Introduction
Major depression has serious and significant consequences for millions of people in the USA and around the world. At least one in five US adults experience depression in their lifetime and the past-year prevalence of depression is approximately 6% (Hasin et al. Reference Hasin, Goodwin, Stinson and Grant2005). Depression is associated with substantial individual suffering; occupational, social, and family role impairment; and is a leading cause of disability and mortality (Lopez & Mathers, Reference Lopez and Mathers2006; Saint Onge et al. Reference Saint Onge, Krueger and Rogers2014; WHO, 2016). By the year 2030, it is estimated that depression will be the leading cause of illness globally, after HIV/AIDS (Mathers & Loncar, Reference Mathers and Loncar2006). Depression is also the single strongest risk factor for suicide behavior (Hasin et al. Reference Hasin, Goodwin, Stinson and Grant2005; Chang et al. Reference Chang, Stuckler, Yip and Gunnell2013; WHO, 2016), which has increased over time (Case & Deaton, Reference Case and Deaton2015; Rockett et al. Reference Rockett, Lilly, Jia, Larkin, Miller, Nelson, Nolte, Putnam, Smith and Caine2016). While there has been substantial progress in both psychopharmacologic and psychotherapeutic treatments for depression (Shim et al. Reference Shim, Baltrus, Ye and Rust2011), most individuals with depression remain untreated or experience extensive delays between the onset of depression and treatment (Riolo et al. Reference Riolo, Nguyen, Greden and King2005; Shim et al. Reference Shim, Baltrus, Ye and Rust2011; Whiteford et al. Reference Whiteford, Harris, McKeon, Baxter, Pennell, Barendregt and Wang2013). Because depression impacts a significant percentage of the US population and has serious individual and societal consequences, it is important to understand whether and how the prevalence of depression has changed over time in the USA so that decisions about funding and strategies for public health efforts can be based on current population needs.
There has been a long-standing interest in estimating whether secular changes in depression and other disorders have occurred (e.g. Häfner, Reference Häfner1985). Several studies have reported increases in depression prevalence over time (e.g. Compton et al. Reference Compton, Conway, Steinson and Grant2006; Hidaka, Reference Hidaka2012). Building on this work by continuing to address this question with recent data is needed in order to identify trends in depression that can inform current public health efforts.
Further, prior cross-sectional epidemiologic studies have repeatedly identified substantial disparities in depression prevalence by demographic subgroups (e.g. gender, income, education). Yet, little data on trends in depression by these subgroups have been available. Younger and older adults report lower prevalences of depression than middle age groups (Pratt & Brody, Reference Pratt and Brody2014). With regard to race/ethnicity, people who identify as non-Hispanic White report a higher prevalence of depression than persons from other racial/ethnic groups with the exception of Native American persons (Hasin et al. Reference Hasin, Goodwin, Stinson and Grant2005; Williams et al. Reference Williams, González, Neighbors, Nesse, Abelson, Sweetman and Jackson2007). Compared with non-Hispanic Black persons, non-Hispanic White persons exhibit stronger relationships between depression symptoms and a subsequent diagnosis of major depressive disorder (Moazen-Zadeh & Assari, Reference Moazen-Zadeh and Assari2016), depression and hopelessness (Assari et al. Reference Assari, Moazen-Zadeh, Lankarani and Micol-Foster2016), and depression and mortality (Assari et al. Reference Assari, Moazen-Zadeh, Lankarani and Micol-Foster2016). In terms of gender, it has been well-established that more women than men report depression (e.g. Hasin et al. Reference Hasin, Goodwin, Stinson and Grant2005, Van de Velde et al. Reference Van de Velde, Bracke and Levecque2010, Pratt & Brody, Reference Pratt and Brody2014, Kuehner, Reference Kuehner2017). Finally, indicators of lower socioeconomic status (SES) are associated with higher prevalences of depression (Everson et al. Reference Everson, Maty, Lynch and Kaplan2002; Lorant et al. Reference Lorant, Deliege, Eaton, Robert, Philippot and Ansseau2003; Pratt & Brody, Reference Pratt and Brody2014; Hasin & Grant, Reference Hasin and Grant2015) and greater odds of chronic depression (Rubio et al. Reference Rubio, Markowitz, Alegría, Pérez-Fuentes, Liu, Lin and Blanco2011). To our knowledge, there is no currently available information estimating trends in depression among demographic subgroups in the USA over the past decade. If depression is found to be increasing overall, or increasing to a greater degree among specific demographic subgroups, this information can help identify populations most in need of public health and outreach efforts.
The purpose of the current study was to examine changes in the prevalence of depression in the USA over an 11-year period. First, the study estimated trends in the prevalence of depression among US individuals, ages 12 and older from 2005 to 2015. Second, the study estimated trends in the prevalence of depression from 2005 to 2015 by demographic characteristics (i.e. age, race/ethnicity, gender, income, education).
Methods
Study population
Study data were drawn from the National Survey on Drug Use and Health (NSDUH) public data portal (http://www.icpsr.umich.edu/). The NSDUH provides annual cross-sectional national data on tobacco use, other substance use, and mental health in the USA and is described in depth elsewhere (SAMHSA, 2015). A multistage area probability sample for each of the 50 states and the District of Columbia was conducted to represent the male and female civilian non-institutionalized population of the USA aged 12 and older. The datasets from each year included in the current analyses (2005–2015) were concatenated, adding a variable for the survey year. Person-level analysis sampling weight for the NSDUH was computed to control for individual-level non-response, and were adjusted to ensure consistency with population estimates obtained from the US Census Bureau. In order to use the 11 years of combined data, a new weight was created upon aggregating the 11 datasets by dividing the original weight by the number of datasets combined. Further descriptions of the sampling methods and survey techniques for the NSDUH are found elsewhere (SAMHSA, 2015). For this study, analyses were restricted to participants who responded to questions about past-year depression at the time of the interview resulting in a total analytic sample of N = 607 520.
Measures
Past-year depression
Questions to assess major depressive episode (MDE) were based on DSM-IV criteria (American Psychological Association, 1994) and adapted from the depression section of the National Comorbidity Survey-Replication (Hedden et al. Reference Hedden, Gfroerer, Barker, Smith, Pemberton, Saavedra, Forman-Hoffman, Ringeisen and Novak2012) for adults and from the National Comorbidity Survey-Adolescent for youth. Separate depression modules were administrated to adults (18 years old or older) and to youth (12–17 years old). Participants were classified as having had a lifetime MDE based on the report of having five or more out of nine symptoms for MDE, including either depressed mood or loss of interest or pleasure in daily activities, during the same 2-week period in their lifetime. Respondents with lifetime MDE were further classified as having past-year MDE if they met criteria for a lifetime MDE and reported feeling depressed or lost interest or pleasure in daily activities, as well as other symptoms, for at least 2 weeks during the past 12 months. Due to changes in the questionnaire in 2008, adjusted past-year MDE variables for adults were developed to allow for comparison between the years 2005 and 2008 and the later years. The past-year MDE variable for this study was created by combining the youth and adult variables.
Demographics
Demographic variables were categorized as follows: age (12–17 years old as reference group, 18–25 years old, 26–34 years old, 35–49 years old, 50 years or older), race/ethnicity (collapsed from seven to four categories: non-Hispanic White as reference group, non-Hispanic Black, Hispanic, and Other), gender (male as reference group, female), total annual family income (less than $20 000 per year as reference group, $20 000 to $49 999 per year, $50 000 to $74 999 per year and greater than $75 000 per year), education (less than high school as reference group, high school graduate, some college, college graduate), and marital status (collapsed from four to three categories: married as reference group, widowed, separated or divorced, never married).
Statistical analysis
First, the prevalence of past-year depression and associated standard errors among the whole population and stratified by each survey year were calculated from the year 2005 to the year 2015. Time trends in the prevalence of past-year depression were tested using logistic regression with continuous year as the predictor for the linear time trend. These analyses were conducted twice: first with no covariates (unadjusted) and then repeated while adjusting for age, gender, race/ethnicity, total annual family income, education, and marital status using the categories listed above.
Second, separate time trend analyses using logistic regression described above were conducted further stratified by either age, race/ethnicity, gender, total annual family income, or education. These analyses were conducted twice: once with no covariates (unadjusted model) and once controlling for the other demographic variables (adjusted model).
Differential time trends in past-year depression between each demographic variable were tested by two-way interactions of year × each demographic in logistic regression. A logistic regression of past-year depression found the two-way interaction of year ×age to be significant so the group-specific two-way interactions were further tested (i.e. 12–17 years old v. 18–25 years old; 12–17 years old v. 26–34 years old; 12–17 years old v. 35–49 years old; and 12–17 years old v. 50 years and older) in logistic regression. All analyses were performed incorporating the NSDUH sampling weights and controlling for the complex clustered sampling using SAS-callable SUDAAN Version 11.0.1 (RTI International, Research Triangle Park, NC) (http://www.rti.org/sudaan/).
Results
Trend in depression in the USA: 2005–2015
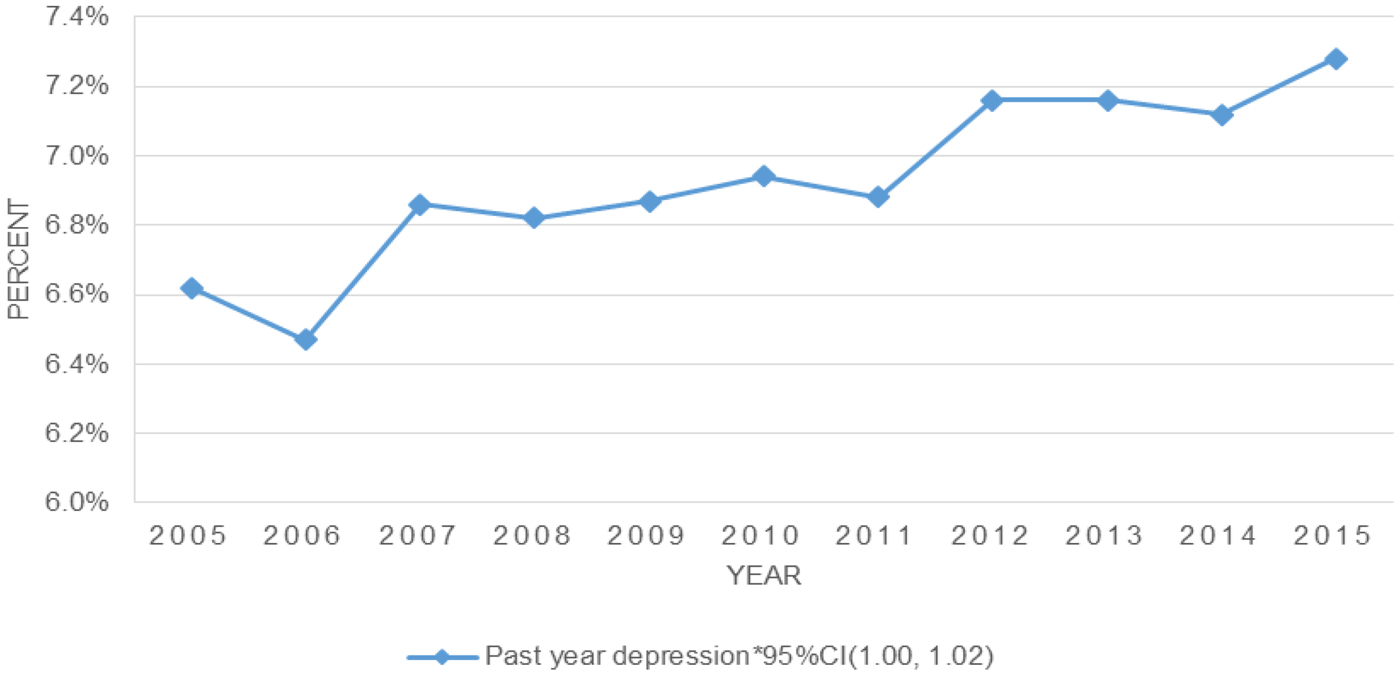
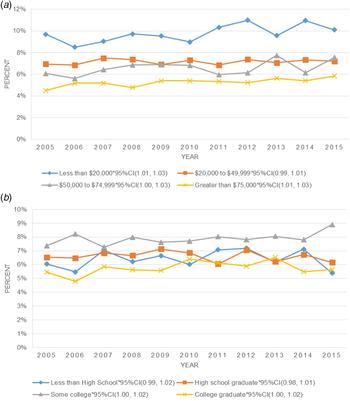
Overall, the prevalence of past-year depression increased significantly from 2005 to 2015 (see Fig. 1); this increase remained statistically significant after adjusting for demographic characteristics (see online Supplemental Table S1).
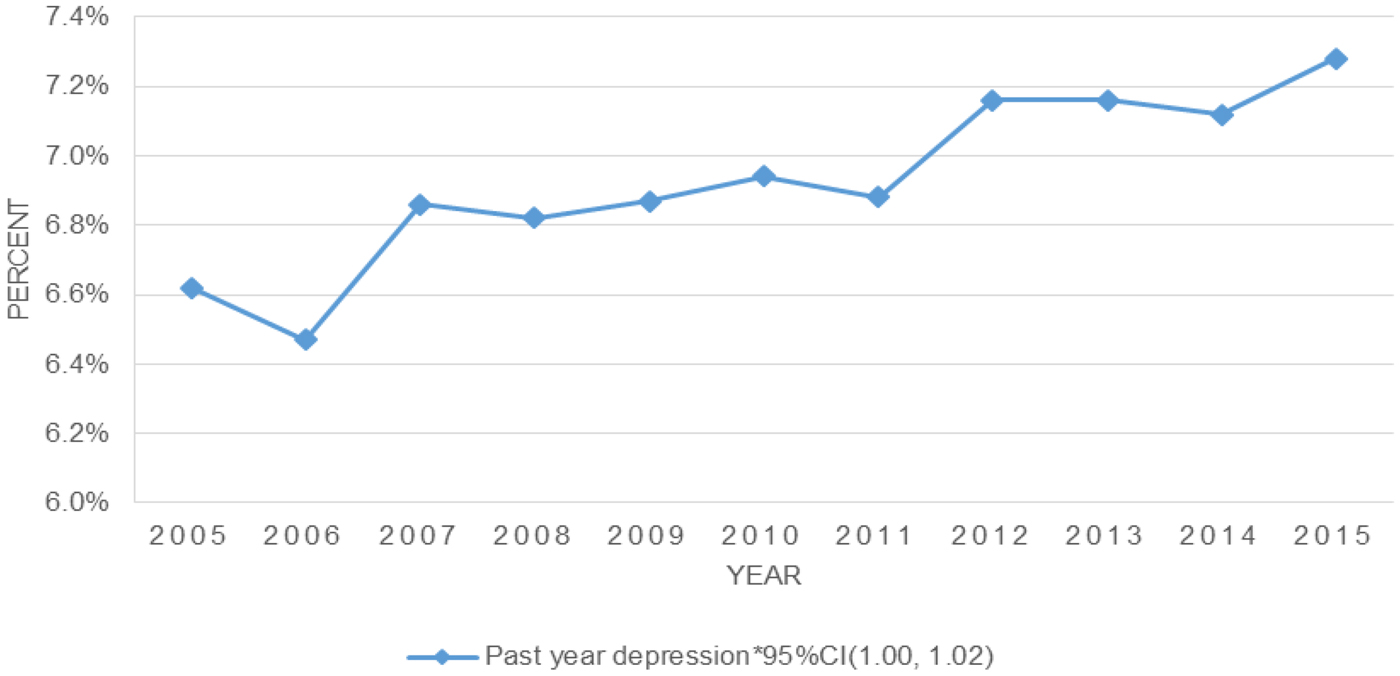
Fig. 1. Depression in the USA from 2005 to 2015.
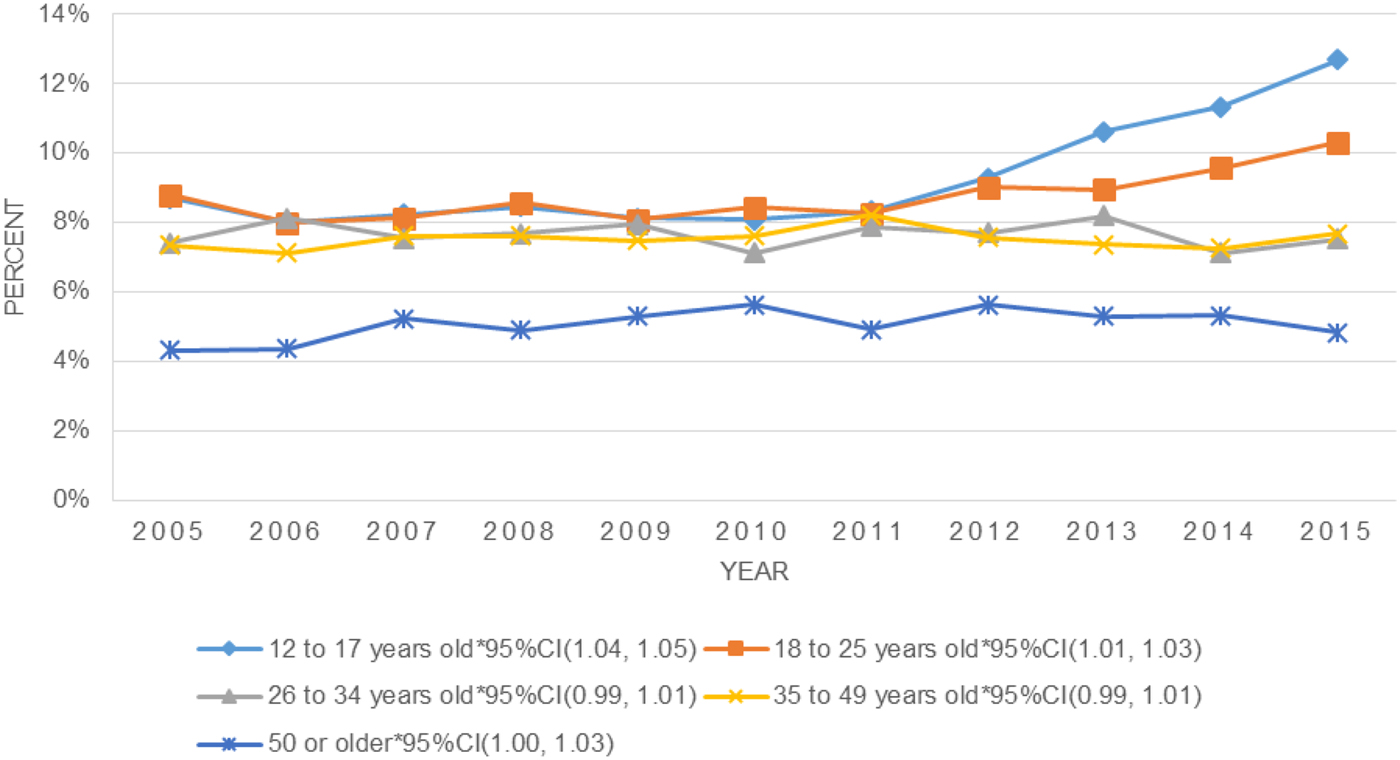
Depression in the USA from 2005 to 2015 by age
Stratifying the population by age, and adjusting for other demographics, significant increases in depression from 2005 to 2015 were observed among those 12–17 years old, 18–25 years old, and 50 years and older (see Fig. 2 and online Supplemental Table S2). There were no significant increases in depression observed among those 26–34 years old or 35–49 years old. There was a significant year × age interaction indicating that the increase in depression among youth ages 12–17 years old was significantly more rapid than the increases in every other age group. These trends remained significant and relatively unchanged after adjusting for demographic characteristics.
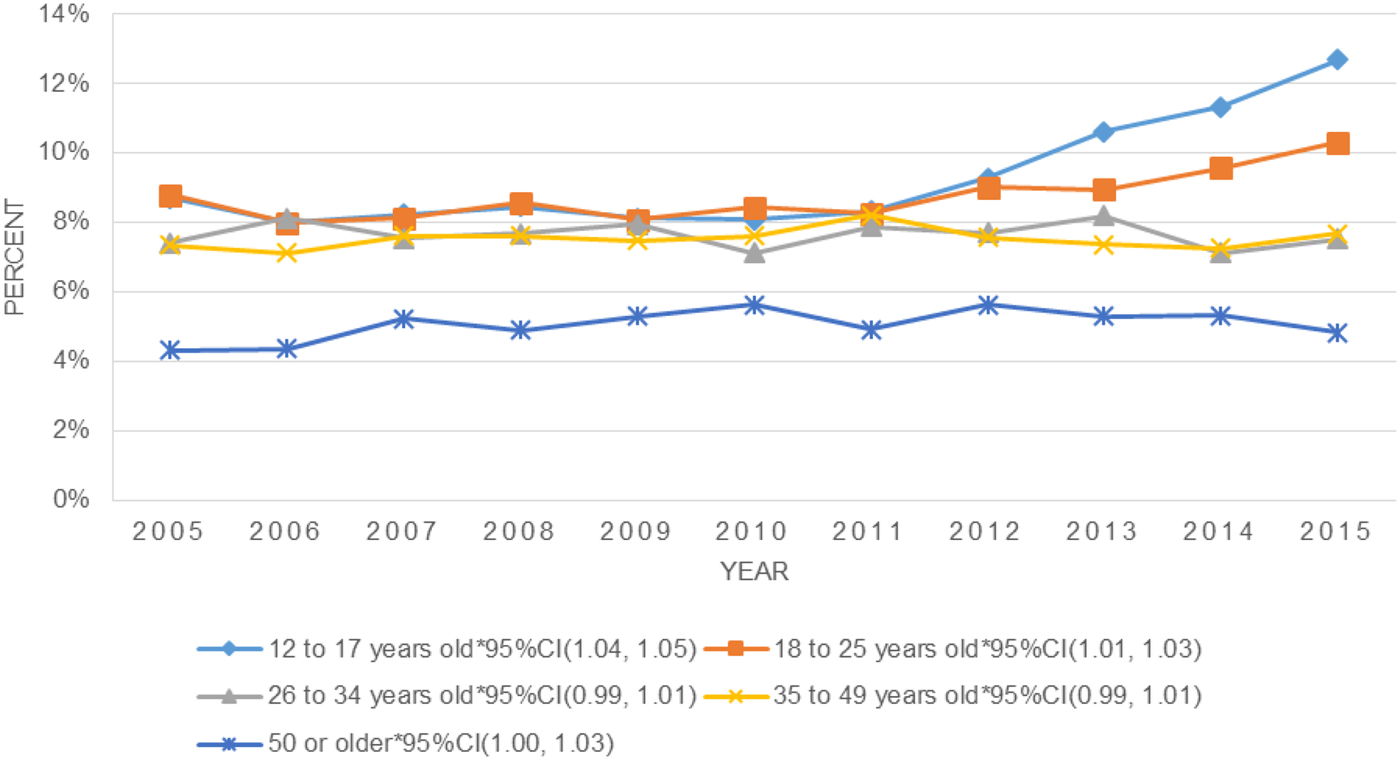
Fig. 2. Depression by age, 2005–2015.
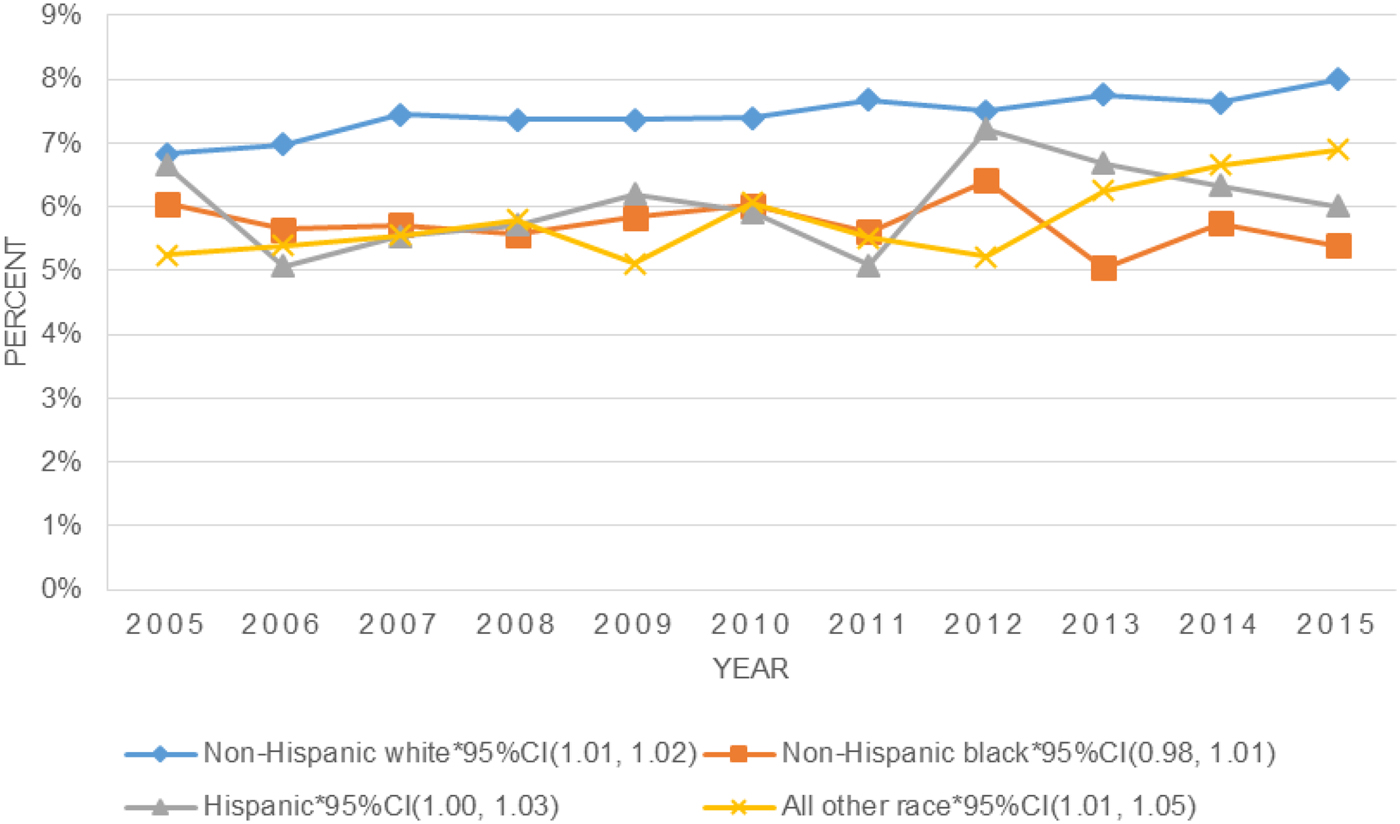
Depression in the USA from 2005 to 2015 by race/ethnicity
Stratifying the population by race/ethnicity, a significant increase in depression from 2005 to 2015 was observed among those who identified as non-Hispanic White (see Fig. 3 and online Supplemental Table S3). This increase remained significant after adjusting for demographic characteristics. Unadjusted analyses revealed a significant increase in depression among those who identified as Other race/ethnicity, though this increase was no longer significant after adjusting for other demographics. There was no significant change in depression observed among those of non-Hispanic Black or Hispanic race/ethnicity. The year × race/ethnicity interaction was not significant.
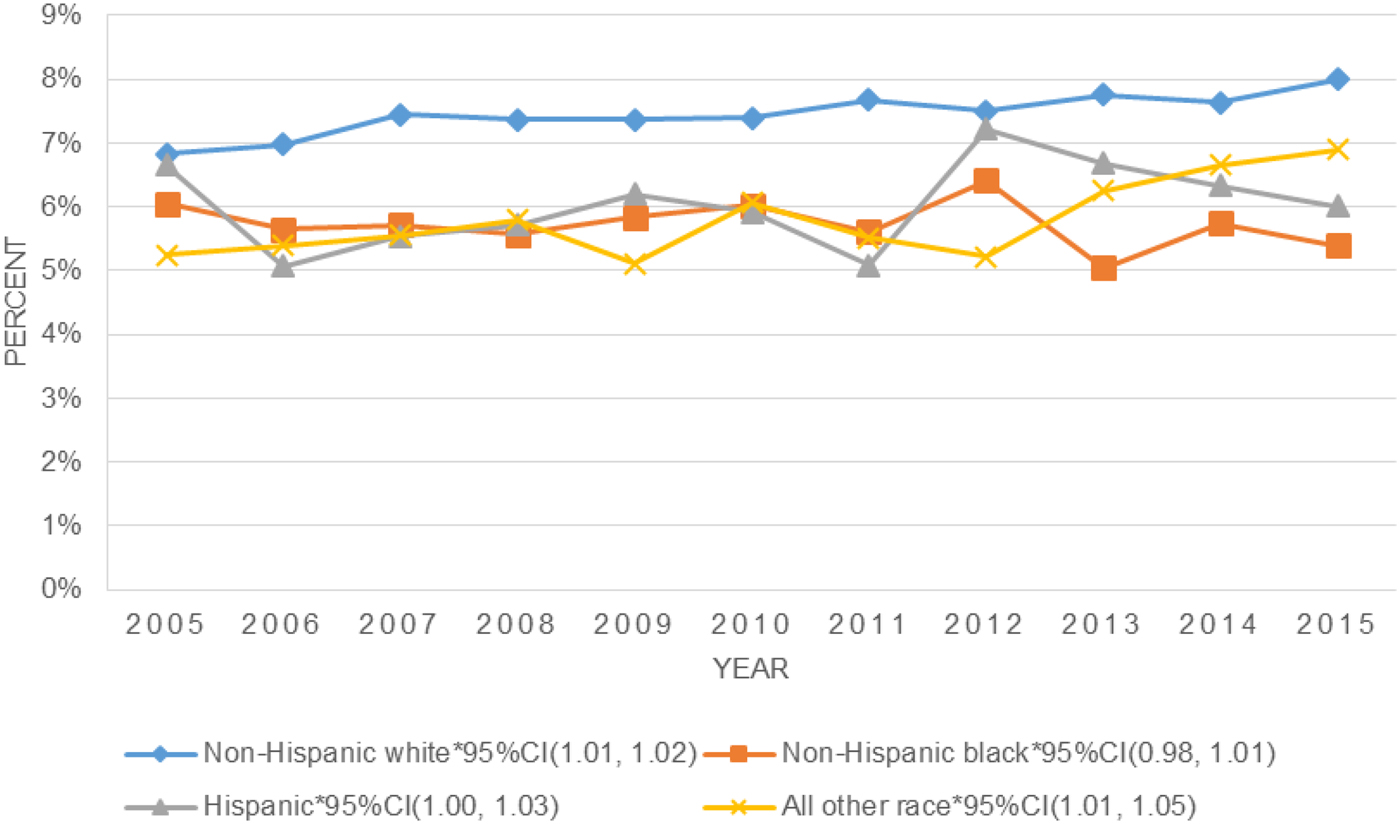
Fig. 3. Depression by race, 2005–2015.
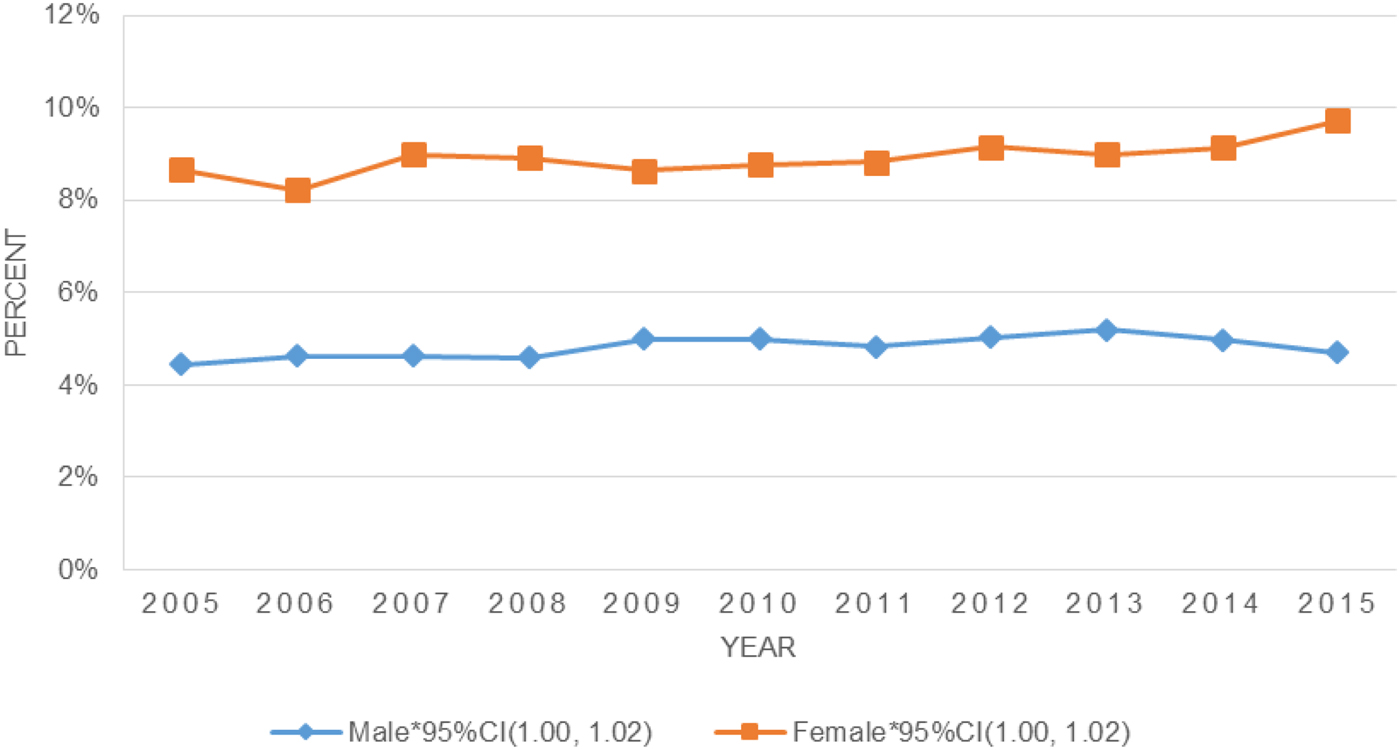
Depression in the USA from 2005 to 2015 by gender
The prevalence of depression increased significantly from 2005 to 2015 among both men and women (see Fig. 4 and online Supplemental Table S4). There was no significant difference in the rate of increase between men and women.
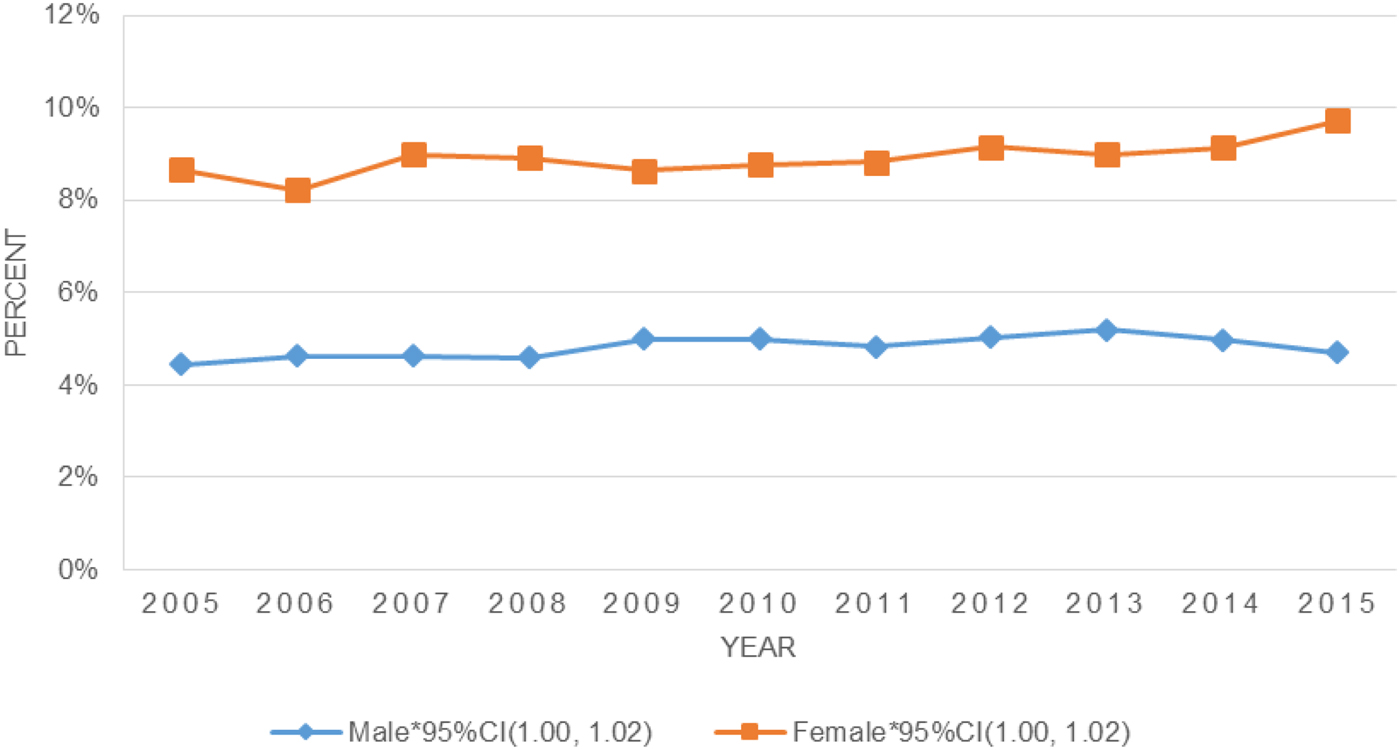
Fig. 4. Depression by gender, 2005–2015.
Depression in the USA from 2005 to 2015 by socioeconomic status indicators
There was a significant increase in depression from 2005 to 2015 among those in the lowest annual household income group and those in the highest annual household income group (see Fig. 5a and online Supplemental Table S5). These associations remained significant after adjusting for demographic characteristics. There was a significant increase in depression for those earning $50 000 to $74 999 per year; however, the increase did not remain significant after adjusting for other demographics. There were no changes observed in the prevalence of depression over time for the other middle-income group (i.e. $20 000–$49 000 per year). The year × income interaction was not significant.
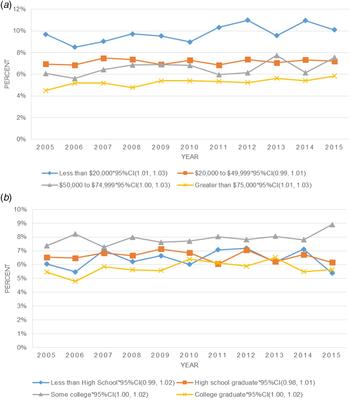
Fig. 5. Depression by socioeconomic status indicators (a, income; b, education) 2005–2015.
In unadjusted analyses, the prevalence of depression increased significantly from 2005 to 2015 among those with some college education (see Fig. 5b and online Supplemental Table S6). This association remained significant after adjusting for demographic characteristics. The increase in depression prevalence was also significant for college graduates after adjusting for demographics. There was no change in the prevalence of depression from 2005 to 2015 among those with less than a high school education or high school graduates. The year × education interaction was not significant.
Discussion
The goal of the current study was to investigate trends in the prevalence of past-year depression from 2005 to 2015 for US persons age 12 years and older. Several key findings emerged. First, the overall prevalence of depression increased significantly over this period of time. Second, more rapid increases in depression prevalence occurred for specific demographic subgroups. Specifically, there was a significant increase in depression among the youngest (12–17 years old and 18–25 years old) and oldest (50 years and older) age groups and the increase was significantly more rapid among the youngest age group (12–17 years old) compared with every other age group. In terms of race/ethnicity, a significant increase in depression was seen only among non-Hispanic White individuals, though the rates of increase over time did not differ significantly by race/ethnicity. There were also significant increases in depression among those in the lowest income group and the highest income group; and among those in the highest education groups (some college or college degree and above) though, again, the rates of increase did not significantly differ by income or education.
Our data suggest an overall increase in depression prevalence in recent years among persons in the USA. The current study provides updated data on depression prevalences over time that are consistent with increases in depression prevalence found in older data on US and non-US adults (e.g. Compton et al. Reference Compton, Conway, Steinson and Grant2006; Hidaka, Reference Hidaka2012) as well as increases in depression treatment (Olfson et al. Reference Olfson, Marcus, Druss, Elinson, Tanielian and Pincus2002; Marcus & Olfson, Reference Marcus and Olfson2010). The increase in depression prevalence over time is also consistent with increases in mental health problems over time seen in data from European countries (Katikireddi et al. Reference Katikireddi, Niedzwiedz and Popham2012; Barr et al. Reference Barr, Kinderman and Whitehead2015).
While demographic differences in depression prevalence at a single time point had been previously identified, the current study is novel in its examination of differences in trends in depression over time by demographic subgroups. With regard to age, past research found lower depression prevalences for younger and older adults (Pratt & Brody, Reference Pratt and Brody2014) yet studies have also reported increases in depression for adolescents and older adults (e.g. Akincigil et al. Reference Akincigil, Olfson, Walkup, Siegel, Kalay, Amin, Zurlo and Crystal2011; Skovlund et al. Reference Skovlund, Kessing, Mørch and Lidegaard2017). Our data suggest that the prevalence of depression is increasing faster for younger age groups than for middle and older age groups which may, over time, reduce the previously found prevalence differences among age groups.
On the other hand, past research found a higher prevalence of depression for White persons than most other race/ethnicities (Hasin et al. Reference Hasin, Goodwin, Stinson and Grant2005) as well as greater increases in suicide over time for midlife White adults compared with other racial/ethnic groups (Case & Deaton, Reference Case and Deaton2015). Our findings suggest that differences in depression and suicidal behavior between Whites and other racial/ethnic groups may be growing over time. Even though the trend lines for White persons v. other racial/ethnic persons did not differ significantly, White persons were the only racial/ethnic group in the current study that showed a significant increase in depression prevalence over time. With regard to gender, more women report depression than men (e.g. Hasin et al. Reference Hasin, Goodwin, Stinson and Grant2005) and we found that both women and men demonstrate increasing depression prevalences over time with no differences in the rate of increase by gender. Finally, not only are lower SES indicators associated with a greater prevalence of depression (e.g. Hasin et al. Reference Hasin, Goodwin, Stinson and Grant2005), those with lower incomes showed significantly increasing prevalences of depression over time that were not found for middle income groups. Notably, the increases in mortality for White persons mentioned above (Case & Deaton, Reference Case and Deaton2015) were found to be greatest for persons with a high school education or less. These data can inform public health efforts aimed at reducing consequences of depression by going beyond determining which groups are reporting higher depression prevalences to bring attention and resources to those groups whose increase in depression over time is greater than others.
Even though the changes in depression by race/ethnicity were not statistically significant between groups, persons who identify as White demonstrated a significant increase of depression while the increase in depression for other racial/ethnic groups, such as persons who identify as Black, were not significant. Other research has reported a higher prevalence of depression and suicide for persons who are White compared with persons who are Black (Barnes et al. Reference Barnes, Keyes and Bates2013; Case & Deaton, Reference Case and Deaton2015; Barnes & Bates, Reference Barnes and Bates2017). This lower prevalence of depression and other mental disorders among Blacks compared with Whites stands in contrast to greater distress, greater stressors including inequality and discrimination, poorer health outcomes, and greater mortality experienced by US persons who are Black compared with those who are White, a difference that has been called the Black–White paradox (Williams & Earl, Reference Williams and Earl2007; Keyes, Reference Keyes2009; Barnes & Bates, Reference Barnes and Bates2017). Further, the relationship between depression and health conditions is stronger for White adults than Black adults (Assari et al. Reference Assari, Burgard and Zivin2015). The gap between Black persons and White persons in mental health increases when controlling for perceived discrimination (Keyes, Reference Keyes2009) and with greater educational attainment (Barnes et al. Reference Barnes, Keyes and Bates2013). As our results found a significant increase in depression prevalence during the study period for White persons and no significant change for Black persons, it is possible that the mental health gap between Blacks and Whites may be widening over time.
There are a wide range of risk factors implicated in depression including environmental and genetic factors (e.g. Sullivan et al. Reference Sullivan, Neale and Kendler2000, Lorant et al. Reference Lorant, Deliege, Eaton, Robert, Philippot and Ansseau2003, Kendler et al. Reference Kendler, Gatz, Gardner and Pedersen2006, Lopez-Leon et al. Reference Lopez-Leon, Janssens, Gonzalez-Zuloeta Ladd, Del-Favero, Claes, Oostra and van Duijn2008, Colman & Ataullahjan, Reference Colman and Ataullahjan2010, Shim et al. Reference Shim, Baltrus, Ye and Rust2011, Hidaka, Reference Hidaka2012) and it is important to understand which factor/s relate to these changes in depression. One environmental factor that may be implicated in increases in depression prevalence over time is stress. The majority of US adults report that their level of stress has increased over time (American Psychological Association, 2014). Money and work are cited as the most common reasons for stress for US adults (American Psychological Association, 2016) and low income, job loss/unemployment, and negative life events are risk factors for depression (Bonde, Reference Bonde2008). The time frame of the current study included 2008 and there is evidence for increases in mental health issues, including depression, from the years before to the years after the 2008 recession from European countries (Katikireddi et al. Reference Katikireddi, Niedzwiedz and Popham2012; Economou et al. Reference Economou, Madianos, Peppou, Patelakis and Stefanis2013; Barr et al. Reference Barr, Kinderman and Whitehead2015). Further, there is evidence for increases in completed suicides in the USA and other countries around the world in the years after the 2008 recession (Reeves et al. Reference Reeves, Stuckler, McKee, Gunnell, Chang and Basu2012; Chang et al. Reference Chang, Stuckler, Yip and Gunnell2013). A better understanding of factors related to increases in depression can inform clinical and public health intervention efforts (e.g. targeting stress, policies to increase employment or reduce economic stress).
With regard to depression among demographic subgroups, several studies in the USA that either included samples from specific states or cities (e.g. Detroit, Michigan) or included subsamples of adults in the USA (e.g. adults age 57 or older) showed relationships between the financial crisis of 2008 and increased depression, anxiety, and suicide rates in various demographic subgroups (Burgard et al. Reference Burgard, Seefeldt and Zelner2012; McLaughlin et al. Reference McLaughlin, Nandi, Keyes, Uddin, Aiello, Galea and Koenen2012; Osypuk et al. Reference Osypuk, Caldwell, Platt and Misra2012; Reeves et al. Reference Reeves, Stuckler, McKee, Gunnell, Chang and Basu2012; Cagney et al. Reference Cagney, Browning, Iveniuk and English2014) and our data demonstrated similar subgroup differences at a US population level. There is evidence that the impact of financial-related stress may be disproportionate among men (Chang et al. Reference Chang, Stuckler, Yip and Gunnell2013; Azorin et al. Reference Azorin, Belzeaux, Fakra, Kaladjian, Hantouche, Lancrenon and Adida2014), who show a stronger relationship between stressful life events and depression compared with women (Rice et al. Reference Rice, Fallon, Aucote, Möller-Leimkühler, Treeby and Amminger2015; Assari & Lankarani, Reference Assari and Lankarani2016b); non-Hispanic White adults, who evidence a stronger relationship between depression and hopelessness (Assari & Lankarani, Reference Assari and Lankarani2016a) and between depression and mortality (Assari et al. Reference Assari, Moazen-Zadeh, Lankarani and Micol-Foster2016) compared with non-Hispanic Black adults; and persons with lower incomes and lower levels of formal education (Burgard et al. Reference Burgard, Seefeldt and Zelner2012; McLaughlin et al. Reference McLaughlin, Nandi, Keyes, Uddin, Aiello, Galea and Koenen2012; Chang et al. Reference Chang, Stuckler, Yip and Gunnell2013). Case & Deaton (Reference Case and Deaton2015) found that White midlife adults, the group that reported the largest increases in mortality, reported increases in poor mental health, psychological distress, and difficulties with activities of daily living including being able to work over time. While stress is one potential contributor to increases in depression prevalence, more research is needed to clarify the role of stress and other factors involved in the increase in depression. More research is also needed to determine the best ways to target implicated factors in order to reduce depression prevalence, duration, and consequences especially in subgroups that are showing quicker increases in depression.
Attention to age-specific risk factors for depression is also needed. In the USA, teens report levels of stress that are comparable with adults (American Psychological Association, 2014) and the mental health of children is impacted by financial stress (Solantaus et al. Reference Solantaus, Leinonen and Punamaki2004). A report using NSDUH data demonstrated an increase in the prevalence of depression in teens from 2005 to 2014 (Mojtabai et al. Reference Mojtabai, Olfson and Han2016) and our study expanded on these data to show that depression for youth is not just increasing but it is actually increasing faster than any other age group. Causes of the rise in depression in adolescents should be further explored as adolescents are increasingly exposed to risk factors derived from the use of new technologies, such as cyberbullying (Kessel Schneider et al. Reference Kessel Schneider, O'Donnell and Smith2012) and problematic social media use (Lin et al. Reference Lin, Sidani, Shensa, Radovic, Miller, Colditz, Hoffman, Giles and Primack2016; Shensa et al. Reference Shensa, Escobar-Viera, Sidani, Bowman, Marshal and Primack2017; see Seabrook et al. Reference Seabrook, Kern and Rickard2016 for a review and examiniation of moderators of social media and depression). Further, young adults may be impacted by economic-related stress through their family members or in terms of their own employment prospects. It is notable that Mojtabai et al. (Reference Mojtabai, Olfson and Han2016) did not find a corresponding increase in mental health treatment along with the increase in depression prevalence for teens suggesting that the proportion of young people with depression who are not receiving treatment for their depression may be increasing over time as well. Efforts to understand depression among teens should also include examining ways to increase the utilization of depression treatments for this age group.
While there are a number of strengths to using the NSDUH data including yearly data collection, which allowed the examination of trends over time; the large sample sizes, which allowed the examination of trends in demographic subgroups; the recency of the data compared with other examinations of depression over time; and the representativeness of the sample to the US population, there are also a number of limitations. Additional research would also be needed to determine whether these results generalize to persons who were not included in the analytic sample (e.g. persons outside of the USA). An increase in depression prevalence over time may be due to an increase in the incidence of depression, an increase in the duration of depression, or a combination of both. We were not able to examine depression incidence in the current study due to the variables available for analysis. Additional important information would be gained from examining the incidence of depression over time overall and by demographic subgroups in future studies. Further, this study included waves of cross-sectional data that are subject to age, period, and cohort effects as well as biases related to retroactive recall. On a related note, cross-sectional data does not allow the examination of individuals over time, specifically the impact of changes in variables potentially related to depression (e.g. employment and financial issues) and how these changes are associated with changes in depression prevalence. Where these data exist, it is important for researchers to examine factors that may be driving changes in depression over time in longitudinal data.
Additional research is needed to understand potential mediators of the increase in depression overall and for specific demographic subgroups. It is likely that there are multiple pathways to increases in depression prevalence; including increases in incidence, increases in duration, and delayed or less access to treatment; and a well-considered model includes a combination of family/genetic and environmental factors (Rubio et al. Reference Rubio, Markowitz, Alegría, Pérez-Fuentes, Liu, Lin and Blanco2011; WHO, 2016). While environmental changes are more likely to be related to the increase of depression incidence or duration than biological/genetic changes due to the short time frame, it would be important to study a range of potential variables that are associated with the increase in depression in order to provide the best prevention and intervention efforts to US persons. The subgroups most affected by the increase in depression prevalence may offer some clues to what the underlying causes of the increase might be, and these require further research.
Over the past 11 years, the prevalence of past-year depression increased significantly overall in the USA and the increases were most concentrated among youth, non-Hispanic White persons, those in the lowest income group, and those in the highest education and income groups. While not always diagnosed, depression is among the most treatable mental disorders. Identifying subgroups that are experiencing significant and/or greater increases in depression over time can help guide the allocation of funding and resources toward the subgroups that are facing the greatest individual and societal consequences from depression. Further research into understanding the macro level, micro level, and individual factors that are contributing to the observed increase in depression, including factors specific to depression in demographic subgroups, would also help to direct public health prevention and intervention efforts.
Supplementary Material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291717002781
Acknowledgments
This work was supported by NIDA/NIH (grant #DA20892).
Declaration of Interest
None.
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.