24 months. When fitted to 6-month data alone, the C-index was 0.775 (95% CI 0.743–0.807) compared with 0.729 (95% CI 0.685–0.774) when fitted to 24-month data alone. The model was most predictive in Slovenia and least predictive in the UK (Table 4).
Table 4. C-indices for all participating countriesFootnote a

CI, Confidence interval.
a The C-index is similar to the area under the relative operating characteristic curve of sensitivity against 1 – specificity. A perfect test has a C-index of 1.00 while a test that performs no better than chance has a C-index of 0.5 (Cooper & Hedges, Reference Cooper and Hedges1994).
b Average C-index over 10 imputed datasets.
c This CI is calculated assuming that observations collected at 6 and 24 months are independent.
d Europe4 is the UK, Spain, Slovenia and Portugal combined.
Table 5. Hedges' g effect size estimatesFootnote a

CI, Confidence interval.
a Predicted probabilities were logarithmically transformed and compared between depressed and non-depressed individuals over the subsequent 6 and 24 months and both time periods. Hedges ' g is preferred to Cohen's d where the sizes of each group (depressed/non-depressed) are markedly unequal. The risk score was computed using unshrunk estimates in Europe and shrunk estimates in Chile.
b Europe4 is the UK, Spain, Slovenia and Portugal combined.
The effect size (Hedges' g) for the difference in log odds of predicted probability between attendees in Europe4 who subsequently developed anxiety and/or panic syndromes at 6 or 24 months and those who did not was 0.972 (95% CI 0.837–1.107) (Table 5). Again, the model discriminated best in Slovenia (1.282) and least well in the UK (0.841).
In order to examine the fit of the model at 6 and 24 months, we divided the predictA risk score into deciles. Within each decile we plotted mean risk score, obtained using the model coefficients shown in Table 3, versus observed probability of anxiety (Fig. 1). Similar plots were also produced using 6- and 12-month data alone (Fig. 1). The average predicted risks within deciles of risk score are close to the observed risks for Europe4 countries (Fig. 1). The occurrence of anxiety or panic syndrome at 6 months in the highest decile of risk score in the Europe4 countries was almost 20% (Fig. 1) compared with the overall incidence of 5.5% in the imputed data.
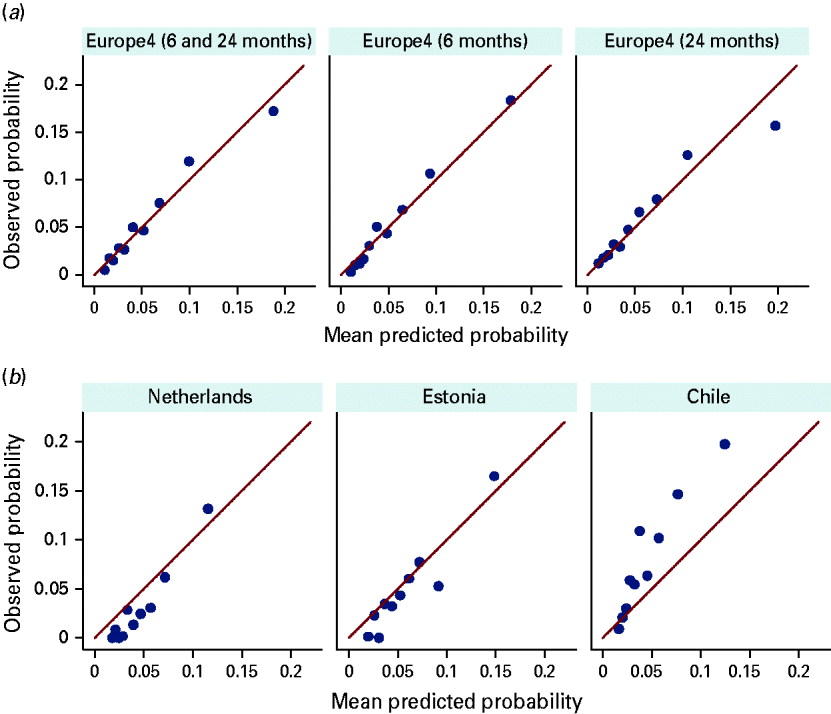
Fig. 1. Mean risk score plotted against observed probability within deciles of the risk score. (a) Estimates of risk for individuals in Europe4 (UK, Spain, Portugal and Slovenia) were produced using the unshrunk coefficients found in Table 3. (b) Risk scores at 6 months for the external datasets (The Netherlands, Estonia and Chile) were obtained using the average intercept of the four countries in Europe4 and the shrunk coefficients in Table 3.
External validation of the predictA algorithm in The Netherlands, Estonia and Chile
Table 1 shows the 6-month incidence rates for anxiety and panic syndromes in The Netherlands, Estonia and Chile. Predicted risks at 6 months for the external countries were obtained using shrunk coefficients. Since the risk model includes coefficients for the Europe4 countries in which it was built, the model for the external countries was modified by adding the average of the four shrunk coefficients arising from Europe4 (including the coefficient for the UK which is zero) to the shrunk intercept (see Tables 4 and 5 and Fig. 1). The predictA algorithm performed best in The Netherlands (C-index 0.811) and least well in Chile (C-index 0.707). This is demonstrated graphically in Fig. 1 where it can be seen that in The Netherlands and Estonia observed risks were in relatively good agreement with predicted risks, while in Chile agreement was less good. The weaker performance of predictA in Chile was possibly due to a higher incidence of panic and anxiety than in the European countries (Table 1), which means that risk is generally underestimated in Chile.
We give examples (Table 6) to illustrate the profiles of attendees at varying levels of risk (predicted probability of anxiety and panic syndromes on the predictA score algorithm). In order to demonstrate the potential impact of mutable factors (Short Form 12 physical health and mental health subscale scores, and unsupported difficulties in paid and/or unpaid work) on risk, we have recalculated scores in the last three examples after reducing or eliminating such factors.
Table 6. Examples of a range of predicted probabilities of anxiety and/or panic syndrome at baseline in Europe4Footnote a countries

SF12, Short Form 12; s.d., standard deviation.
a Europe4 is the UK, Spain, Slovenia and Portugal combined.
b Risk (predicted probability of anxiety) is for the intervals 0–6 and 18–24 months.
c Mean SF12 scores for Europe4 were: mental 48.9 (s.d.=10.6); physical 44.1 (s.d.=11.0). High scores indicate good health/well-being.
d Scores in parentheses correspond to removing work difficulties and correcting SF12 physical and mental health scores to the European mean (see text).
Sensitivity and specificity
Estimates of sensitivity and specificity at 6 and 24 months for varying risk score cut-offs are shown in Table 7.
Table 7. Sensitivity, specificity, likelihood ratio of the predictA model at 6 and 24 months using different cut-offs of the risk score

CI, Confidence interval.
a Europe4 is the UK, Spain, Slovenia and Portugal combined. Estimates were obtained using individuals with complete covariate data.
Discussion
To our knowledge this is the first risk algorithm for anxiety and panic to be developed in a general medical setting and validated in external populations. The C-index is a standard method for comparing the discriminative power of risk models (Pepe et al. Reference Pepe, Janes, Longton, Leisenring and Newcomb2004). In terms of C-indices the predictA risk score compares favourably with our predictD score for onset of major depression (King et al. Reference King, Walker, Levy, Bottomley, Royston, Weich, Bellón-Saameño, Moreno, Svab, Rotar, Rifel, Maaroos, Aluoja, Kalda, Neeleman, Geerlings, Xavier, Carraca, Goncalves-Pereira, Vicente, Saldivia, Melipillan, Torres-Gonzalez and Nazareth2008) as well as for risk indices for cardiovascular events (Conroy et al. Reference Conroy, Pyorala, Fitzgerald, Sans, Menotti, De Backer, De Bacquer, Ducimetiere, Jousilahti, Keil, Njolstad, Oganov, Thomsen, Tunstall-Pedoe, Tverdal, Wedel, Whincup, Wilhelmsen and Graham2003). The risk model developed included a variable for time, which allows us to use it to predict risk at 6 and 24 months (risk at intermediate times can also be calculated by interpolation). However, time had only a weak non-significant effect on risk; thus, in practice, an individual's estimated risk is effectively the same at 6 and 24 months. Our shrinkage factor estimates degree of over-fitting in the Europe4 data and allows for its adjustment in estimating risk of anxiety in new settings. In risk-model development, external validation and shrinkage for over-fitting are often not undertaken (Moons et al. Reference Moons, Donders, Steyerberg and Harrell2004). When the algorithm is applied in a country outside of the Europe4 countries we recommend that either the average Europe4 country coefficient (−0.073) be used or the coefficient for the European country that most closely matches the incidence of anxiety (if known) in the new setting (Table 3). If the algorithm is applied in one of the three external countries we suggest using the coefficient obtained by recalibration of the algorithm in this country (Table 3).
One strength of using data from a cohort that was established originally to develop a risk model for major depression (King et al. Reference King, Walker, Levy, Bottomley, Royston, Weich, Bellón-Saameño, Moreno, Svab, Rotar, Rifel, Maaroos, Aluoja, Kalda, Neeleman, Geerlings, Xavier, Carraca, Goncalves-Pereira, Vicente, Saldivia, Melipillan, Torres-Gonzalez and Nazareth2008) is that participants were unaware of the aim behind this risk modelling. When follow-up of the predictD cohort became possible beyond the 12 months envisaged originally in the Europe4 countries, we took the opportunity of measuring anxiety and panic syndromes as an outcome once again and this allowed us to develop a predictA model over 6 and 24 months in these four countries. One limitation was that anxiety disorders were only measured for the 6 months before each interview. Thus, although participants were followed up at 24 months in the Europe4 countries, the PHQ only enquired about anxiety symptoms in the 6 months preceding that follow-up point. Hence, we will not have captured any anxiety or panic syndromes that developed and resolved in the period 6 to 18 months after recruitment. Another limitation is the lower recruitment rates in the UK and The Netherlands, which possibly occurred because in these two countries researchers approached patients waiting for consultations, while in the other European countries doctors first introduced the study before contact with the research team. However, most importantly, response to follow-up in all countries was high, ensuring high internal validity of these findings. Although our risk factors are based on self-report, we used standardized instruments where possible and unstandardized questions were tested for reliability (King et al. Reference King, Weich, Torres-González, Svab, Maaroos, Neeleman, Xavier, Morris, Walker, Bellón-Saameño, Moreno-Küstner, Rotar, Rifel, Aluoja, Kalda, Geerlings, Carraça, de Almeida, Vicente, Saldivia, Rioseco and Nazareth2006). There is a moderate uncertainty in the parameter estimates due to missing data as measured by the fraction of missing information. This is principally due to missing outcome data at 24 months. However, in all cases the fraction of missing information is below 50%, the value at which Ruben (Reference Rubin2003) questions the usefulness of multiple imputation. Finally, we stress that we have only considered generalized anxiety and panic disorders as defined by the PHQ. Our data do not concern other anxiety disorders such as post-traumatic stress disorder or phobic anxiety disorders.
One notable finding is the overlap in the nature of the risk factors between the predictD model for major depression (King et al. Reference King, Walker, Levy, Bottomley, Royston, Weich, Bellón-Saameño, Moreno, Svab, Rotar, Rifel, Maaroos, Aluoja, Kalda, Neeleman, Geerlings, Xavier, Carraca, Goncalves-Pereira, Vicente, Saldivia, Melipillan, Torres-Gonzalez and Nazareth2008) and predictA for anxiety disorders. Although their contribution to risk was different (in terms of regression coefficients), risk factors common to both disorders were lifetime depression screen, family history of psychological difficulties, Short Form 12 physical health subscale score, Short Form 12 mental health subscale score, and unsupported difficulties in paid and/or unpaid work. Sex, age and country were forced into both models (predictA and predictD). Two additional risk factors in the predictD algorithm for major depression (level of education and recent discrimination) were absent from the predictA model. However, recent discrimination appeared in seven of the 10 imputed datasets, suggesting it was close to inclusion. This similarity between the two risk algorithms may be due at least in part to the close correlation (co-morbidity) of depressive and anxiety/panic disorders (Gorman, Reference Gorman1996). Recent calls have been made for not separating these disorders into separate DSM/International Classification of Diseases (ICD) chapters (Goldberg et al. Reference Goldberg, Krueger, Andrews and Hobbs2009). Moreover, other data have suggested that a core psychopathology of neuroticism is common to both anxiety disorders and depression (Griffith et al. Reference Griffith, Zinbarg, Craske, Mineka, Rose, Waters and Sutton2010). In our study, however, it must be emphasized that the populations in each of our analyses were substantially different; in the predictD analysis, only participants without major depression at recruitment were included, while for predictA, only those without anxiety syndromes were analysed. Furthermore, although lifetime depression was a risk factor in the predictA algorithm for onset of anxiety, major depression at baseline was not a predictor of anxiety any more than an anxiety syndrome at baseline was a predictor of major depression in predictD. An alternative explanation to co-morbidity is the possibility that depressive and anxiety disorders are expressions of a broader latent pathological process (Tyrer et al. Reference Tyrer, Seivewright, Ferguson and Tyrer1992; Middeldorp et al. Reference Middeldorp, Cath, Van Dyck and Boomsma2005; Krueger & Markon, Reference Krueger and Markon2006; Mennin et al. Reference Mennin, Heimberg, Fresco and Ritter2008).
As we have noted previously (King et al. Reference King, Walker, Levy, Bottomley, Royston, Weich, Bellón-Saameño, Moreno, Svab, Rotar, Rifel, Maaroos, Aluoja, Kalda, Neeleman, Geerlings, Xavier, Carraca, Goncalves-Pereira, Vicente, Saldivia, Melipillan, Torres-Gonzalez and Nazareth2008), our results do not address how the risk algorithms predictA and predictD might best be implemented in general practice. However, their potential role in prevention is clear. Our results expressed by the C-index and effect sizes for predictA demonstrate a clear difference in risk between participants who developed anxiety and or panic syndromes and those who did not. In showing a number of thresholds for sensitivity and specificity (Table 7) we have emphasized specificity at the cost of reduced sensitivity. We would recommend setting 6-month specificity at 80–85% (risk score between 0.07 and 0.08 or greater in Europe4 countries), in order to minimize the workload resulting from false positives, despite the obvious risk of missing a proportion of those truly at risk of anxiety syndromes.
Recognition of those at risk in family practice may be helpful when it leads to watchful waiting or active support, such as re-starting treatment in patients with a history of anxiety. Advising patients on the nature of anxiety or on brief cognitive behaviour or problem-solving strategies they might undertake to reduce their risk could also be envisaged. Although efforts to reduce incidence of new or recurrent anxiety disorders might address factors such as physical health problems and work stress, this does not mean that when immutable factors (such as a family history of psychological disorders) predominate there can be no recourse to prevention. The effectiveness of a number of interventions for prevention of generalized anxiety disorders has been evaluated. These include self-help, problem-solving therapy (Hoek et al. Reference Hoek, Schuurmans, Koot and Cuijpers2009), online delivery of cognitive behaviour skills (Christensen et al. Reference Christensen, Griffiths, Mackinnon, Kalia, Batterham, Kenardy, Eagleson and Bennett2010) for adolescents, and stepped care incorporating psycho-education and problem-solving skills in people aged 75 years and over (van 't Veer-Tazelaar et al. Reference van 't Veer-Tazelaar, van Marwijk, van Oppen, Nijpels, van Hout, Cuijpers, Stalman and Beekman2006). Further evaluation of the effectiveness of prevention of anxiety and panic disorders in general adult populations is required, regardless of the risk factors implicated.
Acknowledgements
M.K. had full access to all data in the study and takes responsibility for their integrity and the accuracy of the data analysis. We thank all patients and general practice staff who took part, Dr Carl Walker who assisted with management of the data in London, the European Office at University College London for their administrative assistance at the coordinating centre, Mr Kevin McCarthy, the project's scientific officer in the European Commission, Brussels, for his helpful support and guidance, the UK MRC GPRF, Ms Louise Letley, from the MRC GPRF, the general practitioners of the Utrecht General Practitioners’ Network and the Camden and Islington Foundation National Health Service (NHS) Trust. Collaboration between centres in Spain, Portugal, the UK and Chile was first inspired by the Maristán research network.
The research in Europe was funded by a grant from The European Commission, reference PREDICT-QL4-CT2002-00683. Funding in Chile was provided by project FONDEF DO2I-1140. We are also grateful for part support in Europe from: the Estonian Scientific Foundation (grant no. 5696); the Slovenian Ministry for Research (grant no. 4369-1027); the Spanish Ministry of Health (grant FIS references PI041980, PI041771, PI042450) and the Spanish Network of Primary Care Research, redIAPP (ISCIII-RETIC RD06/0018) and SAMSERAP group; and the UK NHS Research and Development office for providing service support costs in the UK. The funders had no direct role in the design or conduct of the study, interpretation of the data or review of the manuscript.
Declaration of Interest
None.










