Introduction
For emergency communication centers that are using the software version of the Medical Priority Dispatch System (MPDS), and have achieved the distinction of Accredited Center of Excellence (ACE) through the International Academies of Emergency Dispastch (IAED; Salt Lake City, Utah USA), a secondary triage process – the Emergency Communication Nurse System (ECNS) – has the potential to reduce the high number of ambulance responses to non-emergency calls and to help alleviate overcrowding in busy hospital emergency rooms. The ECNS places specially trained triage nurses, known as Emergency Communication Nurses (ECNs), inside the emergency medical dispatch center to provide secondary triage for patients with low-acuity conditions once the initial triage has been completed by the Emergency Medical Dispatcher (EMD). After completing a secondary triage, the ECN has the authority to direct qualifying patients to non-ambulance, non-hospital, treatment venues such as urgent care clinics, walk-in clinics, primary care physician’s offices, and various other outpatient facilities, or (in rare instances ) they can escalate the urgency of an ambulance response, should it be indicated.
During the initial 911 triage process, the EMD is responsible for correctly identifying the patient’s “determinant code.” This determinant code includes the priority level: OMEGA, ALPHA, BRAVO, CHARLIE, DELTA, and ECHO (Figure 1) – in essence, the dispatch triage level – along with a more specific description of the patient’s primary condition or symptom.Reference Scott, Clawson, Fivaz, McQueen, Gardett, Schultz, Youngquist and Olola 1 The necessity to require high protocol compliance of EMDs before attempting dispatch triage and referral of low-acuity cases is a prerequisite. High compliance to protocol results in significantly higher accuracy in determinant code selection (in Los Angeles (California USA), a 56% improvement),Reference Clawson, Dernocoeur and Murray 2 and that compliance can be affected very positively by a formal case-review program with routine feedback of standardized compliance levels to EMDs.Reference Clawson, Dernocoeur and Murray 3
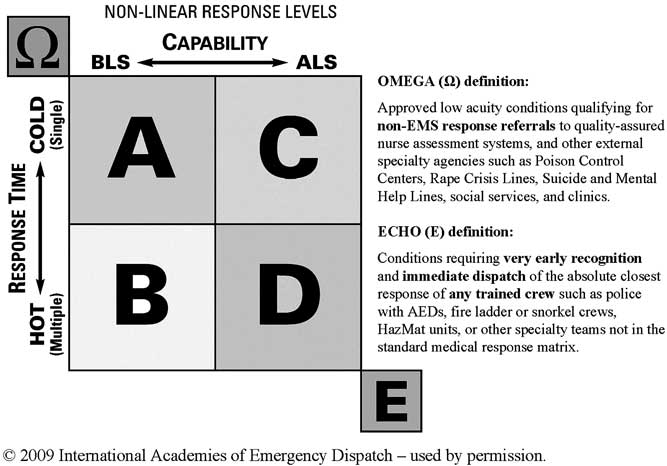
Figure 1 Medical Priority Dispatch System Response Matrix. Abbreviations: Ω, OMEGA; A, ALPHA; ALS, Advanced Life Support; B, BRAVO; BLS, Basic Life Support; C, CHARLIE; D, DELTA; E, ECHO.
The lowest-acuity patients in the dispatch protocols are categorized as (priority level) OMEGA. These OMEGA-level cases have been earmarked as the best candidates for secondary nurse triage since they represent the absolute safest conditions with very low risk of immediate or short-term life threatening pathologies; in other words, those patients who are least likely to need an ambulance and most likely to benefit from non-hospital care and treatment. The ALPHA-level sits just above the OMEGA-level in triage priority, representing a much larger subset of patients. Like OMEGA cases, ALPHA-level patients are presumed stable, but often have a more urgent or more resource-intensive treatment need than do OMEGA-level patients. While not true time-critical emergencies, ALPHA-level patients may benefit from Basic Life Support (BLS) ambulance crew assessment and treatment, as well as transport to the closest hospital emergency department. Also, there is a slight risk that an ALPHA-level patient has a more serious underlying condition than the initial EMD triage has identified, in which case the patient can deteriorate rapidly, becoming a true life-threatening emergency.
In a traditional tiered Emergency Medical Services (EMS) response system, any such rapid decline in patient status (eg, decreased level of consciousness, onset of difficulty breathing, or cardiac symptoms), should an ALPHA-level patient deteriorate, typically happens between the time the initial telephone triage is completed by the EMD and the time the dispatched ambulance crew arrives at the patient’s side. Therefore, the practice of dispatching BLS ambulances for ALPHA-level patients, in a timely manner, although generally in a non-lights-and-siren mode, has served as a safety net to catch any high-acuity or critical patients that are not discovered in the initial 911 triage process, since the arriving BLS ambulance crew can initiate rapid transport when necessary. Clearly, the introduction of a secondary nurse telephone triage process completed after EMD triage changes this paradigm, lengthening the dispatch time of a BLS ambulance, and potentially removing the buffer of the BLS ambulance response altogether (since many low-acuity calls presumably would be directed to non-ambulance care, extending the time for a medical professional to actually get eyes and hands on the patient).
So while it has been widely established that the vast majority of ALPHA-level patients are lower-acuity and not time-critical in nature,Reference Clawson, Cady, Martin and Sinclair 4 - Reference Stratton 8 assigning them for secondary nurse triage in the 911 center is a largely non-validated practice in North America. And a comprehensive body of outcome data, with a complete list of the codes most and least likely to carry a degree of risk, is still lacking.
It was hypothesized for this study that most of the proposed ALPHA-level codes would have little risk of high-acuity or critical status, and therefore, were suitable candidates for secondary 911 nurse triage.
Objectives
The primary objective of this study was to determine the clinical status of those ALPHA-level patients, as determined by on-scene EMS crews’ patient care records, in two US agencies. A secondary objective was to determine which ALPHA-level codes are suitable candidates for secondary nurse triage in the 911 center.
Methods
Study Setting and Design
The sites studied were two urban EMS systems in the United States. One site serves a total population of nearly 200,000 permanent residents, with a daytime population of over 300,000. The other serves a total population of just over 1,000,000.
Study Populations
Both study sites are currently ACEs with the IAED. Accredited centers are required to maintain and report monthly on protocol compliance, which must be consistently above 90%. This high compliance ensures that the dispatch protocol is in fact being studied as it is designed to be used, rather than a heterogeneous dispatch triage process with a high degree of non-compliance and haphazard subjectivity.
Study Protocol
One full year (2013) of all dispatch records, available at the time of the study, were collected from each dispatch center in electronic databases. During the study period, both dispatch centers used the ProQA software application (Salt Lake City, Utah USA) containing MPDS version 12.2, 2012 (IAED; Salt Lake City, Utah USA). All calls coded at the ALPHA-level were extracted from the dispatch dataset. The first recorded set of vital signs was retrieved from electronic patient care record (ePCR) forms completed by responders, including the hospital transport status.
Ethical Approval
This study was approved by the IAED Institutional Review Board.
Outcome Measure
The primary endpoint of this study was the percentage of low-acuity, ALPHA-level cases that had stable vital sign values. The secondary endpoint was the percentage of ALPHA-level cases that resulted in a lights-and-siren (high priority) EMS transport.
Data Management
The specific data element extracted from dispatch database was the (MPDS) determinant code for each call collected over the one year of the study period. The data elements extracted electronically from EMS responder run records were the first recorded measures for each of the following: pulse rate (PR), Glasgow Coma Score (GCS), systolic blood pressure (SBP), and pulse oximetry reading (SpO2). Any cases which had no vital signs data (ie, all elements missing) were excluded from the final study sample.
Each case the EMS crew transported “hot” (with lights-and-siren) to the hospital was also recorded by electronically extracting a specific data element from each run record. No chart review was done, nor necessary, in extracting the data elements required for this study. Therefore, abstractors were not used in this study because there was no evaluation and summarization of any information contained in the patient’s medical records, per se. The electronic data (a quantitative value in the case of vital signs, and a binary yes/no indicator in the case of a lights-and-siren transport) were simply extracted from respective electronic databases and used as a direct measure of outcome, based on the defined cut-off ranges for low, moderate, high, and critical vital sign values categories.
The respiratory rate was not used as an outcome measure of patient status for several reasons. First, respiratory rate is higher in infants and pediatric patients, and a link to age was not established to each specific patient record in one of the two systems studied. Also, recent studies suggest that respiratory rate as measured by clinicians often has low accuracy and high variability.Reference Garza, Gratton, McElroy, Lindholm and Glass 9 , Reference Philip, Pack, Cambiano, Rollmann, Weil and O’Bierne 10 While it is not a complete substitute for respiratory rate, the SpO2 has been shown to be a reasonably good surrogate for measuring adequacy of respiratory function.Reference Lovett, Buchwald, Sturmann and Bijur 11 This measure is independent of age, and it was readily accessible from the ePCR.
The hot (lights-and-siren) transport data were included as a way to demonstrate the field EMS crews’ subjective judgment of patient acuity, and they took into account factors such as patient history, medications, mechanism of injury, and other face-to-face observations that were not accounted for in the vital sign scale. Previous studies suggest the EMS crews’ decision to transport light-and-siren is predictive of high patient acuity when using transport protocols containing a combination of criteria, including the crews’ own judgment and experience.Reference Nitzan, Romem and Koppel 12 , Reference Kupas, Dula and Pino 13 The two EMS systems studied here used very similar criteria, but not an identical, standardized transport protocol.
Data Analysis
STATA for Windows software (STATA Statistical Software: Release 13.1, 2013, StataCorp; College Station, Texas USA) was used for data analysis. Frequencies, percentages, and median descriptive statistics were used to present study findings. Patient age was then classified into eight groups: < three months, three to 11 months, one to three years, four to five years, six to 15 years, 16-34 years, 35-64 years, and 65+ years, and descriptive statistics of each age group were presented. The nonparametric median test was used to assess if the medians of each vital sign were identical between study groups, at 0.05 significance level.
The vital sign measures were categorized into four groups: low, moderate, high, and critical (Table 1). This vital sign scale is a modification of the Hillrod Acute Process Triage system scaleReference Merlin, Baldino and Lehrfeld 14 that is widely used in Denmark and establishes abnormal vital signs as a strong predictor of acuity of adult patients triaged in the emergency department. The frequencies and percentages of each group were tabulated for each vital sign measure.
Table 1 Patient Vital Signs Acuity-level Scale Definitions

Abbreviations: GCS, Glasgow Coma Score; PR, pulse rate; SBP, systolic blood pressure; SpO2, oxygen saturation.
The median value for each vital sign measure was then compared overall. The percentage of high and critical acuity cases were presented for the top 10 most frequently used Chief Complaints and Determinant Codes for each vital sign measure, and then overall. Finally, the distribution of lights-and-siren transports was characterized for the top 10 most frequently used Determinant Codes and Determinant Codes that had at least one high or critical vital sign value with a frequency of 10 cases and above.
Results
A total of 19,300 ALPHA-level cases were analyzed, of which, 1,032 (5.3%) were transfers/interfacility/palliative care cases (ie, calls from a health care facility such as a hospital, nursing home, or other supervised clinical setting) and 1,505 (7.8%) cases had no vital signs value (in all the four vital signs measures) were excluded. The remaining 16,763 (86.9%) of the cases were included in the final analysis.
Overall, a majority 94.7% of the patients were 16 years and older, and a significant 74.8% were 35 years and older (Table 2). Patients less than three months old constituted approximately 0.43% of the cases. Additionally, all the vital signs values were within the normal ranges.
Table 2 Age Distribution and Patient Median Vital Signs Values for ALPHA-level Calls from All Emergency Dispatch 911 Calls during the Study Period

a Q1 and Q3 are the 25th and 75th percentiles, respectively.
A significant majority 97.8% had stable vital signs, or low or moderate values (97.8% for GCS, 97.6% for PR, 97.5% for SpO2, and 94.1% for SBP; Table 3). Overall, generally less than 0.5% of all the cases had critical vital signs (0.49% for SpO2, 0.47% for GCS, 0.36% for SBP, and 0.34% for PR).
Table 3 Percentage of Cases that had Low, Moderate, High, and Critical Vital Signs Measures

Abbreviation: SBP, systolic blood pressure.
Overall, the top 10 Chief Complaint Protocols included 94.6% of all the cases, consisting of 10.0% of cases that had at least one high vital sign (ie, 5.5% for SBP, 2.1% for PR, 2.1% for SpO2, and 1.8% for GCS; Table 4). And 0.97% of all the cases had at least one critical vital value (ie, 0.49% for SpO2, 0.47% for GCS, 0.36% for SBP, and 0.34% for PR).
Table 4 Percentage of a High and Critical Acuity Vital Sign Value for the Top 10 Most Frequently Used Chief Complaint Protocols (1-Abdominal Pain/Problems; 5-Back Pain; 12-Convulsions/Seizures; 13-Diabetic Problems; 17- Falls; 21-Hemorrhage/Lacerations; 25-Psychiatric/Abnormal Behavior/Suicide Attempt; 26-Sick Person; 30-Traumatic Injuries; 31-Unconscious/Fainting; Others-Other Determinants Combined.)

Abbreviations: GCS, Glasgow Coma Score; PR, pulse rate; SBP, systolic blood pressure; SpO2, oxygen saturation.
a Percentage of the top 10 chief complaints for the vital sign measure.
Overall, the top three Chief Complaints with the highest percentage of high vital sign values were: 19.6% for Protocol 12 (Convulsions/Seizures), 11.7% for Protocol 26 (Sick Person), and 11.4% for Protocol 13 (Diabetic Problems). The top three Chief Complaints with the highest percentage of a critical vital sign value were: 4.6% for Protocol 12 (Convulsions/Seizures), 2.0% for Protocol 31 (Unconscious/Fainting (Near)), and 2.0% for Protocol 13 (Diabetic Problems).
Specifically, Protocol 17 (Falls) had the greatest percentage of critical SBP and SpO2 values. The highest percentage of cases with a high (9.8%) and a critical (3.7%) GCS value, and high (8.3%) and critical (0.85%) PR values, were recorded in Protocol 12 (Convulsions/Seizures). However, Protocol 31 (Unconscious/Fainting (Near)) and Protocol 13 (Diabetic Problems) had the highest percentage of cases with critical (1.1%) and high (8.8%) SBP values, respectively.
The Chief Complaint Determinant Code 26-A-10, Sick Person- Unwell/Ill, had the highest overall percentage of high (14.4%) and critical (2.4%) vital sign measures, among the top 10 most frequently used Determinant Codes (Table 5). Generally, the same determinant code (26-A-10) had the highest percentage of cases with a high and/or critical vital sign value in a majority of vital sign measures.
Table 5 Percentage of a High and Critical Vital Sign Value for the Top 10 Most Frequently Used Determinant Codes (1-A-1, Abdominal Pain; 5-A-1, Non-traumatic Back Pain; 17-A-1, Not Dangerous Body Area Fall; 17-A-1-G, Not Dangerous Body Area Fall, on the Ground or Floor; 25-A-1, Non-suicidal and Alert Psychiatric/Abnormal Behavior Case; 26-A-1, Sick Person-Blood Pressure Abnormality; 26-A-5, Sick Person-General Weakness; 26-A-8, Sick Person-Other Pain; 26-A-10, Sick Person-Unwell/Ill; 26-A-11, Sick Person-Vomiting.)

Abbreviations: GCS, Glasgow Coma Score; PR, pulse rate; SBP, systolic blood pressure; SpO2, oxygen saturation.
a Percentage of the top 10 determinants for the vital sign measure.
Otherwise, Protocol 26-A-5 (Sick Person-General Weakness) had the highest percentage of critical category (1.3%) SpO2 value. Protocol 26-A-11 (Sick Person-Vomiting) had the highest percentage of a high category (8.6%) SBP value.
Approximately 1.1% of all cases were transported lights-and-siren, overall (Table 6). The Determinant Codes that had the top three highest percentage of lights-and-siren transports, among the top 10 most frequently used Determinants, were: 26-A-11, Sick Person-Vomiting, (1.7%); 17-A-1-G, Not Dangerous Body Area Fall-on the Ground or Floor, (1.5%); and 26-A-10, Sick Person-Unwell/Ill, (1.2%).
Table 6 The Percentage of Lights-and-siren Transports for the Top 10 Most Frequently Used Determinant Codes by Acuity Level (1-A-1, Abdominal Pain; 5-A-1, Non-traumatic Back Pain; 17-A-1, Not Dangerous Body Area Fall; 17-A-1-G, Not Dangerous Body Area Fall-on the Ground or Floor; 25-A-1, Non-suicidal and Alert Psychiatric/Abnormal Behavior Case; 26-A-1, Blood Pressure Abnormality; 26-A-5, Sick Person-General Weakness; 26-A-8, Sick Person-Other Pain; 26-A-10, Sick Person-Unwell/Ill; 26-A-11, Sick Person-Vomiting.)

Abbreviation: L&S, lights and siren.
a An overlap of cases may occur among the high and critical vital sign values since a case may have one or more vital sign measures with a high or critical value. This effect may explain the differences in sample sizes presented in subsequent tables.
b Percentage of cases for the top 10 most frequently used determinant codes by acuity level.
Determinant Codes 26-A-5, Sick Person-General Weakness, 26-A-11, Sick Person-Vomiting, and 17-A-1-G, Not Dangerous Body Area Fall-on the Ground or Floor, had the highest top three percentage of lights-and-siren transports (4.6%, 4.3%, and 4.0%, respectively) for cases that had a high vital sign value. Otherwise, the Determinants that had the top three highest percentage of lights-and-siren transports for cases that had a critical vital sign value were: 17-A-1-G, Not Dangerous Body Area Fall-on the Ground or Floor, (33.3%); 26-A-11, Sick Person-Vomiting, (22.2%); and 25-A-1, Non-suicidal and Alert Psychiatric/Abnormal Behavior Case, (14.3%).
Overall, 11.1% of all Determinant Codes had at least one high or critical vital sign value (Table 7). Specifically, the top five Determinant Codes with the highest percentage of at least one high or critical vital sign were: 12-A-3, Convulsions/Seizures-Not Seizing Now and Effective Breathing Verified (≤6, Confirmed No Seizure Disorder), (54.5%); 26-A-2, Sick Person-Blood Pressure Abnormality (Asymptomatic), (33.5%); 26-A-4, Sick Person-Fever, Chills, (24.1%); 12-A-1, Convulsions/Seizures-Not Seizing Now and Effective Breathing Verified (Known Seizure Disorder), (23.6%); and 12-A-1-E, Convulsions/Seizures-Not Seizing Now and Effective Breathing Verified (Known Seizure Disorder)-Epileptic or Previous Seizure Diagnosis, (22.2%).
Table 7 Percentage and Lights-and-Siren Transport Status of the Determinant Codes that had One or More High or Critical Vital Sign Values, and a Frequency of 10 Cases and Above
Abbreviation: L&S, lights and siren.
a Percentage of cases that had at least one high or critical vital signs value from all cases per determinant code.
b Percentage of Lights-and-Siren for cases that had one or more high and/or critical value.
1-A-1 Abdominal Pain
5-A-1 Non-traumatic Back Pain
10-A-1 Chest Pain-Breathing Normally <35
12-A-1 Convulsions/Seizures-Not Seizing Now and Effective Breathing Verified (Known Seizure Disorder)
12-A-1-E Convulsions/Seizures- Not Seizing Now and Effective Breathing Verified (Known Seizure Disorder)-Epileptic or Previous Seizure Diagnosis
12-A-2 Convulsions/Seizures- Not Seizing Now and Effective Breathing Verified (Seizure Disorder Unknown)
12-A-3 Convulsions/Seizures- Not Seizing Now and Effective Breathing Verified (≤6, Confirmed No Seizure Disorder)
13-A-1 Diabetic Problems-Alert and Behaving Normally
17-A-1 Not Dangerous Body Area Fall
17-A-1-G Not Dangerous Body Area Fall, on the Ground or Floor
17-A-2 Falls-Non-recent (≥6 hours) Injuries (without Priority Symptoms)
17-A-3 Falls-Public Assist (No Injuries and No Priority Symptoms)
17-A-3-G Falls-Public Assist (No Injuries and No Priority Symptoms)- On the Ground or Floor
19-A-1 Heart Problems/A.I.C.D, HR≥50 bpm and <130 bpm
21-A-1 Hemorrhage/Lacerations-Not Dangerous
25-A-1 Non-suicidal and Alert Psychiatric/Abnormal Behavior Case
26-A-1 Sick Person-No Priority Symptoms
26-A-10 Sick Person-Unwell/Ill
26-A-11 Sick Person-Vomiting
26-A-2 Sick Person-Blood Pressure Abnormality (Asymptomatic)
26-A-3 Sick Person-Dizziness/Vertigo
26-A-4 Sick Person-Fever, Chills
26-A-5 Sick Person-General Weakness
26-A-6 Sick Person-Nausea
26-A-7 Sick Person-New Onset of Immobility
26-A-8 Sick Person-Other Pain
30-A-1 Traumatic Injuries-Not Dangerous Body Area
30-A-2 Traumatic Injuries-Non-recent (≥6 hours) Injuries without Priority Symptoms)
31-A-1 Unconscious/Fainting (Near)-Fainting Episode(s) and Alert ≥35 (without Cardiac History)
31-A-2 Unconscious/Fainting (Near)-Fainting Episode(s) and Alert <35 (with Cardiac History)
31-A-3 Unconscious/Fainting (Near)-Fainting Episode(s) and Alert <35 (without Cardiac History)
Approximately 4.3% of all the cases that had a high/critical vital sign value were transported lights-and-siren to the hospital. Among the same group, determinant codes that had the highest top five percentage of lights-and-siren transports were: 19-A-1, Heart Problems/A.I.C.D, HR ≥50 bpm and <130 bpm, (14.3%); 12-A-2, Convulsions/Seizures-Not Seizing Now and Effective Breathing Verified (Seizure Disorder Unknown), (12.5%); 12-A-1, Convulsions/Seizures-Not Seizing Now and Effective Breathing Verified (Known Seizure Disorder), (12.2%); 10-A-1, Chest Pain-Breathing Normally <35, (11.8%); 31-A-2, Unconscious/Fainting (Near)-Fainting Episode(s) and Alert <35 (with Cardiac History), (9.1%); and 21-A-1, Hemorrhage/Lacerations-Possibly Dangerous, (9.1%). Additionally, the high/critical group had an overall 4.3% lights-and-siren transport rate. Determinant Codes 17-A-3, Falls-Public Assist (No Injuries and No Priority Symptoms), 30-A-2, Traumatic Injuries-Non-recent (≥6 hours) Injuries without Priority Symptoms), and 31-A-3, Unconscious/Fainting (Near -Fainting Episode(s)) and Alert <35 (without Cardiac History) had no lights-and-siren transports.
Otherwise, Determinants 12-A-3 Convulsions/Seizures-Not Seizing Now and Effective Breathing Verified (≤6, Confirmed No Seizure Disorder), 12-A-1-E, Convulsions/Seizures-Not Seizing Now and Effective Breathing Verified (Known Seizure Disorder)-Epileptic or Previous Seizure Diagnosis, 19-A-1, Heart Problems/A.I.C.D, HR ≥50 bpm and <130 bpm, 12-A-1, Convulsions/Seizures-Not Seizing Now and Effective Breathing Verified (Known Seizure Disorder), and 26-A-4, Sick Person-Fever, Chills, had the top five highest percentage of cases that had a critical vital sign value (10.1%, 3.6%, 3.1%, 2.9%, and 2.8%, respectively).
Discussion
The MPDS ALPHA-level dispatch priority comprises a wide spectrum of conditions and symptoms that can range from minor injuries such as ground-level falls or low-force trauma, to chronic pain, nausea, vomiting, colds and flu, mild allergic reactions, high or low blood sugar in an asymptomatic diabetic, a post-seizure patient who’s breathing is returning to normal but may not yet be completely alert, post-syncope, vertigo, and general weakness, to name just a few. Clearly, not all patients experiencing these conditions and/or symptoms will always have a complete set of vital signs within the range considered “normal,” even when their baseline condition is stable. Hence, it was expected that some ALPHA-level patients would have at least one recorded vital sign in the moderate-acuity category on the scale, as defined in Table 1.
What is of greater concern are those patients who appear in the high and critical categories, as well as those that were transported “hot.” While it is true that one high-acuity vital sign does not necessarily make for an unstable patient, if ALPHA-level patients are expected to be good candidates for secondary triage and non-ambulance care, the incidence of patients in these upper two categories must be very low, as must the number of patients transported hot (using lights-and-siren).
The results in this study support the view that a large majority of ALPHA-level patients are stable and low-risk, making them good candidates for secondary nurse triage. Just over 89% of all ALPHA-level cases did not have even one high or critical vital sign value. And over one-half of the occurrences of high vital signs were for blood pressure abnormalities – most often high blood pressure. Given the widespread occurrence of hypertension in the US population (32.5% for adults age 20 and over),Reference Barford, Lauritzen and Danker 15 it is likely that many patients with this single high-acuity indicator would still be candidates for non-ambulance care, if otherwise asymptomatic. The above population statistic also explains the relatively high percentage of high-acuity indicators in the 26-A-2, Sick Person-Blood Pressure Abnormality (Asymptomatic), determinant code.
Yet, a few truly unstable patients do exist in the ALPHA-level. And given this finding, the possibility must be considered that any delay while performing the secondary nurse triage, or removing the ambulance response altogether for time-delayed care at an alternative venue, poses a risk to those few patients. On the other hand, there may be a benefit to secondary nurse triage for these at-risk, ALPHA-level patients if the ECN is able to identify those few critical and high acuity patients consistently (and re-triage them to a higher determinant code level), thus triggering a more rapid, higher level, EMS response than would otherwise have been assigned by the EMD without further ECN evaluation.
The seizure codes 12-A-1, Convulsions/Seizures-Not Seizing Now and Effective Breathing Verified (Known Seizure Disorder), and 12-A-1-E, Convulsions/Seizures-Not Seizing Now and Effective Breathing Verified (Known Seizure Disorder)-Epileptic or Previous Seizure Diagnosis, 12-A-2, Convulsions/Seizures-Not Seizing Now and Effective Breathing Verified (Seizure Disorder Unknown), and 12-A-3, Convulsions/Seizures-Not Seizing Now and Effective Breathing Verified (≤6, Confirmed No Seizure Disorder), appear to be problematic for transfer to ECNS since they all had a relatively high percentage of high/critical vital signs and “hot” (lights-and-siren) transports. In fact, unpublished data from the UK on these codes showed the secondary nurse triage return rate for ambulance response on these codes as: 12-A-3, Convulsions/Seizures-Not Seizing Now and Effective Breathing Verified (≤6, Confirmed No Seizure Disorder), (28%); 12-A-2, Convulsions/Seizures-Not Seizing Now and Effective Breathing Verified (Seizure Disorder Unknown), (22%); and 12-A-1, Convulsions/Seizures-Not Seizing Now and Effective Breathing Verified (Known Seizure Disorder), (11%), which are similar to the findings in this study in Table 7. These patients have lower GCS scores, most likely because many of them are in a post-ictal state and not completely alert at the time the initial 911 call was made. A not-alert patient is inherently more difficult to triage beyond the point of obtaining a simple description of the patient’s primary signs and symptoms since they are often not able to provide the detailed patient and event information that is necessary for a comprehensive secondary triage process. And adult-onset seizures (particularly first-time, with no apparent provocation) may simply be too complex to manage by telephone triage alone. 16 , Reference Clawson 17
Protocol 26 (Sick Person) ALPHA-levels also present a challenge to a system looking to utilize secondary triage. Emergency Medical Dispatchers are trained to select the Protocol 26 (Sick Person) when (in their initial chief complaint query) they have not been able to identify a “priority symptom” (ie, breathing problems, chest pain, altered level of consciousness, and severe hemorrhage), or another more specific condition such as back pain, a mechanism of injury such as a fall or traffic accident, or another hazardous circumstance such as an overdose, burn, or chemical exposure. Protocol 26, therefore, can be viewed as a collection of conditions, symptoms, and signs that, on the surface, do not pose an immediate risk to the patient. Again however, these data demonstrate that there are a few outliers. Also, unpublished data collected in 2004 from an accredited center using a (now-outdated) previous version of the MPDS, had documented some potential at-risk, ALPHA-level patients residing within the Protocol 26 (Sick Person) determinant codes, particularly with identifying those patients that are completely alert.Reference Krumholz, Wiebe and Gronseth 18 Since then, the “completely alert” condition was clarified further in a more recent version of the MPDS by adding a CHARLIE-level determinant code for any patient described initially as being in a state considered less than completely alert, even when the caller does not explicitly indicate “not alert.” While use of this CHARLIE-level determinant code largely has resolved the issue of under-triaging patients with potentially altered states of consciousness, the original finding of these “less than alert” patients in Protocol 26 (Sick Person) ALPHA-level code serves as a cautionary note, as attempts continue to further refine the practice of assigning ALPHA-level codes, particularly within Protocol 26 (Sick Person).
So, is it possible for secondary nurse triage to identify, consistently and accurately, those few ALPHA-level patients that are more serious than the initial EMD triage determines, particularly for the high-frequency, ALPHA-level codes in Protocol 26 (Sick Person)? Additional studies are needed to answer this question. One recent study done in two emergency communication centers (not the two centers studied here), where pilot ECNS programs have been implemented, reported that 3.0% and 4.2% (respectively) of all cases (a mix of ALPHA-level and OMEGA-level; approximately 70% ALPHA-level calls) given to the ECN for triage subsequently were returned to the ambulance response system as a higher priority code (above ALPHA-level).Reference Clawson 19 This finding provides some evidence that the most suspect ALPHA-level patients are getting re-triaged to a higher level, possibly from the same or similar patient group that appeared in the high and critical categories. Future studies should evaluate, in detail, the efficacy of a secondary nurse triage program within the 911 center.
Limitations
A major limitation is the lack of corresponding hospital outcome data for the cases studied here. While prehospital vital signs recorded by the ambulance crew and ambulance transport (hot or cold) data tell a great deal about the status of the patient, a greater understanding of the actual patient treatment need could have been gained – both the urgency and level of care required – by knowing the treatment provided and final discharge (or admission) diagnosis from the hospital, which could provide a more granular view of how well certain patients would fare without an ambulance transport to the hospital. Another limitation was the inability to link certain elements of the ePCR to the dispatch case record (from the emergency communication center) in one of the two systems studied. Since age was one of those elements, age data could only be gathered in the aggregate for most of the records.
The vital sign measurements collected by paramedics and Emergency Medical Technicians (EMTs) are subject to the standard degree of variation with this professional group, and because this was a retrospective study, there was no way to scientifically validate their accuracy. It was verified that all these measurements were completed by trained, and currently certified, paramedics and/or EMTs using standard measurement methods and equipment. The lights-and-siren transport is generally a subjective decision based on paramedic/EMT impression; hence, there was no single, standard, transport protocol applied.Reference Nitzan, Romem and Koppel 12 , Reference Kupas, Dula and Pino 13
Conclusion
The vast majority of cases coded as ALPHA-level calls did not have a single vital sign indicator of unstable status (high or critical), and demonstrated a very low incidence of a high-priority (lights-and-siren) EMS transport. With the exception of the ALPHA-level seizure cases, the results in this study support the feasibility of using MPDS ALPHA codes as clinically sound criteria to initiate secondary nurse triage at 911 for systems that utilize the dispatch protocol at high compliance rates. However, a secondary nurse triage system must be sensitive enough to identify the few at-risk patients that exist in the ALPHA-level, particularly those categorized as “Sick Person” by the EMD, when serious underlying medical conditions are present and are not identified in a standard MPDS interrogation.
Acknowledgements
The authors thank Brandee Rowley, IAED Administrative Assistant, for logistics management, formatting, and proofing the manuscript.