Introduction
Tetanus is a potentially fatal condition, but the introduction of the tetanus toxoid vaccine tremendously decreased its incidence in the developed world.Reference Finkelstein, Teisch, Allen and Ruiz 1 In developing and poor countries where vaccination rates can be low, tetanus is still a substantial public health concern. 2 When natural disasters strike, the incidence increases despite the under-reporting of cases from local hospitals.Reference Taylor 3
Tetanus is a non-communicable disease caused by Clostridium tetani (C. tetani) bacillus.Reference Finkelstein, Teisch, Allen and Ruiz 1 , 2 C. tetani usually enters through puncture wounds or wounds with significant tissue injury; rarer ways to contract tetanus include scrapes, surgical procedures, insect bites, and intravenous/IV drug use.Reference Afshar, Raju, Ansell and Bleck 4 However, in 20% of cases, no obvious entry wound is identified. 5
Natural disasters, like earthquakes for instance, create the perfect environment for the outbreak of the diseaseReference Cook, Protheroe and Handel 6 that typical urban physicians may lack experience treating. The combination of absent infrastructure and medical supplies with severe soft tissue trauma cases may be responsible for the outbreaks seen in certain countries.Reference Taylor 3 Trauma puncture wounds are likely to promote germination of the microorganism due to their low oxygen microenvironment in which C. tetani thrives.Reference Finkelstein, Teisch, Allen and Ruiz 1
Globalization has facilitated the ability of physicians from resource-rich countries to be brought to areas in need after a disaster. Thus, despite the low incidence of tetanus in the developed world, clinical awareness of tetanus, its prophylaxis, clinical manifestations, and treatment are important, especially when the potential of an outbreak in the setting of natural disaster is very high. Therefore, the purpose of this report was to provide a review of the epidemiology, pathogenesis, and management of tetanus in the trauma patient.
Methods
A thorough literature review was conducted to look for the most current and thorough guidelines on the prophylaxis and treatment of tetanus. PUBMED (National Center for Biotechnology Information, National Institutes of Health; Bethesda, Maryland USA), MEDLINE (US National Library of Medicine, National Institutes of Health; Bethesda, Maryland USA), and Cochrane Library (The Cochrane Collaboration; Oxford, United Kingdom) databases were searched for articles in English, published from 2005 to 2015, using the keywords “Tetanus,” “Trauma/Surgery,” and “Disaster.” Controlled trials, randomized controlled trials, trials of adult patients, published guidelines, expert opinions, and review articles were selected and extracted.
Epidemiology
Globally, most cases of tetanus take place in developing countries where immunity is rarer, and furthermore, where tetanus incidence increases after natural disasters.Reference Taylor 3
Tetanus is categorized into three forms: generalized/neonatal, local, and cephalic.Reference Kouadio, Aljunid, Kamigaki, Hammad and Oshitani 7 Generalized tetanus is the most common type of tetanus (80% of reported cases),Reference Kouadio, Aljunid, Kamigaki, Hammad and Oshitani 7 whereas neonatal tetanus is generalized tetanus in children less than one month old. 8 Worldwide, deaths due to neonatal tetanus have decreased in incidence from 490,000 in 1994 to 49,000 in 2013. 8 In 1999, the Maternal and Neonatal Tetanus Elimination Initiative was established to eliminate maternal and neonatal tetanus as a public health concern,Reference Vandelaer, Raza, Zulu, Yakubu and Khan 9 and since 1999, 35 of 59 priority countries have eliminated maternal and neonatal tetanus. 8 Local tetanus is uncommon, and only one percent results in death.Reference Finkelstein, Teisch, Allen and Ruiz 1 Finally, cephalic tetanus is characterized by cranial nerve palsies and high mortality rates of approximately 15%-30% as it progresses to generalized tetanus. 10
In 2015, the World Health Organization (Geneva, Switzerland) reported a total of 13,532 cases of tetanus worldwide,Reference Jagoda, Riggio and Burguieres 11 but the global incidence has been estimated to be as high as one million cases annually. 2 The mortality rates of tetanus vary based on barriers to care; 12 with care, the tetanus toxoid series has a clinical efficacy of almost 100%.Reference Finkelstein, Teisch, Allen and Ruiz 1 Herd immunity does not play a role in protecting members of a population against tetanus, so almost all people should be vaccinated to garner protection.Reference Roper, Vandelaer, Çois and Gasse 13
Pathogenesis
C. tetani is spore-forming, obligate anerobe which releases two toxins: tetanospasmin and tetanolysin.Reference Finkelstein, Teisch, Allen and Ruiz 1 C. tetani spores are typically found in soil and feces and are highly resistant to heat and common disinfectants.Reference Finkelstein, Teisch, Allen and Ruiz 1
Tetanospasmin is a neurotoxin which induces the classic muscle spasms seen in tetanus by inhibiting the release of γ-amino-butyric acid (GABA) and glycine in the central nervous system. 5 Tetanospasmin itself, however, is an inactive peptide that needs enzymatic cleavage prior to initiating inhibition. 5 Upon activation, tetanospasmin is split into two chains. The heavy chain travels in a retrograde fashion into the central nervous system.Reference Paul 14 - Reference Edlich 16 Once within the spinal cord and brainstem, tetanospasmin cleaves synaptobrevin (VAMP), which inhibits GABA, and glycine release.Reference Farrar, Yen and Cook 17 , Reference Linnenbrink and McMichael 18 Both glycine and GABA act as skeletal muscle inhibitors; therefore, upon blockade, clinical muscle spasms are seen.Reference Edlich 16 , Reference González-Forero, Morcuende, Alvarez, de la Cruz and Pastor 19 - Reference Humeau, Doussau, Gran and Poulain 21
Tetanolysin and its exact function in the pathophysiology of tetanus remains not well understood.Reference Montecucco and Schiavo 22
The incubation period for tetanus ranges from four days to 14 days.Reference Bleck 23 The further the initial wound is from the central nervous system, the longer the incubation period.Reference Hinfey 24 Often, the initial symptom is local tetanus manifested by rigidity in the original wound area of the body.Reference Bleck 23 Generalized tetanus presents with trismus, stiffness, neck rigidity, restlessness, and reflex spasms. Reflex spasms can occur with minimal external stimuli and increase in frequency with disease progression. Muscle rigidity is spread in a descending pattern throughout the next 24-48 hours, and other extra-muscular symptoms including fever, sweating, hypertension, and elevated heart rate may appear.Reference Bleck 23 The clinical triad of tetanus is often denoted as muscle rigidity, spasms, and autonomic dysfunction. 25 Table 1 shows the Ablett Classification of Severity for tetanus.
Table 1 Ablett Classification of Severity

Management
Immunizations
Four combination vaccines are used to prevent tetanus: diphtheria, tetanus toxoid, and pertussis (DTaP); tetanus toxoid, reduced dose of diphtheria, and reduced dose of pertussis (Tdap); diphtheria and tetanus toxoid (DT); and tetanus toxoid and reduced dose of diphtheria (Td). Table 2 shows the recommended age schedule of the various tetanus vaccines.Reference Quasim 26 - 28
Table 2 Recommended Guidelines for Tetanus Vaccines

Abbreviations: DTaP, diphtheria, tetanus toxoid, and pertussis; Td, tetanus toxoid and reduced dose of diphtheria; Tdap, tetanus toxoid, reduced dose of diphtheria, and reduced dose of pertussis.
DTaP and DT are given to children under the age of seven,Reference Kouadio, Aljunid, Kamigaki, Hammad and Oshitani 7 whereas Tdap and Td are given to those over the age of seven.Reference Kouadio, Aljunid, Kamigaki, Hammad and Oshitani 7 DTaP should be given at the following ages: two months, four months, six months, 15-18 months, and four to six years old.Reference Quasim 26 , 29 DT can be given for those who cannot tolerate the pertussis portion of DTaP.Reference Quasim 26 , 29 Td is given as a booster shot every 10 years, or after an exposure to tetanus, and Tdap should be given as a single dose to adults over the age of 19. 27 , 29 Women should receive Tdap during each pregnancy, 28 , 29 and Tdap can be given regardless of when the last dose of Td was given. 29
Vaccinations generally have limited side effects and include fever, redness or swelling and soreness at injection site, and generalized body aches and tiredness. These are less common with the acellular DTaP vaccine.Reference Hinfey 24
Medical and Surgical
Initially, the main goal of tetanus treatment is to prevent further toxin release in the central nervous system. 25 This can be done with wide surgical debridement of the wound and antibiotic treatment. Metronidazole is generally the antibiotic of choice and is preferred over penicillin, which not only has lower tissue penetration, but also displays GABA-antagonistic activity that may potentiate the effects of the neurotoxin tetanospasmin. 25 Other acceptable antibiotic choices include erythromycin, tetracycline, chloramphenicol, and clindamycin.Reference Kouadio, Aljunid, Kamigaki, Hammad and Oshitani 7 , 25
The second goal of treatment is to neutralize the toxin present in the body, but outside the central nervous system, with human tetanus immune globulin (TIG). This should be done within 24 hours of diagnosis; if human TIG is unavailable, anti-tetanus horse serum can be given.Reference Kouadio, Aljunid, Kamigaki, Hammad and Oshitani 7 , 25 Figure 1 shows current guidelines as to the medical treatment of tetanus based on wound type. 30 If the wound is clean, and the patient is up to date with the tetanus diphtheria series with their most recent dose in the past 10 years, no vaccine is needed. If the wound is clean, and the patient’s vaccination status is unknown or if the patient is up to date with the tetanus diphtheria series and their most recent dose was not given in the past 10 years, the vaccine should be given at time of presentation with injury. If the wound is dirty, and the patient has completed a primary tetanus diphtheria series but has not had a recent dose in the past five years, the vaccine should be administered at time of presentation. If the wound is dirty, the patient has completed a primary tetanus diphtheria series, and has had a recent dose in the past five years, the vaccine is not needed at time of presentation. If, however, the wound is dirty and the patient’s primary tetanus diphtheria series is incomplete or vaccination status is unknown, both the vaccine and TIG should be administered. 30
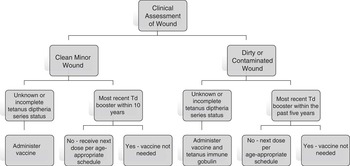
Figure 1 Algorithm for Tetanus Prophylaxis in Wound Management. Abbreviation: Td, tetanus toxoid and reduced dose of diphtheria.
The third goal of treatment is to minimize the effects due to the toxin affecting the central nervous system. This can be done through sedation, respiratory support, and autonomic control as needed.Reference Kouadio, Aljunid, Kamigaki, Hammad and Oshitani 7 Large doses of benzodiazepines are often used to help control muscle spasms. 31
Tetanus Outbreaks During Natural Disasters
Infections are common after large-scale natural disasters such as earthquakes. Most outbreaks, however, occur in places where tetanus is common due to low vaccination rates. After the 2010 earthquake in Haiti, there was increased tetanus compared to their baseline incidence even with the potential of significant under-reporting.Reference Rodrigo, Fernando and Rajapakse 32
The mortality of tetanus after a severe natural disaster ranges from 19%-31%. 33 Hospital type and distance to medical care are significant predictors of mortality in these settings. Lack of resources (ie, surgical care, intensive care, and mechanical ventilatory support) significantly increases tetanus mortality in the field after severe natural disasters. 34
When severe natural disasters occur, many patients may not be able to provide a reliable vaccination history. As mentioned in the treatment section, in these situations, TIG is indicated. If resources are not limited, both tetanus toxoid and TIG should be given to those with high-risk wounds. If resources are limited, TIG should be reserved for those that would most benefit or those least likely to have the protective antibodies (ie, those greater than 60 years of age, women, and immigrants of other regions other than North America or Europe).Reference Trujillo, Castillo, España, Manzo and Zerpa 35
Conclusion
Although tetanus is a disease that has a low incidence in the developed world due to high rates of immunization, during large-scale natural disasters, compounding factors like the type of injuries, the lack of medical services and supplies, and the delay in treatment associated to already low immunity in non-developed society result in an increased incidence and outbreaks of the disease that has higher mortality. Thus, it is necessary that the urban physician that cares for trauma patients becomes familiar with the protocols for treatment and immunization of patients that have tetanus-prone wounds, as well as recognizes the risk of outbreaks in the setting of natural disasters.





