Introduction
Up to 40 patients per million inhabitants per year suffer from severe spinal cord trauma with paraplegia. The most affected are young men between the ages of 15 and 30 years old.Reference Sekhon and Fehlings1 The main areas for spinal cord injuries are the lower cervical spine and the upper and middle thoracic spine.Reference FH and MV2 More than 66% of cervical spine injuries are accompanied by neurological disorders. In contrast, only approximately 20% of injuries of the thoracic and lumbar spine are accompanied by neurological disorders. Injuries to the spine and spinal cord are a great burden for patients and society.Reference Bernhard, Gries, Kremer and Bottiger3
Immediate immobilization of the cervical spine by professional emergency care providers is a standard procedure performed world-wide.Reference Sundstrom, Asbjornsen, Habiba, Sunde and Wester4 In most Western Emergency Medical Services (EMS), various immobilization tools are available. Recent literature also reports on the complications associated with the different techniques of spinal immobilization.Reference Davies, Deakin and Wilson5-Reference Liao, Schneider and Huttlin13 At the very least, immobilization of the spine is said to increase the mortality rate of patients in special cases.Reference Haut, Kalish and Efron14 Otherwise, prehospital immobilization of the cervical spine is recommended by several established treatment guidelines,15-Reference Kornhall, Jorgensen and Brommeland17 even if there is no agreement on a preferred immobilization technique.15,Reference Theodore, Hadley and Aarabi16,18-20 Thus, the EMS provider is almost left alone with the decision of the best immobilization technique. The literature on the quality of the different immobilization techniques is sparse and mostly outdated concerning the immobilization tools and the methods of analysis.
This study aimed to analyze the residual cervical spine movement under different types of external cervical spine immobilization.
Methods
Study Design
This study uses biomechanical data measured using various techniques to immobilize the cervical spine in a standardized environment. The subjects participated voluntarily and agreed in writing that all collected photographs, videos, and biomechanical data could be used in this study. Approval by the Ethics Committee of the State Medical Association of the Rhineland-Palatinate, Germany (ID 837.508.15) was obtained. The study is registered in the German Clinical Trials Register (German Institute of Medical Documentation and Information; Cologne, Germany) with the ID DRKS00009505.
Study Participants
All three test persons (TPs) had a normal body shape and a normal body-mass-index (18.5 to 25.0kg/m2). The TPs medical histories did not include spinal injuries or spinal diseases. More details about the TPs are given in Table 1.
Table 1. Information on the Test Persons (TPs)

Cervical Spine Movement Measurement
The primary endpoints were the remaining range of motion for flexion, extension, lateral bending, and rotation on both sides under correct immobilization. The healthy TP was in the supine position, while experienced EMS staff performed the immobilization techniques described below.
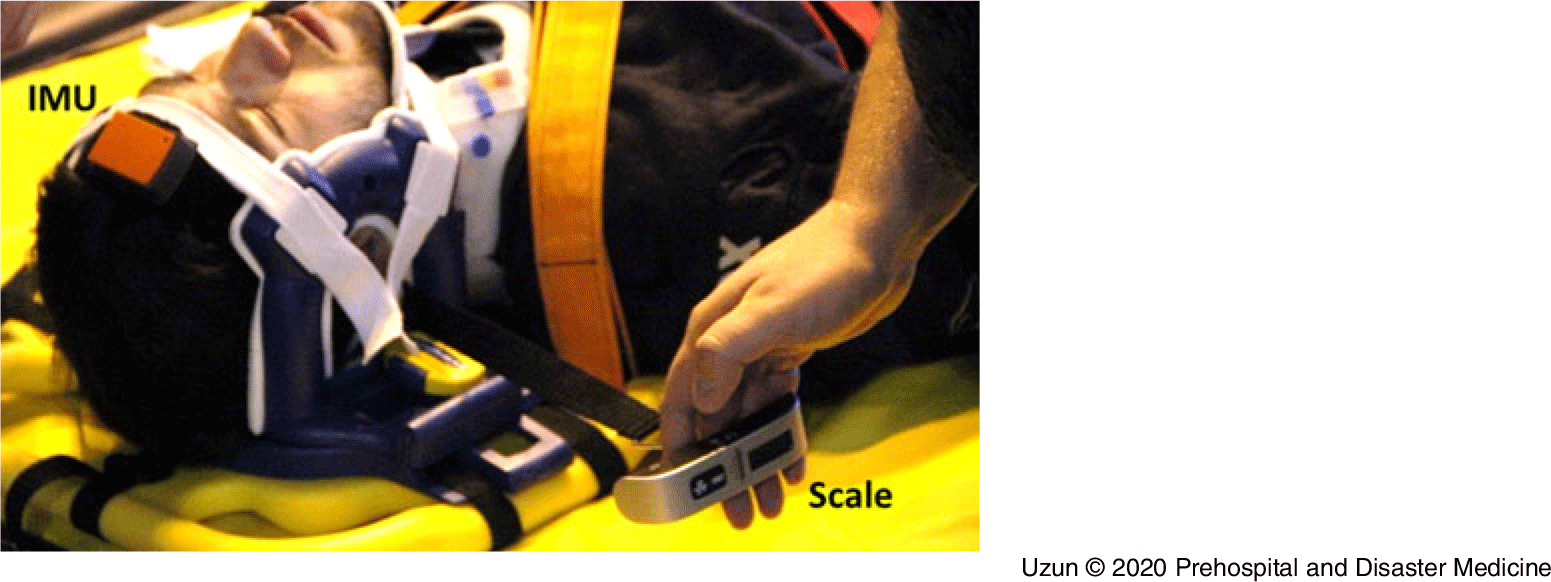
Next, the head of the TP was passively moved to cause: (1) rotation of the cervical spine to the right and left side; as well as (2) flexion and extension of the cervical spine. Controlled by a mobile luggage scale (Lina 79416, KORONA; Sundern, Germany) that was attached to the TP’s head, the effective weight force used to move the TP’s cervical spine was standardized in all test runs (Figure 1). The head was moved up within two seconds to an effective weight force of around 100 Newton (10kg on the scale), that is within the same range of force measured on the cervical spine during intubation proceduresReference Hindman, Santoni, Puttlitz, From and Todd21 and that might affect the spinal canal in case of severe cervical spine injury.Reference Liao, Schneider and Weilbacher22
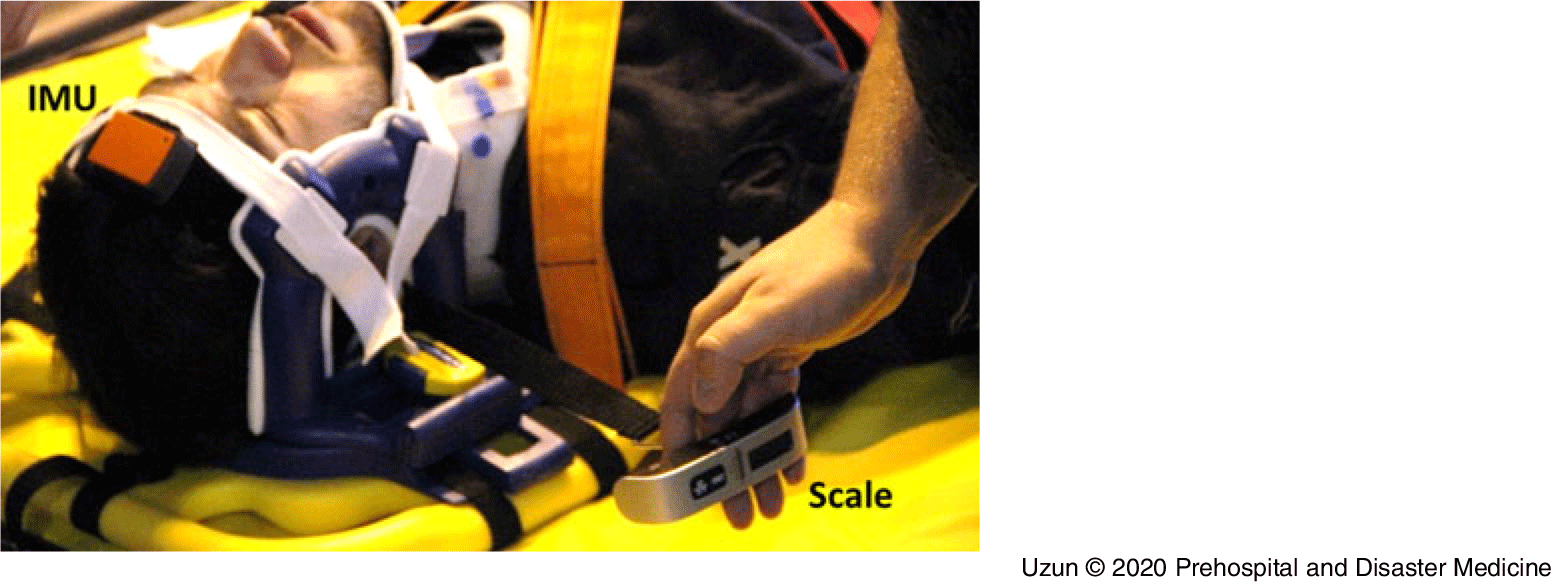
Figure 1. Measurement of Cervical Spine Movement.
A wireless human motion tracker (Xsens Technologies; Enschede, Netherlands) was used to collect biomechanical data on the movement of the cervical spine. Two inertial measurement units (IMUs) were used to record the 3D motion. The IMUs were positioned exactly opposite each other on the forehead and sternum, and the data were synchronized with the Xsens recording tool every 10 microseconds.
The maximum movement (in degrees) in terms of extension, flexion, rotation, and transverse flexion during passive cervical spine movement was analyzed.
Different Immobilization Techniques
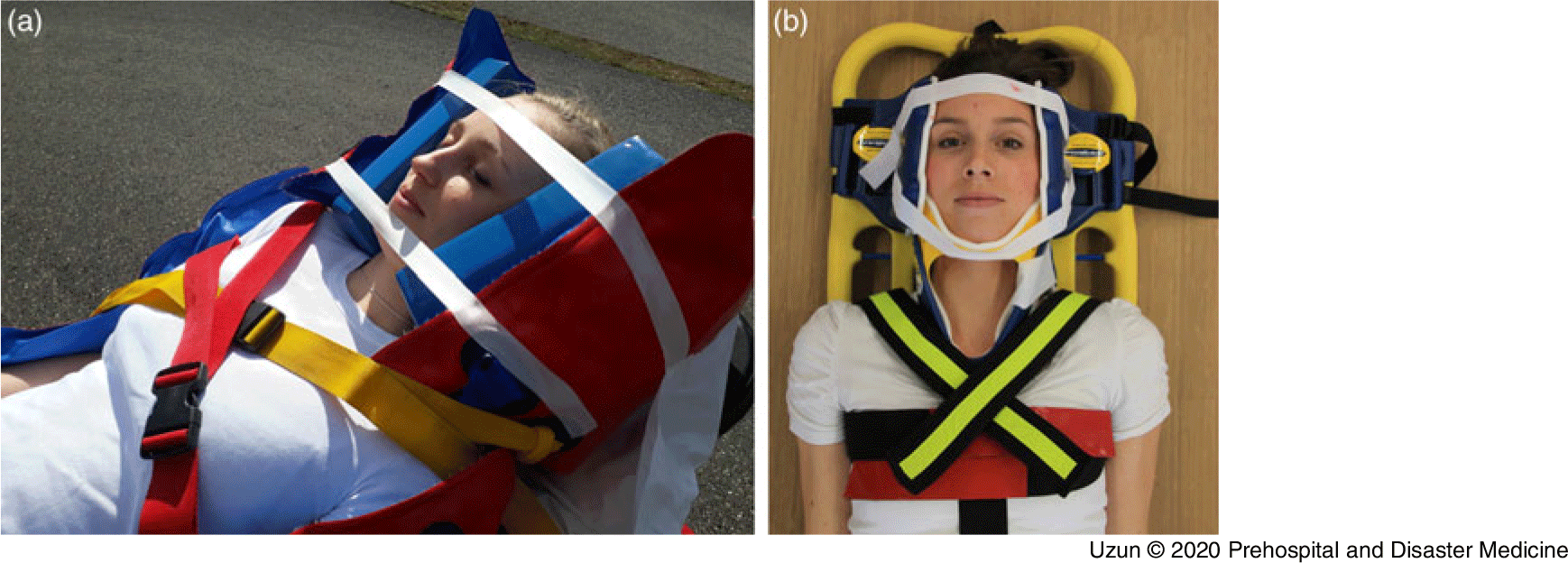
Vacuum Mattress—The immobilization of the cervical spine was performed by placing the TP in the supine position on a straight (0°) vacuum mattress (RedVac 200cm, Kohlbrat & Bunz; Radstadt, Austria). The vacuum mattress was modulated onto the body of the TP. Afterwards, the vacuum mattress was evacuated. This immobilization technique was performed with and without an additional cervical collar. Furthermore, this immobilization technique was performed with and without additional fixation of the TP’s head with two headblocks (Combi Head Immobiliser, Ferno; Troisdorf, Germany; Figure 2A).
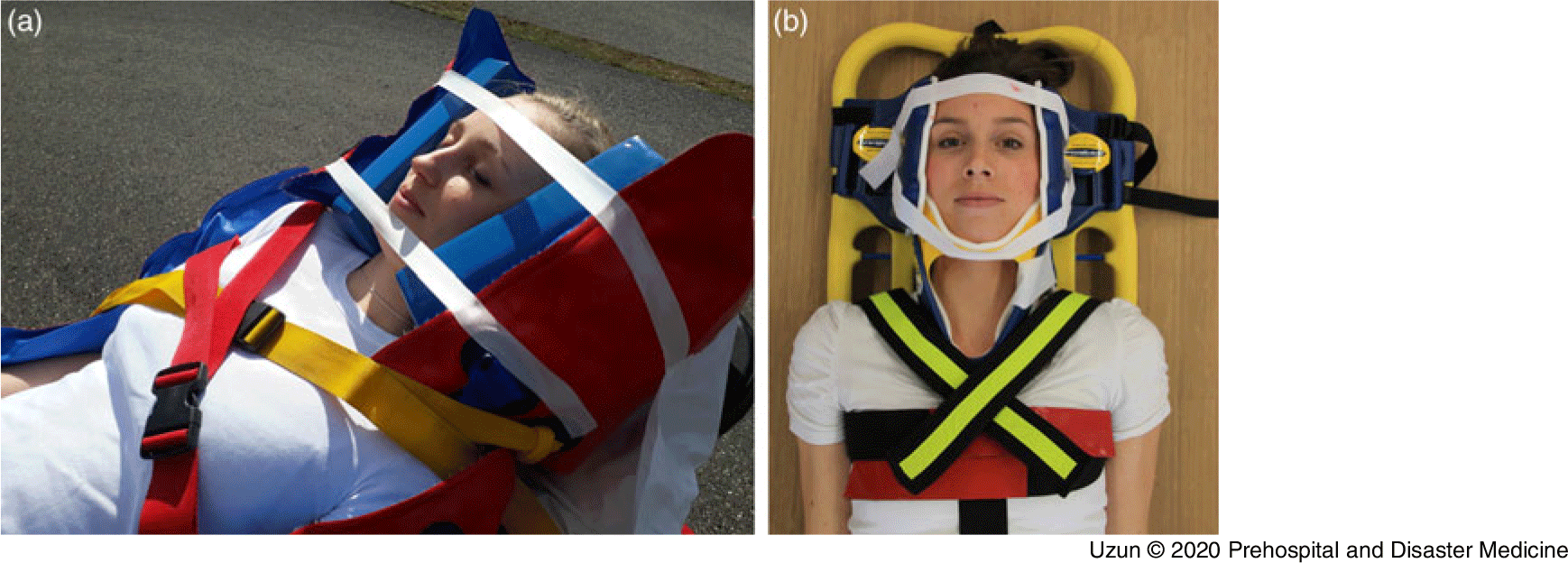
Figure 2. Cervical Spine Immobilization in Case of Severe Traumatic Brain Injury.
To simulate the immobilization of the cervical spine in patients with severe traumatic brain injury, an inclined (30°) vacuum mattress was used in a second test run. Therefore, no additional collar was used in this scenario (Figure 2A). In severe traumatic brain injuries, positioning the patient with the trunk and head 30° upright is recommended, while the use of a cervical collar can lead to severe complications.15
Spine Board—The cervical spine was immobilized by immobilizing the TP in the supine position on a spine board (BaXstrap, Laerdal; Stavanger, Norway). The head was fixed with a headlock system (Speedblocks, Laerdal; Stavanger, Norway). The immobilization was carried out with and without an additional collar (Figure 2B). Also, two different fixation systems for the patient’s body were analyzed: the immobilization Spider Strap (MIH-Medical; Georgsmarienhütte, Germany; Figure 2B) and the immobilization Speedclip belt system (Laerdal; Stavanger, Norway). The Speedclip belt system is attached to the spine board with a snap hook. This allows the patient to be fixed to the spine board more quickly.
Statistics
There have been no studies addressing the amount or type of movements that will further damage an already traumatized cervical spine. Also, it is not clear whether the direction of the remaining cervical spine movement is important after immobilization. Therefore, it is not possible to define significant differences between different immobilization techniques. Thus, a sample size calculation is not possible. Therefore, the current study focuses on an exploratory analysis that provides only descriptive data. All values are given as median and range.
Results
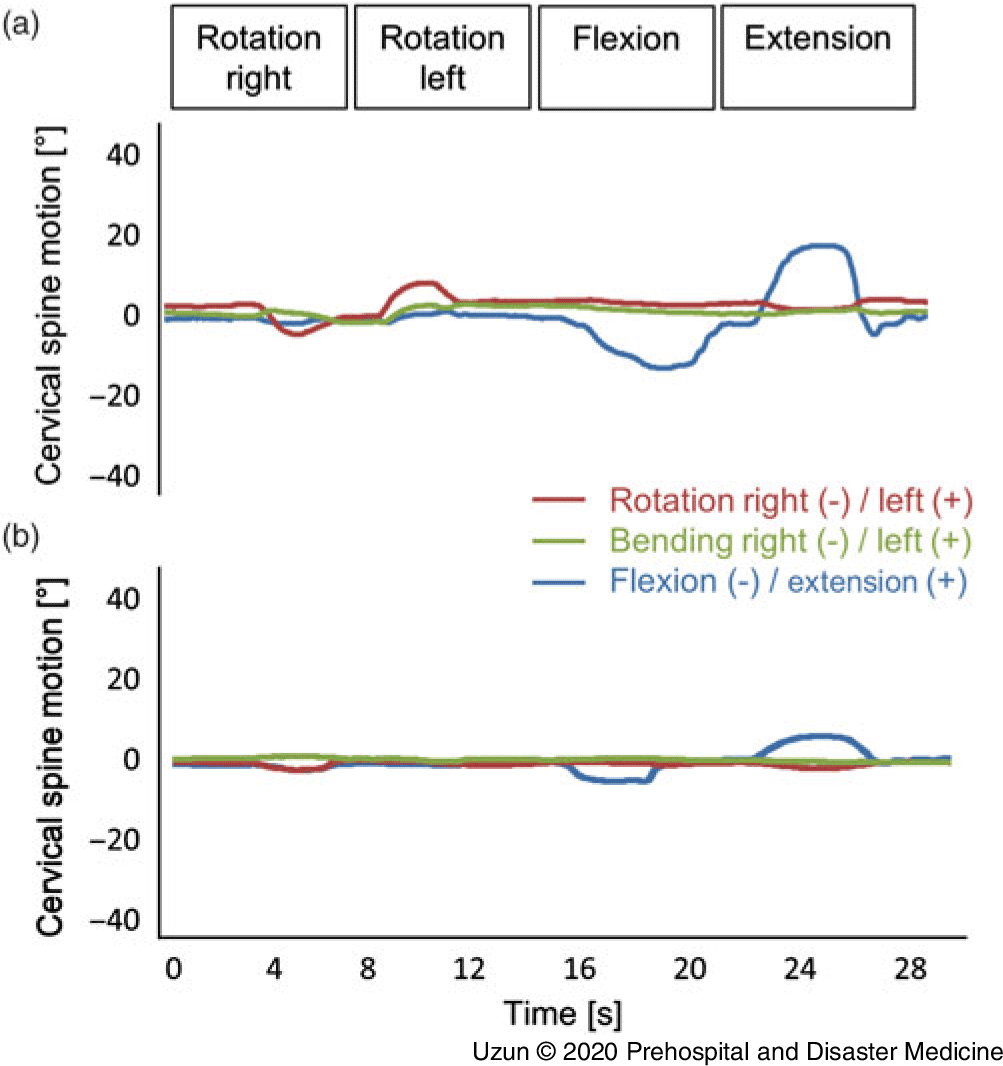
In the case of immobilization of the TPs with a neck collar on a straight vacuum mattress, the remaining movement of the cervical spine could be reduced by additional headblocks (Figure 3). The mean rotation of all subjects was reduced from 7° (range: 6° to 7°; n = 3) to 3° (1° to 5°). Also, the remaining flexion and extension were reduced from 14° (11° to 16°) to 3° (1° to 5°) and from 15° (13° to 18°) to 6° (5° to 8°; Table 2). The remaining side bending was in the same range, regardless of the use of additional headblocks (Table 2).
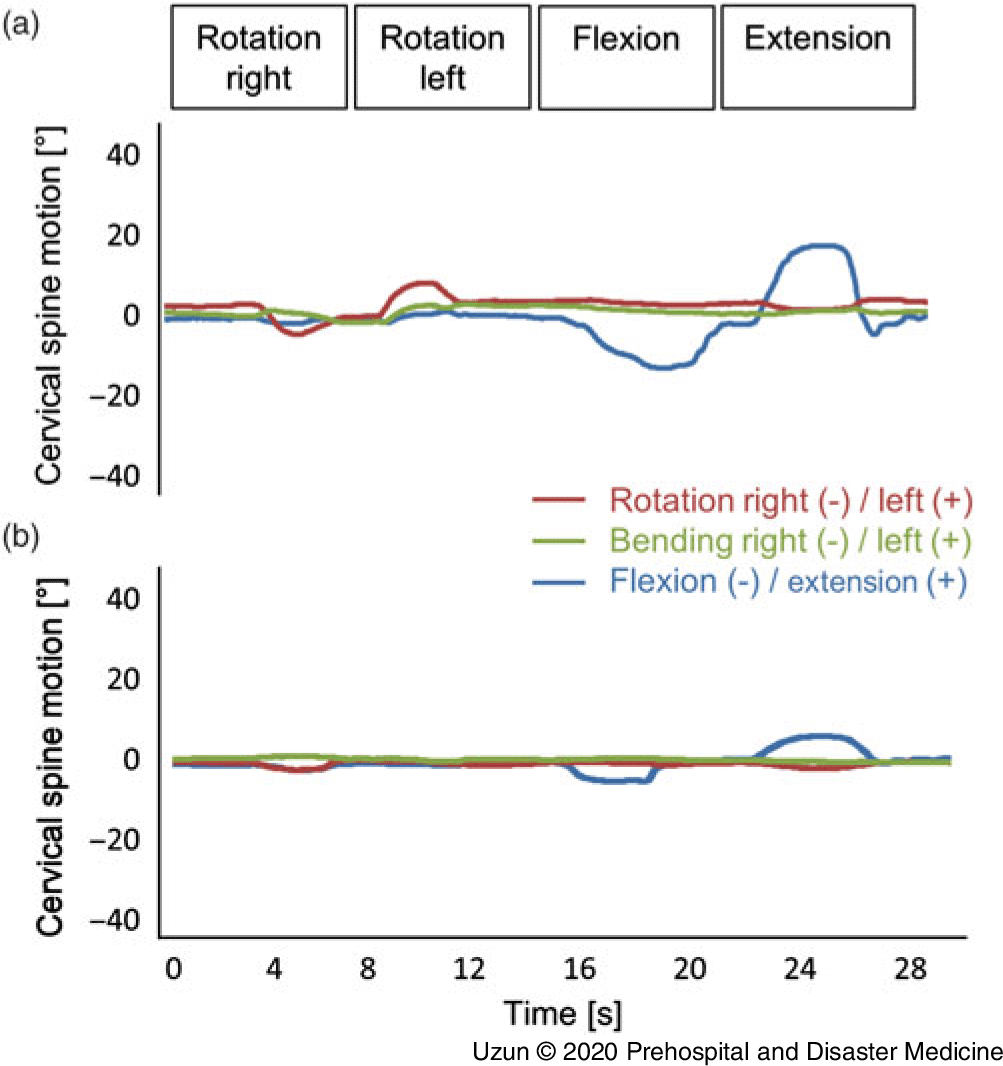
Figure 3. Cervical Spine Motion during Passive Movement.
Table 2. Maximal Remaining Cervical Spine Movement under Different Immobilization Techniques
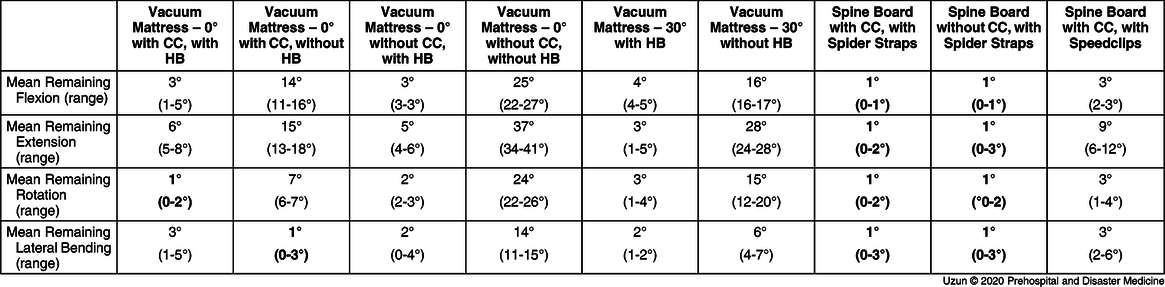
Abbreviations: CC, cervical collar; HB, headblock.
If additional headblocks were used during immobilization on a straight vacuum mattress, the additional use of a neck collar did not seem to be of much benefit; the mean remaining flexion and extension did not increase in the absence of a neck collar (Table 2).
The immobilization of the TP only on a straight vacuum mattress without the additional use of a cervical collar and headblocks lead to a significantly increased residual movement of the cervical spine in all directions; the remaining flexion and extension increased up to 25° (22° to 27°) and 37° (33° to 34°), respectively. The residual rotation (24°) and the lateral bending (14°) were also increased (Table 2).
If a spine board was used to immobilize the cervical spine, so-called headlocks (Figure 1) were a matter of course. The immobilization of the TPs was better on a spine board compared to immobilization on a vacuum mattress; when using the Spider Strap belt system (Figure 2B), the mean remaining cervical spine movement was 1° in each direction (Table 2). The additional use of a cervical collar could not further improve the immobilization of the cervical spine on a spine board (Table 2). However, the remaining cervical spine extension increased from 1° (0° to 2°) to 9° (6° to 12°) if a Speedclip belt system was used instead of the Spider Strap belt system (Table 2).
Discussion
Previous studies showed that immobilization of the cervical spine is best if full body immobilization is performed.Reference Horodyski, DiPaola, Conrad and Rechtine23-Reference Chandler, Nemejc, Adkins and Waters25 Therefore, only different techniques of cervical spine immobilization were analyzed that were all based on full body immobilization. The study found that immobilization of the cervical spine is most effective by attaching the patient’s head and torso to a spine board using a Spider Strap belt system. Comparable results have already been described.Reference Johnson, Hauswald and Stockhoff26 The remaining movement of the cervical spine increases when the Speedclip belt system is used alternatively.
However, the remaining movement of the cervical spine when immobilized on a spine board with the Spider Strap harness system is in the same range as immobilized on a vacuum mattress when additional headblocks are used.
Current scientific literature reports on the immobilization of the patient on a spine board coming along with many possible complications; due to the stiffness of the spine board, patients complain of pain when lying on a it.Reference Cordell, Hollingsworth, Olinger, Stroman and Nelson7,Reference Cross and Baskerville27-Reference Chan, Goldberg, Mason and Chan30 Moreover, lying on a spine board can cause pressure ulcers.Reference Berg, Nyberg, Harrison, Baumchen, Gurss and Hennes31 Both effects can be reduced by the use of soft toppings on the spine board,Reference Hemmes, Poeze and Brink32-Reference Sheerin and de Frein34 but this might impair patient transfer on the spine board. Furthermore, the immobilization on a spine board can cause restrictive effects on pulmonary function.Reference Bauer and Kowalski35
Since the above-mentioned complications have not been described during the immobilization of the patient on a vacuum mattress, it should be noted that immobilization on a vacuum mattress is preferred. Also, immobilization on a vacuum mattress should take less time.Reference Johnson, Hauswald and Stockhoff26 However, the analysis shows that to sufficiently limit the remaining cervical spine movement, additional headblocks have to be used.
In the present study, the additional use of a cervical collar does not further reduce the movement of the cervical spine when combined with either a spine board or a vacuum mattress. These results are supported by other studies analyzing the effects of cervical collars.Reference Butler and Bates37,Reference Ala, Shams-Vahdati and Taghizadieh38 Because many complications seem to accompany the use of a cervical collar,Reference Sundstrom, Asbjornsen, Habiba, Sunde and Wester4,Reference Holla36-Reference Ala, Shams-Vahdati and Taghizadieh38 it remains questionable if the general application of a cervical collar in almost every trauma patient represents best practice.
One of the most severe complications associated by the use of a cervical collar is the possibility of increased intracranial pressure.Reference Davies, Deakin and Wilson5,Reference Kolb, Summers and Galli39 Especially in patients with severe traumatic brain injury, a further increase in intracranial pressure can drastically worsen the patient’s outcome. In the specific case of a severe traumatic brain injury, it is recommended that the patient is placed in an inclined, almost seated position (30°) to facilitate venous drainage from the brain. However, since a traumatic brain injury is often accompanied by an injury to the cervical spine, the cervical spine should be immobilized in these patients. Thus, it is recommended to consider immobilization techniques other than the use of a collar.40,Reference Kreinest, Gliwitzky, Schuler, Grutzner and Munzberg41 The patient’s inclined position and an acceptable immobilization of the cervical spine could be achieved by placing the patient on a vacuum mattress that lies on a stretcher and is inclined by 30° as described above (Figure 2A).Reference Kreinest, Gliwitzky, Schuler, Grutzner and Munzberg41 The current study shows that the remaining cervical spine motions are within the same range when comparing the immobilization on a straight vacuum mattress and on a spine board. Additional headblocks are essential in this case.
Limitations
This study has some limitations. The study population consisted of three healthy volunteers of normal body shape with full compliance and without injury to the cervical spine. Also, the passive, unidirectional movement of the cervical spine was highly standardized. Thus, the results in real patients can be different if multidirectional forces influence a conscious patient.
Therefore, the aim of the study was to focus on descriptive statistics and avoid calculating significant differences between the different immobilization techniques. Apart from statistical values, it is not yet clear how much residual movement of the cervical spine can cause further damage to an injured cervical spine. Many factors, such as the exact nature of the injury, the location of the injury, the patient’s muscle tone, and the patient’s body shape, among others, can influence the dependence of the height of spinal movement on whether an injured spine will be further damaged.
However, the results of the current study give a first idea of the remaining movement of the cervical spine using various immobilization techniques. Thus, further investigations can be based on these data.
Conclusion
There are several techniques for prehospital immobilization of trauma patients. Based on the results and taking into account further data from the current scientific literature, the following conclusions can be drawn:
1. The remaining movement of the cervical spine is the least when the patient is immobilized on a spine board with a headlock system and a Spider Strap harness system.
2. The remaining movement of the cervical spine is in the same range when a vacuum mattress and additional headblocks are used to immobilize the patient. The complication rate can be reduced by using a vacuum mattress.
3. Regardless of whether a spine board or vacuum mattress is used, as described above, the additional use of a cervical collar does not improve the immobilization of the patient’s cervical spine. And,
4. In the case of severe traumatic brain injury, an alternative immobilization technique may be considered; the immobilization of the patient on an inclined (30°) vacuum mattress with additional headblocks, but without cervical collar, is as good as the immobilization on a straight vacuum mattress and leads to an absolutely acceptable residual amount of cervical spine movement.
Conflicts of interest/funding
Funding received from the BG Trauma Centre Ludwigshafen, Germany; the German Association of Emergency Medical Technicians (Deutscher Berufsverband Rettungsdienst e.V. DBRD; Lübeck, Germany); and the Friends Association of the Air Rescue Centre Frankfurt, Germany. The sponsors did not influence the study design, data collection and analysis, decision to publish, or preparation of the manuscript. All authors declare that they have no competing interests.
Author Contributions
MK and DH were the principal investigators in the study and developed the study design. DDU, JW, MKJ, PAG, and MM assisted in developing the study design. JONW developed measurement procedures. DH and MK planned the logistics and testing processes. Data acquisition was performed by DDU, DH, MK, and JW. Data evaluation was performed by DDU, DH, MK, JW, and MKJ; while DDU, MKJ, and MK drafted the manuscript and undertook the final write up.
Acknowledgments
The authors would like to thank all participating staff. Furthermore, they thank the team from the Fire and Rescue Training Centre (FRTC) of the Frankfurt, Germany Fire Department.